What is autonomic dysreflexia
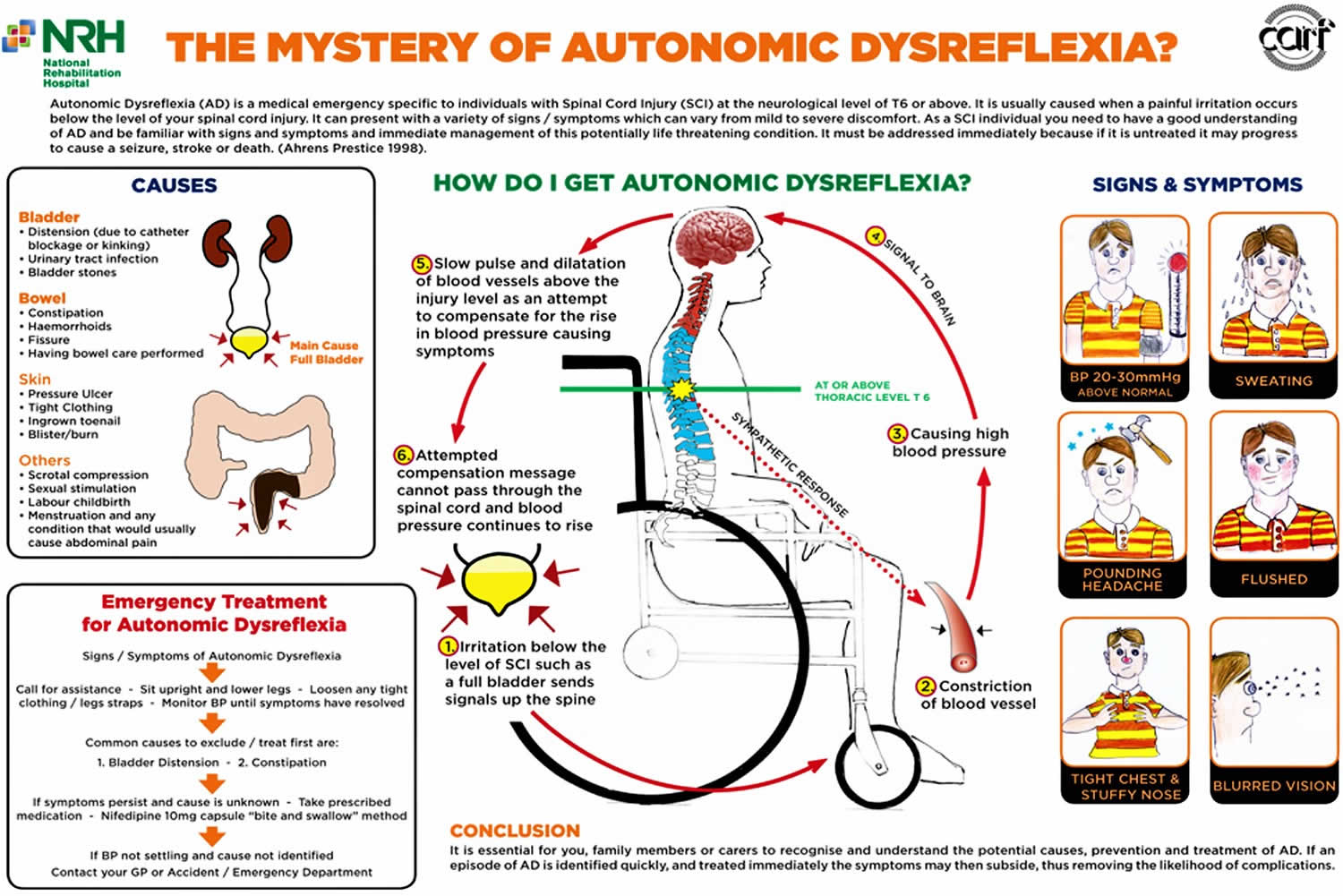
Autonomic dysreflexia is an abnormal, overreaction of the involuntary (autonomic) nervous system to stimulation that most often emerges after a spinal cord injury, usually when the injury has occurred above the T6 level 1. Autonomic dysreflexia develops in 20% to 70% of patients with spinal cord injury above the T6 level and is unlikely to develop if the injury is below T10. The higher the level of the spinal cord injury, the greater the risk with up to 90% of patients with cervical spinal or high-thoracic spinal cord injury being susceptible 1. Dysregulation of the autonomic nervous system leads to an uncoordinated autonomic response that may result in a potentially life-threatening hypertensive episode when there is a noxious stimulus below the level of the spinal cord injury. In about 85% of cases, this stimulus is from a urological source such as a urinary tract infection (UTI), a distended bladder, or a clogged Foley catheter. There is a significantly increased risk of stroke by 300% to 400% 1. Autonomic dysreflexia can occur in susceptible individuals up to 40 times per day. The initial presenting complaint is usually a headache which can be severe. Susceptible individuals with spinal cord lesions above T6 who complain of a headache should immediately have their blood pressure checked. If elevated, a presumptive diagnosis of autonomic dysreflexia can be made. Prompt recognition and correction of the disorder, usually just by irrigating or changing the Foley catheter, can be life-saving. Although approximately 90% of individuals with complete tetraplegia experience autonomic dysreflexia 2, there remains no effective permanent treatment for this disorder, partly due to limited understanding of its pathophysiology.
Women with spinal cord injury who become pregnant are at risk for developing a dysreflexia episode during labor and delivery. In women with spinal cord injury, the symptoms of labor may only be some abdominal discomfort, increased spasticity, and autonomic dysreflexia. Epidural anesthesia has been reported to be the superior choice for control of autonomic dysreflexia during labor. For cesarean delivery or instrumentally assisted delivery, a spinal or epidural may be used. The American College of Obstetrics and Gynecology states that it is vital that any obstetrician caring for a patient with spinal cord injury be familiar with the complications related to such injuries.
