How to detect ovulation
Ovulation occurs each month when an egg is released from one of your ovaries. Occasionally, more than one egg is released, usually within 24 hours of the first egg. Ovulation usually happens at around the same time each month.
Ovulation occurs though a sequence of hormonal responses. Located deep within your brain, the pituitary gland releases the follicle-stimulating hormone (FSH) and luteinizing hormone (LH), which travel through your blood stream to your ovaries. These hormones signal the development and release a single egg cell from one of your ovaries. The sweeping motion of the fimbriae draws the egg cell through a very small space in the open body cavity into the uterine tube or fallopian, tube. The egg may be fertilized here if there is sperm in the fallopian tube. At the same time, the lining of your womb begins to thicken for the egg to be implanted in it after it has been fertilized and the mucus in your cervix becomes thinner, so that sperm can swim through it more easily. An unfertilized egg may live for up to 12 hours. If your egg is not fertilized, it passes out of your body during the your monthly period, along with the lining of your womb. The egg is so small that it cannot be seen.
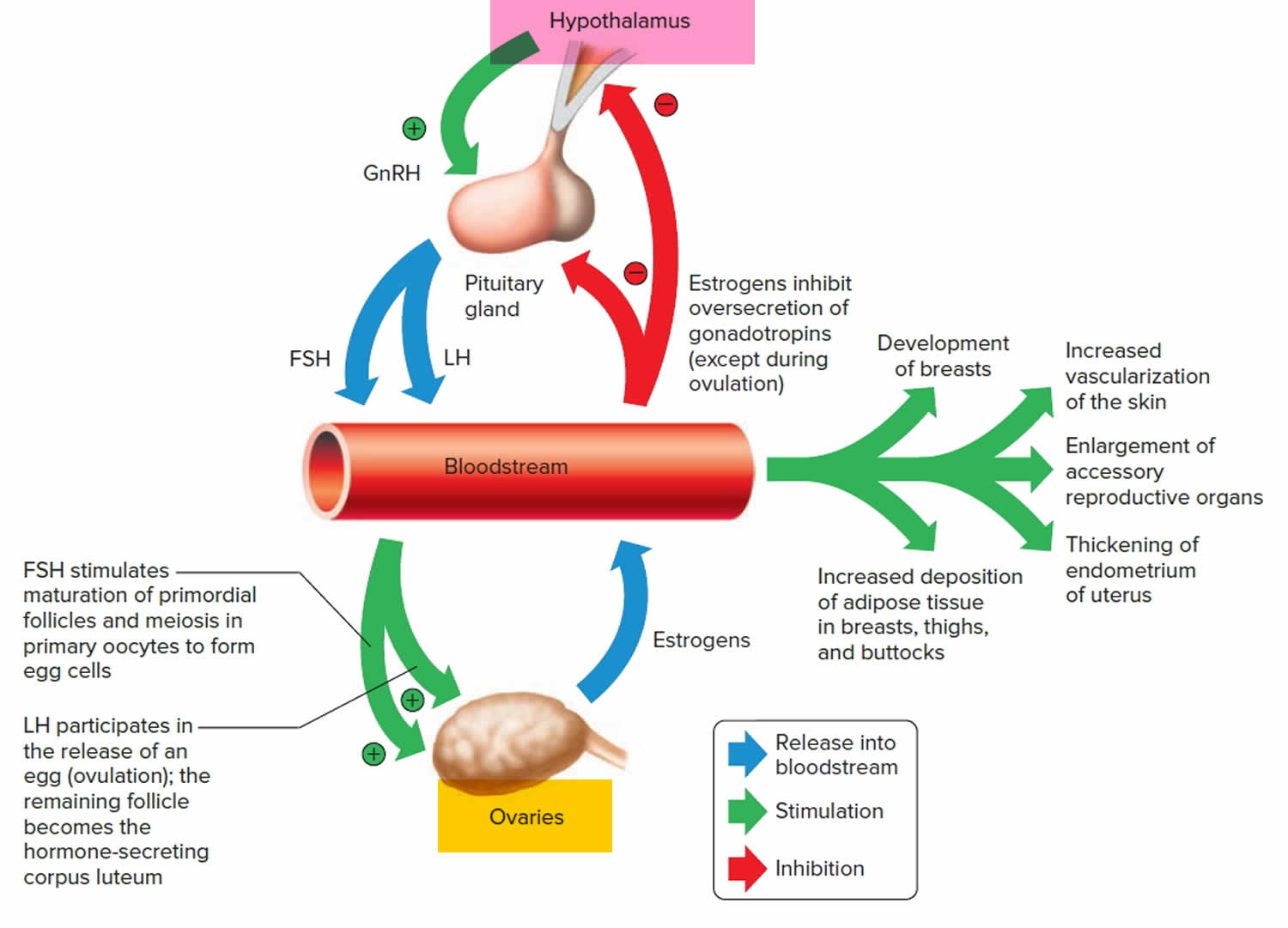
Ovulation depends on the activity of various glands and their hormones, including:
- Hypothalamus – located within the brain. The hypothalamus uses hormones to communicate with the pituitary
- Pituitary gland – known as the ‘master gland’ of the hormone (endocrine) system. It is located within the brain, at the base of the skull, and is connected to the hypothalamus by a thin stalk. The pituitary uses chemicals to prompt the ovaries to produce their hormones
- Ovaries – the two almond-shaped glands located within a woman’s pelvis that contain the ova. The ovaries make the two female sex hormones estrogen and progesterone.
