What is phlegm
Phlegm is also called sputum, which is a thick mucus or viscous material that is derived from the lower respiratory tract such as the lungs and bronchi that is expelled and it is not the saliva that is produced by the glands in the mouth. Phlegm is produced by the lower respiratory tracts as a defense against infections or irritants. Phlegm (sputum) may contain substances such as mucus, blood, pus and/or bacteria. Sputum is not sterile. That means that when a person has a bacterial respiratory infection, there will typically be harmless bacteria that are normally present in the mouth, throat, etc. (normal flora) as well as disease-causing (pathogenic) bacteria present.
People whose lungs have become damaged through disease, exposure to toxins or chronic exposure to irritants, or from previous infections have an increased risk of recurrent infections.
With bacterial respiratory infections, the sputum may have a thick consistency (viscous), appear discolored – yellowish, greenish, grayish, or (rarely) rusty or bloody – and may have an unpleasant odor.
Sputum color is related to the degree of infection 1. Bacterial colonization has been demonstrated to be low (5%), moderate (43.5%), and very important (86.4%) in mucoid, mucopurulent, and purulent sputum, respectively 2. The purulence of sputum has also been associated with the bacterial load during exacerbations in subjects with chronic obstructive pulmonary disease (COPD) 3. However, the phlegm color can be difficult to evaluate, and when reported by patients, it is not reliable 4.
A trained laboratory scientist can differentiate normal harmless bacteria from pathogenic bacteria and identifies the various types of bacteria present in the culture. Identification is a step-by-step process that may involve several biochemical, immunological, and/or molecular tests and observations of the organism’s growth characteristics.
Antimicrobial susceptibility testing is frequently required to guide the treatment and to determine whether the bacteria present are likely to respond to specific antibiotics.
The sputum culture, Gram stain(s), and susceptibility testing all contribute to a report that informs the health practitioner which pathogen(s) are present and which antibiotic therapies are likely to inhibit their growth.
There is a pneumococcal vaccine that helps protect against invasive Streptococcus pneumoniae (pneumococcus) infections, the most common cause of bacterial pneumonia in adults. There is also a different pneumococcal vaccine for young children that protects them against serious infections with these bacteria, and there is a vaccine for infants to protect against serious infections by Haemophilus influenza type b.
A nagging cough or slight wheeze may barely register in the course of our busy days, but it’s critically important to pay attention to even mild symptoms. Sometimes people think having trouble breathing is just something that comes with getting older. It is important to pay attention to these symptoms as they could be the first signs of lung disease, including chronic obstructive pulmonary disease (COPD), asthma and lung cancer. Knowing the early warning signs of lung disease can help you receive treatment before the disease becomes serious or even life threatening. If you experience any of the following warning signs, make an appointment with your healthcare provider as soon as possible. Early detection could save your life.
Warning Signs
Chronic cough
A cough that you have had for a month or longer is considered chronic. This is an important early symptom that tells you something is wrong with your respiratory system.
Shortness of breath
It’s not normal to experience shortness of breath that doesn’t go away after exercising, or that you have after little or no exertion. Labored or difficult breathing—the feeling that it is hard to breathe in out—is also a warning sign.
Chronic phlegm production
Phlegm, also called sputum or mucus, is produced by the airways as a defense against infections or irritants. If your mucus production has lasted a month or longer, this could indicate lung disease.
Wheezing
Noisy breathing or wheezing is a sign that something unusual is blocking your lungs’ airways or making them too narrow.
Coughing up blood
If you are coughing up blood, it may be coming from your lungs or upper respiratory tract. Wherever it’s coming from, it signals a health problem.
Chronic chest pain
Unexplained chest pain that lasts for a month or more—especially if it gets worse when you breathe in or cough—also is a warning sign.
Human respiratory mucus
The air your breathe is full of dust, dirt, and air-borne microorganisms. To keep your lungs clear and healthy, this debris must be constantly swept out. To perform this task, the larger airways are lined by a relatively thick respiratory epithelium (Figure 2), which is the principal barrier protecting the lungs from the external environment. The human airway epithelium is comprised of three major cell types, basal cells, ciliated cells with cilia that beat and secretory cells (Goblet cells and Club cells) and a small number of endocrine cells, secreting serotonin and peptides that act as local mediators (Figure 3). These signal molecules affect nerve endings and other neighboring cells in the respiratory tract, so as to help regulate the rate of mucus secretion and ciliary beating, the contraction of surrounding smooth muscle cells that can constrict the airways, and other functions. Basal cells are also present, and serve as stem cells for renewal of the epithelium.
Airway mucus is a heterogeneous mixture of secreted polypeptides, cells, and cellular debris that are present in the airway surface lining fluid subphase or are tethered together at the fluid surface by oligomeric mucin complexes 5. Mucins are glycoproteins that due to their heavy glycosylation (∼ 75–90% carbohydrate by mass) can exhibit very high molecular weights (in the million Da range).
Where does phlegm come from
Goblet cells (so named because of their shape), together with submucosal glands are the principal secretors of MUC5AC and MUC5B mucin glycoproteins respectively 6. These gel-forming mucins form the glycoprotein component of airway mucus. MUC5AC and MUC5B form homotypic polymers (i.e., MUC5AC monomers bond only with MUC5AC, and MUC5B monomers bond only with MUC5B), structured as long single chains rather than branches . They form the mucus gel both by entanglement in a mesh and by noncovalent calcium-dependent cross-linking of adjacent polymers 7. The glycan side chains bind large amounts of liquid (hundreds of times their weight), which allows mucus to act as a lubricant and the gel layer to serve as a liquid reservoir for the periciliary layer 8. The hydration of mucus dramatically affects its viscous and elastic properties, which in turn determine how effectively it is cleared by ciliary action and cough 9. Healthy mucus contains 3% solids, with the consistency of egg white. However, mucin hypersecretion or dysregulation of surface liquid volume may increase the concentration of solids up to 15%, resulting in viscous and elastic mucus that is not easily cleared 10. In addition, dehydrated mucus adheres more readily to the airway wall 11. Pulmonary disease conditions, such as cystic fibrosis (CF), chronic obstructive pulmonary disorder (COPD), and asthma, generally result in an increase in the viscoelasticity of mucus, owing in part to reduced water content and an increased fraction of glycoproteins 12, 13.
