What is L-Glutamine
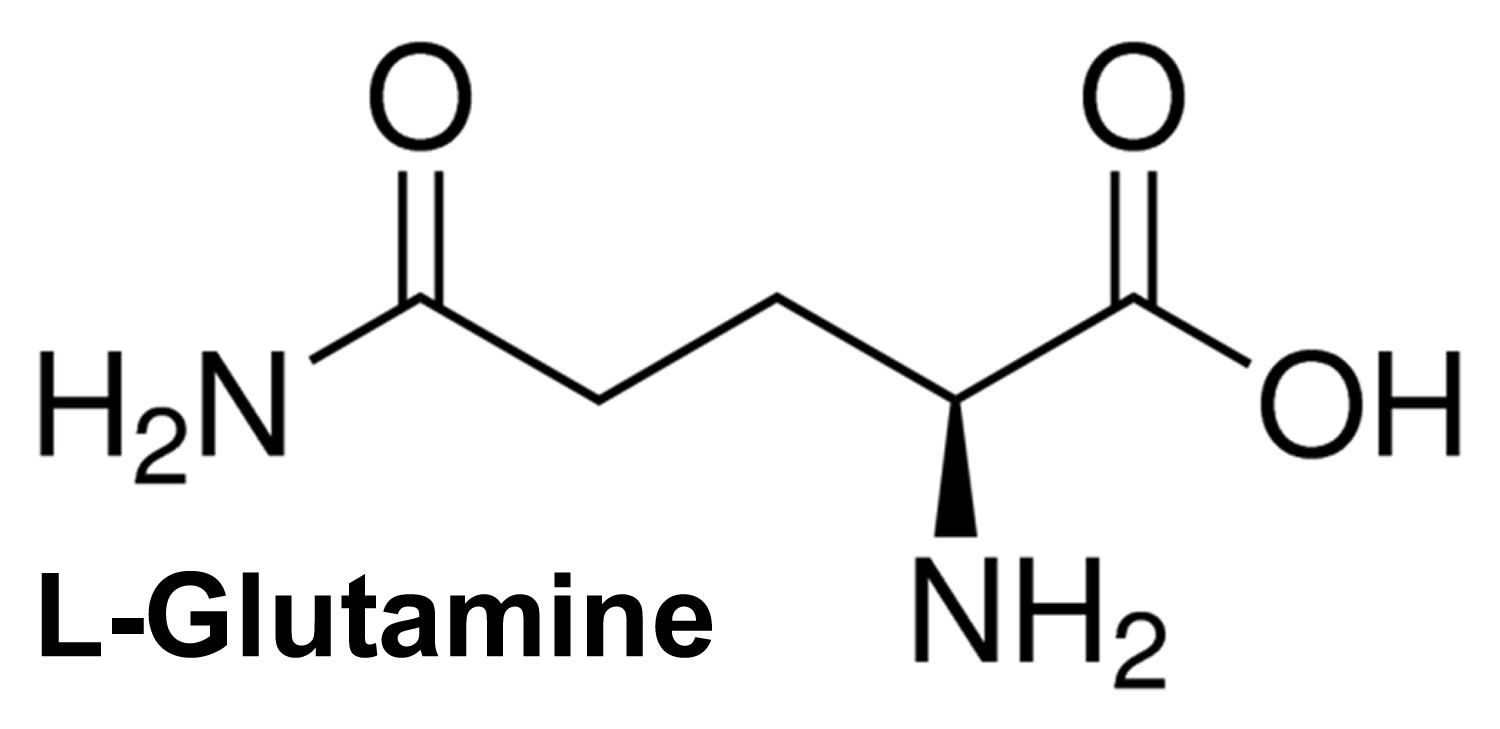
L-glutamine is in a class of medications called amino acids. It works by helping to prevent damage to red blood cells. L-glutamine is a non-essential branched-chain amino acid that is present abundantly throughout the body and is involved in many metabolic processes 1. L-glutamine is an important non-toxic nitrogen carrier in the body and an essential component of diet, especially dairy products, fish and green leafy vegetables 2. L-glutamine participates in a variety of physiological functions, and is a major fuel source of enterocytes (intestine or gut cells) and is a substrate for gluconeogenesis (glucose formation) in the kidney, lymphocytes (white blood cells) and monocytes (white blood cells). L-glutamine is also a nutrient in muscle protein metabolism in response to infection, inflammation and muscle trauma 3. Because of glutamine’s importance as a nitrogen carrier and respiratory fuel for enterocytes of the gut and other rapidly proliferating cells, including lymphocytes and fibroblasts, glutamine can be considered as a conditionally essential amino acid 4. Although there are no known drug interactions with glutamine, physiological antagonism may occur with lactulose when given to treat high ammonia levels in liver failures. In some patients, glutamate may lead to brain excitation, and in patients with seizure, may make the drug less effective.
