What is a bartholin cyst
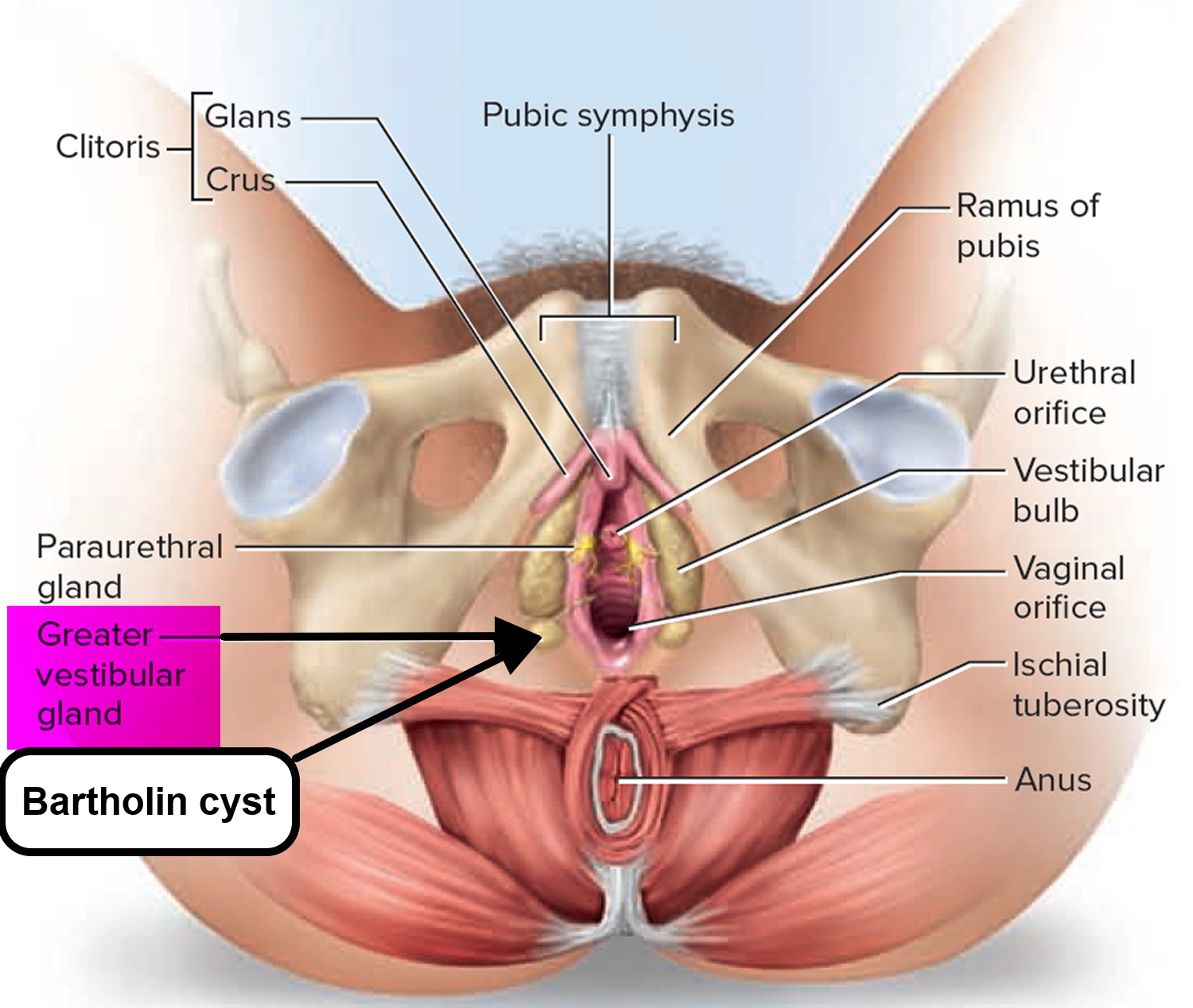
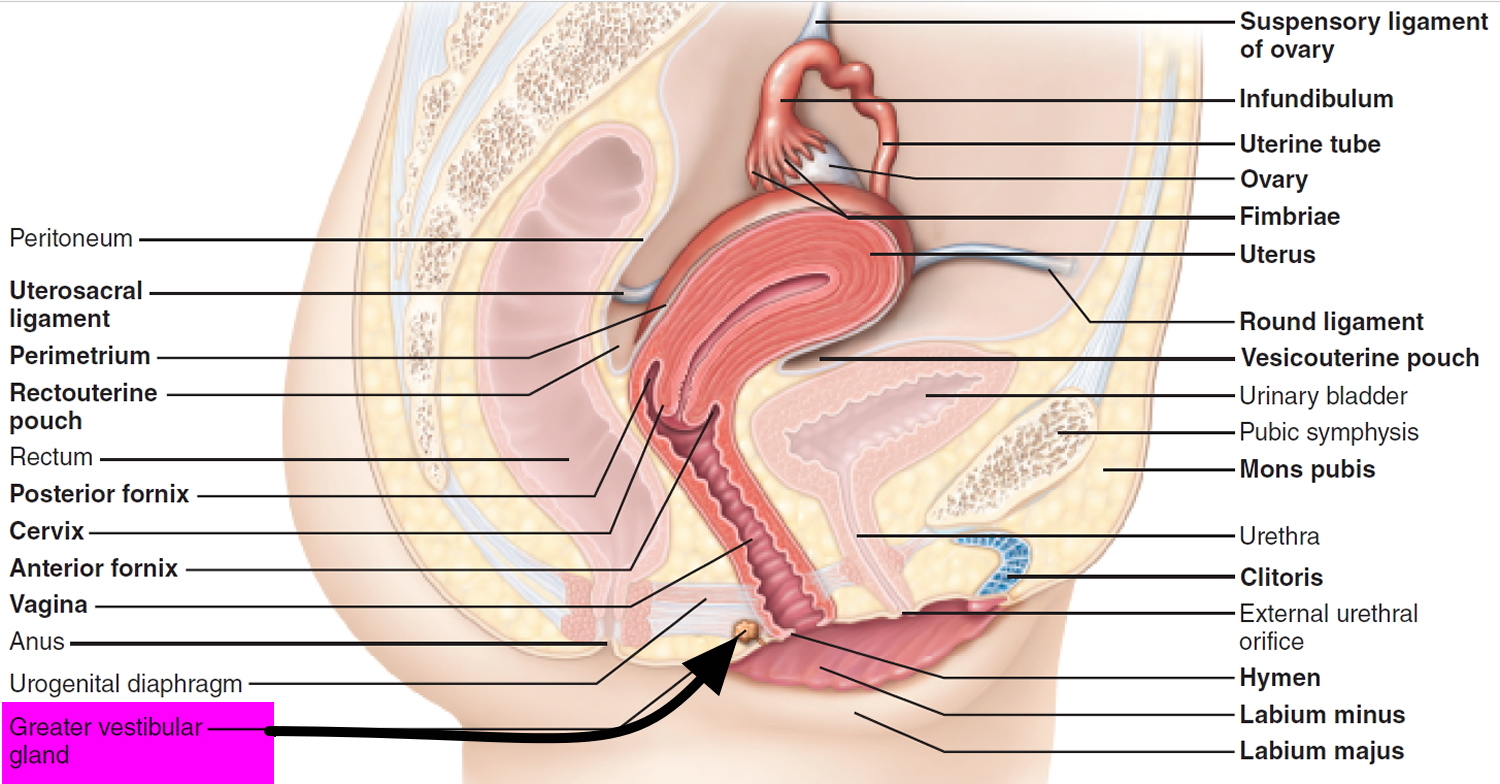
The Bartholin’s glands or greater vestibular glands, are a pair of pea-sized (rarely exceed 1 cm) exocrine glands, located at 4 O’ clock and 8 O’ clock position in the labia minora and drain through 2- to 2.5-cm–long ducts that empty into the vestibule (see Figures 1 and 2). They are not palpable except in the presence of disease or infection. They resemble salivary glands in structure. They are similar to Cowper’s glands in males. They secret colorless, mucoid discharge on sexual excitation which moisturizes the vestibule. During sexual stimulation, Bartholin’s glands release lubricant fluid 1. Bartholin’s glands begin to function at puberty 2.
The first person to describe this gland was Kaspar Bartholin, in 1977. This Dane became known for describing it along with the accessory ducts of the salivary and sublingual glands 3.
Bartholin cysts are common complications of the Bartholin’s gland, affecting the ductal region due to outlet blockage. When the Bartholin’s gland duct orifice becomes obstructed, the glands produce a build-up of mucus. This build-up leads to a cystic dilation of the duct and cyst formation. Infection of this cyst is likely to result in Bartholin’s gland abscess. Duct cyst is not required for the development of abscess 4. Bartholin’s abscess and cyst account for 2% of all gynaecological visits per annum in women at child-bearing age.