The mucus secreted by the goblet cells forms a viscoelastic blanket about 5 μm thick over the tops of the cilia. The cilia, all beating in the same direction, at a rate of about 12 beats per second, sweep the mucus out of the lungs, carrying with it the debris that has become stuck to it. This conveyor belt for the removal of rubbish from the lungs is called the mucociliary escalator. Of course, some inhaled particles may reach the alveoli themselves, where there is no escalator. Here, the unwanted matter is removed by yet another class of specialized cells, macrophages, which roam the lungs and engulf foreign matter and kill and digest bacteria. Many millions of macrophages, loaded with debris, are swept out of the lungs every hour on the mucociliary escalator.
At the upper end of the respiratory tract, the wet mucus-covered respiratory epithelium gives way abruptly to stratified squamous epithelium. This cell sheet is structured for mechanical strength and protection, and, like epidermis, it consists of many layers of flattened cells densely packed with keratin. It differs from epidermis in that it is kept moist and its cells retain their nucleus even in the outermost layers. Abrupt boundaries of epithelial cell specialization, such as that between the mucous and the stratified squamous epithelium of the respiratory tract, are also found in other parts of the body, but very little is known about how they are created and maintained.
Goblet cell differentiation is believed to have evolved to combat parasitic infection and is an essential step for the clearance of inhaled pathogens from the airways 14. In healthy individuals, transient goblet cell differentiation results in an increase in goblet cell number at the affected areas of the epithelium, and temporarily upregulates mucus production. In contrast, chronic airways diseases, such as asthma, chronic obstructive pulmonary disease (COPD) and cystic fibrosis (CF), are characterized by a persistent goblet cell phenotype and continually high levels of secreted mucins 15. Over time this persistent mucin production is linked to intraluminal mucus accumulation, increased rates of infection and airway obstruction 16.
Figure 1. Mucus (biochemical features of gel-forming mucins)
Footnote: Major biochemical features of gel-forming mucins. (A) Several mucin monomers are shown linked together in an oligomeric gel. (B) Mucin monomers are crosslinked end-to-end via disulfide bonds between disulfide-rich domains (labeled “D”) near the amino- and carboxyl-termini 17. (C) Interspersed along each fiber are “naked” globular protein regions, with small exposed hydrophobic patches [198]. These regions are stabilized by multiple disulfide bonds. (D) Individual mucin fibers are densely glycosylated with O- and N-linked glycans, most of which are negatively charged with sialic acids or sulfate groups 17.
[Source 18 ]Figure 2. Respiratory epithelium
Footnote: The goblet cells secrete mucus, which forms a blanket over the tops of the ciliated cells. The regular, coordinated beating of the cilia sweeps the mucus up and out of the airways, carrying any debris that is stuck to it. The mechanism that coordinates the ciliary beating is a mystery, but it seems to reflect an intrinsic polarity in the epithelium. If a segment of rabbit trachea is surgically reversed, it carries on sweeping mucus, but in the wrong direction, back down toward the lung, in opposition to adjacent unreversed portions of trachea.
[Source 19 ]Figure 3. Human airway epithelium
Footnote: Normal vs diseased airway epithelium. In the normal airway epithelium (A) basal cells undergo regulated differentiation to form two major cell types, ciliated cells or secretory (Club and Goblet) cells. Goblet cells and submucosal glands are responsible for regulated mucus secretion into the airway which is normally present as a mucous bilayer. Club cells act to protect the airways through detoxification of harmful compounds and secretion of glycoproteins and lipids which physically protect surfactant and small airways. Mucocilliary clearance which is dependent on ciliary function actively moves mucus to remove foreign particles. In chronic airways disease (B) persistent goblet cell differentiation results in goblet cell hyperplasia. In addition to goblet cell differentiation, is the enlargement or hypertrophy of submucosal glands. These two events dramatically upregulate the production and secretion of mucin glycoproteins and result in a highly viscous and thickened mucus layer that is difficult to clear. This persistent goblet cell differentiation is directly linked to increased mucus accumulation in airways.
Abbreviation: MCVs = mucin containing vesicles.
[Source 20 ]Figure 4. Mucus clearance in normal airways
Footnote: Mucus is continuously swept from distal to proximal airways. In the most distal bronchioles, epithelial cells are cuboidal and do not produce mucin (bottom box), and bronchiolar patency is stabilized by surfactant from adjacent alveoli.8 In the adjacent small airways, a thin mucus gel layer is produced by columnar secretory (Clara) cells that do not stain for intracellular mucins because they are produced in low amounts and steadily secreted. In the large airways lined by a pseudostratified epithelium, a thick mucus gel layer (up to 50 µm) accumulates from mucus transported from distal airways and additional mucins are produced by surface secretory cells and glands. After mucus ascends the trachea, it is propelled through the vocal cords by ciliary epithelium in the posterior commissure of the larynx. It then enters the pharynx and is swallowed, with approximately 30 ml of airway mucus eliminated by the gastrointestinal tract daily. The vocal cords are covered by squamous epithelium, so they do not participate in ciliary clearance, although they promote cough clearance by closing while expiratory pressure builds and then opening suddenly so airflow is forceful.