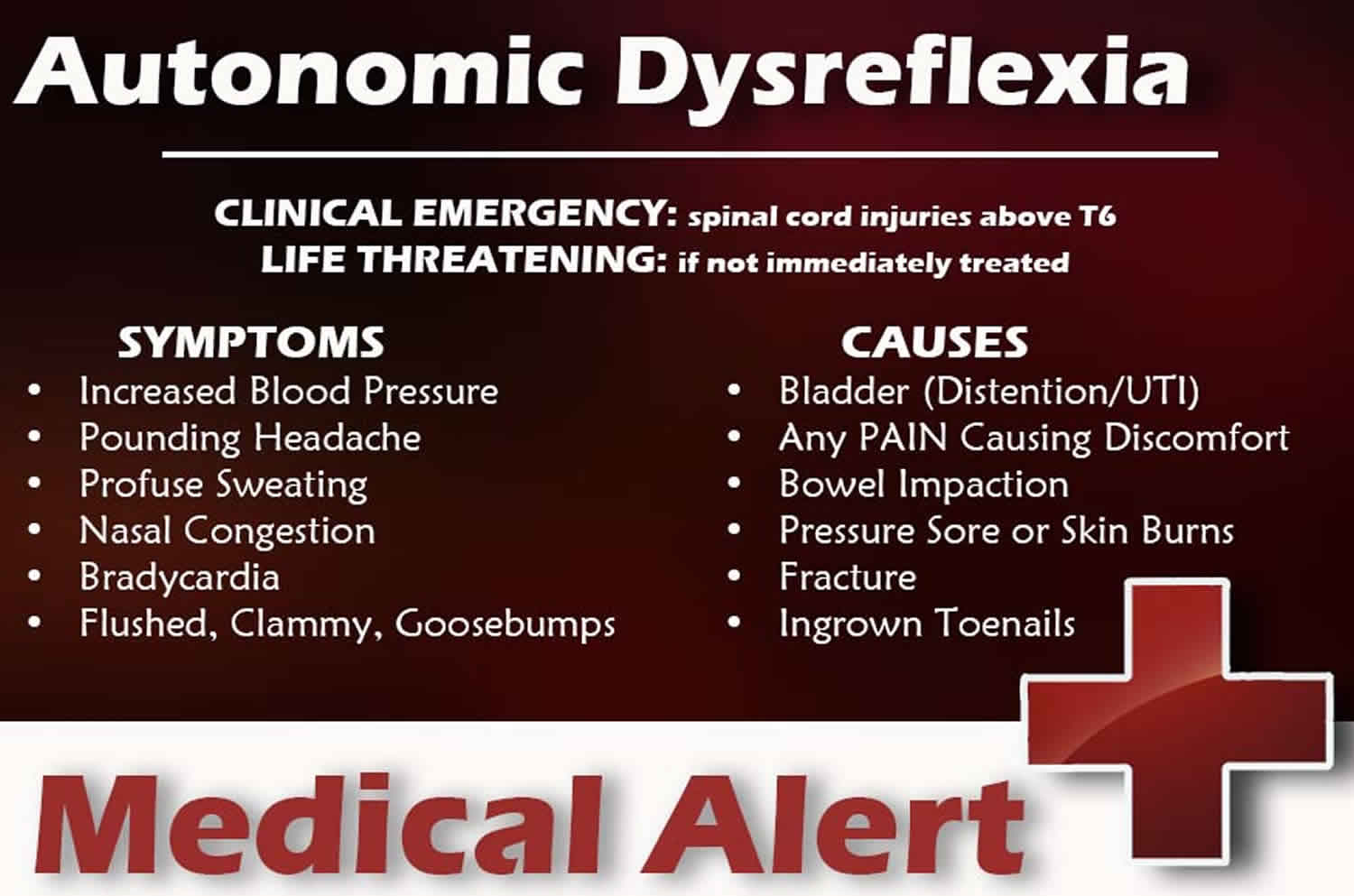
Autonomic dysreflexia reaction may include:
- Change in heart rate
- Excessive sweating
- High blood pressure
- Muscle spasms
- Skin color changes (paleness, redness, blue-gray skin color)
Autonomic dysreflexia is a medical emergency and can be life threatening 3. Autonomic dysreflexia is the only cardiovascular condition to directly cause death or irrevocable damage to individuals with spinal cord injury 4. Autonomic dysreflexia has been linked with cardiovascular events such as myocardial ischemia and fatal cerebral hemorrhage 5. Unstable control of blood pressure (including autonomic dysreflexia), endothelial dysfunction, glucose intolerance and metabolic syndrome are the major contributors to early cardiovascular-related complications and death in people with spinal cord injury 6.
Guidelines of the Consortium for Spinal Cord Medicine recommend several steps to manage autonomic dysreflexia 7:
- First, sit the patient upright to induce the orthostatic hypotension response.
- Second, loosen or remove any restrictive clothing and monitor the patient’s heart rate and blood pressure at five-minute intervals.
- Third, perform a survey of the possible causes of autonomic dysreflexia, starting with bladder distension.
- Lastly, if the patient’s systolic blood pressure remains above 150 mm Hg, administer a short- and fast-acting antihypertensive agent, such as nifedipine or captopril.