Bartholin’s abscesses are almost three times more common than Bartholin’s cysts 5. Bartholin’s abscess cultures often show polymicrobial infection. Large proportions of Bartholin’s gland abscess are bacterial culture positive with Escherichia coli being a common pathogen (Table 1). When determining antibacterial treatment options, it is essential to correlate the microbiological findings with their anti-biogram 6.
One case-control study 7 found that white and black women were more likely to develop Bartholin’s cysts or abscesses than Hispanic women, and that women of high parity were at lowest risk.
Bartholin’s gland abscess has been reported to have a recurrence up to 38% 2.
Bartholin’s gland abscess presents with a swelling in the vulva associated with pain and fever. On examination, an erythematous, localized, tender, soft, fluctuant swelling would be present in the labia minora. This is usually polymicrobial warranting broad-spectrum antibiotics 8. If not treated in time, it can rupture spontaneously but tends to recur 8.
Gradual involution of the Bartholin’s glands can occur by the time a woman reaches 30 years of age 9. This may account for the more frequent occurrence of Bartholin’s duct cysts and gland abscesses during the reproductive years, especially between 20 and 29 years of age.
The differential diagnosis includes hematoma, infected inguinal hernia or hydrocele of the canal of Nuck, infected lymphangioma, leiomyoma, lipoma, teratoma and sarcoma 8.
Because a vulvar mass in a postmenopausal woman can be cancer, excisional biopsy may be required. Some investigators 10 have suggested that surgical excision is unnecessary because of the low risk of Bartholin’s gland cancer (0.114 cancers per 100,000 woman-years). However, if the diagnosis of cancer is delayed, the prognosis can be poor.