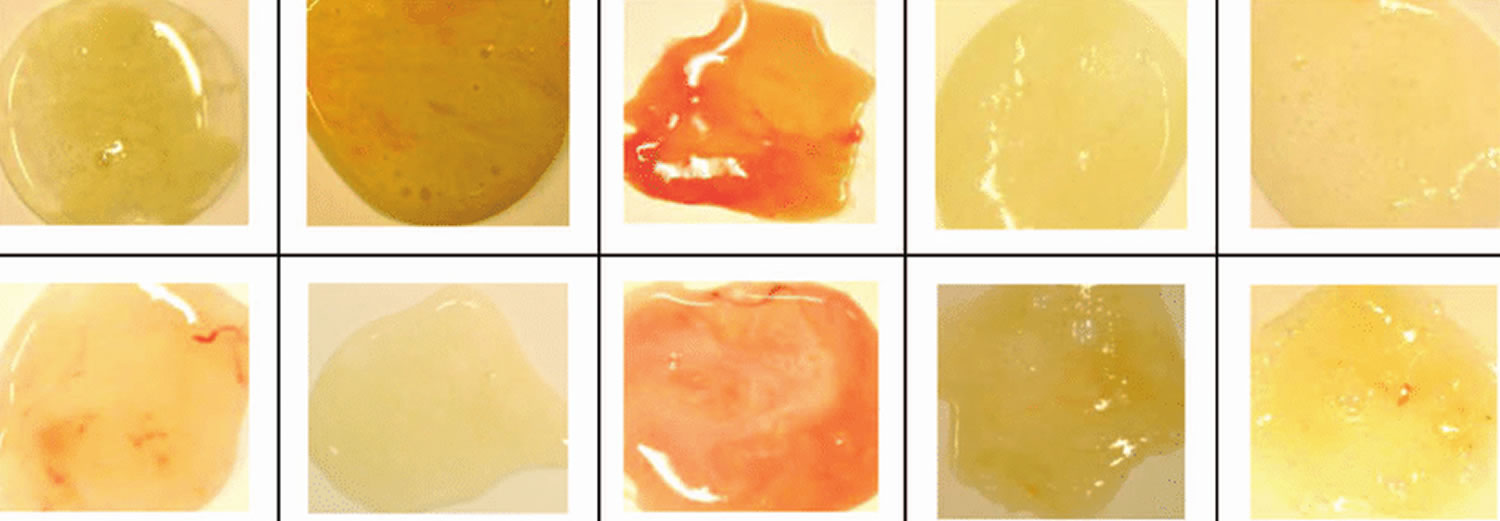
[Source 21 ]Phlegm color chart
Discolored sputum or phlegm is commonly interpreted by both patients and physicians as a clinical sign for the presence of bacterial infection 22. Thus in patients with acute respiratory infections yellowish and greenish phlegm as well as certain non-specific symptoms such as fatigue are strong predictors for antibiotic prescribing in primary care 23. In reality, purulence primarily occurs when inflammatory cells or sloughed mucosal epithelial cells are present, and it can result from either viral or bacterial infection 24. Robertson discovered in 1955 that green sputum color is caused by crystallized peroxidase. Since this enzyme is released by leukocytes (white blood cells) that are part of the general immune response, discolored sputum color can be due to a variety of causes. Therefore, yellowish or green sputum may be a normal feature in patients with viral bronchitis. Also, phlegm production in viral airway infections may be clear, white, or even tinged with blood 25. It has been shown that a yellowish or greenish phlegm color is often related to the bacterial load of patients suffering from COPD (chronic obstructive pulmonary disease) exacerbation 26 or patients hospitalized due to respiratory conditions 27. In otherwise healthy patients only indirect evidence showed that yellowish or greenish phlegm did not influence outcomes with or without antibiotic therapy 28. However, few studies have specifically examined the role of phlegm color in primary care patients without chronic respiratory diseases, although these patients are the most prevalent in general practice. In everyday practice only sputum samples of problematic patients will be sent in for microbiological investigation. In a recent study, Johnson et al. 24 examined such 289 consecutive outpatient samples sent in by primary care physicians, finding that the bacterial yield from phlegm colors green, yellow-green, yellow, and rust was higher than the yield from cream, white, or clear samples.
- Green or yellow phlegm. This shade is usually a sign that you have an infection of some kind, like a cold or the flu. The green color comes from a protein released from your inflammatory cells. It’s a toxic substance that kills germs trying to get in.
- Red or pink phlegm. If you’re sick and coughing a lot, you may notice blood-tinged sputum. This can come from broken blood vessels in your nose or throat. In some cases, it can also be a sign of cancer. Your doctor can do tests to find out the cause.
- Brown or black phlegm. Dark-colored phlegm can signal an infection. It’s also common in heavy smokers or people who are around smoke or coal dust at their job. This type of phlegm also shows up in people with chronic lung disease. The color comes from a mix of blood and inflammation in the lungs.
So far there has been no evidence that discolored sputum is correlated with a bacterial cause of acute respiratory infections in otherwise healthy adults. This study 29 investigates the correlation of discolored phlegm in patients with acute cough and a bacterial cause. The findings imply that the color of sputum or phlegm cannot be used to differentiate between viral and bacterial infections in otherwise healthy adults 29. The color of phlegm should not be used to make a decision on whether to prescribe an antibiotic within this group of patients.
In 28 samples (12%) a bacterial infection was proven. Yellowish or greenish color of the sputum sample and bacterial infection showed a significant correlation. The sensitivity of yellowish or greenish sputum used as a test for a bacterial infection was 0.79; the specificity was 0.46. The positive likelihood-ratio was 1.46.