L-glutamine is used by doctors as prescription medicine to reduce the frequency of painful episodes (crises) in adults and children 5 years of age and older with sickle cell anemia (an inherited blood disorder in which the red blood cells are abnormally shaped [shaped like a sickle] and cannot bring enough oxygen to all parts of the body) 5. And L-glutamine is often prescribed to treat short bowel syndrome (short gut syndrome). Glutamine is used together with human growth hormone and a specialized diet to treat short bowel syndrome. This medicine is available only with your doctor’s prescription.
- L-glutamine has Pregnancy Category C: Animal studies have shown an adverse effect and there are no adequate studies in pregnant women OR no animal studies have been conducted and there are no adequate studies in pregnant women.
- Breast Feeding: There are no adequate studies in women for determining infant risk when using this medication during breastfeeding. Weigh the potential benefits against the potential risks before taking this medication while breastfeeding.
In addition to L-glutamine usage in sickle cell anemia and short bowel syndrome, L-glutamine supplement may have an important role in the prevention of gastrointestinal, neurologic and, possibly, cardiac complications of cancer therapy 2. The influence of glutamine on body homeostasis is protean (able to do many different things, versatile). States of physiologic stress, including those resulting from the treatment of malignant disease, are characterized by a relative deficiency of glutamine. These complications often negatively affect the quality of life and may also lead to changes in therapy, which potentially alter efficacy. L-glutamine may also improve the therapeutic index of both chemotherapy and radiation, increasing cytotoxicity while concurrently protecting against toxicity. However, the current evidence is not sufficient to recommend its regular use. Further studies of glutamine supplementation in these areas is warranted and multicentric, placebo-controlled phase III studies are needed to evaluate the role of L-glutamine for the prevention of mucositis, neurotoxicity and cardiotoxicity, and for the prevention of hepatic venoocclusive disease in patients undergoing hematopoietic cell transplantation before any definitive recommendation can be made.
Figure 1. L-Glutamine
What does L-glutamine do?
Glutamine is a major component of tissue of the skeletal muscle, which is the main site for the synthesis and storage of L-glutamine. When the supply of glutamine in plasma is inadequate to meet the demand, glutamine synthesis occurs in skeletal muscle and liver. Glutamine is transported to the neurons and, by the enzyme glutaminase, is converted to glutamate – the potential excitotoxin. L-glutamine accounts for 30–35% of the amino acid nitrogen in the plasma. It contains two ammonia groups, one from its precursor, glutamate, and the other from free ammonia in the bloodstream. Glutamine plays an important role to prevent fluctuations in the levels of ammonia in blood by acting as a “nitrogen shuttle.” It does so by acting as a buffer, accepting and then releasing excess ammonia when needed to form other amino acids, amino sugars, nucleotides and urea. This capacity to accept and donate nitrogen makes glutamine the major vehicle for nitrogen transfer among tissues. Glutamine is one of the three amino acids involved in glutathione synthesis. Glutathione synthesis, an important intracellular antioxidant and hepatic detoxifier, is comprised of glutamic acid, cysteine and glycine 6. Glutamine is one of the most important substrates for ammoniagenesis in the gut and the kidney due to its important role in the regulation of acid–base homeostasis 7. It decomposes readily to yield ammonia and glutamate or via intramolecular catalysis to pyroglutamate. Deamidation of glutamine via the enzyme glutaminase produces glutamate, a precursor of gamma-amino butyric acid. The transfer of the amide nitrogen from glutamine via the amido transferase reaction is involved in the biosynthesis of purines and pyrimidines and in the production of hexosamines. Glutamine via glutamate is converted to α-ketoglutarate, an integral component of the citric acid cycle. It is a component of the antioxidant glutathione synthesis and of the polyglutamated folic acid. The cyclization of glutamate produces proline, an amino acid important for the synthesis of collagen and connective tissue. However, excess glutamine in a protein is of pathological importance, and a number of neurodegenerative diseases have been found to be due to a CAG expansion that causes expansion of glutamine repeats in affected proteins (CAA and CAG codons are responsible for the insertion of glutamine from its transfer RNA with its anti-codon triplet into the genetically determined position of the coded polypeptide chain). This leads to abnormal protein folding 8 and neuronal diseases 9.
Glutamine is involved in many metabolic processes in the body. Glutamine is converted to glucose when more glucose is required by the body as an energy source. Glutamine also plays a part in maintaining proper blood glucose levels and the right pH range. It is also used by white blood cells and is important for immune function. Glutamine assists in maintaining the proper acid/alkaline balance in the body, and is the basis of the building blocks for the synthesis of RNA and deoxyribonucleic acid (DNA). Glutamine regulates the expression of certain genes, including those that govern certain protective enzymes, and helps regulate the biosynthesis of DNA and RNA. Construction of DNA is dependent on adequate amounts of glutamine. It also increases the body’s ability to secrete human growth hormone, which assists in metabolizing body fat and helps to support new muscle tissue growth. The glutamic acid–glutamine interconversion is of central importance to the regulation of the levels of toxic ammonia in the body, and thus among all the amino acids of blood plasma, glutamine has the highest concentration.
L-glutamine benefits
Glutamine is one of the most common plasma amino acids, and its concentration often decreases post-operatively 10, during sepsis 11 and after multiple trauma 12 or major burns 13, similar to a fall in the concentrations of many other amino acids, electrolytes, minerals and trace elements; therefore, it seems prudent to give glutamine supplementation in all these conditions 14.