Autonomic dysreflexia occurs to some extent in up to 90% of people with upper thoracic (above the neurologic level of T6) and cervical spinal cord injury 3. Although autonomic dysreflexia can be asymptomatic, the signs and symptoms of autonomic dysreflexia generally include a sudden increase in blood pressure, altered heart rate (reflex bradycardia), anxiety, blurred vision, headache, flushing and sweating (above the level of injury) 3. Because people with upper thoracic and cervical injuries often have a low resting blood pressure (90–100 mm Hg), elevated blood pressure from autonomic dysreflexia may not always be obvious.
- Dysreflexia is related to the interruption of descending inhibition and the development of hyperresponsiveness of peripheral receptors.
- Bradycardia (low heart rate) resulting from a hypertensive crisis is due to activation of baroreceptors and a vagal-mediated response above the lesion to compensate for the hypertensive crisis.
Autonomic dysreflexia is triggered by stimuli from below the level of spinal cord injury 3. Autonomic dysreflexia can occur on a daily basis and can be triggered by stimuli such as distension of the bladder (most common), bladder or kidney stones, a kink in a urinary catheter, infection of the urinary tract, fecal impaction, pressure sores, an ingrown toenail, fractures, menstruation, hemorrhoids, invasive testing and sexual intercourse 8. Even benign stimuli, such as a shoelace that is tied too tightly or a sunburn can trigger autonomic dysreflexia. Autonomic dysreflexia usually resolves as soon as the precipitating stimuli are eliminated (e.g., bladder voided or colon emptied). In some cases, autonomic dysreflexia episodes do not resolve simply with removal of the stimulus 9.
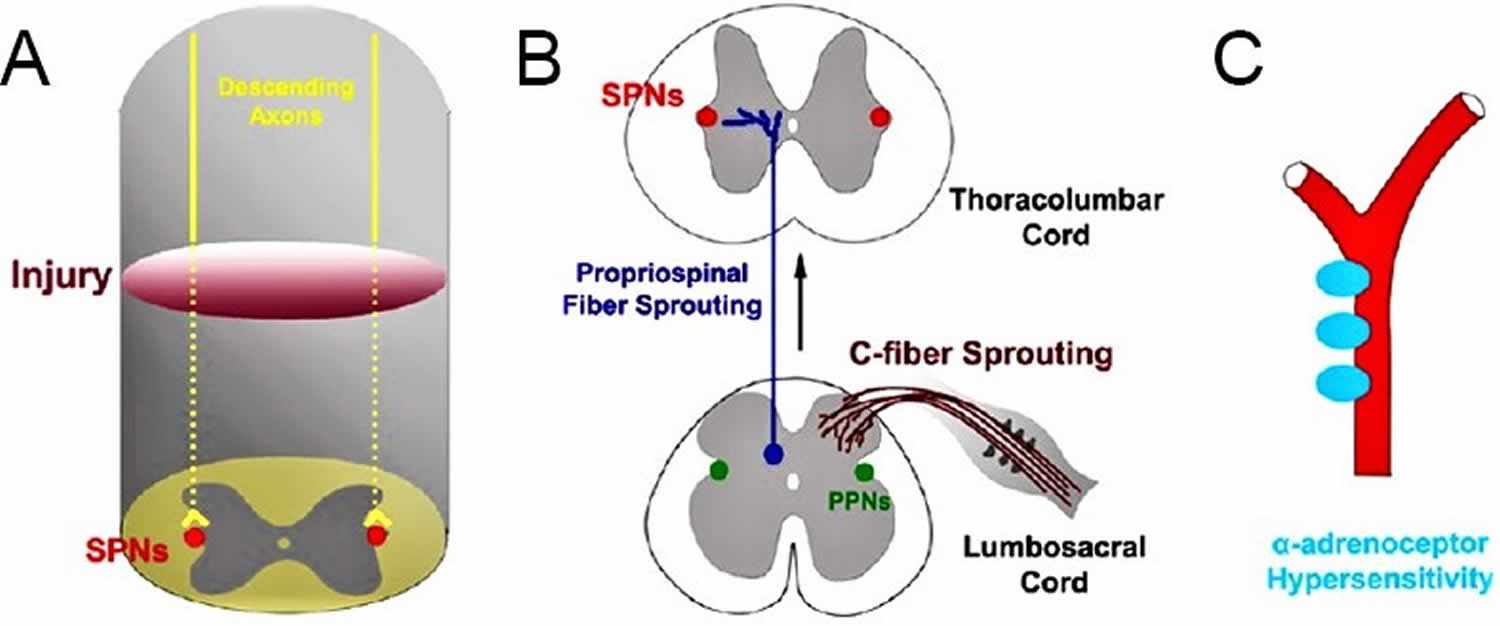
The primary underlying cause of autonomic dysreflexia is loss of supraspinal control over sympathetic preganglionic neurons below the injury, which renders the sympathetic preganglionic neurons hyper-responsive to stimulation 10. Central maladaptive plasticity, including C-fiber sprouting and propriospinal fiber proliferation exaggerates noxious afferent transmission to the sympathetic preganglionic neurons, causing them to release massive sympathetic discharges that result in severe hypertensive episodes 10. In parallel, upregulated peripheral vascular sensitivity following spinal cord injury exacerbates the hypertensive response by augmenting gastric and pelvic vasoconstriction. Currently, the majority of clinically employed treatments for autonomic dysreflexia involve anti-hypertensive medications and Botox injections to the bladder 10. Although these approaches mitigate the severity of autonomic dysreflexia, they only yield transient effects and target the effector organs, rather than addressing the primary issue of central sympathetic dysregulation 10. As such, strategies that aim to restore supraspinal reinnervation of sympathetic preganglionic neurons to improve cardiovascular sympathetic regulation are likely more effective for autonomic dysreflexia.