Table 1. Sputum color and microbiological proof of bacterial infection
| Bacterial infection | No bacterial infection | Totals | |
| Yellowish or greenish sputum sample | 22 (16.2%) | 114 (83.8%) | 136 (100%) |
| Colorless sputum sample | 6 (5.7%) | 99 (94.3%) | 105 (100%) |
| Totals | 28 (11.6%) | 213 (88.4%) | 241 |
Conclusions
The sputum color or phlegm of patients with acute cough and no underlying chronic lung disease cannot be used in the consultation with otherwise healthy adult patients suffering from acute cough to differentiate between viral and bacterial infections. Thus it should not be used to make a decision on the choice of therapy and especially not on whether to prescribe an antibiotic 29.
Cough with phlegm
A cough with phlegm is your body’s way of responding when something irritates your throat or airways. An irritant stimulates nerves that send a message to your brain. The brain then tells muscles in your chest and abdomen to push air out of your lungs to force out the irritant.
An occasional cough is normal and healthy. A cough that persists for several weeks or one that brings up discolored or bloody mucus may indicate a condition that needs medical attention.
At times, coughing can be very forceful — the velocity of air from a vigorous cough can approach 500 miles an hour. Prolonged, vigorous coughing is exhausting and can cause sleeplessness, headaches, urinary incontinence and even broken ribs.
The prevalence of chronic cough and chronic phlegm, are important indicators of respiratory morbidity and mortality 30. These symptoms were associated with an accelerated decline in lung function 31, increased hospitalization 32 and an increased all cause of death 33. An important concern was the findings of a longitudinal study in 5,002 young adults aged 20 to 44 year by de Marco et al. 34 which followed the subjects for a median of 8.9 years for incident COPD (chronic obstructive pulmonary disease), which showed that a substantial number of young subjects with chronic cough and chronic phlegm developed COPD (chronic obstructive pulmonary disease) and that the presence of chronic cough and phlegm almost doubled the risk of COPD (chronic obstructive pulmonary disease) after adjusting for risk factors for this disease. In another longitudinal study by Lindberg et al. 35 respiratory symptoms were found to be significantly associated with incident COPD in both men and women.
Cough with phlegm causes
Some causes of cough with phlegm include:
Common causes — acute (lasts less than three weeks):
- Common cold
- Influenza (flu)
- Inhaling an irritant
- Pneumonia
- Whooping cough
Common causes — chronic (lasts longer than eight weeks or four weeks in children):
- Allergies
- Asthma (most common in children)
- Bronchitis (swelling and inflammation in the main passages that carry air to the lungs)
- Gastroesophageal reflux disease (GERD)
- Postnasal drip
Others causes cough with phlegm
- Acute sinusitis (sinus infection)
- Bronchiectasis (a chronic lung condition in which abnormal widening of bronchial tubes inhibits mucus clearing)
- Bronchiolitis (especially in young children)
- Choking: First aid (especially in children)
- Chronic sinusitis
- COPD (chronic obstructive pulmonary disease)
- Croup (especially in young children)
- Cystic fibrosis
- Emphysema
- Flare up of chronic obstructive pulmonary disease (COPD) or cystic fibrosis
- Heart failure
- Laryngitis
- Lung abscess (collection of pus in the lung)
- Lung cancer
- Medications called angiotensin-converting enzyme (ACE) inhibitors
- Neuromuscular diseases, such as parkinsonism, which weaken the coordination of upper airway and swallowing muscles
- Respiratory syncytial virus (RSV) — especially in young children
- Sarcoidosis
- Tuberculosis
The most common cause of bacterial pneumonia in adults in the U.S. is Streptococcus pneumoniae (pneumococcus).
Other common bacteria include:
- Staphylococcus aureus (staph)
- Haemophilus influenzae
- Moraxella catarrhalis
- Klebsiella pneumoniae
- Streptococcus pyogenes
A culture that is reported as “no growth in 24 or 48 hours” is usually considered negative. If pathogenic bacteria are not detected with a culture, then it may be that the person’s symptoms are due to a viral infection, or that the pathogen was not present in sufficient quantity in the sample collected. It may also be due to the fact that the microorganism responsible is not detectable with a routine bacterial culture.
Examples of organisms NOT detected with a routine bacterial culture of the sputum include:
- Mycoplasma pneumoniae and Chlamydia pneumonia—common in young adults
- Legionella species
- Mycobacterium tuberculosis (tuberculosis; see AFB Testing)
- Pneumocystis jiroveci—a fungus that can be seen in those who have had organ transplants or who have HIV/AIDS
- Other fungi (see Fungal Tests)
- Viruses
- Rarely, a parasitic infection may also cause symptoms of a lower respiratory infection.
See your doctor if your cough doesn’t go away after several weeks or if you or your child is:
- Coughing up thick, greenish-yellow phlegm
- Wheezing
- Experiencing a fever more than 100 °F (38 °C)
- Experiencing shortness of breath
Seek emergency care if you or your child is:
- Choking
- Having difficulty breathing or swallowing
- Coughing up bloody or pink-tinged phlegm
Coughing up blood in phlegm
Coughing up blood can be alarming, but isn’t usually a sign of a serious problem if you’re young and otherwise healthy. The medical term for coughing up blood is hemoptysis. Blood in phlegm is more a cause for concern in older people, particularly those who smoke. Don’t self diagnose yourself. Always leave that to a doctor.
You may cough up small amounts of bright red blood, or frothy blood-streaked sputum (phlegm). The blood is usually from your lungs and is often the result of prolonged coughing or a chest infection.
If the blood is dark and contains bits of food or what look like coffee grounds, it may be coming from your digestive system. This is a more serious problem and you should go to hospital straight away.
Common causes of coughing up blood
The most common reasons for coughing up blood are:
- a prolonged, severe cough
- a chest infection – this is more likely if your sputum is discolored or contains pus, you have a fever, or you have a tight feeling in your chest
- bronchiectasis – this is more likely if you’re also wheezy or short of breath
Sometimes a severe nosebleed or bleeding from the mouth or throat can cause blood to come out in your saliva when you cough.