Table 1. Bacteriology of Bartholin’s gland cyst and abscess
| Bacterial agents: aerobes | Bacterial agents: anaerobes |
|---|---|
| Brucella melitensis | Bacteroides species |
| Chlamydia trachomatis | Pasteurella bettii |
| Escherichia coli | Salmonella panama |
| Hypermucoviscous Klebsiella pneumonia | Clostridium perfringens |
| Neisseria gonorrhea | Peptostreptococcus species |
| Neisseria sicca | Fusobacterium species |
| Pseudomonas aeruginosa | |
| Staphylococcus aureus: Panton-Valentine | |
| Leucocidin production | |
| Streptococcus species |
Lesions in the Bartholin’s gland can occur in the form of carcinomas, a rare type of gynecological tumor that accounts for 2-7% of vulvar carcinomas. This type of vulvar growth is carefully monitored among postmenopausal women who are more prone to Bartholin’s malignancy 12. The median age at which Bartholin’s gland cancer is diagnosed is 57 years old and carcinoma incidence is highest among women in their 60’s. The 2 common types, adenocarcinoma and squamous cell carcinoma, account for 80-90% of primary cases. The remaining 10-20% of cases include transitional, adenoid-cystic or undifferentiated carcinomas 13. Human papillomavirus is only related to squamous cell lesions. Benign tumors are rarer than carcinomas.
See your doctor if you have a painful lump near the opening of your vagina that doesn’t improve after two or three days of self-care — for instance, soaking the area in warm water (sitz bath). If the pain is severe, make an appointment with your doctor right away.
Also see your doctor promptly if you find a new lump near your vaginal opening and you’re older than 40. Although rare, such a lump may be a sign of a more serious problem, such as cancer.
The Bartholin’s glands