Short Bowel Syndrome
Short bowel syndrome is a group of problems related to poor absorption of nutrients. Short bowel syndrome typically occurs in people who have:
- had at least half of their small intestine removed and sometimes all or part of their large intestine removed
- significant damage of the small intestine
- poor motility, or movement, inside the intestines
Short bowel syndrome may be mild, moderate, or severe, depending on how well the small intestine is working.
People with short bowel syndrome cannot absorb enough water, vitamins, minerals, protein, fat, calories, and other nutrients from food. What nutrients the small intestine has trouble absorbing depends on which section of the small intestine has been damaged or removed.
What causes Short Bowel Syndrome ?
The main cause of short bowel syndrome is surgery to remove a portion of the small intestine. This surgery can treat intestinal diseases, injuries, or birth defects.
Some children are born with an abnormally short small intestine or with part of their bowel missing, which can cause short bowel syndrome. In infants, short bowel syndrome most commonly occurs following surgery to treat necrotizing enterocolitis, a condition in which part of the tissue in the intestines is destroyed 15.
Short bowel syndrome may also occur following surgery to treat conditions such as:
- cancer and damage to the intestines caused by cancer treatment
- Crohn’s disease, a disorder that causes inflammation, or swelling, and irritation of any part of the digestive tract
- gastroschisis, which occurs when the intestines stick out of the body through one side of the umbilical cord
- internal hernia, which occurs when the small intestine is displaced into pockets in the abdominal lining
- intestinal atresia, which occurs when a part of the intestines doesn’t form completely
- intestinal injury from loss of blood flow due to a blocked blood vessel
- intestinal injury from trauma
- intussusception, in which one section of either the large or small intestine folds into itself, much like a collapsible telescope
- meconium ileus, which occurs when the meconium, a newborn’s first stool, is thicker and stickier than normal and blocks the ileum
- midgut volvulus, which occurs when blood supply to the middle of the small intestine is completely cut off
- omphalocele, which occurs when the intestines, liver, or other organs stick out through the navel, or belly button
Even if a person does not have surgery, disease or injury can damage the small intestine.
How common is Short Bowel Syndrome ?
Short bowel syndrome is a rare condition. Each year, short bowel syndrome affects about three out of every million people 15.
What are the signs and symptoms of Short Bowel Syndrome ?
The main symptom of short bowel syndrome is diarrhea—loose, watery stools. Diarrhea can lead to dehydration, malnutrition, and weight loss. Dehydration means the body lacks enough fluid and electrolytes—chemicals in salts, including sodium, potassium, and chloride—to work properly. Malnutrition is a condition that develops when the body does not get the right amount of vitamins, minerals, and nutrients it needs to maintain healthy tissues and organ function. Loose stools contain more fluid and electrolytes than solid stools. These problems can be severe and can be life threatening without proper treatment.
Other signs and symptoms may include:
- bloating
- cramping
- fatigue, or feeling tired
- foul-smelling stool
- heartburn
- too much gas
- vomiting
- weakness
People with short bowel syndrome are also more likely to develop food allergies and sensitivities, such as lactose intolerance. Lactose intolerance is a condition in which people have digestive symptoms—such as bloating, diarrhea, and gas—after eating or drinking milk or milk products.
What are the complications of Short Bowel Syndrome ?
The complications of short bowel syndrome may include
- malnutrition
- peptic ulcers—sores on the lining of the stomach or duodenum caused by too much gastric acid
- kidney stones—solid pieces of material that form in the kidneys
- small intestinal bacterial overgrowth—a condition in which abnormally large numbers of bacteria grow in the small intestine
How is Short Bowel Syndrome treated ?
A health care provider will recommend treatment for short bowel syndrome based on a patient’s nutritional needs. Treatment may include
- nutritional support
- medications
- surgery
- intestinal transplant
Nutritional Support
The main treatment for short bowel syndrome is nutritional support, which may include the following:
- Oral rehydration. Adults should drink water, sports drinks, sodas without caffeine, and salty broths. Children should drink oral rehydration solutions—special drinks that contain salts and minerals to prevent dehydration—such as Pedialyte, Naturalyte, Infalyte, and CeraLyte, which are sold in most grocery stores and drugstores.
- Parenteral nutrition. This treatment delivers fluids, electrolytes, and liquid vitamins and minerals into the bloodstream through an intravenous (IV) tube—a tube placed into a vein. Health care providers give parenteral nutrition to people who cannot or should not get their nutrition or enough fluids through eating.
- Enteral nutrition. This treatment delivers liquid food to the stomach or small intestine through a feeding tube—a small, soft, plastic tube placed through the nose or mouth into the stomach. Gallstones—small, pebble like substances that develop in the gallbladder—are a complication of enteral nutrition.
- Vitamin and mineral supplements. A person may need to take vitamin and mineral supplements during or after parenteral or enteral nutrition.