Common causes of ovulatory problems include:
- Hypothalamus – conditions that can alter the functioning of the hypothalamus include polycystic ovary syndrome (PCOS), overexercising, poor nutrition and chronic stress
- Pituitary gland – conditions that can prevent the pituitary gland from producing enough hormones include benign pituitary tumors or direct injury to the pituitary itself
- Ovaries – conditions that can prevent the ovaries from releasing ova include early menopause (also known as ovarian failure), or damage to or removal of the ovaries.
If you want to find out when you ovulate, there are a number of things you can use:
- The length of your menstrual cycle – A menstrual cycle is counted from the first day of one period to the first day of the next period. Some women have shorter and some have longer cycles and timing of ovulation depends on the length of the cycle. A normal menstrual cycle is between 28 to 32 days. The day a woman starts her period is considered to be cycle day 1. Ovulation often occurs around day 14 of your cycle (ovulation usually occurs around 10 to 16 days before your period starts), so you may be able to work out when you’re likely to ovulate if you have a regular menstrual cycle. If on average you have a period every 28 days you ovulate around day 14 and your best chance of conceiving is between days 11 and 14. But if you have a shorter interval between periods, say 24 days, ovulation happens around day 10 and your ‘fertile window’ is between days 7 and 10 (see Figure 6 below). If on the other hand you have 35 days between periods, you should focus your baby making efforts between days 18 and 21.
- One way to calculate your estimated time of ovulation is as follows:
- Work out the length of your average menstrual cycle. Day one is the first day of the menstrual period and the last day is the day before your next period begins. Let’s say your menstrual cycle is 28 days long.
- Subtract 17 days. In our example, 28 days minus 17 days equals day 11.
- Use the ovulation predictor kit on day 11. Continue testing daily until the test comes back positive. A positive result means you are going to ovulate within the next 24 to 36 hours.
- Having sex around the time of ovulation means that the sperm and ovum have a good chance of meeting in the fallopian tube.
- One way to calculate your estimated time of ovulation is as follows:
- Changes in your cervical mucus (mucus method) – During ovulation, your cervical mucus is stretchy, clear, and slick. You may notice wetter, clearer and more slippery mucus around the time of ovulation. It looks and feels like an uncooked egg white.
- Changes in your body temperature (symptothermal method) – there’s a small rise in your body temperature after ovulation takes place, which you may be able to detect with a thermometer. You can take your body temperature in your mouth, vagina, or rectum. A regular basal body temperature is between 97°F and 98°F (36.1° C to 36.7° C). At the time of ovulation, your basal body temperature will rise between 0.5 and 1 degree. You should take your basal body temperature in the morning before you have moved or get out of bed. Ideally, it should be the same time of day. You should use the thermometer the same way each day to get accurate results.
- Ovulation predictor kits – hormone levels increase around the time of ovulation and this can be detected using ovulation predictor kits also known as luteinizing hormone urine test (LH urine test) that measure the level of luteinizing hormone (LH) in your urine
Using a combination of these methods is likely to be most accurate. In all 4 methods, you must use a calendar or chart to track the data and changes. This predicts when you ovulate, so you can partake in (or abstain from sex). You may notice other symptoms you can track. These include bloating, backache, tender breasts, or pain in your ovaries.
Some women may experience other symptoms when they’re ovulating, including breast tenderness, bloating and mild one-sided pain in their lower abdomen, but these are not a reliable way of predicting ovulation.
Ovulation pain also called mittelschmerz (German for “middle pain” or “pain in the middle of the month”) happens about 14 days before your period, when your ovary releases an egg as part of your menstrual cycle.