Leakage of urine around catheters that are not obstructed is often due to bladder spasms that may be associated with dysreflexia episodes. For these cases, overactive bladder medications such as oxybutynin and mirabegron can be used. In severe cases, bladder wall injections of botulinum toxin (Botox) can be used. Urinary infections may also cause bladder spasms without catheter blockage, but such spasms are usually transient and disappear when the urinary tract infection (UTI) is successfully treated. Constipation may also be a contributing factor.
Patients with spinal cord injury and autonomic dysreflexia often undergo medical procedures and surgeries such as urologic instrumentations that can trigger dysreflexia episodes. General or regional anesthesia may be used for these procedures. Regional anesthesia in the form of a spinal anesthetic has the advantage of blocking both limbs of the reflex arc and thereby avoids autonomic dysreflexia. However, determining the level of anesthesia may be difficult, and placement of the spinal may be challenging in patients with spinal cord injuries. An epidural catheter may also be considered for longer cases as it has the advantage of being able to be “topped off.” Epidurals are subject to incomplete blocks and may be even more difficult to place. If general anesthesia is used and hypertension or other evidence of a dysreflexia episode develops, deepening the level of anesthesia by increasing the anesthetic agent often alleviates the episode. If however, the hypertension is not resolved by deepening the anesthetic, then antihypertensive medications should be used until the stimulus is withdrawn.
The use of 10 ml of 2% lidocaine administered intravesically 4-6 minutes prior to routine Foley catheter changes has been shown to reduce episodes of autonomic dysreflexia significantly.
Use of botox for chemodenervation of the bladder has also been shown to reduce autonomic dysreflexia in susceptible individuals.
Minocycline has been shown to have a neuroprotective effect in animal testing models, but has not yet been shown to have a similar clinical effect in humans.
Autonomic dysreflexia causes
The most common cause of autonomic dysreflexia is spinal cord injury, usually above the T6 level. It is unlikely to occur if the level is below T10 11. The higher the injury level, the worse the severity of the cardiovascular dysfunction. The severity and frequency of autonomic dysreflexia episodes are also associated with the completeness of the spinal cord injury. Patients usually develop autonomic dysreflexia one month to one year after their injury. However, it has also been described in the first days or weeks after the original trauma. Objectively, an episode is defined as an increase in systolic blood pressure of 25 mm Hg.
Other causes include:
- Guillain-Barré syndrome (disorder in which the body’s immune system mistakenly attacks part of the nervous system)
- Side effects of some medicines
- Severe head trauma and other brain injuries
- Subarachnoid hemorrhage (a form of brain bleeding)
- Use of illegal stimulant drugs such as cocaine and amphetamines
Autonomic dysreflexia is a condition characterized by transient bursts of massive sympathetic discharges that result in dangerous episodic hypertension in response to a noxious stimulus below the level of injury 12. Clinically, autonomic dysreflexia is indicated when systolic blood pressure rises above baseline by at least 20 mmHg. However, since individuals with spinal cord injury are typically hypotensive, a rise of blood pressure towards “normal” ranges could also suggest a dysreflexic event. Autonomic dysreflexia manifests in both acute and chronic stages of spinal cord injury, and although it is more prevalent in complete injuries above T6 13, individuals with incomplete spinal cord injury are prone to developing it as well (Helkowski et al., 2003). Noxious cutaneous and visceral stimuli below the neurological level trigger autonomic dysreflexia, but bladder and colorectal distention are the most potent triggers for this response. Accordingly, colorectal distention-induced autonomic dysreflexia via an inflatable balloon tipped catheter has become a well-established method for studying the hyper-reflexive response in animal studies 14. However, a major limitation to this method is that it is not natural, as in these investigations, autonomic dysreflexia is stimulated in an artificial manner. Therefore, another method of evaluating autonomic dysreflexia in pre-clinical studies is by detecting the frequency of spontaneous autonomic dysreflexia, which refers to the number of hyperreflexic episodes experienced in a given period of time. Typically, blood pressure and heart rate are simultaneously measured over a 24-hour period via implantable telemetry, and whenever blood pressure spikes instantaneously by more than 20 mmHg, autonomic dysreflexia is signified.
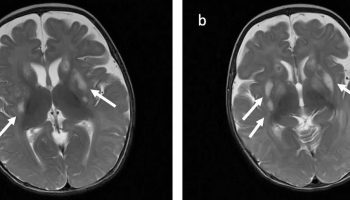
The exact mechanisms underlying autonomic dysreflexia are still unknown, but formation of new intraspinal circuitry paralleled with peripheral vascular plasticity contribute to such a disorder (Figure 1). When afferent fibers below the injury transmit noxious inputs via the dorsal horn, sympathetic preganglionic neurons caudal to the injury that undergo maladaptive plasticity respond by reflexively releasing massive amounts norepinephrine to the splanchnic region, which consequently causes severe hypertension. Due to damaged bulbospinal pathways, inhibitory efferent signals cannot reach and neutralize the activated sympathetic preganglionic neurons below the injury, which results in rostral vasodilation and sustained caudal vasoconstriction. The presentation of autonomic dysreflexia can range from asymptomatic 15 to mildly symptomatic to life-threatening 16. Classic symptoms include sudden hypertension, throbbing headache, face flushing and sweating above injury level. More severe consequences of autonomic dysreflexia include seizures 17, cardiac arrhythmias 18, cerebrovascular hemorrhage 16 and death 4.