- Special diet. A health care provider can recommend a specific diet plan for the patient that may include:
- small, frequent feedings
- avoiding foods that can cause diarrhea, such as foods high in sugar, protein, and fiber
- avoiding high-fat foods.
Bone marrow transplant
Bone marrow transplant is a sophisticated procedure consisting of the administration of high-dose chemoradiotherapy followed by intravenous infusion of hemopoietic stem cells to re-establish marrow function when the bone marrow is damaged or defective. Bone marrow transplant is used in the treatment of solid tumors, hematological diseases and autoimmune disorders. Glutamine has protein-anabolic effects and has shown a clear reduction of complications in patients undergoing bone marrow transplant who exhibit post-transplant body protein wasting, gut mucosal injury leading to mucositis of gastrointestinal tract, acute graft versus host disease and immunodeficiency. Studies indicate that enteral and parenteral glutamine supplementation is well tolerated and potentially efficacious after high-dose chemotherapy or bone marrow transplant for cancer treatment. Although not all studies demonstrate benefits, sufficient data has been published to suggest that this nutrient should be considered as adjunctive metabolic support of some individuals undergoing marrow transplant 16. However, bone marrow transplant is a rapidly evolving clinical procedure with regard to the conditioning and supportive protocols used. Thus, additional randomized, double-blind, controlled clinical trials are indicated to define the efficacy of glutamine with current bone marrow transplant regimens 17.
Glutamine and Cancer
Numerous studies on glutamine metabolism in cancer indicate that many tumors are avid glutamine consumers in vivo and in vitro. As a consequence of progressive tumor growth, host glutamine depletion develops and becomes a hallmark. This glutamine depletion occurs in part because the tumor behaves as a “glutamine trap” and also because of cytokine-mediated alterations in glutamine metabolism in host tissues. Animal and human studies that have investigated the use of glutamine-supplemented nutrition in the host with cancer suggest that pharmacologic doses of dietary glutamine may be beneficial. Understanding the control of glutamine metabolism in the tumor-bearing host not only improves the knowledge of metabolic regulation in the patient with cancer but also leads to improved nutritional support regimens targeted to benefit the host.
Glutamine supplementation in chemotherapy
The results of glutamine supplementation and oncology in animals and humans are conflicting 18. In vitro (test tube) studies reveal an increase in cellular growth with glutamine supplementation 19. While in vivo (animal) studies show the opposite effect, i.e. reduction in tumor growth 20. Glutamine uptake in patients with colon cancer, regardless of tumor size and cell type, is comparable to uptake in patients with healthy intestinal tissue 21, also enteral diet containing glutamine increase muscle glutamine in rats by 60% without increasing tumor growth or tumor glutamine use 22. Glutamine supplementation in rats receiving methotrexate chemotherapy causes reduction in methotrexate-induced side-effects, including mucositis, and improved survival is observed 23. Mucosal ulceration in rats subjected to abdominal radiation is also prevented 24.
GLUTAMINE: ROLE IN INCREASING SELECTIVITY OF CHEMOTHERAPEUTIC AGENTS
Chemotherapy doses are limited by toxicity to normal tissues. Intravenous glutamine protects liver cells from oxidant injury by increasing intracellular glutathione synthesis content 25. The effects of oral glutamine on tumor and host glutathione synthesis metabolism and response to methotrexate have been studied in rat models of sarcoma as well as in human patients with inflammatory breast cancer. Feeding the glutamine-enriched diets to rats receiving methotrexate decreases tumor glutathione synthesis while increasing or maintaining host glutathione synthesis stores 26. Diminished glutathione synthesis levels in tumor cells increases susceptibility to chemotherapy. Significantly decreased glutathione synthesis content in tumor cells in the glutamine-supplemented group correlates with enhanced tumor volume loss 27. These data suggest that oral glutamine supplementation will enhance the selectivity of antitumor drugs by protecting normal tissues from and possibly sensitizing tumor cells to radiation-induced and chemotherapy treatment-related injury 28.
GLYCYL-GLUTAMINE-DIPEPTIDE IN THE PARENTERAL NUTRITION OF PATIENTS WITH ACUTE LEUKEMIA UNDERGOING INTENSIVE CHEMOTHERAPY
The effects of parenteral glycyl-glutamine supplementation in patients with acute leukemia receiving intensive conventional chemotherapy was evaluated in a randomized, double-blind, controlled study that compared a standard glutamine-free parenteral nutrition with a glycyl-glutamine-supplemented parenteral nutrition containing 20 g of glutamine. There was significant faster neutrophil recovery in the group that received glutamine supplementation along with high-dose cytarabine chemotherapy as compared with those patients receiving cytarabine regimen alone. There was no significant difference in the recovery of CD4+ or CD8+ lymphocytes or monocyte activation between the two groups. The authors concluded that there is a possible role of glutamine in the stimulation of lymphocyte proliferation 29.
Other Uses of L-glutamine
Possibly Effective for:
- Burns. Administering glutamine through a feeding tube or intravenously (by IV) seems to reduce infections, shorten hospital stays, and improve wound healing in people with burns.
