The Lemonade Diet
The Lemonade Diet, also called the Master Cleanse, is a liquid-only diet consisting of three things: a lemonade-like beverage, salt-water drink, and herbal laxative tea.
Celebrities including Beyoncé have used this diet. But it’s far from the principles of healthy eating, and the results aren’t likely to last.
The claim is simple: Give it 10 days (or more) and you’ll drop pounds, “detox” your digestive system, and feel energetic, vital, happy, and healthy. You’ll also curb cravings for unhealthy food.
Does It Work ?
Because you’re getting so few calories, you’ll probably lose weight. You’ll also be losing muscle, bone, and water. And you’re likely to gain the weight right back.
It’s an unhealthy way to temporarily lose weight.
There’s no proof that detoxifying leads to long-term weight loss. Plus, you don’t need to detox your body — your liver takes care of that.
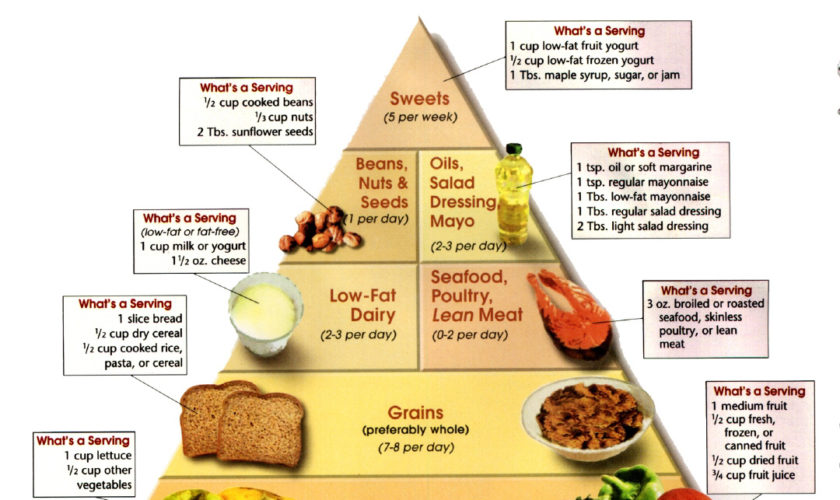
For lasting change, you’re better off eating a healthy diet of fruits, vegetables, whole grains, low-fat dairy, and lean proteins like fish, skinless chicken or turkey, and healthy fats like olive oil.
What You Can Eat and What You Can’t
You’re only allowed a salt-water drink, a “lemonade,” and an herbal laxative tea for the first 10 days. You can’t have any solid food, and you can’t drink alcohol.
After 10 days, you can gradually add back foods, but only a few at first, starting with juice and soup, and leading to raw fruits and vegetables. After this, the plan calls for eating very little meat and no dairy.
Conclusion: This is not a diet we recommend. If weight loss is the goal, it is better to lose weight gradually with a balanced diet that makes sure you get the nutrients you need. Cross this one off your list.
What is Detox ?
Before it was co-opted in the recent craze, the word “detox” referred chiefly to a medical procedure that rids the body of dangerous, often life-threatening, levels of alcohol, drugs, or poisons. Patients undergoing medical detoxification are usually treated in hospitals or clinics. The treatment generally involves the use of drugs and other therapies in a combination that depends on the type and severity of the toxicity. 1
The detox programs now being promoted to the health-conscious public are a different matter. These are largely do-it-yourself procedures aimed at eliminating alleged toxins that are held responsible for a variety of symptoms, including headache, bloating, joint pain, fatigue, and depression. Detox products are not available by prescription; they are sold in retail stores, at spas, over the Internet, and by direct mail. Many are advertised as useful for detoxifying specific organs or systems; others are portrayed as “whole body” cleansers. Here is a review of some of the most widely promoted procedures and products.