Less common causes of coughing up blood
Less commonly, coughing up blood may be the result of:
- pulmonary embolism (a blood clot in the lungs) – this usually causes sudden shortness of breath and chest pain
- pulmonary edema (fluid in the lungs) – your sputum will be pink and frothy, and this usually occurs in people with pre-existing heart problems
- lung cancer – this is more likely if you’re over 40 and smoke
- tuberculosis (TB) – a severe lung infection associated with fever and sweating; this is becoming more common in the US, but can be treated with prolonged antibiotics
- cancer of the throat or windpipe
- taking anticoagulants – medications that help stop your blood clotting, such as warfarin, rivaroxaban, or dabigatran
Sometimes, no cause can be found and it never happens again.
What to do if you cough up blood
Call your doctor as soon as possible if you cough up blood, even if it’s just a few spots or specks.
Your doctor will check if you might have a serious medical condition that needs to be investigated and treated.
Call your local emergency services number for an ambulance or go to your nearest accident and emergency (A&E) department immediately if you’re coughing up a lot of blood or are struggling to breathe.
Cough with phlegm diagnosis
As with any illness, a full and detailed medical history accompanied with an appropriate physical exam is the most important aspect of any medical evaluation. Diagnosis of a cough with phlegm is an obvious, clinical observation. A cough with phlegm is a symptom, rather than a diagnosis of disease. As such, many patients present for evaluation of the secondary or underlying effects of a cough rather than a cough itself. Essential components of the history taking session should include:
- Details about duration
- Cigarette smoking
- Use of angiotensin-converting enzyme (ACE) inhibitors
- Weight loss
- Occupation
- Diurnal variation
- Relieving factors
- Aggravating factors
- Productive with sputum or nonproductive, if productive, what is color of phlegm
- Associated hemoptysis (blood in phlegm)
- Associated fever
- Associated shortness of breath
- Presence of an upper respiratory tract infection at the onset of a cough
Your doctor may decide to refer you to a specialist at your local hospital for a chest X-ray or a more detailed scan, such as a computerized tomography (CT) scan.
Cat scan or CT scan, is a diagnostic test that uses a series of computerized views taken from different angles to create detailed internal pictures of your body. CT Scan-Guided Lung Biopsy: Radiologists use a CT scan-guided lung biopsy to guide a needle through the chest wall and into the lung nodule to obtain and examine tissue.
You may be asked for a sample of your sputum so it can be checked for infection. Other tests, such as blood tests, may also be needed.
In some cases, further tests may be required to find out where the blood is coming from. For example, you may be referred to a specialist who may decide to arrange a test called a bronchoscopy.
- Bronchoscopy is a technique used to look at your air passages with a small camera that is located at the end of a flexible tube.
- Endobronchial Ultrasound (EBUS): Endobronchial ultrasound bronchoscopy is a procedure used to diagnose different types of lung disorders, including inflammation, infections or cancer.
- Exhaled Nitric Oxide Test: An exhaled nitric oxide level test can help diagnose and manage asthma.
- Lung function tests (or pulmonary function tests) include a variety of tests that check how well the lungs work.
- Spirometry is the most common type of pulmonary function or breathing test that measures how much air you can breathe in and out of your lungs.
- Methacholine challenge test (also known as bronchoprovocation test) is performed to evaluate how “reactive” or “responsive” your lungs are to things in the environment.
How to get rid of phlegm
The development of rationally designed treatments for pathologic phlegm has been hindered by a lack of understanding of the mechanisms of mucus dysfunction. Over-the-counter medications for airway mucus dysfunction, including guaifenesin, have not been rigorously evaluated in clinical trials, and they are not recommended in treatment guidelines for cystic fibrosis, asthma, or chronic obstructive pulmonary disease (COPD) 36. Multiple additional agents with uncertain mechanisms are used worldwide without clear evidence of a benefit 37, 38. Asthma, chronic obstructive pulmonary disease (COPD), and cystic fibrosis (CF) have important differences in pathologic mucus, and mucus treatment should be tailored accordingly. Current therapies do this to an extent, but they may be facilitated by therapies that are currently under development. Therapies can be subdivided into those that decrease mucin production, those that decrease mucin secretion, those that promote mucus clearance, and those that treat airway infection (Table 1).
Recent insights into the formation of pathologic mucus in disease have led to the introduction of tailored therapies such as hydration by means of aerosolized hypertonic saline solutions or the reduction of mucus viscosity and elasticity by aerosolized dornase alfa 21. Targeted treatment of pathologic airway mucus not only improves symptoms of cough and dyspnea but also decreases the frequency of disease-related exacerbations and slows disease progression. Elucidation of how mucin production is controlled is still needed, since that might allow the development of additional therapies to prevent overproduction 21.