- Critical illness (trauma). There is some evidence that glutamine keeps bacteria from moving out of the intestine and infecting other parts of the body after major injuries. However, not all evidence is consistent. It is not clear if glutamine reduces the risk of death in critically ill people. Some studies suggest that it might reduce the risk of death, while others do not.
- Treating weight loss and intestinal problems in people with HIV/AIDs disease. Taking glutamine by mouth seems to help HIV/AIDS patients absorb food better and gain weight. Doses of 40 grams per day seem to produce the best effect.
- Soreness and swelling inside the mouth, caused by chemotherapy treatments. Some evidence suggests that glutamine reduces soreness and swelling inside the mouth caused by chemotherapy. However, glutamine does not seem to have this effect for all chemotherapy patients. It is not clear which patients are likely to benefit. Some researchers suspect that chemotherapy patients who do not have enough glutamine to start with are most likely to be helped.
- Surgery. Giving glutamine intravenously (by IV) along with intravenous nutrition seems to improve immune function and reduce complications related to infections after major surgery. Also, giving glutamine intravenously (by IV) along with intravenous nutrition after a bone marrow transplant seems to reduce the risk of infection and improve recovery compared to intravenous nutrition alone. However, not all people who undergo major surgery or who receive bone marrow transplants seem to benefit from glutamine.
Possibly Ineffective for 30:
- Athletic performance. Taking glutamine by mouth does not seem to improve athletic performance.
- Crohn’s disease. Taking glutamine by mouth does not seem to improve symptoms of Crohn’s disease.
- Inherited disease that causes stones in the kidneys or bladder (Cystinuria). Taking glutamine by mouth does not seem to improve an inherited condition that causes stones to form in the kidneys or bladder.
- Muscular dystrophy. Research shows that taking glutamine by mouth does not improve muscle strength in children with muscular dystrophy.
Insufficient Evidence for 30:
- Diarrhea caused by drugs used to treat HIV. Early research shows that taking glutamine by mouth reduces the severity of diarrhea in people with HIV who are taking the drug nelfinavir.
- Diarrhea caused by chemotherapy treatments. There is some evidence that glutamine might help to prevent diarrhea after chemotherapy, but not all research findings agree.
- Reducing damage to the immune system during cancer treatment. There is some evidence that glutamine reduces damage to the immune system caused by chemotherapy. However, not all research findings agree.
- Diarrhea. There are inconsistent findings about the effects of glutamine when used to treat diarrhea in children and infants. One early study suggests that taking glutamine by mouth reduces the duration of diarrhea in children. However, taking glutamine by mouth along with conventional rehydration solutions does not appear to have an advantage over rehydration solutions alone.
- Low birth weight. There are inconsistent findings about the effects of glutamine in infants with low to very low birth weight. Some research suggests that using glutamine in feeding tubes decreases infections in some low birth weight infants. However, most research suggests that it does not benefit low birth weight infants.
- Muscle and joint pains caused by the drug paclitaxel (Taxol, used to treat cancer). There is some evidence that glutamine might help to reduce muscle and joint pains caused by paclitaxel.
- Inflammation of the pancreas (pancreatitis). An early study shows that giving glutamine intravenously (by IV) along with intravenous nutrition improves immune function but does not reduce the risk for complications or the amount of time spent in the hospital in people with pancreatitis.
- Nutrition problems after major gut surgery (short bowel syndrome). Researchers have studied whether glutamine combined with growth hormone is effective in treating short bowel syndrome. This combination seems to help some patients become less dependent on tube feeding. However, glutamine alone does not seem to be effective.
- Depression.
- Moodiness.
- Irritability.
- Anxiety.
- Attention deficit-hyperactivity disorder (ADHD).
- Insomnia.
- Stomach ulcers.
- Ulcerative colitis.
- Sickle cell anemia.
- Treating alcoholism.
- Other conditions.
More evidence is needed to rate glutamine for these uses.
When to take L-glutamine supplement
L-glutamine comes as a powder to be mixed with a liquid or soft wet food and taken by mouth twice a day. Take L-glutamine at around the same times every day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take L-glutamine exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
You will need to mix the medication powder with 8 ounces (240 ml) of a liquid such as water, milk, or apple juice, or 4 to 6 ounces (120 to 180 ml) of a soft wet food such as applesauce or yogurt right before you take it. The liquid or food must be cold or room temperature. The powder does not need to be completely dissolved in the liquid or food before you take the mixture.
What special precautions should I follow when taking L-glutamine ?
Before taking L-glutamine:
- tell your doctor and pharmacist if you are allergic to L-glutamine, any other medications.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take. Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor if you are pregnant, plan to become pregnant, or are breastfeeding. If you become pregnant while taking L-glutamine, call your doctor.
What special dietary instructions should I follow when taking L-glutamine ?
Unless your doctor tells you otherwise, continue your normal diet.
What should I do if I forget a dose ?
Take the missed dose as soon as you remember it. However, if it is almost time for the next dose, skip the missed dose and continue your regular dosing schedule. Do not take a double dose to make up for a missed one.