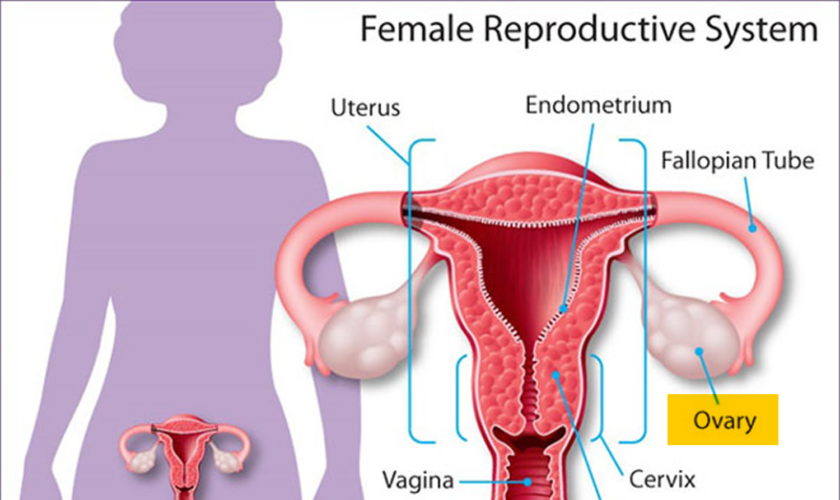
Figure 1. Female reproductive organs
Menstrual cycle
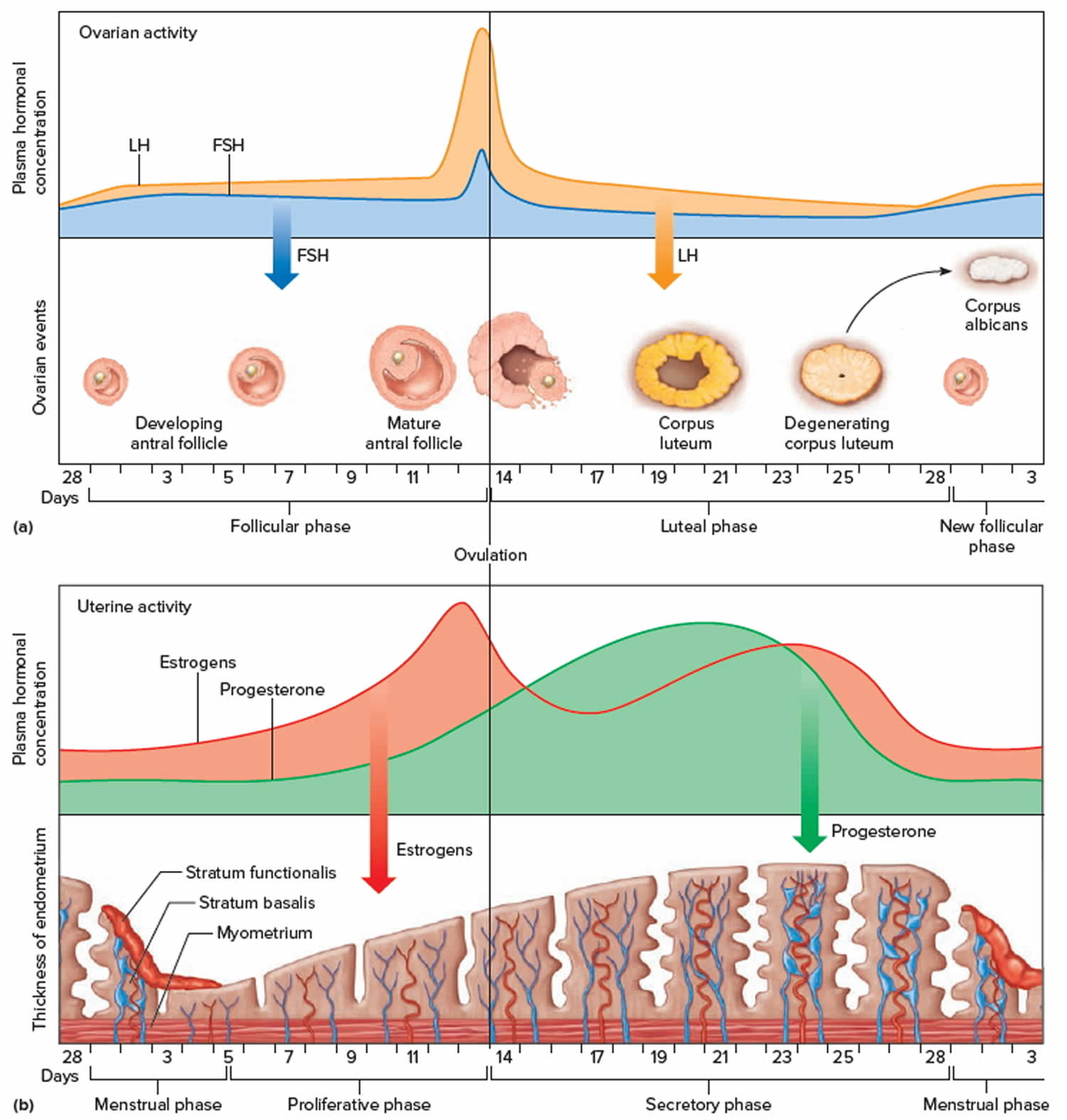
Ovulation is part of the menstrual cycle. This cycle is caused by the complex and interrelated activity of various hormones. The cycle includes:
- Menstruation – the shedding of the uterine lining (also known as menstrual bleeding or having your period)
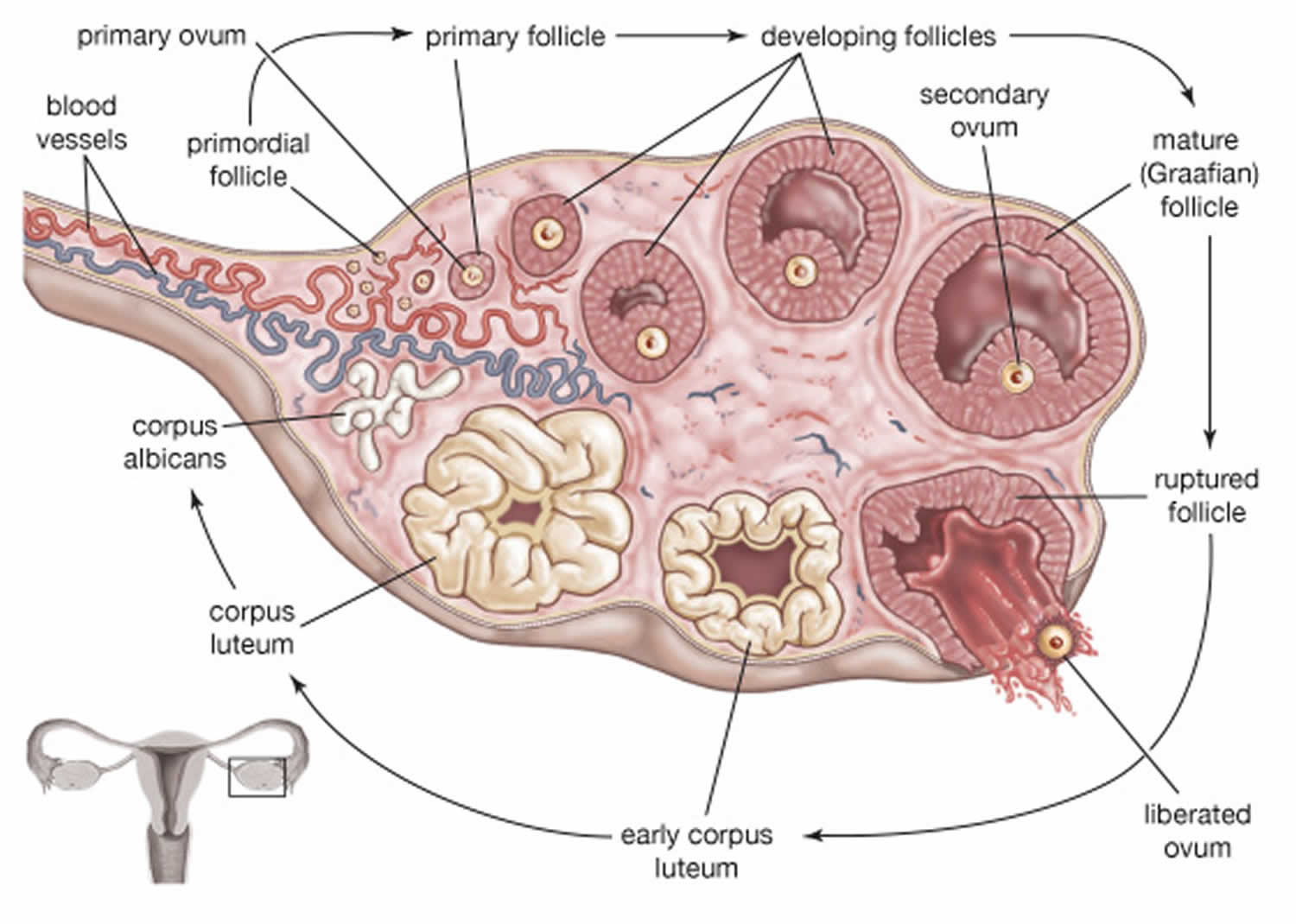
- Follicular phase – the hypothalamus triggers the pituitary gland to release follicle stimulating hormone (FSH), which prompts the ovaries to produce up to 20 follicles. Each follicle contains an immature ovum. Usually, only one follicle survives to maturity. Assuming the menstrual cycle is around 28 days long, a single ovum matures at about day 10. This event also prompts the thickening of the uterine lining (endometrium) in preparation for a fertilised ovum
- Ovulation – the maturing follicle prompts the release of higher amounts of oestrogen. The hypothalamus responds by secreting a chemical known as gonadotrophin-releasing hormone (GnRH), which makes the pituitary produce luteinizing hormone (LH) and follicle stimulating hormone (FSH). High levels of LH trigger ovulation within about two days. The mature follicle releases the ovum into the peritoneal cavity; it is then drawn into the open end of the fallopian tube. Small hair-like structures within the fallopian tube wave or ‘massage’ the ovum towards the uterus. Unless the ovum encounters a sperm within 24 hours, it will die
- Luteal phase – the follicle becomes the corpus luteum, a structure that makes the hormone progesterone. Unless a fertilised ovum implants into the uterine lining, the corpus luteum dies. Without its contribution of progesterone, the uterus can’t maintain the thickened uterine lining, and menstruation occurs.