Table 2. Treatment of Mucus Hypersecretion
| Purpose and treatment | Comments |
|---|---|
| Decrease mucin production | |
| Available treatments | |
| Glucocorticoids | Allergen-induced increases in numbers of airway goblet cells are inhibited by glucocorticoids. In acute severe asthma, glucocorticoids may also reduce bronchovascular permeability and promote neutrophildriven mucus turnover. Glucocorticoids are much less effective in treating mucus in other airway diseases. |
| Agents in development | |
| ErbB-receptor inhibitors | A recent trial of inhaled BIBW 2948 BS, an epidermal growth factor receptor inhibitor (ClinicalTrials.gov number, NCT00423137), did not show a benefit in reducing airway mucin gene expression or epithelial mucin stores in patients with COPD, and the treatment was associated with adverse effects on lung and liver function. |
| Decrease mucin secretion | |
| Available treatments | |
| None | |
| Agents in development | |
| MARCKS inhibitors | MARCKS regulates the reconfiguration of actin filaments at the apical pole of goblet cells during mucin secretion. A peptide derived from the MARCKS N-terminal that is myristoylated so that it enters cells inhibits stimulated mucin secretion in mice. In a phase 2 trial (NCT00648245), this peptide is being administered by aerosol in patients with COPD who have mucus hypersecretion. |
| Botulinum neurotoxins | Botulinum neurotoxins are zinc proteases that cleave SNARE proteins to inhibit release of synaptic vesicles. The C and E neurotoxins have been engineered so that they are active against non-neuronal SNARE isoforms, inhibiting epithelial-cell mucin secretion, and the modified C toxin has been conjugated to epidermal growth factor to promote delivery to goblet cells, but no related clinical trial has been registered. |
| Promote phlegm clearance | |
| Available treatments | |
| Physical measures | Chest percussion and postural drainage improve clearance of purulent airway mucus in cystic fibrosis. The value of alternative methods, including positive expiratory pressure, flutter valves, or high-frequency chest-compression vests, is difficult to assess objectively, although trials are in progress (e.g., NCT01057524). Mucus clearance is probably aided by any maneuver that promotes coughing and increased minute ventilation, including exercise. Since airflow generates shear stress on airway cell surfaces that stimulate release of nucleotides that interact with P2Y2 receptors to regulate mucus hydration, there are both mechanical and biochemical mechanisms of benefit from nonpharmacologic approaches to mucus clearance. |
| Bronchodilators | Bronchodilation with beta-adrenergic agonists or anticholinergic drugs may improve mucus clearance in the short term because of an enlarged luminal diameter. In addition, beta-adrenergic agonists increase the frequency of ciliary beats, and anticholinergic drugs may decrease surface mucin secretion and mucin secretion from the submucosal gland. However, beta-adrenergic agonists up-regulate mucin production in animal models, so they are not recommended for long-term treatment of mucus hypersecretion. The long-term effects of both classes of bronchodilators on mucus clearance warrant further study. |
| Inhaled dornase alfa | Inhaled dornase alfa hydrolyzes DNA, improves lung function, and decreases the frequency of exacerbation in patients with cystic fibrosis, in whom airway mucus concentrations of DNA are very high (5–10 mg/ml). The concentration of DNA in other airway diseases, including non−cystic fibrosis bronchiectasis, COPD, and asthma, is 1/5 to 1/10 as great; dornase alfa does not have beneficial effects in these diseases and may even be harmful. |
| Inhaled hypertonic saline | Treatment twice daily with aerosolized 7% hypertonic saline solution is associated with significant improvements in mucus clearance, modest improvements in airflow, and clinically meaningful reductions in rates of exacerbation among patients with cystic fibrosis. The mechanism of benefit is thought to be rehydration of the periciliary layer through the drawing of water from epithelial cells, but other mechanisms such as promotion of cough and direct effects on mucus elasticity and entanglement may also contribute. Trials are under way for the treatment of other airway diseases with 3 to 7% hypertonic saline; these diseases include infantile bronchiolitis (NCT01016249, NCT00677729, NCT00729274, NCT00619918, NCT00151905, and NCT00696540), COPD (NCT00639236), atelectasis (NCT00671723), non−cystic fibrosis bronchiectasis (NCT00484263), and asthma (NCT01073527). |
| N-acetylcysteine | N-acetylcysteine breaks the disulfide bonds that link mucin monomers to polymers, and it is very effective in vitro in solubilizing sputum. Case reports attest to its usefulness when applied through the bronchoscope to break up mucus plugs. Clinical studies of N-acetylcysteine and carbocysteine in COPD have shown some promise. Aerosolized N-acetylcysteine also can be irritating to the airway, so its routine use is not recommended. Oral N-acetylcysteine is under study as an antiinflammatory (glutathione-replenishing and antioxidant) treatment in cystic fibrosis and COPD (NCT00969904 and NCT00809094). |
| Agents in development | |
| Mannitol | Nonabsorbable osmotic agents have a theoretical advantage of drawing liquid into the periciliary layer for longer periods than sodium chloride. Inhaled mannitol is undergoing safety and efficacy testing in cystic fibrosis, COPD, and bronchiectasis (NCT00446680, NCT00117208, and NCT00669331). Its use in children with cystic fibrosis is associated with bronchoconstriction and cough, but a 3-month treatment protocol showed similar efficacy to that of dornase alfa. |
| P2Y2 agonists | P2Y2 agonists promote the activity of calcium-activated chloride channels and inhibit the activity of epithelial sodium channels, so they may normalize the height of the periciliary layer and improve mucus clearance, especially in cystic fibrosis. Phase 2 and 3 trials of denufusol in cystic fibrosis are ongoing (NCT00625612 and NCT00357279). |
| CFTR modulation | Several therapeutic agents are in development to augment the function of mutant CFTR, including ataluren to promote read-through of premature termination codons (NCT00803205), VX-809 to promote transport of misfolded CFTR protein to the cell surface (NCT00865904 and NCT00966602), and VX-770 to promote the opening of CFTR proteins expressed on the cell surface (NCT00909532 and NCT00966602). |
| Epithelial sodium-channel modulation | An aerosolized inhibitor of epithelial sodium-channel function, GS-9411, is being evaluated as a potential therapy to improve airway hydration and mucociliary clearance in cystic fibrosis (NCT00800579, NCT009999531, NCT01025713, and NCT00951522). |
| Actin filament depolymerizing agents, proteases, and antiproteases | Gelsolin and thymosin β4 depolymerize actin filaments, which could be helpful in promoting mucus clearance in cystic fibrosis; however, the results of clinical studies of recombinant human plasma gelsolin in cystic fibrosis in the 1990s were not promising, and no trials are currently registered. Proteases that digest gel-forming mucins could be helpful in treating mucus plugs in severe asthma, although no trials are yet under way. Inhaled alpha1-antitrypsin is being studied to prevent lung parenchymal damage from leukocyte proteases in cystic fibrosis (NCT00499837). |
| Treat airway infection | |
| Available treatments | |
| Inhaled antibiotics | Treatment with inhaled tobramycin is associated with improved lung function and reduced exacerbation frequency in patients with cystic fibrosis. |
| Oral antibiotics | Prolonged use of azithromycin improves lung function in cystic fibrosis, although it is associated with increased nausea and diarrhea. Long-term treatment with oral erythromycin reduces the frequency of exacerbation in COPD and several groups, including the COPD Clinical Research Network (NCT00119860), are studying azithromycin in patients with this condition. The value of oral antibiotics in the short-term treatment of COPD exacerbations is questionable. In patients with bronchiectasis who do not have cystic fibrosis, long-term treatment with low-dose azithromycin reduces the frequency of exacerbation and improves lung function. |
| Intravenous antibiotics | Intravenous antibiotics directed against pseudomonas species infections are effective in the treatment of pulmonary exacerbations of cystic fibrosis. |
| Agents in development | |
| Inhaled antibiotics | Inhaled aztreonam reduced the time to exacerbation in cystic fibrosis in two phase 3 studies (NCT00112359, NCT00104520), and a study comparing inhaled aztreonam with inhaled tobramycin in cystic fibrosis is ongoing (NCT00757237). Also under study are inhaled ciprofloxacin (NCT00645788), liposomal amikacin (NCT00558844), and tobramycin combined with fosfomycin (NCT00794586). |
Abbreviations: *CFTR = cystic fibrosis transmembrane conductance regulator; COPD = chronic obstructive pulmonary disease; MARCKS = myristoylated alanine-rich C-kinase substrate; SNARE = soluble N-ethylmaleimide–sensitive factor attachment protein receptor.