L-glutamine dosage
Your doctor will tell you how much L-glutamine medicine to use. Take this medicine exactly as directed by your doctor. Do not take more of it, do not take it more often, and do not take it for a longer time than your doctor ordered.
For patients using the oral powder for solution:
- Mix a packet of this medicine with water just before using it.
- Take it with a meal or snack every 2 to 3 hours while you are awake. Be sure to drink all of the mixture.
- Do not use the medicine during the night unless your doctor tells you to.
For patients using the oral powder:
- Mix the oral powder with 4 to 6 ounces (oz) of food (eg, applesauce, yogurt) or 8 oz of cold or room temperature beverage (eg, water, milk, or apple juice).
- Complete dissolution of the mixture is not required.
- Be sure to drink or swallow all of the mixture.
Dosing
The dose of this medicine will be different for different patients. Follow your doctor’s orders or the directions on the label. The following information includes only the average doses of this medicine. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of medicine that you take depends on the strength of the medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine.
For oral dosage form (powder for oral solution):
For short bowel syndrome:
- Adults—30 grams (g) per day in divided doses (5 g taken 6 times a day) for up to 16 weeks. Taken with meals or snacks, 2 to 3 hours apart while awake. Be sure to drink all of the mixture. Do not use this medicine during the night unless your doctor tells you to.
- Children—Use and dose must be determined by your doctor.
For oral dosage form (oral powder):
For sickle cell disease:
- Adults and children 5 years of age and older and weighs greater than 65 kilograms (kg)—15 grams (g) per dose (3 packets per dose) 2 times a day or 30 g per day (6 packets per day).
- Adults and children 5 years of age and older and weighs 30 to 65 kg—10 g per dose (2 packets per dose) 2 times a day or 20 g per day (4 packets per day).
- Children 5 years of age and older and weighs less than 30 kg—5 g per dose (1 packet per dose) 2 times a day or 10 g per day (2 packets per day).
- Children younger than 5 years of age—Use and dose must be determined by your doctor.
- Mix the oral powder with 4 to 6 ounces (oz) of food (including apple sauce or yogurt) or with 8 oz of cold or room temperature beverage (including water, milk, or apple juice) as instructed by your doctor or pharmacist. Be sure to drink or swallow all of the mixture. Complete dissolution of the mixture is not required.
Missed dose: Take a dose as soon as you remember. If it is almost time for your next dose, wait until then and take a regular dose. Do not take extra medicine to make up for a missed dose.
Storage
Store the medicine in a closed container at room temperature, away from heat, moisture, and direct light. Keep from freezing.
Keep out of the reach of children.
Do not keep outdated medicine or medicine no longer needed.
Ask your healthcare professional how you should dispose of any medicine you do not use.
L-glutamine side effects and safety
Special Precautions & Warnings 31:
Children: Glutamine is POSSBILY SAFE when taken by mouth appropriately. Children aged 3 to 18 years should not be given doses that are larger than 0.7 grams per kg of weight daily. Not enough information is known about the safety of higher doses in children.
Pregnancy and breast-feeding: Not enough is known about the use of glutamine during pregnancy and breast-feeding. Stay on the safe side and avoid use.
Cirrhosis: Glutamine could make this condition worse. People with this condition should avoid glutamine supplements.
Severe liver disease with difficulty thinking or confusion (hepatic encephalopathy): Glutamine could make this condition worse. Do not use it.
Monosodium glutamate (MSG) sensitivity (also known as “Chinese restaurant syndrome”): If you are sensitive to MSG, you might also be sensitive to glutamine, because the body converts glutamine to glutamate.
Mania, a mental disorder: Glutamine might cause some mental changes in people with mania. Avoid use.
Seizures: There is some concern that glutamine might increase the likelihood of seizures in some people. Avoid use.
Drug Interactions
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. Tell your healthcare professional if you are taking any other prescription or nonprescription (over-the-counter [OTC]) medicine.
Other Interactions
Certain medicines should not be used at or around the time of eating food or eating certain types of food since interactions may occur. Using alcohol or tobacco with certain medicines may also cause interactions to occur. Discuss with your healthcare professional the use of your medicine with food, alcohol, or tobacco.
L-glutamine common side effects.
Tell your doctor if any of these symptoms are severe or do not go away:
- constipation
- nausea
- headache
- abdominal pain
- cough
- back, leg, feet, hands, or arm pain
L-glutamine may cause other side effects. See your doctor if you have any unusual problems while taking this medication.
Less common side effects
- Blood in urine
- changes in skin color
- chills
- cold hands and feet
- confusion
- cough
- difficulty swallowing
- dizziness
- fainting
- fast heartbeat
- fever
- frequent and painful urination
- headache
- hives, itching, skin rash
- light headedness
- lower back or side pain
- pain, redness, or swelling in the arm or leg
- puffiness or swelling of the eyelids or around the eyes, face, lips, or tongue
- rapid, shallow breathing
- stomach pain
- sudden decrease in amount of urine
- tightness in the chest
- unusual tiredness or weakness
- wheezing
Some side effects may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them.
