What is calcaneus
Calcaneus or heel bone, is one of seven tarsal bones that forms the heel of the foot. The weight of the body is carried primarily by the two largest tarsal bones, the talus, which articulates with the tibia and fibula superiorly, the strong calcaneus, which forms the heel of the foot. The tibia articulates with the talus at the trochlea of the talus. The ankle joint is a hinge joint between the united inferior ends of the tibia and fibula and the talus of the foot. Inferiorly, the talus articulates with the calcaneus. The subtalar or calcaneotalar joint accounts for at least some foot and ankle dorsal/plantar flexion. The thick tendon of the calf muscles attaches to the posterior surface of the calcaneus. The part of the calcaneus that touches the ground is the calcaneal tuberosity, and the medial, shelf like projection is the sustentaculum tali (supporter of the talus) or talar shelf. Calcaneus anatomy is demonstrated in Figures 1 to 3.
The calcaneus is surrounded by and receives its blood supply from a superficial network of arteries called the calcaneal anastomosis, which is formed by branches of the posterior tibial and fibular arteries. Much of the lymphatic flow follows the vasculature and flows up the leg through the popliteal and inguinal lymph nodes before passing through the thoracic duct 1.
The calcaneus receives its nerve supply from branches of the tibial and sural nerves 2.
Plantar fasciitis or painful heel syndrome is an inflammatory reaction due to chronic irritation of the plantar aponeurosis (fascia) at its origin on the calcaneus (heel bone). Plantar fasciitis is also related to weight bearing activities (walking, jogging, lifting heavy objects), improperly constructed or fitting shoes, excess weight (which puts pressure on the feet), and poor biomechanics (flat feet, high arches, and abnormalities in gait that may cause uneven distribution of weight on the feet). Plantar fasciitis is the most common cause of heel pain in runners and arises in response to the repeated impact of running. Treatments include ice, deep heat, stretching exercises, weight loss, prosthetics (such as shoe inserts or heel lift s), steroid injections, and surgery.
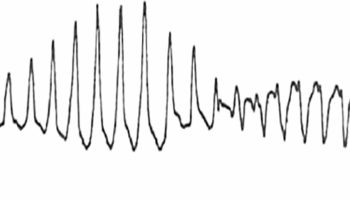
Figure 1. Foot bone anatomy
Figure 2. Calcaneus bone anatomy (right foot)
Calcaneus function
The calcaneus serves as an attachment point for the tendocalcaneous (Achilles) tendon which produces aids in plantar flexion of the foot vital for standing, walking, running, and jumping 3. The calcaneus also serves as an attachment point for muscles that move the toes. The calcaneus and the talus make up the subtalar joint or the talocalcaneal joint which allows for inversion, eversion, dorsiflexion, and plantarflexion of the foot. The calcaneus has a number of joint stabilizing ligaments attached to it, such as the calcaneofibular, talocalcaneal, calcaneocuboid, and calcaneonavicular ligaments. The plantar aponeurosis and long plantar ligament support the arch of the foot and attach to the calcaneus as well 1.
There are 3 muscles that combine to form the Achilles tendon and attach on the calcaneal tubercle. These muscles are the primary plantar flexors and consist of the gastrocnemius, soleus, and plantaris. There are 6 muscles that originate on portions of the calcaneus and provide movement to the toes. The extensor digitorum brevis originates on the dorsal side of the calcaneus and provides extension of the 2 to 4 digits. The abductor hallucis originates on the medial process of calcaneal tuberosity and abducts the first digit. The extensor hallucis brevis originates on the dorsal aspect of the calcaneus and extends the first digit. The abductor digiti minimi originates on the calcaneal tubercle and provides flexion and extension of the fifth toe. The flexor digitorum brevis originates on the calcaneal tubercle and helps provide flexion to the 2 to 4 digits. The quadratus plantae originates on the lateral and medial processes of the calcaneus and helps provide flexion at the distal interphalangeal (DIP) joint 4.
Calcaneus pain
Every mile you walk puts 60 tons of stress on each foot. Your feet can handle a heavy load, but too much stress pushes them over their limits. When you pound your feet on hard surfaces playing sports or wear shoes that irritate sensitive tissues, you may develop heel pain, the most common problem affecting the foot and ankle.
A sore heel will usually get better on its own without surgery if you give it enough rest. However, many people try to ignore the early signs of heel pain and keep on doing the activities that caused it. When you continue to use a sore heel, it will only get worse and could become a chronic condition leading to more problems. Surgery is rarely necessary.