[Source 21 ]Home remedies
There are things you can try at home to relieve your symptoms, such as:
- avoiding things that trigger your symptoms, such as allergens or smoky places
- taking sips of cold water when you feel the need to clear your throat – constantly clearing your throat may make things worse
- using a saline nasal rinse several times a day – these can be bought from a pharmacy or made at home with half a teaspoon of salt in a pint of boiled water that’s been left to cool
- avoiding warm, dry atmospheres, such as places with air conditioning and car heating systems – placing plants or bowls of water in a room may help to keep the air humid
- staying well hydrated
- talking to a pharmacist about suitable over-the-counter medications – including decongestants, antihistamines or steroid nasal sprays
Techniques to bring up phlegm
People with chronic obstructive pulmonary disease (COPD) and chronic bronchitis often produce a large amount of phlegm. If the phlegm is allowed to collect in the airways, breathing may become difficult, and infection may occur. Techniques to remove phlegm are often done after using an inhaled bronchodilator medication. The medication helps loosen the mucus and open the airways to make the techniques more effective. Common techniques used to help remove phlegm include these, which can be ordered and demonstrated by your doctor.
Deep Coughing
Start by taking a deep breath. Hold the breath for 2-3 seconds. Use your stomach muscles to forcefully expel the air. Avoid a hacking cough or merely clearing the throat. A deep cough is less tiring and more effective in clearing mucus out of the lungs.
Huff Coughing
Huff coughing, or huffing, is an alternative to deep coughing if you have trouble clearing your mucus. Take a breath that is slightly deeper than normal. Use your stomach muscles to make a series of three rapid exhalations with the airway open, making a “ha, ha, ha” sound. Follow this by controlled diaphragmatic breathing and a deep cough if you feel mucus moving.
Other Techniques
If you produce a large amount of phlegm, your health care provider may recommend other techniques to help clear the phlegm.
- Devices such as the Acapella® or Aerobika® are small devices into which you exhale.
- Postural drainage is a technique that uses gravity to promote drainage of mucus from the lungs.
- Each technique can be ordered and demonstrated by your health care provider. Ask your health care provider if this may be helpful for you.
Exercise is also a good way to help bring up mucus in the lungs.
References- Reychler, Gregory & André, Emmanuel & Couturiaux, Laurence & Hohenwarter, Kinga & Liistro, Giuseppe & Pieters, Thierry & Robert, Annie. (2016). Reproducibility of the Sputum Color Evaluation Depends on the Category of Caregivers. Respiratory Care. 61. 10.4187/respcare.04547.
- Murray MP, Pentland JL, Turnbull K, MacQuarrie S, Hill AT. Sputum colour: a useful clinical tool in non-cystic fibrosis bronchiectasis. Eur Respir J 2009;34(2):361-364.
- Stockley RA, O’Brien C, Pye A, Hill SL. Relationship of sputum color to nature and outpatient management of acute exacerbations of COPD. Chest 2000;117(6):1638-1645.
- DanielsJM,de GraaffCS,Vlaspolder F, Snijders D, JansenHM,Boersma WG. Sputum colour reported by patients is not a reliable marker of the presence of bacteria in acute exacerbations of chronic obstructive pulmonary disease. Clin Microbiol Infect 2010;16(6):583-588.
- Williams OW, Sharafkhaneh A, Kim V, Dickey BF, Evans CM. Airway mucus: From production to secretion. Am J Respir Cell Mol Biol. 2006;34(5):527-36. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2644218/
- Hovenberg, H. W., Davies, J. R., & Carlstedt, I. (1996). Different mucins are produced by the surface epithelium and the submucosa in human trachea: Identification of MUC5AC as a major mucin from the goblet cells. Biochemical Journal, 318(Pt 1), 319–324.
- Thornton DJ, Rousseau K, McGuckin MA. Structure and function of the polymeric mucins in airways mucus. Annu Rev Physiol. 2008;70:459–486.
- Knowles MR, Boucher RC. Mucus clearance as a primary innate defense mechanism for mammalian airways. J Clin Invest. 2002;109:571–577
- Cone RA. Barrier properties of mucus. Adv Drug Deliv Rev. 2009;61:75–85.