Other Less common side effects
- Abnormal or decreased touch sensation
- back pain
- bacterial infection
- bleeding after defecation
- bleeding, blistering, burning, coldness, discoloration of skin, feeling of pressure, hives, infection, inflammation, itching, lumps, numbness, pain, rash, redness, scarring, soreness, stinging, swelling, tenderness, tingling, ulceration, or warmth at site
- bloated full feeling
- body aches or pain
- breast pain, female
- chest pain
- change in the color, amount, or odor of vaginal discharge
- congestion
- constipation
- Crohn’s disease, aggravated
- dark urine
- decreased urination
- diarrhea
- difficulty having a bowel movement (stool)
- difficulty in moving
- discoloration of fingernails or toenails
- discouragement
- dry mouth
- dryness or soreness of throat
- ear or hearing symptoms
- excess air or gas in stomach or intestines
- feeling sad or empty
- feeling unusually cold shivering
- flatulence
- full or bloated feeling
- general feeling of discomfort or illness
- increase in heart rate
- indigestion
- irritability
- joint pain;
- lack of appetite
- light-colored stools
- loss of appetite
- loss of interest or pleasure
- muscle aches and pains
- muscle pain or stiffness
- nausea
- pain in joints
- pain or burning while urinating
- pains in stomach, side, or abdomen, possibly radiating to the back
- passing gas
- pressure in the stomach
- rash
- rectal bleeding
- runny nose
- shivering
- sleeplessness
- sneezing
- sore throat
- stomach bloating, burning, cramping, or pain
- stuffy nose
- sunken eyes
- sweating
- swelling of abdominal or stomach area
- swelling of face
- swelling of hands, ankles, feet, or lower legs
- swollen joints
- tender, swollen glands in neck;
- thirst
- trouble concentrating
- trouble sleeping
- trouble in swallowing
- unable to sleep
- uncomfortable swelling around anus
- unpleasant breath odor
- unusual tiredness or weakness
- voice changes
- vomiting
- vomiting of blood
- weight loss
- wrinkled skin
- yellow eyes or skin
Other side effects not listed may also occur in some patients. If you notice any other effects, check with your healthcare professional.
Call your doctor for medical advice about side effects.
- L-glutamine. https://pubchem.ncbi.nlm.nih.gov/compound/L-glutamine[↩]
- Gaurav K, Goel RK, Shukla M, Pandey M. Glutamine: A novel approach to chemotherapy-induced toxicity. Indian Journal of Medical and Paediatric Oncology : Official Journal of Indian Society of Medical & Paediatric Oncology. 2012;33(1):13-20. doi:10.4103/0971-5851.96962. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3385273/[↩][↩]
- Intracellular free amino acid concentration in human muscle tissue. Bergström J, Fürst P, Norée LO, Vinnars E. J Appl Physiol. 1974 Jun; 36(6):693-7. https://www.ncbi.nlm.nih.gov/pubmed/4829908/[↩]
- Is glutamine a conditionally essential amino acid? Lacey JM, Wilmore DW. Nutr Rev. 1990 Aug; 48(8):297-309. https://www.ncbi.nlm.nih.gov/pubmed/2080048/[↩]
- L-glutamine. Medline Plus. https://medlineplus.gov/druginfo/meds/a617035.html[↩]
- Souba WW. Glutamine Physiology, Biochemistry, and Nutrition in Critical Illness. Austin, TX: R.G. Landes Co; 1992.[↩]
- Halperin HL, Kamel HS, Ethier JH. Biochemistry and physiology of ammonium excretion. In: Seldin DW, Giebisch L, editors. The kidney: Physiology and pathology. New York: Raven Press; 1992. pp. 2645–80[↩]
- Polyglutamine aggregates alter protein folding homeostasis in Caenorhabditis elegans. Satyal SH, Schmidt E, Kitagawa K, Sondheimer N, Lindquist S, Kramer JM, Morimoto RI. Proc Natl Acad Sci U S A. 2000 May 23; 97(11):5750-5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC18505/[↩]
- Bacterial and yeast chaperones reduce both aggregate formation and cell death in mammalian cell models of Huntington’s disease. Carmichael J, Chatellier J, Woolfson A, Milstein C, Fersht AR, Rubinsztein DC. Proc Natl Acad Sci U S A. 2000 Aug 15; 97(17):9701-5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC16928/[↩]
- Blomqvist BI, Hammarqvist F, von der Decken A, Wernerman J. Glutamine and alpha-ketoglutarate prevent the decrease in muscle free glutamine concentration and influence protein synthesis after total hip replacement. Metabolism. 1995;44:1215–22. https://www.ncbi.nlm.nih.gov/pubmed/7666798[↩]