Figure 2. Menstrual cycle
Figure 3. Pituitary gland hormones under the influence of the hypothalamus controlling the ovaries production of egg cell, ovulation and development of the female secondary sex characteristics
Abbreviations: GnRH = Gonadotropin-Releasing Hormone; FSH = Follicle-Stimulating Hormone; LH= Luteinizing Hormone
Figure 4. Ovarian Follicle Maturation
Figure 5. Ovarian activity during the Menstrual cycle
Footnote: Major events in the female menstrual cycle. (a) Plasma hormonal concentrations of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) affect follicle maturation in the ovaries. (b) Plasma hormonal concentrations of estrogen and progesterone influence changes in the uterine lining.
Abbreviations: FSH = Follicle-Stimulating Hormone; LH= Luteinizing Hormone
How does ovulation relate to my periods?
Ovulation is the release of an egg from one of your ovaries. The same hormones that cause the uterus lining to build up also cause an egg to leave one of the ovaries. The egg travels through a thin tube called a fallopian tube to the uterus.
If the egg is fertilized by a sperm cell, it attaches to the wall of the uterus, where over time it develops into a baby. If the egg is not fertilized, the uterus lining breaks down and bleeds, causing a period.
When am I are most fertile?
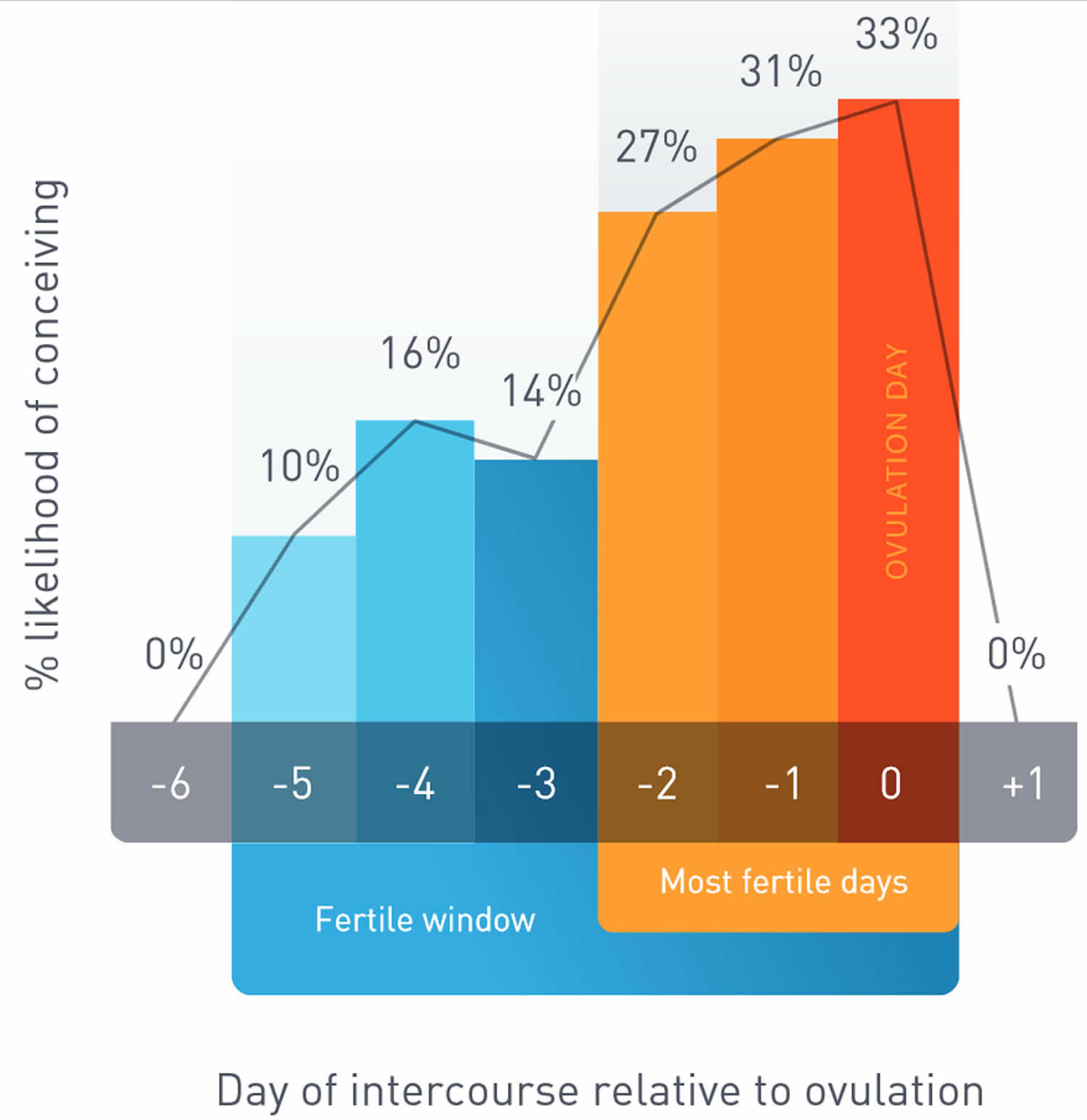
The five days before ovulation, together with the day you ovulate, are the days when you are most likely to conceive. Sperm can live up to five days inside your body, so if you have sex up to five days before your egg is released, you can get pregnant. After ovulation, though, your egg can only live for 12 to 24 hours. After this time is up, your time for getting pregnant has gone for now till the following month.