Detox Diets
A seemingly infinite array of products and diets is available for detoxifying the entire body. One of the most popular is the Master Cleanse diet, favored by a number of Hollywood celebrities. Dieters take a quart of warm salt water in the morning; consume a 60-ounce concoction of water, lemon juice, maple syrup, and cayenne pepper throughout the day; and finish with a cup of laxative tea in the evening. Proponents of the Master Cleanse diet recommend adhering to it for at least 10 days.
Purpose : To restore energy, lose weight, and relieve symptoms of chronic conditions like arthritis and fibromyalgia.
Evidence of effectiveness : There are no data on this particular diet in the medical literature. But many studies have shown that fasts and extremely low-calorie diets invariably lower the body’s basal metabolic rate as it struggles to conserve energy. Once the dieter resumes normal eating, rapid weight gain follows. Much of the weight loss achieved through this diet results from fluid loss related to extremely low carbohydrate intake and frequent bowel movements or diarrhea produced by salt water and laxative tea. When the dieter resumes normal fluid intake, this weight is quickly regained.
Risks : The diet is lacking in protein, fatty acids, and other essential nutrients. Carbohydrates supply all the calories — an extremely low 600. The daily laxative regimen can cause dehydration, deplete electrolytes, and impair normal bowel function. It can also disrupt the native intestinal flora, microorganisms that perform useful digestive functions. A person who goes on this diet repeatedly may run the risk of developing metabolic acidosis, a disruption of the body’s acid-base balance, which results in excessive acidity in the blood. Severe metabolic acidosis can lead to coma and death.
Cost : The price of the book and a handful of food items.
Intestinal Cleansing
Numerous kits are marketed for this purpose, most of which include a high-fiber supplement, a “support” supplement containing herbs or enzymes, and a laxative tea, each to be used daily. Manufacturers of the herbal detox kits recommend continuing the regimen for several weeks. Such regimens may be accompanied by frequent enemas.
Purpose : The aim is to eradicate parasites and expel fecal matter that allegedly accumulates and adheres to the intestinal walls.
Evidence of effectiveness : Several studies suggest that milk thistle, which is often included as a supportive supplement, may improve liver function with few side effects. But there’s no medical evidence for the cleansing procedure as a whole. Promotional materials often include photographs of snake-like gelatinous substances expelled during cleansing. When these pictures are not faked, they are probably showing stool generated by large doses of the regimen’s fiber supplement. More important, the rationale for intestinal cleansing — to dislodge material adhering to the colon walls — is fundamentally mistaken. When fecal matter accumulates, it compacts into firm masses in the open interior of the colon; it does not adhere to the intestinal walls as the “sludge” depicted in the advertisements.
Risks : Like fasting, colonic cleansing carries a risk of dehydration, electrolyte imbalance, impaired bowel function, and disruption of intestinal flora.
Cost : A month’s supply of the supplements and laxatives sold on most Web sites is $20 to $70. The manufacturers recommend continuing the procedure for two to three months.
Foot detox
One method employs a special type of adhesive pad worn on the bottoms of the feet during sleep. Another approach is to immerse the feet for 30 minutes in a basin, sometimes referred to as an “ionic foot bath,” containing salt water and two electrodes that supply a low-voltage electric charge.
Purpose : Toxins are allegedly drawn out of the body through the soles of the feet.
Evidence of effectiveness. Both methods claim to emit ions that stimulate the outflow of toxins through the feet. The pads contain tourmaline crystals, which are purported to emit ion-generating infrared rays. The foot baths allegedly generate ions by running an electric current through salt water. However, there is no scientific evidence that ionic changes in the environment can stimulate a discharge of toxins through pores in the feet — or any other part of the body, for that matter. Promoters assert that the success of the process can be monitored by a color change in the pad or in the water of the foot bath as impurities are leached from the body. But the pads, which are impregnated with wood vinegar, have been shown to turn the same dark color whether they absorb foot perspiration or are sprayed with tap water; and the color of the foot bath changes because the metal electrodes corrode.
Risks : No ill effects on health have been reported for either method.
Cost : Single-use pads average $1. Ionic foot bath sessions are available at spas for $40 to $50. Ionic foot bath devices are sold online at prices ranging from $85 to $2,000.
References