- Planas M, Schwartz S, Arbós MA, Farriol M. Plasma glutamine levels in septic patients. J Parenter Enteral Nutr. 1993;17:299–300. https://www.ncbi.nlm.nih.gov/pubmed/8505843[↩]
- Wernerman J, Hammarkvist F, Ali MR, Vinnars E. Glutamine and ornithine-alpha-ketoglutarate but not branched-chain amino acids reduce the loss of muscle glutamine after surgical trauma. Metabolism. 1989;38:63–6. https://www.ncbi.nlm.nih.gov/pubmed/2503684[↩]
- Parry-Billings M, Evans J, Calder PC, Newsholme EA. Does glutamine contribute to immunosuppression after major burns? Lancet. 1990;336:523–5. https://www.ncbi.nlm.nih.gov/pubmed/1975037[↩]
- Ziegler TR. Glutamine and Acute Illness. Br J Nutr. 2002;87(Suppl 1):S9–15. https://www.ncbi.nlm.nih.gov/pubmed/11895159[↩]
- Thompson JS, Rochling FA, Weseman RA, Mercer DF. Current management of short bowel syndrome. Current Problems in Surgery. 2012;49(2):52–115.[↩][↩]
- Goringe AP, Brown S, O’Callaghan U, Rees J, Jebb S, Elia M, et al. Glutamine and vitamin E in the treatment of hepatic veno-occlusive disease following high-dose chemotherapy. Bone Marrow Transplant. 1998;22:2879–84. https://www.ncbi.nlm.nih.gov/pubmed/9603409[↩]
- Muscaritoli M, Grieco G, Capria S, Iori AP, Rossi Fanelli F. Nutritional and metabolic support in patients undergoing bone marrow transplantation. Am J Clin Nutr. 2002;75:183–90. http://ajcn.nutrition.org/content/75/2/183.long[↩]
- Miller AL. Therapeutic considerations of L-glutamine: A review of the literature. Alternat Med Rev. 1999;4:239–48. https://www.ncbi.nlm.nih.gov/pubmed/10468648[↩]
- Kang YJ, Feng Y, Hatcher EL. Glutathione stimulates A549 cell proliferation in glutamine-deficient culture: The effect of glutamine supplementation. J Cell Physiol. 1994;161:589–96. https://www.ncbi.nlm.nih.gov/pubmed/7962140[↩]
- Bartlett DL, Charland S, Torosian MH. Effect of glutamine on tumor and host growth. Ann Surg Oncol. 1995;2:71–6. https://www.ncbi.nlm.nih.gov/pubmed/7530589[↩]
- Van der Hulst RR, von Meyenfeldt MF, Deutz NE, Soeters PB. Glutamine extraction by the gut is reduced in depleted [corrected] patients with gastrointestinal cancer. Annals of Surgery. 1997;225(1):112-121. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1190613/[↩]
- Klimberg VS, Souba WW, Dolson DJ, Salloum RM, Hautamaki RD, Plumley DA, et al. Prophylactic glutamine protects the intestinal mucosa from radiation injury. Cancer. 1990;66:62–8. https://www.ncbi.nlm.nih.gov/pubmed/2354410[↩]
- Fox AD, Kripke SA, De Paula J, Berman JM, Settle RG, Rombeau JL. Effect of a glutamine-supplemented enteral diet on methotrexate-induced enterocolitis. JPEN J Parenter Enteral Nutr. 1988;12:325–31. https://www.ncbi.nlm.nih.gov/pubmed/3138440[↩]
- Klimberg VS, Souba WW, Salloum RM, Plumley DA, Cohen FS, Dolson DJ, et al. Glutamine-enriched diets support muscle glutamine metabolism without stimulating tumor growth. J Surg Res. 1990;48:319–23. https://www.ncbi.nlm.nih.gov/pubmed/2338817[↩]
- Smith CV, Mitchell JR. Pharmacological aspects of glutathione in drug metabolism. In: Dolphin D, Poulson R, Avramovic O, editors. Coenzymes and Cofactors. New York: John Wiley and Sons; 1989. pp. 1–44.[↩]
- Nirenberg A, Mosende C, Mehta BM, Gisolfi AL, Rosen G. High-dose methotrexate concentrations and corrective measures to avert toxicity. Cancer Treat Rep. 1977;61:779–83. https://www.ncbi.nlm.nih.gov/pubmed/302143[↩]
- Jensen JC, Nwokedi E, Baker ML, Bevans DW, 3rd, Baker ML, Pappas AA, et al. Prevention of chronic radiation enteropathy by dietary glutamine. Ann Surg Oncol. 1994;1:157–63. https://www.ncbi.nlm.nih.gov/pubmed/7834441[↩]
- Rouse K, Nwokedi E, Woodliff JE, Epstein J, Klimberg VS. Glutamine enhances selectivity of chemotherapy through changes in glutathione metabolism. Annals of Surgery. 1995;221(4):420-426. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1234593/[↩]
- Scheid C, Hermann K, Kremer G, Holsing A, Heck G, Fuchs M, et al. Randomized, double-blind, controlled study of glycyl-glutamine-dipeptide in the parenteral nutrition of patients with acute leukemia undergoing intensive chemotherapy. Nutrition. 2004;20:249–54. https://www.ncbi.nlm.nih.gov/pubmed/14990264[↩]
- GLUTAMINE. https://www.webmd.com/vitamins-supplements/ingredientmono-878-glutamine.aspx?activeingredientid=878[↩][↩]
- Glutamine (Oral route). https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0046028/[↩]