The Bartholin’s glands, also called greater vestibular glands, are two pea-sized glands located at the posterior region of the vaginal opening. The glands have an oval shape with an average size of 0.5 cm and are located lateral to the bulbospongiosus muscle. The glands are homologous to the male bulbourethral or Cowper’s glands. The glands are connected to ducts, approximately 2.5 cm in width, situated between the labia minora and the hymenal edge. Through these ducts, the glands drain the mucus into the vaginal vestibule. The ducts open at the 4 and 8 o’clock position at the vaginal vestibule on each side of the vaginal opening. Embryologically, the Bartholin’s glands originate from the urogential sinus and therefore, utilize the external pudendal artery as a blood source. The gland is innervated by the pudendal nerve. The lymphatic drainage of Bartholin’s glands includes superficial inguinal and pelvic nodes.
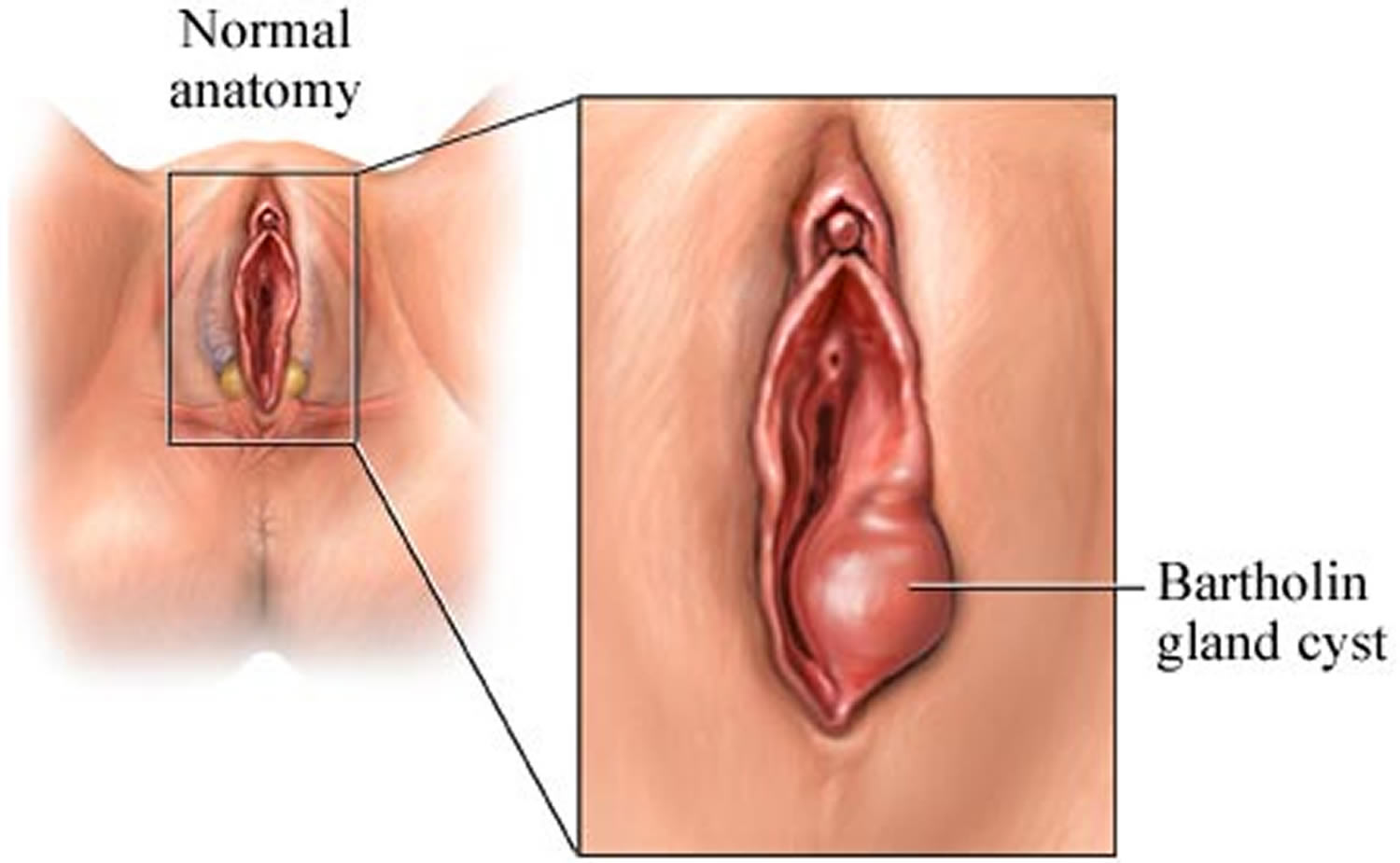
Figure 1. Bartholin glands (greater vestibular glands)
Figure 2. Bartholin glands (greater vestibular glands)
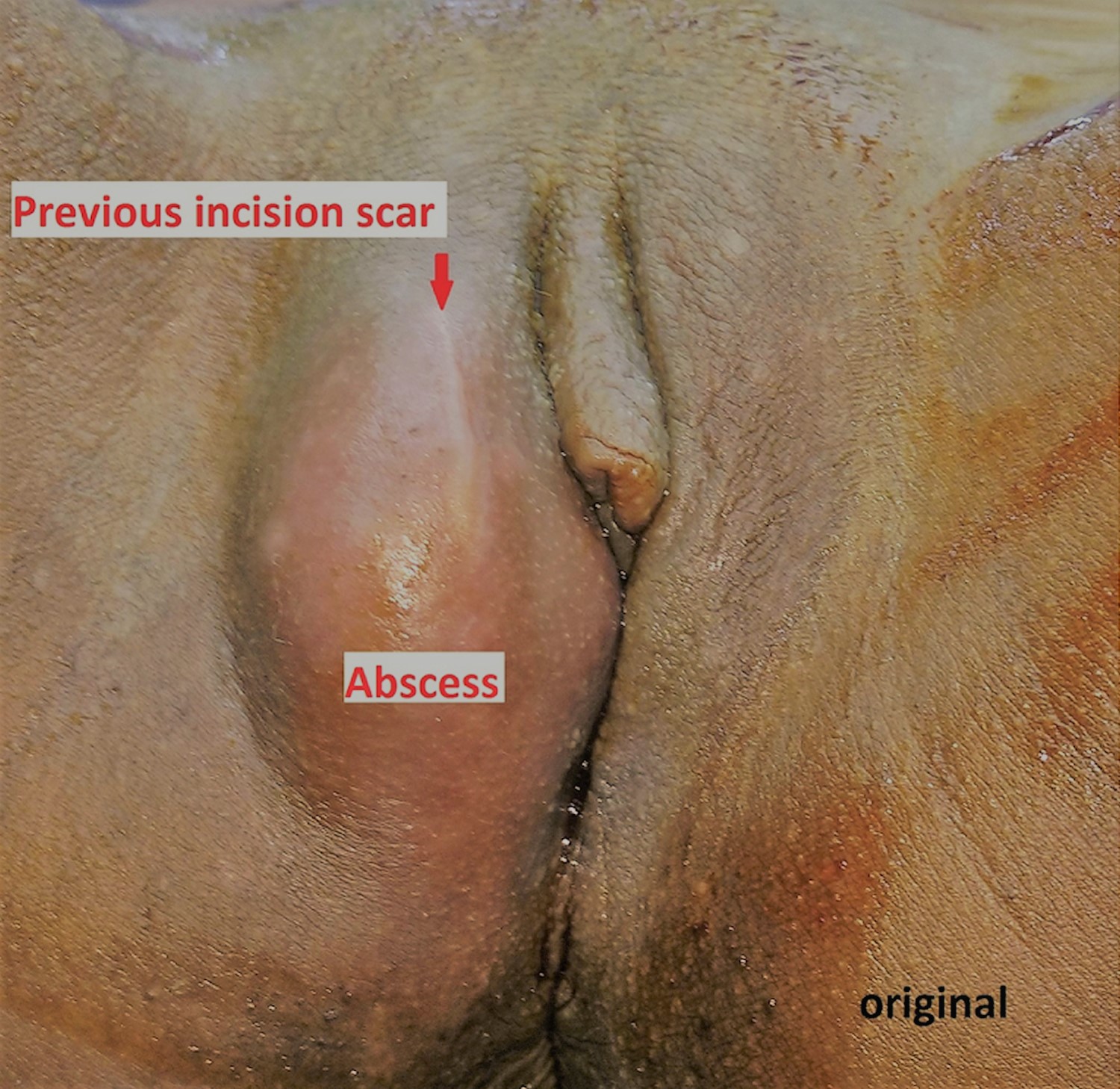
Figure 3. Bartholin gland abscess (right Bartholin’s gland abscess)
Note: A linear scar of previous incision is seen.
Bartholin’s cyst complications
A Bartholin’s cyst or abscess may recur and again require treatment.
Bartholin cyst causes
Experts believe that the cause of a Bartholin’s cyst is a backup of fluid. Fluid may accumulate when the opening of the gland (duct) becomes obstructed, perhaps caused by infection or injury.
A Bartholin’s cyst can become infected, forming an abscess. A number of bacteria may cause the infection, including Escherichia coli (E. coli) and bacteria that cause sexually transmitted infections such as gonorrhea and chlamydia.
Bartholin cyst prevention
There’s no way to prevent a Bartholin’s cyst. However, practicing safe sex — in particular, using a condom — and maintaining good hygiene habits may help to prevent infection of a cyst and the formation of an abscess.