Figure 1. Autonomic dysreflexia pathophysiology
Footnote: (A) Loss of supraspinal control over sympathetic preganglionic neurons is the primary cause of disordered blood pressure regulation and AD after spinal cord injury. (B) Increased sprouting of C-fibers (CGRP) within the dorsal horn of the sacral region enhances noxious inputs from the pelvic region. Corresponding propriospinal neuron sprouting transmits these noxious signals rostrally to sympathetic preganglionic neurons (SPNs) within the thoracolumbar region. The sympathetic preganglionic neurons (SPNs) within the thoracolumbar region also undergo morphological changes that render them unstable and supersensitive when stimulated, causing them to release massive surges of sympathetic discharge which markedly increases blood pressure. (C) α-Adrenoceptors within the peripheral vasculature become hypersensitive to sympathetic stimulation resulting in a greater degree of vasoconstriction and smooth muscle contraction when activated by catecholamines thus further augmenting the hypertensive responses.
[Source 10 ]Autonomic dysreflexia prevention
Awareness of the triggers of autonomic dysreflexia is the key to prevention. Appropriate management of bladder care and bowel routine is the best preventive measure because most episodes of autonomic dysreflexia are triggered by such stimuli 8. To prevent autonomic dysreflexia, DO NOT take medicines that cause this condition or make it worse.
In people with spinal cord injury, the following may also help prevent autonomic dysreflexia:
- DO NOT let the bladder become too full
- Pain should be controlled
- Practice proper bowel care to avoid stool impaction
- Practice proper skin care to avoid bedsores and skin infections
- Prevent bladder infections
Autonomic dysreflexia signs and symptoms
Signs and symptoms of autonomic dysreflexia can include any of the following:
- Elevated blood pressure by at least 20 mmHg from baseline
- Pounding headache
- Face and neck flushing
- Heavy sweating above the level of spinal cord injury
- Shivering
- Anxiety or worry
- Bladder or bowel problems
- Blurry vision, widened (dilated) pupils
- Lightheadedness, dizziness, or fainting
- Nausea
- Eyes watering
- Fever
- Goosebumps, flushed (red) skin above the level of the spinal cord injury
- Irregular heartbeat, slow or fast pulse
- Muscle spasms, especially in the jaw
- Nasal congestion
- Rapid breathing
Sometimes there are no symptoms, even with a dangerous rise in blood pressure.
Autonomic dysreflexia possible complications
Complications may occur due to side effects of medicines used to treat the condition. Long-term, severe high blood pressure may cause seizures, bleeding in the eyes, stroke, or death.
Autonomic dysreflexia prognosis
Autonomic dysreflexia prognosis depends on the cause.
People with autonomic dysreflexia due to a medicine usually recover when that medicine is stopped. When autonomic dysreflexia is caused by other factors, recovery depends on how well the disease can be treated.
Autonomic dysreflexia diagnosis
Your health care provider will do a complete nervous system and medical examination. Tell the provider about all the medicines you are taking now and that you took in the past. This helps determine which tests you need.
Tests may include:
- Blood and urine tests
- CT or MRI scan
- ECG (measurement of the heart’s electrical activity)
- Lumbar puncture
- Tilt-table testing (testing of blood pressure as the body position changes)
- Toxicology screening (tests for any drugs, including medicines, in your bloodstream)
- X-rays
Other conditions share many symptoms with autonomic dysreflexia, but have a different cause. So the exam and testing help your doctor rule out these other conditions, including:
- Carcinoid syndrome (tumors of the small intestine, colon, appendix, and bronchial tubes in the lungs)
- Neuroleptic malignant syndrome (a condition caused by some medicines that leads to muscle stiffness, high fever, and drowsiness)
- Pheochromocytoma (tumor of the adrenal gland)
- Serotonin syndrome (drug reaction that causes the body to have too much serotonin, a chemical produced by nerve cells)
- Thyroid storm (life-threatening condition from an overactive thyroid)
Autonomic dysreflexia treatment
There are currently no permanent effective treatments for autonomic dysreflexia, as the most commonly used interventions only have transient and fleeting effects.
Autonomic dysreflexia is life threatening, so it is important to quickly find and treat the problem. During a dysreflexic episode, non-pharmacological measures should be employed first in order to alleviate the symptoms and decrease the hypertensive spikes. If non-pharmacological measures are ineffective in doing so, pharmacological agents with rapid anti-hypertensive properties should be implemented 7. Which if are also unsuccessful in reducing blood pressure, then the individual must be taken to the hospital immediately.
A person with symptoms of autonomic dysreflexia should:
- First, sit upright to induce the orthostatic hypotension response.
- Second, loosen or remove any restrictive clothing and monitor the heart rate and blood pressure at five-minute intervals.
- Third, perform a survey of the possible causes of autonomic dysreflexia, starting with bladder distension.
- Lastly, if the systolic blood pressure remains above 150 mm Hg, administer a short- and fast-acting antihypertensive agent, such as nifedipine or captopril.
Proper treatment depends on the cause. If medicines or illegal drugs are causing the symptoms, those drugs must be stopped. Any illness needs to be treated. For example, the healthcare provider will check for a blocked urinary catheter and signs of constipation.
If a slowing of the heart rate is causing autonomic dysreflexia, drugs called anticholinergics (such as atropine) may be used.
Very high blood pressure needs to be treated quickly but carefully, because the blood pressure can drop suddenly.
A pacemaker may be needed for an unstable heart rhythm.
Nonpharmacological management
A step-by-step protocol for acute and immediate management of autonomic dysreflexia is outlined in the Guidelines of the Consortium for Spinal Cord Medicine 7. First, prompt recognition of symptoms is a must, which can also be confirmed by obtaining a blood pressure measurement. Second, the individual must be kept in an upright position, as this could facilitate blood pooling in the lower limbs due to orthostatic gravitation. In addition, keeping a patient in supine during autonomic dysreflexia can increase the risk for cerebrovascular hemorrhage and/or hypertensive encephalopathy. The next step is to loosen any tight clothing or constricting devices caudal to the injury to improve lower limb blood pooling, but also, tight clothing may act as a noxious stimulus in overly sensitive individuals. This is followed by rapid investigative work to identify and remove the source of noxious stimulation triggering autonomic dysreflexia, however, in 85% of cases it is related to bladder distension or fecal impaction 19. In this case, indwelling urinary catheters should be examined for possible blockages, urinary bags must be emptied and steps must be taken to facilitate voiding. Elimination of the noxious trigger usually eliminates autonomic dysreflexia immediately, however, if elevated blood pressure is sustained, then pharmacological interventions become necessary.