Your chances of getting pregnant are at their highest in the three days leading up to and including ovulation.
Do periods happen regularly when my menstruation starts?
For the first few years after a girl starts her period, it may not come regularly. This is normal at first. By about 2–3 years after her first period, a girl’s periods should be coming around once every 4–5 weeks.
Can a girl get pregnant as soon as her period starts?
Yes, a girl can get pregnant as soon as her period starts. A girl can even get pregnant right before her very first period. This is because a girl’s hormones might already be active. The hormones may have led to ovulation and the building of the uterine wall. If a girl has sex, she can get pregnant, even though she has never had a period.
How to detect fertile days
Knowing when ovulation happens is critical when you want to get pregnant because the window of opportunity to conceive is fairly small every month. As shown in the graph below (Figure 6), conception is only possible from about five days before ovulation through to the day of ovulation. These six days are the “fertile window” in a woman’s cycle and reflect the lifespan of sperm (five days) and the lifespan of the egg (24 hours). But the likelihood of conceiving is dramatically increased if sex occurs in the three days leading up to and including ovulation. If a woman has sex six or more days before she ovulates, the chance she will get pregnant is virtually zero. Then, the probability of pregnancy rises steadily and is 27-33% in the three days leading up to and including ovulation. From that point, the probability of pregnancy declines rapidly. Twelve to 24 hours after ovulation, a woman is no longer able to get pregnant during that cycle.
If all this seems too complicated, an alternative is to have sex every two to three days. That way all bases are covered without getting too technical about when the chance of conceiving is greatest.
Figure 6. Fertile window
Signs and symptoms of ovulation
The female body shows several signs of ovulation. You may experience some or all of these signs, including:
- regular menstrual cycles – menstrual periods that arrive every 24–35 days are more likely to be ovulatory than periods that occur more or less often
- mucus changes – about two weeks before menstruation, if you are ovulating you may notice slick and slippery cervical mucus
- abdominal pain – some women experience pain during ovulation. The pain may be general or localised to one side of the abdomen
- premenstrual symptoms – ovulation may accompany premenstrual symptoms such as breast enlargement and tenderness, abdominal bloating and moodiness
- temperature rise – women who use a natural family planning method of contraception will notice a small rise in their basal temperature after ovulation has occurred. The temperature rise is about half a degree Fahrenheit (Celsius). This temperature rise does not predict ovulation – it suggests that ovulation has already taken place.
How to detect ovulation at home
There are many different kinds of ovulation predictor kits on the market. Most work by measuring the level of luteinizing hormone (LH) in your urine (LH urine test). Luteinizing hormone (LH) levels rise about 24 to 36 hours before ovulation takes place.
An ovulation home test also known as luteinizing hormone urine test (LH urine test) is used by some women to detect ovulation. The LH urine test involves normal urination. There is no pain or discomfort. Ovulation home test helps you to determine the time in your menstrual cycle when getting pregnant is most likely. This at-home ovulation test is often used by women to help predict when an egg release is likely. This is when pregnancy is most likely to occur. These kits can be bought at most drug stores.
The ovulation test detects a rise in luteinizing hormone (LH) in the urine. A rise in this hormone signals the ovary to release the egg. A positive result indicates an “LH surge.” This is a sign that ovulation may soon occur. Talk to your doctor if you are unable to detect an “LH surge” or do not become pregnant after using the kit for several months. You may need to see an infertility specialist.
Luteinizing hormone (LH) urine tests are not the same as the home fertility monitors. Fertility monitors are digital handheld devices. They predict ovulation based on electrolyte levels in your saliva, luteinizing hormone (LH) levels in your urine or your basal body temperature. These devices can store ovulation information for several menstrual cycles.
How the ovulation test is performed
Ovulation prediction test kits most often come with five to seven sticks. You may need to test for several days to detect a surge in luteinizing hormone (LH).
The specific time of month that you start testing depends on the length of your menstrual cycle. For example, if your normal cycle is 28 days, you’ll need to begin testing on day 11. That is, the 11th day after you started your period. If you have a different cycle interval than 28 days, talk to your doctor about the timing of the test. In general, you should begin testing 3 to 5 days prior to the expected date of ovulation.
You will need to urinate on the test stick, or place the stick into urine that has been collected into a sterile container. The test stick will turn a certain color or display a positive sign if a surge is detected.