Calcaneus pain causes
Pain Beneath the Heel
If it hurts under your heel, you may have one or more conditions that inflame the tissues on the bottom of your foot:
- Stone bruise. When you step on a hard object such as a rock or stone, you can bruise the fat pad on the underside of your heel. It may or may not look discolored. The pain goes away gradually with rest.
- Plantar fasciitis (subcalcaneal pain). Doing too much running or jumping can inflame the tissue band (fascia) connecting the heel bone to the base of the toes. The pain is centered under your heel and may be mild at first but flares up when you take your first steps after resting overnight. You may need to do special exercises, take medication to reduce swelling and wear a heel pad in your shoe.
- Heel spur. When plantar fasciitis continues for a long time, a heel spur (calcium deposit) may form where the fascia tissue band connects to your heel bone. Your doctor may take an X-ray to see the bony protrusion, which can vary in size. Treatment is usually the same as for plantar fasciitis: rest until the pain subsides, do special stretching exercises and wear heel pad shoe inserts.
Pain Behind the Heel
If you have pain behind your heel, you may have inflamed the area where the Achilles tendon inserts into the heel bone (retrocalcaneal bursitis). People often get this by running too much or wearing shoes that rub or cut into the back of the heel. Pain behind the heel may build slowly over time, causing the skin to thicken, get red and swell. You might develop a bump on the back of your heel that feels tender and warm to the touch. The pain flares up when you first start an activity after resting. It often hurts too much to wear normal shoes. You may need an X-ray to see if you also have a bone spur.
Treatment includes resting from the activities that caused the problem, doing certain stretching exercises, using pain medication and wearing open back shoes.
- Your doctor may want you to use a 3/8″ or 1/2″ heel insert.
- Stretch your Achilles tendon by leaning forward against a wall with your foot flat on the floor and heel elevated with the insert.
- Use nonsteroidal anti-inflammatory medications for pain and swelling.
- Consider placing ice on the back of the heel to reduce inflammation.
Calcaneus pain diagnosis
Heel pain can have many causes. If your heel hurts, see your doctor right away to determine why and get treatment. Tell him or her exactly where you have pain and how long you’ve had it.
Your doctor will examine your heel, looking and feeling for signs of tenderness and swelling. You may be asked to walk, stand on one foot or do other physical tests that help your doctor pinpoint the cause of your sore heel.
Calcaneus pain treatment
Conditions that cause heel pain generally fall into two main categories: pain beneath the heel and pain behind the heel.
Plantar fasciitis
Plantar fasciitis is one of the most common causes of heel pain or calcaneus pain. Plantar fasciitis involves inflammation of a thick band of tissue that runs across the bottom of your foot and connects your heel bone to your toes called the plantar fascia. The plantar fascia is a thick strong band of tissue on the bottom of the foot. It begins at the calcaneus and spreads out to insert onto the phalanges (toe bones).
Plantar fasciitis commonly causes stabbing pain that usually occurs with your first steps in the morning. As you get up and move more, the pain normally decreases, but it might return after long periods of standing or after rising from sitting.
Plantar fasciitis is more common in runners. In addition, people who are overweight and those who wear shoes with inadequate support have an increased risk of plantar fasciitis.
The inflammation at this site sometimes triggers excessive growth of the bone leading to the formation of a bony spur on the heel.
The swollen fascia may also cause a nerve entrapment syndrome, resulting in pins and needles or reduced sensation over the foot. For this reason, it is important that you tell your doctor about any changes in sensation or strength in your foot.
Plantar fasciitis is more common in ladies who are older than 40 and are overweight.
Plantar fasciitis causes
Under normal circumstances, your plantar fascia acts like a shock-absorbing bowstring, supporting the arch in your foot. If tension and stress on that bowstring become too great, small tears can arise in the fascia. Repetitive stretching and tearing can cause the fascia to become irritated or inflamed, though in many cases of plantar fasciitis, the cause isn’t clear.
There are many possible causes of plantar fasciitis, including:
- Abnormal foot arches. If the arches of your foot are unusually high or low (eg flatfoot), you are more likely to develop plantar fasciitis than if your arches are normal.