Pharmacological interventions
In a recent systematic review, Krassioukov et al. 19 discussed in detail the most commonly used drugs to alleviate symptoms of autonomic dysreflexia. Nifedipine, a calcium channel blocker traditionally used to treat hypertension and angina, is the most widely used drug for immediate treatment of autonomic dysreflexia. It has been the preferred method by patients due to its instant effects on reducing blood pressure and ameliorating minor and major symptoms 19. It is typically administered via a ‘bite and swallow’ method at a dose of 10 mg, which ensures rapid release and absorption of its contents. The same dose may be taken again within 30–60 minutes if blood pressure has not completely subsided back to normal 20. Nifedipine is also effective in reducing blood pressure spikes during noxious procedures such as cystometry 21, cystoscopy 22 and vibro-ejaculation 23. Nitrates are the second most commonly used agents for acute treatment of autonomic dysreflexia in individuals with spinal cord injury 19. In contrast to nifedipine, nitrates are potent vasodilators that work directly on vascular smooth muscle, and are also primarily used for the treatment of angina. Sublingual administration of nitrates is the preferred method, as it has rapid onset of action and longer lasting effects compared to inhalation 24. Besides anecdotal observations and expert opinions, no studies have provided empirical evidence for the effectiveness of nitrates on autonomic dysreflexia. Although not validated in clinical trials yet, acute administration of neuropathic pain medication, gabapentin, was recently shown to alleviate colorectal distention-induced autonomic dysreflexia in spinal cord injury rats 25. Gabapentin is thought to exert its positive effects by decreasing presynaptic glutamatergic release, as glutamate neurotransmission may contribute to the development of autonomic dysreflexia 25. However, further studies are required to establish gabapentin’s efficacy for treating autonomic dysreflexia in humans with spinal cord injury. Other drugs that are commonly used to reduce hypertensive episodes during autonomic dysreflexia include α-adrenoceptor blockers, angiotensin I converting enzyme inhibitors, ganglionic blockers, and sildenafil (viagra) 19.
Botulinum toxin
Botulinum toxin (Botox) is a potent neurotoxin produced by the anaerobic gram-positive bacterium Clostridium botulinum 26. It contains 8 subtypes, however, subtype A (botulinum toxin type A) is most commonly used in clinical practice due to its potent propensity to cause temporary paralysis of skeletal muscles. Thus, botulinum toxin type A has been widely used as a means for treating abnormal muscle contractions and spasms in a wide range of neuromuscular disorders. It exerts effects by blocking the release of acetylcholine into the neuromuscular junction, thereby inhibiting post-synaptic uptake of the neurotransmitter and preventing muscle contractions. Due to botulinum toxin type A’s ability to cause temporary muscle paralysis, it has been an effective strategy for treating hyper-reflexive bladders and detrusor-sphincter dyssynergia in individuals with spinal cord injury 27. Both detrusor-sphincter dyssynergia and bladder hyper-reflexia are well appreciated triggers for autonomic dysreflexia, as obstruction of the urethral outlet during detrusor muscle contractions increases intravesical pressure, thereby resulting in robust transmission of noxious bladder sensations. Several human studies reported dramatic reductions or disappearance of autonomic dysreflexia secondary to improved detrusor-sphincter dyssynergia and detrusor hyperreflexia after administration of botulinum toxin type A 28. In addition, more recent clinical trials reported decreased severity and frequency of autonomic dysreflexia during urodynamics after administration treatment with botulinum toxin type A, which was related to increased bladder volume, compliance and voiding threshold 29. However, these results are not universal, there is a need to resolve literature dispute as one study showed exacerbation of autonomic dysreflexia in a subpopulation of spinal cord injury individuals following botulinum toxin type A injections 30.
Capsaicin
Capsaicin is a neurotoxin extracted from red peppers and has a selective inhibitory effect on sensory C-fibers through their vanilloid receptors. Low doses of capsaicin initially excite and depolarize C-fibers in the dorsal root, while prolonged application eventually desensitizes and damages the sensory fibers, thus inhibiting transmission of noxious sensations 31. As C-fiber sprouting plays an important role in the pathogenesis of autonomic dysreflexia (see mechanisms section), it is plausible that ablating them with capsaicin would reduce the severity of the hyper-reflexia. One study demonstrated elimination of autonomic dysreflexia during bladder distension following capsaicin treatment in patients with spinal cord injury 32, while another showed exacerbation of autonomic dysreflexia 33. In the latter study, however, resiniferatoxin RXT, a more selective and potent C-fiber desensitizer, eliminated autonomic dysreflexia. These findings suggest that capsaicin must be administered in sufficiently high doses to eliminate C-fibers, since low doses could alternatively stimulate a hyper-reflexive event.
Anti-CD11d antibody
Anti CD-11d antibody is an anti-inflammatory agent specific to the CD11d/CD18 integrin. It has a neuroprotective immunomodulatory effect by blocking the interaction between CD11d and vascular cell adhesion molecule 1 (VCAM), thus preventing pro-inflammatory cytokines from being released and further damaging the spinal cord 34. Administration of CD11d antibody acutely after experimental spinal cord injury markedly reduced CRD-induced autonomic dysreflexia by at least 50%, which persisted for 6 weeks 35. These improvements were not related to changes in CGRP-fiber content, but possibly due to enhanced preservation of neural tissue over several segments caudal to the injury site 36. Moreover, CD11d administration within the first 6 hours of an injury substantially reduced the magnitude of the hypertensive reflex during colorectal distention, suggesting an early window of opportunity for this form of treatment with clinical relevance, as humans typically get to a hospital after a spinal cord injury within 6–12 hours 37.