A positive result means you should ovulate in the next 24 to 36 hours, but this may not be the case for all women. The booklet that is included in the kit will tell you how to read the results.
You may miss your surge if you miss a day of testing. You may also not be able to detect a surge if you have an irregular menstrual cycle.
How to prepare for the ovulation test
DO NOT drink large amounts of fluids before using the test.
Drugs that can decrease luteinizing hormone (LH) levels include estrogens, progesterone, and testosterone. Estrogens and progesterone may be found in birth control pills and hormone replacement therapy.
The drug clomiphene citrate (Clomid) can increase luteinizing hormone (LH) levels. This drug is used to help trigger ovulation.
Why the ovulation test is performed?
The ovulation test is most often done to determine when a woman will ovulate to assist in difficulty in getting pregnant. For women with a 28-day menstrual cycle, this release normally occurs between days 11 and 14.
If you have an irregular menstrual cycle, the kit can help you tell when you are ovulating.
The ovulation home test may also be used to help you adjust doses of certain medicines such as infertility drugs.
Medical tests for ovulation
Medical tests can check whether or not ovulation took place. These tests can include:
- blood test – to check for the presence of progesterone. A level greater than 20 nmol/L indicates that ovulation took place. This test must be taken about three to 10 days before the first day of the next expected period
- pregnancy ultrasound – the presence of a fetus is the only absolute proof that ovulation took place. Medical tests such as ovulation predictor kits and blood tests can only ascertain that ovulation probably – not definitely – occurred.
How to increase your chances of ovulation
Ways to increase your chances of ovulation include:
- Women who are seriously obese or underweight may have problems with ovulation. Try to keep your weight around the average for your height and build.
- Excessive exercise can prevent ovulation. Ease back on your physical activity levels – this may require expert help if your desire to exercise is actually a form of bulimia.
- Repeated crash dieting, fasting, skipping meals and other disordered eating habits can hamper your body’s ability to regularly ovulate. Make sure to eat properly and regularly. Once again, you may need expert help if these habits are associated with an eating disorder such as anorexia or bulimia nervosa.
- Chronic emotional stress can play havoc with your menstrual cycle. Try to reduce the amount of stress in your life, and learn ways to better cope with stress. For example, relaxation training may be helpful.
Some women who aren’t ovulating regularly can be helped by reproductive technologies including tablets and injections to trigger higher production of ovulatory hormones. The dosage needs to be carefully monitored, because ovulation induction can trigger the maturation of a number of ova, which could lead to a multiple pregnancy.
The best time to get pregnant
You’re most likely to get pregnant if you have sex within a day or so of ovulation (releasing an egg from the ovary). This is usually about 14 days after the first day of your last period, if your cycle is around 28 days long. An egg lives for about 12-24 hours after being released. For pregnancy to happen, the egg must be fertilized by a sperm within this time. Sperm can live for up to 7 days inside a woman’s body. So if you’ve had sex in the days before ovulation, the sperm will have had time to travel up the fallopian tubes to “wait” for the egg to be released. When the egg and sperm meet, it’s called fertilization. The fertilized egg also called an embryo moves through your fallopian tubes and attaches to the wall of your uterus where it grows and develops into a baby. When the embryo attaches to the uterus, it’s called implantation.
It’s difficult to know exactly when ovulation happens, unless you are practising natural family planning, or fertility awareness.
If you want to get pregnant, having sex every 2 to 3 days throughout the month will give you the best chance.
You don’t need to time having sex only around ovulation.
To get pregnant:
- A woman’s body must release an egg from one of her ovaries (ovulation).
- A man’s sperm must join with the egg along the way (fertilize).
- The fertilized egg must go through a fallopian tube toward the uterus (womb).
- The fertilized egg must attach to the inside of the uterus (implantation).
- Infertility may result from a problem with any or several of these steps.
- If you want to get pregnant, having sex every 2 to 3 days throughout the month will give you the best chance. You don’t need to time having sex only around ovulation.
Getting pregnant (conception) happens when a man’s sperm fertilizes a woman’s egg. For some women this happens quickly, but for others it can take longer.
You can get pregnant if you have unprotected sex any time from 5 days before and the day of ovulation. The more often you have sex during this time, the more likely you are to get pregnant. Your egg is fertile (can become an embryo) for 12 to 24 hours after ovulation. Your partner’s sperm can live inside you for up to 72 hours after you have sex.
However, it’s difficult to know exactly when your ovulation happen, unless you are practising natural family planning, or fertility awareness.
Out of every 100 couples trying for a baby, 80 to 90 will get pregnant within 1 year. The rest will take longer, or may need help to conceive.
To understand getting pregnant (conception) and pregnancy, it helps to know about the male and female sexual organs, and to understand how a woman’s monthly menstrual cycle and periods work.
The menstrual cycle is counted from the first day of a woman’s period (day 1). Some time after her period she will ovulate, and then around 12-16 days after this she’ll have her next period.