Bartholin cyst signs and symptoms
Bartholin’s cyst may be asymptomatic if Bartholin’s cyst is small and not inflamed. However, a small Bartholin’s cyst may be observed by physicians as a small mass in the region of the Bartholin’s gland. If the cyst grows, you might feel a lump or mass near your vaginal opening. Although a cyst is usually painless, it can be tender. A painless mass may be present without surrounding cellulitis, while abscesses commonly present with cellulitis and lymphangitis. Larger cysts and abscess tend to cause severe vulvar pain and swelling such that the patient experiences difficulty in walking, sitting and engaging in sexual intercourse (dyspareunia). During examination, an abscess presents as a tender mass in the lower vestibular region surrounded by erythema and edema. When the abscess grows large enough to extend to the upper labia, it may result in skin rupture and spontaneous drain 14. The patient may experience a sudden relief of pain after a discharge, highly suggesting presence of spontaneous rupture. Cysts can present in form of inguinal hernia 15.
A full-blown infection of a Bartholin’s cyst can occur in a matter of days. If the cyst becomes infected, you may experience:
- A tender, painful lump near the vaginal opening
- Discomfort while walking or sitting
- Pain during intercourse
- Fever
A Bartholin’s cyst or abscess typically occurs on only one side of the vaginal opening.
In neonate, Bartholin’s duct cyst associated with hydrouretero-nephrosis and contralateral renal cyst can cause urinary retention 16. In the case of Bartholin’s gland cancer, painless mass is also present in the vulva-region. Mass fixated to the underlying tissue is often suspected for malignancy. First detection of sentinel node may lead to diagnosis of adenocarcinoma of Bartholin’s gland 17.
Diagnosis of Bartholin’s gland carcinoma is established upon histological examination. Women over the age of 40 are recommended to undergo drainage and biopsy to eliminate possible occurrence of carcinoma. Due to the rarity of Bartholin’s cancer, a biopsy is recommended over excision 18. In cases where Bartholin’s cancer is suspected, diagnostic criteria is as follows. The tumor must be primarily located in the labia, the surrounding skin must remain undamaged, and there must be at least a small amount of glandular epithelium present. When Bartholin gland carcinomas are present, metastatic disease is likely due to the vulva’s extensive vascular and lymphatic network 19.
Bartholin cyst diagnosis
To diagnose a Bartholin’s cyst, your doctor may:
- Ask questions about your medical history
- Perform a pelvic exam
- Take a sample of secretions from your vagina or cervix to test for a sexually transmitted infection
- Recommend a test of the mass (biopsy) to check for cancerous cells if you’re postmenopausal or over 40
If cancer is a concern, your doctor may refer you to a gynecologist who specializes in cancers of the female reproductive system.
Several labia and vaginal lesions can imitate Bartholin’s gland diseases. In such situations, differential diagnosis should be considered for the abscess or mass. Differential diagnosis include different types of cysts (inclusion, Gartner, Skene’s, sebaceous, vestibular mucosa, canal of Nuck), leiomyomas fibroma, hernia, hidradenoma, hematomas, lipomas, endometriosis, syringoma, accessory breast tissue, folliculitis, urethral diverticula, hidradenitis suppurativa, chancroid, gonorrhea, syphilis, vaginitis, warts or Bartholin’s gland cyst, abscess or cancer (Table 2) 20.
Table 2. Pathology of Bartholin’s Glands
| Classification | Histomorphology |
|---|---|
| Cancer of Bartholin’s gland | adenoid cystic carcinoma |
| squamous cell carcinoma | |
| lymphoepithelioma-like carcinoma | |
| vulvar leiomyosarcoma | |
| endometrial adenocarcinoma | |
| Merkel cell carcinoma | |
| mucinous adenocarcinoma | |
| transitional cell carcinoma | |
| epithelioid sarcoma | |
| malignant melanoma | |
| Non-Hodgkin’s lymphoma | |
| human papillomavirus type 16 | |
| Paget’s disease | |
| small cell neuroendocrine | |
| Benign | nodular hyperplasia |
| endometriosis | |
| adenoma and adenomyoma | |
| papilloma | |
| mucocele | |
| Abscess | cellular blue nevus |
Bartholin cyst treatment
Often a Bartholin’s cyst requires no treatment — especially if the cyst causes no signs or symptoms 21, but symptomatic Bartholin’s duct cysts and gland abscesses require drainage. Unless spontaneous rupture occurs, an abscess rarely resolves on its own. When needed, treatment depends on the size of the cyst, your discomfort level and whether it’s infected, which can result in an abscess.
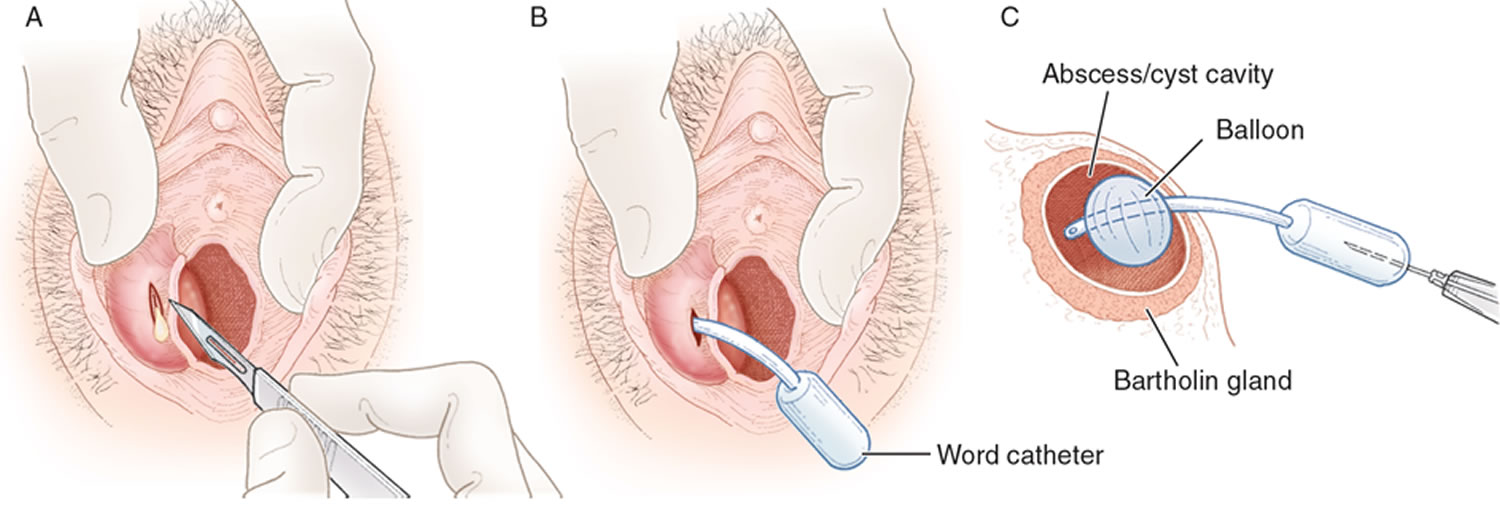
Definitive drainage involves Word catheter placement for Bartholin’s duct cysts and gland abscesses, and marsupialization for duct cysts.