Cell transplantation
Cell transplantation has been extensively studied for its therapeutic potential to restore sensory/motor function following spinal cord injury, however, little is known about its ability to improve autonomic deficits in this population. Only recently pre-clinical studies started to examine the effects of cell transplantation on cardiovascular autonomic function in spinal cord injury. In the first study to do so, Kalincík et al. 38 showed that transplanting olfactory ensheathing cells following spinal cord injury did not alleviate the severity of autonomic dysreflexia, but accelerated blood pressure recovery time during a hyper-reflexive episode by approximately 50%. Although olfactory ensheathing cells transplantation did not promote nerve regeneration across the graft, there was evidence for morphological alterations in the sympathetic preganglionic neurons caudal and rostral to the injury site, which may have mediated the partial autonomic recovery. In contrasts, transplantation of neural stem cells may be a more promising strategy for restoring cardiovascular autonomic function after spinal cord injury. Recently, Hou et al. 39 transplanted embryonic rat brainstem neural stem cells into a complete T4 transection, which improved resting hemodynamics and dramatically reduced colorectal distention-induced autonomic dysreflexia. These improvements were in conjunction with robust long-distance axonal growth and subsequent topographic reinnervation of caudal sympathetic preganglionic neurons 39. Moreover, since spinal serotonergic depletion caudal to the injury contributes to the initiation of autonomic dysreflexia 40, transplantation of serotonergic cells from fetal raphe nucleus reduced the frequency and magnitude of autonomic dysreflexia in rats with spinal cord injury.
Autonomic dysreflexia nursing interventions
Guidelines of the Consortium for Spinal Cord Medicine recommend several steps to manage autonomic dysreflexia 7:
- First, sit the patient upright to induce the orthostatic hypotension response.
- Second, loosen or remove any restrictive clothing and monitor the patient’s heart rate and blood pressure at five-minute intervals.
- Third, perform a survey of the possible causes of autonomic dysreflexia, starting with bladder distension.
- Lastly, if the patient’s systolic blood pressure remains above 150 mm Hg, administer a short- and fast-acting antihypertensive agent, such as nifedipine or captopril.
- Allen KJ, Leslie SW. Autonomic Dysreflexia. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482434[↩][↩][↩]
- Curt A, Nitsche B, Rodic B, Schurch B, Dietz V. Assessment of autonomic dysreflexia in patients with spinal cord injury. J Neurol Neurosurg Psychiatry. 1997;62:473–477.[↩]
- Autonomic dysreflexia. CMAJ January 10, 2012 184 (1) 66; http://www.cmaj.ca/content/cmaj/184/1/66.full.pdf[↩][↩][↩][↩]
- Dolinak D, Balraj E. Autonomic dysreflexia and sudden death in people with traumatic spinal cord injury. Am J Forensic Med Pathol. 2007;28:95–98.[↩][↩]
- Ho CP, Krassioukov AV. Autonomic dysreflexia and myocardial ischemia. Spinal Cord 2010;48:714-5.[↩]
- Groah SL, Nash MS, Ward EA, et al. Cardiometabolic risk in community-dwelling persons with chronic spinal cord injury. J Cardiopulm Rehabil Prev 2011;31:73-80.[↩]
- Consortium for Spinal Cord Medicine (2002) Acute management of autonomic dysreflexia: individuals with spinal cord injury presenting to health-care facilities. J Spinal Cord Med. 25(Suppl 1):S67–88.[↩][↩][↩][↩]
- Consortium for Spinal Cord Medicine. Acute management of autonomic dysreflexia: individuals with spinal cord injury presenting to health care facilities. J Spinal Cord Med 2001;25(Suppl 1):S67-88.[↩][↩]
- Elliott S, Krassioukov A. Malignant autonomic dysreflexia in spinal cord injured men. Spinal Cord 2006;44:386-92.[↩]
- Sharif H, Hou S. Autonomic dysreflexia: a cardiovascular disorder following spinal cord injury. Neural Regen Res. 2017;12(9):1390-1400. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5649450/[↩][↩][↩][↩][↩]
- Allen KJ, Leslie SW. Autonomic Dysreflexia. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482434/[↩]
- Karlsson AK. Autonomic dysreflexia. Spinal Cord. 1999;37:383–391.[↩]
- Mathais CJ. Handbook of Clinical Neurology. New York: Elsevier Science; 1992. The cardiovascular sysem in tetraplegia and paraplegia.[↩]
- Krassioukov AV, Weaver LC. Reflex and morphological changes in spinal preganglionic neurons after cord injury in rats. Clin Exp Hypertens. 1995;17:361–373.[↩]
- Ekland MB, Krassioukov AV, McBride KE, Elliott SL. Incidence of autonomic dysreflexia and silent autonomic dysreflexia in men with spinal cord injury undergoing sperm retrieval: implications for clinical practice. J Spinal Cord Med. 2008;31:33–39[↩]