The average menstrual cycle lasts 28 days. But normal cycles can vary from 21 to 35 days. The amount of time before ovulation occurs is different in every woman and even can be different from month to month in the same woman, varying from 13 to 20 days long. Learning about this part of the cycle is important because it is when ovulation and pregnancy can occur. After ovulation, every woman (unless she has a health problem that affects her periods or becomes pregnant) will have a period within 14 to 16 days.
Being aware of your menstrual cycle and the changes in your body that happen during this time can help you know when you are most likely to get pregnant. See how the menstrual cycle works by watching the video below. Each month your ovaries release an egg about 14 days before the first day of your period. This is called ovulation. When you and your partner have unprotected sex around the time of ovulation, his sperm swim to meet your egg. Unprotected sex means you don’t use any kind of birth control to help prevent pregnancy.
Trouble getting pregnant
Trouble getting pregnant, difficulty conceiving is also known as infertility, which is usually defined as not being able to get pregnant after 12 months of unprotected sexual intercourse. A broader view of infertility includes not being able to carry a pregnancy to term. Finding out that you or your partner are unable to fall pregnant can be upsetting and difficult to deal with.
Because fertility in women is known to decline steadily with age, some health providers evaluate and treat women aged 35 years or older after just 6 months of unprotected sex. Women with infertility should consider making an appointment with a reproductive endocrinologist—a doctor who specializes in managing infertility. Reproductive endocrinologists may also be able to help women with recurrent pregnancy loss, defined as having two or more spontaneous miscarriages.
Pregnancy is the result of a process that has many steps.
To get pregnant:
- A woman’s body must release an egg from one of her ovaries (ovulation).
- A man’s sperm must join with the egg along the way (fertilize).
- The fertilized egg must go through a fallopian tube toward the uterus (womb).
- The fertilized egg must attach to the inside of the uterus (implantation).
Infertility may result from a problem with any or several of these steps.
Impaired fecundity (the ability to produce new offspring or fertility) is a condition related to infertility and refers to women who have difficulty getting pregnant or carrying a pregnancy to term.
- About 6% of married women aged 15 to 44 years in the United States are unable to get pregnant after one year of trying (infertility). Also, about 12% of women aged 15 to 44 years in the United States have difficulty getting pregnant or carrying a pregnancy to term, regardless of marital status (impaired fecundity).
- Infertility is not always a woman’s problem. Both men and women can contribute to infertility. Many couples struggle with infertility and seek help to become pregnant, but it is often thought of as only a woman’s condition. However, in about 35% of couples with infertility, a male factor is identified along with a female factor. In about 8% of couples with infertility, a male factor is the only identifiable cause.
- Almost 9% of men aged 25 to 44 years in the United States reported that they or their partner saw a doctor for advice, testing, or treatment for infertility during their lifetime.
For couples trying for a baby, it is normal to have feelings of uncertainty, disappointment and anxiety. It may affect a couple the same way or in different ways.
It is good to talk through any problems, and have both of you talk about how you feel.
If there are difficulties between you, talk to your doctor as a couple. Your doctor may refer you both to a counsellor if necessary.
There are many causes of infertility. For about 4 couples in 10 it will relate to a sperm problem. In another 4 couples in 10 there will be a female reproductive cause. Sometimes there is a combination of factors.
Infertility in women, your fertility may depend on:
- your age
- if you have any problems with your fallopian tubes
- if you have endometriosis or an ovulation problem
- any uterine fibroids
- pelvic inflammatory disease or sexually transmitted infections (STI).
Infertility in men may be affected by:
- problems with the tubes connected to the testes
- low sperm production
- high numbers of abnormal sperm
- genetic problems
- problems with sperm DNA.
Treatment for infertility is available and can bring hope to people wanting to have a baby, but it also has financial, physical and emotional costs. And success is not guaranteed.
Most experts suggest at least one year for women younger than age 35. However, for women aged 35 years or older, couples should see a health care provider after 6 months of trying unsuccessfully. A woman’s chances of having a baby decrease rapidly every year after the age of 30.
If you’re older than 40, your doctor may want to begin testing or treatment right away.
Your doctor may also want to begin testing or treatment right away if you or your partner has known fertility problems, or if you have a history of irregular or painful periods, pelvic inflammatory disease, repeated miscarriages, prior cancer treatment, or endometriosis.
Some health problems also increase the risk of infertility. So, couples with the following signs or symptoms should not delay seeing their health care provider when they are trying to become pregnant:
- Irregular periods or no menstrual periods.
- Very painful periods.
- Endometriosis.
- Pelvic inflammatory disease.
- You’ve had multiple miscarriages.
- You have known fertility problems.
- You’ve been diagnosed with endometriosis.
- You’ve undergone treatment for cancer
- Suspected male factor (i.e., history of testicular trauma, hernia surgery, chemotherapy, or infertility with another partner).
It is a good idea for any woman and her partner to talk to a health care provider before trying to get pregnant. They can help you get your body ready for a healthy baby, and can also answer questions on fertility and give tips on conceiving.