Treatment options your doctor may recommend include:
- Sitz baths. Soaking in a tub filled with a few inches of warm water (sitz bath) several times a day for three or four days may help a small, infected cyst to rupture and drain on its own.
- Surgical drainage. You may need surgery to drain a cyst that’s infected or very large. Drainage of a cyst can be done using local anesthesia or sedation. For the procedure, your doctor makes a small incision in the cyst, allows it to drain, and then places a small rubber tube (catheter) in the incision. The catheter stays in place for up to six weeks to keep the incision open and allow complete drainage. Although incision and drainage is a relatively quick and easy procedure that provides almost immediate relief to the patient, this approach should be discouraged because there is a tendency for the cyst or abscess to recur 22, 23. One investigator 24 reported a 13 percent failure rate for the procedure. Furthermore, incision and drainage may make later Word catheter placement or marsupialization difficult 23.
- Antibiotics. Your doctor may prescribe an antibiotic if your cyst is infected or if testing reveals that you have a sexually transmitted infection. But if the abscess is drained properly, you may not need antibiotics. Antibiotic therapies include Ceftriaxone, Ciprofloxacin, Doxycycline and Azithromycin. This treatment option should be restricted to women who have high risk of complicated infection such as recurrence, pregnancy, immunosuppression, MRSA risk, widespread surrounding cellulitis and gonorrhea or chlamydia infection. Topical or local anesthetics such as lidocaine and bupivacaine are also used to treat abscesses.
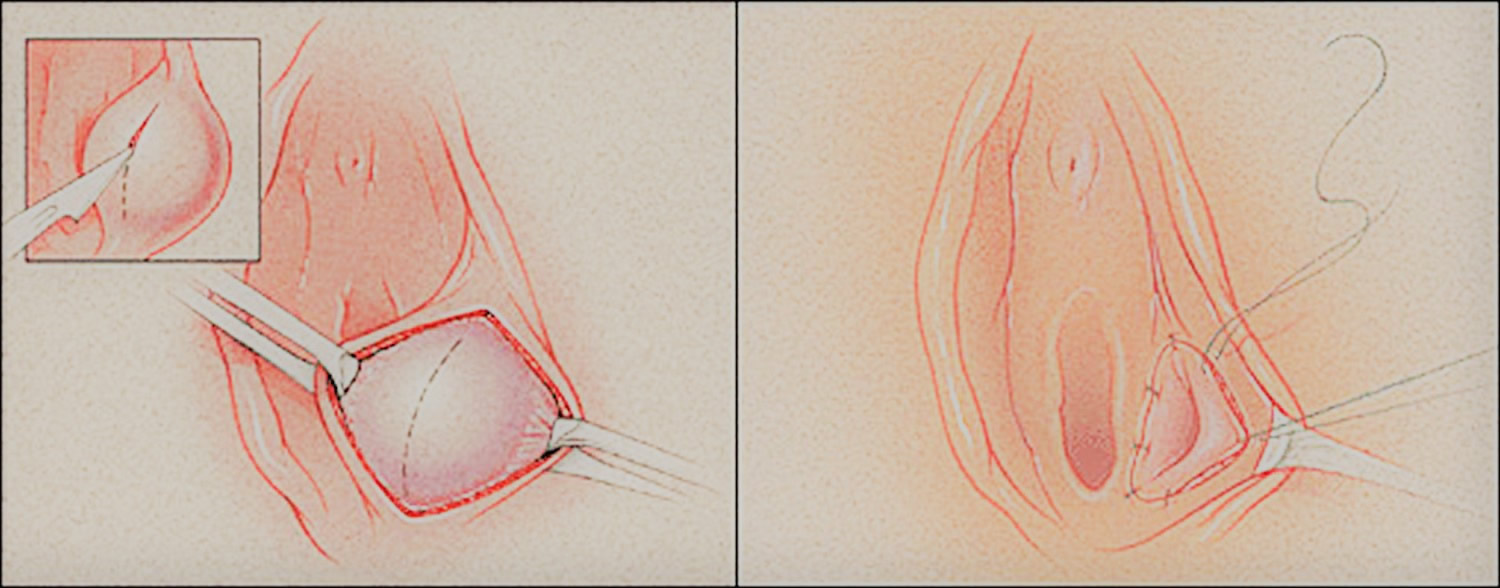
- Marsupialization of bartholin cyst. An alternative to Word catheter placement is marsupialization of a Bartholin’s cyst (Figure 6). This procedure should not be used when an abscess is present 25. Marsupialization can be performed in the office or if the cyst is deeply seated, in an outpatient surgical suite. Your doctor places stitches on each side of a drainage incision to create a permanent opening less than 1/4-inch (about 6-millimeter) long. An inserted catheter may be placed to promote drainage for a few days after the procedure and help prevent recurrence. Approximately 5 to 15 percent of Bartholin’s duct cysts recur after marsupialization 26. Complications associated with the procedure include dyspareunia (painful sex), hematoma, and infection 22.