- Vallès M, Benito J, Portell E, Vidal J. Cerebral hemorrhage due to autonomic dysreflexia in a spinal cord injury patient. Spinal Cord. 2005;43:738–740.[↩][↩]
- Fausel RA, Paski SC. Autonomic dysreflexia resulting in seizure after colonoscopy in a patient with spinal cord injury. ACG Case Rep J. 2014;1:187–188.[↩]
- Pine ZM, Miller SD, Alonso JA. Atrial fibrillation associated with autonomic dysreflexia. Am J Phys Med Rehabil. 1991;70:271–273.[↩]
- Krassioukov A, Warburton DE, Teasell R, Eng JJ Spinal Cord Injury Rehabilitation Evidence Research Team. A systematic review of the management of autonomic dysreflexia after spinal cord injury. Arch Phys Med Rehabil. 2009;90:682–695.[↩][↩][↩][↩][↩]
- Ferguson RK, Vlasses PH. Hypertensive emergencies and urgencies. JAMA. 1986;255:1607–1613.[↩]
- Thyberg M, Ertzgaard P, Gylling M, Granerus G. Effect of nifedipine on cystometry-induced elevation of blood pressure in patients with a reflex urinary bladder after a high level spinal cord injury. Paraplegia. 1994;32:308–313.[↩]
- Dykstra DD, Sidi AA, Anderson LC. The effect of nifedipine on cystoscopy-induced autonomic hyperreflexia in patients with high spinal cord injuries. J Urol. 1987;138:1155–1157.[↩]
- Steinberger RE, Ohl DA, Bennett CJ, McCabe M, Wang SC. Nifedipine pretreatment for autonomic dysreflexia during electroejaculation. Urology. 1990;36:228–231.[↩]
- Braddom RL, Rocco JF. Autonomic dysreflexia. A survey of current treatment. Am J Phys Med Rehabil. 1991;70:234–241.[↩]
- Rabchevsky AG, Patel SP, Lyttle TS, Eldahan KC, O’Dell CR, Zhang Y, Popovich PG, Kitzman PH, Donohue KD. Effects of gabapentin on muscle spasticity and both induced as well as spontaneous autonomic dysreflexia after complete spinal cord injury. Front Physiol. 2012;3:329.[↩][↩]
- Nigam PK, Nigam A. Botulinum toxin. Indian J Dermatol. 2010;55:8–14.[↩]
- Khera M, Somogyi GT, Kiss S, Boone TB, Smith CP. Botulinum toxin A inhibits ATP release from bladder urothelium after chronic spinal cord injury. Neurochem Int. 2004;45:987–993.[↩]
- Schurch B, Stöhrer M, Kramer G, Schmid DM, Gaul G, Hauri D. Botulinum-A toxin for treating detrusor hyperreflexia in spinal cord injured patients: a new alternative to anticholinergic drugs? Preliminary results . J Urol. 2000;164:692–697.[↩]
- Fougere RJ, Currie KD, Nigro MK, Stothers L, Rapoport D, Krassioukov AV. Reduction in bladder-related autonomic dysreflexia after onabotulinumtoxina treatment in spinal cord injury. J Neurotrauma. 2016;33:1651–1657.[↩]
- Chen SF, Kuo HC. Improvement in autonomic dysreflexia after detrusor onabotulinumtoxinA injections in patients with chronic spinal cord injuries. Ci Ji Yi Xue Za Zhi. 2012;24:201–204.[↩]
- Lynn B. Capsaicin: actions on nociceptive C-fibres and therapeutic potential. Pain. 1990;41:61–69.[↩]
- Igawa Y, Satoh T, Mizusawa H, Seki S, Kato H, Ishizuka O, Nishizawa O. The role of capsaicin-sensitive afferents in autonomic dysreflexia in patients with spinal cord injury. BJU Int. 2003;91:637–641.[↩]
- Giannantoni A, Di Stasi SM, Stephen RL, Navarra P, Scivoletto G, Mearini E, Porena M. Intravesical capsaicin versus resiniferatoxin in patients with detrusor hyperreflexia: a prospective randomized study. J Urol. 2002;167:1710–1714.[↩]
- Weaver LC, Bao F, Dekaban GA, Hryciw T, Shultz SR, Cain DP, Brown A. CD11d integrin blockade reduces the systemic inflammatory response syndrome after traumatic brain injury in rats. Exp Neurol. 2015;271:409–422.[↩]
- Gris D, Marsh DR, Oatway MA, Chen Y, Hamilton EF, Dekaban GA, Weaver LC. Transient blockade of the CD11d/CD18 integrin reduces secondary damage after spinal cord injury, improving sensory, autonomic, and motor function. J Neurosci. 2004;24:4043–4051.[↩]
- Gris D, Marsh DR, Dekaban GA, Weaver LC. Comparison of effects of methylprednisolone and anti-CD11d antibody treatments on autonomic dysreflexia after spinal cord injury. Exp Neurol. 2005;194:541–549.[↩]
- Ditor DS, Bao F, Chen Y, Dekaban GA, Weaver LC. A therapeutic time window for anti-CD 11d monoclonal antibody treatment yielding reduced secondary tissue damage and enhanced behavioral recovery following severe spinal cord injury. J Neurosurg Spine. 2006;5:343–352.[↩]
- Kalincík T, Choi EA, Féron F, Bianco J, Sutharsan R, Hayward I, Mackay-Sim A, Carrive P, Waite PM. Olfactory ensheathing cells reduce duration of autonomic dysreflexia in rats with high spinal cord injury. Auton Neurosci. 2010;154:20–29.[↩]
- Hou S, Tom VJ, Graham L, Lu P, Blesch A. Partial restoration of cardiovascular function by embryonic neural stem cell grafts after complete spinal cord transection. J Neurosci. 2013;33:17138–17149.[↩][↩]
- Cormier CM, Mukhida K, Walker G, Marsh DR. Development of autonomic dysreflexia after spinal cord injury is associated with a lack of serotonergic axons in the intermediolateral cell column. J Neurotrauma. 2010;27:1805–1818.[↩]