- Lai SK, Wang YY, Wirtz D, Hanes J. Micro- and macrorheology of mucus. Adv Drug Deliv Rev. 2009;61:86–100.
- Rubin BK. Mucus and mucins. Otolaryngol Clin North Am. 2010;43:27–34.
- Rubin BK. Mucus structure and properties in cystic fibrosis. Paediatr Respir Rev. 2007;8:4–7.
- Voynow JA, Gendler SJ, Rose MC. Regulation of mucin genes in chronic inflammatory airway diseases. Am J Respir Cell Mol Biol. 2006;34:661–665.
- Evans, C. M., Kim, K., Tuvim, M. J., & Dickey, B. F. (2009). Mucus hypersecretion in asthma: Causes and effects. Current Opinion in Pulmonary Medicine, 15, 4–11.
- McCullagh, C. M., Jamieson, A. M., Blackwell, J., & Gupta, R. (1995). Viscoelastic properties of human tracheobronchial mucin in aqueous solution. Biopolymers, 35, 149–159.
- Rose, M. C., & Voynow, J. A. (2006). Respiratory tract mucin genes and mucin glycoproteins in health and disease. Physiological Reviews, 86, 245–278.
- Van Klinken BJ, Dekker J, Buller HA, Einerhand AW. Mucin gene structure and expression: protection vs. adhesion. Am J Physiol. 1995;269:G613–G627.
- Cone R. Mucus. In: Michael WS, Lamm E, McGhee Jerry R, Mayer Lloyd, Mestecky Jiri, Bienenstock John, editors. Mucosal Immunlogy. San Diego: Academic Press; 1999. pp. 43–64.
- Alberts B, Johnson A, Lewis J, et al. Molecular Biology of the Cell. 4th edition. New York: Garland Science; 2002. The Airways and the Gut. Available from: https://www.ncbi.nlm.nih.gov/books/NBK26875/
- Persistent induction of goblet cell differentiation in the airways: Therapeutic approaches. Reid, A.T., Pharmacology and Therapeutics (2017), https://doi.org/10.1016/j.pharmthera.2017.12.009
- Fahy JV, Dickey BF. Airway mucus function and dysfunction. N Engl J Med. 2010;363(23):2233-47. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4048736/
- Wilm S, Knauf A, Kreilkamp R, Schlegel U, Altiner A. The doctor, his patient and the sputum. Z Allg Med. 2006;82:260–67.
- Cals JW, Boumans D, Lardinois RJ, Gonzales R, Hopstaken RM, Butler CC, et al. Public beliefs on antibiotics and respiratory tract infections: An internet-based questionnaire study. Br J Gen Pract. 2007;57:942–7.
- Johnson AL, Hampson DF, Hampson NB. Sputum color: Potential implications for clinical practice. 2008;53:450–4. http://rc.rcjournal.com/content/53/4/450/tab-pdf
- Knutson D, Braun C. Diagnosis and management of acute bronchitis. Am Fam Physician. 2002;65:2039–44.
- Allegra L, Blasi F, Diano P, Cosentini R, Tarsia P, Confalonieri M, et al. Sputum color as a marker of acute bacterial exacerbations of chronic obstructive pulmonary disease. Respir Med. 2005;99:742–7.
- Flournoy DJ, Davidson LJ. Sputum quality: Can you tell by looking? Am J Infect Control. 1993;21:64–9.
- Stott NC, West RR. Randomised controlled trial of antibiotics in patients with cough and purulent sputum. BMJ. 1976;4:556–9
- Altiner A, Wilm S, Däubener W, et al. Sputum colour for diagnosis of a bacterial infection in patients with acute cough. Scand J Prim Health Care. 2009;27(2):70-3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3410464/
- Mahesh PA, Jayaraj BS, Prabhakar AK, Chaya SK, Vijayasimha R. Prevalence of chronic cough, chronic phlegm & associated factors in Mysore, Karnataka, India. Indian J Med Res. 2011;134(1):91-100. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3171924
- Sherman CB, Xu X, Speizer FE, Ferris BG, Jr, Weiss ST, Dockery DW. Longitudinal lung function decline in subjects with respiratory symptoms. Am Rev Respir Dis. 1992;146:855–9.
- Vestbo J, Prescott E, Lange P. Association of chronic mucus hypersecretion with FEV1 decline and chronic obstructive pulmonary disease morbidity. Copenhagen City Heart Study Group. Am J Respir Crit Care Med. 1996;153:1530–5.
- Lange P, Nyboe J, Appleyard M, Jensen G, Schnohr P. Relation of ventilatory impairment and of chronic mucus hypersecretion to mortality from obstructive lung disease and from all causes. Thorax. 1990;45:579–85.
- de Marco R, Accordini S, Cerveri I, Corsico A, Anto JM, Kunzli N, et al. Incidence of chronic obstructive pulmonary disease in a cohort of young adults according to the presence of chronic cough and phlegm. Am J Respir Crit Care Med. 2007;175:32–9.
- Lindberg A, Jonsson AC, Ronmark E, Lundgren R, Larsson LG, Lundback B. Ten-year cumulative incidence of COPD and risk factors for incident disease in a symptomatic cohort. Chest. 2005;127:1544–52.
- Flume PA, Mogayzel PJ, Jr, Robinson KA, et al. Cystic fibrosis pulmonary guidelines: treatment of pulmonary exacerbations. Am J Respir Crit Care Med. 2009;180:802–808.
- Rogers DF. Mucoactive agents for airway mucus hypersecretory diseases. Respir Care. 2007;52:1176–1193.
- Boogaard R, de Jongste JC, Merkus PJ. Pharmacotherapy of impaired mucociliary clearance in non-CF pediatric lung disease: a review of the literature. Pediatr Pulmonol. 2007;42:989–1001.