Word catheter
A Word catheter is commonly used to treat Bartholin’s duct cysts and gland abscesses 27. The stem of this rubber catheter is 1 inch long and the diameter of a no. 10 French Foley catheter. The small, inflatable balloon tip of the Word catheter can hold about 3 mL of saline (Figure 4).
The inflated balloon allows the catheter to remain within the cavity of the cyst or abscess (Figure 5). The free end of the catheter can be placed in the vagina 23. To allow epithelialization of the surgically created tract, the Word catheter is left in place for four to six weeks 23, although epithelialization may occur as soon as three to four weeks 26.
Sitz baths taken two to three times daily may aid patient comfort and healing during the immediate postoperative period. Sex may be resumed after catheter insertion.
Unless there is evidence of cellulitis, antibiotic therapy is unnecessary. If cellulitis is present, cultures may be obtained, but the results rarely change management. Empiric broad-spectrum antibiotic therapy is started before culture results are available 28.
If a Bartholin’s cyst or abscess is too deep, Word catheter placement is impractical, and other options must be considered 25.
Figure 4. Word catheter
Figure 5. Word catheter insertion procedure
Figure 6. Marsupialization of Bartholin’s duct cyst
Note: (Left) A vertical incision is made over the center of the cyst to dissect it free of mucosa. (Right) The cyst wall is everted and approximated to the edge of the vestibular mucosa with interrupted sutures.
Rarely, for persistent cysts that aren’t effectively treated by the above procedures, your doctor may recommend surgery to remove the Bartholin’s gland. Surgical removal is usually done in a hospital under general anesthesia. Surgical removal of the gland carries a greater risk of bleeding or complications after the procedure.
Excision
Although Bartholin’s gland abscesses may rupture and drain spontaneously, recurrence is likely, and surgical excision may be necessary. Excision is not an office-based procedure.
Cultures for N. gonorrhoeae and C. trachomatis may be obtained. However, Bartholin’s gland abscesses tend to be polymicrobial, and empiric broad-spectrum antibiotic therapy should be used.
Excision of the Bartholin’s gland should be considered in patients who do not respond to conservative attempts to create a drainage tract, but the procedure should be performed when there is no active infection 22. If multiple attempts have been made to drain a cyst or an abscess, adhesions may be present, making excision difficult and resulting in postoperative scarring and chronic pain in the area 21.
Some investigators 21, 25 recommend excision of the Bartholin’s gland to exclude adenocarcinoma when cysts or abscesses occur in patients more than 40 years of age. Even though adenocarcinoma of the Bartholin’s gland is rare, gynecologic oncology referral should be considered for older patients with Bartholin’s duct cysts or gland abscesses.
Treatment of Bartholin’s carcinomas
Treatment of Bartholin’s carcinomas may vary between surgical methods, vulvectomy, or radiotherapy 29. Hyperbaric oxygen therapy following radical vulvectomy promotes wound healing 30. Primary adenoid cystic carcinoma is a rare malignancy of Bartholin’s cancer. Patients with the cancer can undergo adjuvant external beam radiation or hemivulvectomy 31. Early stage I of Bartholin’s carcinoma can be approached with lymphadenectomy 32.
References- Bora SA, Condous G. Bartholin’s, vulval and perineal abscesses. Best Pract Res Clin Obste Gynaecol. 2009;23(5):661–666. Review. https://www.ncbi.nlm.nih.gov/pubmed/19647493
- Reif P., Ulrich D., Bjelic-Radisic V., Hausler M., Schnedl-Lamprecht E., Tamussino K. Management of Bartholin’s cyst and abscess using the Word catheter: implementation, recurrence rates and costs. Eur. J. Obstet. Gynecol. 2015;190:81–84. https://www.ncbi.nlm.nih.gov/pubmed/25963974
- Pundir J, Auld BJ. A review of the management of diseases of the Bartholin’s gland. J Obstet Gynaecol. 2008;28(2) 161-5. Review. https://www.ncbi.nlm.nih.gov/pubmed/18393010
- Lee M.Y., Dalpiaz A., Schwamb R., Miao Y., Waltzer W., Khan Ali. Clinical pathology of Bartholin’s glands: a review of the literature. Curr. Urol. 2014;8:22–25. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4483306/
- Management of Bartholin’s duct cyst and gland abscess. Omole F, Simmons BJ, Hacker Y. Am Fam Physician. 2003 Jul 1; 68(1):135-40. https://www.ncbi.nlm.nih.gov/pubmed/12887119/
- Kessous R, Aricha-Tamir B, Sheizaf B, Steiner N, Moran-Gilad J, Weintraub AY. Clinical and microbiological characteristics of Bartholin gland abscesses. Obstet Gynecol. 2013;122:794–799. https://www.ncbi.nlm.nih.gov/pubmed/24084536
- Aghajanian A, Bernstein L, Grimes DA. Bartholin’s duct abscess and cyst: a case-control study. South Med J. 1994;87:26–9.
- Lee MY, Dalpiaz A, Schwamb R, Miao Y, Waltzer W, Khan A. Clinical Pathology of Bartholin’s Glands: A Review of the Literature. Current Urology. 2015;8(1):22-25. doi:10.1159/000365683. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4483306/
- Stillman FH, Muto MG. The vulva. In: Ryan KJ, Berkowitz RS, Barbieri RL, eds. Kistner’s Gynecology: principles and practice. 6th ed. St. Louis: Mosby, 1995:66–8.
- Visco AG, Del Priore G. Postmenopausal Bartholin gland enlargement: a hospital-based cancer risk assessment. Obstet Gynecol. 1996;87:286–90.
- Management of Bartholin’s Duct Cyst and Gland Abscess. Am Fam Physician. 2003 Jul 1;68(1):135-140. https://www.aafp.org/afp/2003/0701/p135.html
- Schwarzlos G, Bolz M, Muller H. Primary carcinoma of Bartholin’s glands with HPV 18 detection. Zentralbl Gynakol. 1997;119:133–135. https://www.ncbi.nlm.nih.gov/pubmed/9173772
- Felix JC, Cote RJ, Kramer EE, Saigo P, Goldman GH. Carcinomas of Bartholin’s gland. Histogenesis and the etiological role of human papillomavirus. Am J Pathol. 1993;142:925–933. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1886794/
- Omole F, Simmons BJ, Hacker Y. Management of Bartholin’s duct cyst and gland abscess. Am Fam Physician. 2003;68:135–140. https://www.aafp.org/afp/2003/0701/p135.html
- Altstiel T, Coster R. Bartholin cyst presenting as inguinal hernia. S D J Med. 1993;46:7–8. https://www.ncbi.nlm.nih.gov/pubmed/8424150
- Cevik M, Savas M, Guldur ME, Boleken ME. Urinary retention as the presentation of Bartholin’s duct cyst in a neonate. J Pediatr Adolesc Gynecol. 2012;25:e65–67. https://www.ncbi.nlm.nih.gov/pubmed/22578485
- Balepa L, Baeyens L, Nemec E, Verhas M. First detection of sentinel node in adenocarcinoma of Bartholin’s gland. J Gynecol Obstet Biol Reprod (Paris) 2004;33:649–651. https://www.ncbi.nlm.nih.gov/pubmed/15550884
- Mayeaux EJ, Jr, Cooper D. Vulvar procedures: biopsy, bartholin abscess treatment, and condyloma treatment. Obstet Gynecol Clin North Am. 2013;40:759–772. https://www.ncbi.nlm.nih.gov/pubmed/24286999
- Antvorskov JC, Josefsen K, Engkilde K, Funda DP, Buschard K. Dietary gluten and the development of type 1 diabetes. Diabetologia. 2014;75:1770–1780. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4119241
- Koc O, Sengul N, Gurel S. Perineal leiomyoma mimicking complex Bartholin mass. Int Urogynecol J. 2010;21:495–497. https://www.ncbi.nlm.nih.gov/pubmed/19756340
- Hill DA, Lense JJ. Office management of Bartholin gland cysts and abscesses. Am Fam Physician. 1998;57:1611–6.1619–20.
- Stenchever MA. Comprehensive gynecology. 4th ed. St. Louis: Mosby, 2001:482–6,645–6.
- Apgar BS. Bartholin’s cyst/abscess: Word catheter insertion. In: Pfenninger JL, Fowler GC, eds. Procedures for primary care physicians. St. Louis: Mosby, 1994:596–600.
- Mathews D. Marsupialization in the treatment of Bartholin’s cysts and abscesses. J Obstet Gynaecol Br Commonw. 1966;73:1010–2.
- Wilkinson EJ, Stone IK. Atlas of vulvar disease. 5th ed. Baltimore: Williams & Wilkins, 1995:11–5.
- Horowitz IR, Buscema J, Woodruff JD. Surgical conditions of the vulva. In: Rock JA, Thompson JD, eds. Te Linde’s Operative gynecology. 8th ed. Philadelphia: Lipincott-Raven, 1997:890–3.
- Word B. Office treatment of cyst and abscess of Bartholin’s gland duct. South Med J. 1968;61:514–8.
- Brook I. Aerobic and anaerobic microbiology of Bartholin’s abscess. Surg Gynecol Obstet. 1989;169:32–4.
- Duun S. Adenoid cystic carcinoma of Bartholin’s gland-a review of the literature and report of a patient. Acta Obstet Gynecol Scand. 1995;74:78–80. https://www.ncbi.nlm.nih.gov/pubmed/7856439
- Reedy MB, Capen CV, Baker DP, Petersen WG, Kuehl TJ. Hyperbaric oxygen therapy following radical vulvectomy: an adjunctive therapy to improve wound healing. Gynecol Oncol. 1994;53:13–16. https://www.ncbi.nlm.nih.gov/pubmed/8175014
- Hsu ST, Wang RC, Lu CH, Ke YM, Chen YT, Chou MM, Ho ES. Report of two cases of adenoid cystic carcinoma of Bartholin’s gland and review of literature. Taiwan J Obstet Gynecol. 2013;52:113–116. https://www.ncbi.nlm.nih.gov/pubmed/23548230
- Kraemer B, Guengoer E, Solomayer EF, Wallwiener D, Hornung R. Stage I carcinoma of the Bartholin’s gland managed with the detection of inguinal and pelvic sentinel lymph node. Gynecol Oncol. 2009;114:373–374. https://www.ncbi.nlm.nih.gov/pubmed/19428095