- Wearing high heels. Wearing high-heeled shoes for long periods of time is one possible cause. If you wear high-heeled shoes, including western-style boots, the fascia can become shorter. Pain then occurs when you stretch fascia that has shortened. This painful stretching might happen, for example, when you walk barefoot after getting out of bed in the morning.
- Weight. If you gain weight, you might be more likely to have plantar fasciitis, especially if you walk a lot or stand in shoes with poor heel cushioning.
- Activities. Increased walking, standing, or stair-climbing can lead to plantar fasciitis. Runners may get plantar fasciitis when they change their workout and increase their mileage or frequency of workouts. It can also happen with a change in exercise surface or terrain, or if your shoes are worn out and don’t provide enough cushion for your heels.
- Tight Achilles tendons
- Abnormal walking patterns. Many people who have had previous injuries in their foot, hips or knees unconcsiously develop a different way of walking to adapt to their injury. This may be very subtle, and increases their risk of developing further injuries.
Risk factors for plantar fasciitis
Though plantar fasciitis can arise without an obvious cause, factors that can increase your risk of developing plantar fasciitis include:
- Age. Plantar fasciitis is most common between the ages of 40 and 60.
- Certain types of exercise. Activities that place a lot of stress on your heel and attached tissue — such as long-distance running, ballistic jumping activities, ballet dancing and aerobic dance — can contribute to an earlier onset of plantar fasciitis.
- Foot mechanics. Being flat-footed, having a high arch or even having an abnormal pattern of walking can affect the way weight is distributed when you’re standing and put added stress on the plantar fascia.
- Obesity. Excess pounds put extra stress on your plantar fascia.
- Occupations that keep you on your feet. Factory workers, teachers and others who spend most of their work hours walking or standing on hard surfaces can damage their plantar fascia.
Plantar fasciitis symptoms
Symptoms of plantar fasciitis include:
- A painful heel. The main symptom of plantar fasciitis is pain, especially when you walk. For example, when first getting out of bed.
- The pain tends to subside at first, only to return later after long periods of weight-bearing
- Pain may also be felt along the centre of the foot
- Stiffness of the ankle. Bringing your foot towards to shin bone leads to pain.
Plantar fasciitis typically causes a stabbing pain in the bottom of your foot near the heel. The pain is usually the worst with the first few steps after awakening, although it can also be triggered by long periods of standing or rising from sitting. The pain is usually worse after exercise, not during it.
Plantar fasciitis complications
Ignoring plantar fasciitis may result in chronic heel pain that hinders your regular activities. Changing the way you walk to minimize plantar fasciitis pain might lead to foot, knee, hip or back problems.
Plantar fasciitis diagnosis
The diagnosis is made based on the medical history and physical examination. During the exam, your doctor will check for areas of tenderness in your foot. Where your pain is situated can help determine its cause.
Imaging tests
Usually no tests are necessary. Your doctor might suggest an X-ray or magnetic resonance imaging (MRI) to make sure your pain isn’t being caused by another problem, such as a stress fracture or a pinched nerve.
Sometimes an X-ray shows a spur of bone projecting forward from the heel bone. In the past, these bone spurs were often blamed for heel pain and removed surgically. But many people who have bone spurs on their heels have no heel pain.
Plantar fasciitis treatment
Most people who have plantar fasciitis recover with conservative treatments, including resting, icing the painful area and stretching, in several months.
Medications
Pain relievers such as ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve) can ease the pain and inflammation associated with plantar fasciitis.
Therapies
Stretching and strengthening exercises or use of specialized devices may provide symptom relief. These include:
- Physical therapy. A physical therapist can instruct you in a series of exercises to stretch the plantar fascia and Achilles tendon and to strengthen lower leg muscles, which stabilize your ankle and heel. A therapist might also teach you to apply athletic taping to support the bottom of your foot.
- Night splints. Your physical therapist or doctor might recommend that you wear a splint that stretches your calf and the arch of your foot while you sleep. This holds the plantar fascia and Achilles tendon in a lengthened position overnight and facilitates stretching.
- Orthotics. Your doctor might prescribe off-the-shelf or custom-fitted arch supports (orthotics) to help distribute pressure to your feet more evenly.
Surgical or other procedures
When more-conservative measures aren’t working after several months, your doctor might recommend:
- Injections. Injecting a type of steroid medication into the tender area can provide temporary pain relief. Multiple injections aren’t recommended because they can weaken your plantar fascia and possibly cause it to rupture. More recently, platelet-rich plasma has been used, under ultrasound guidance, to provide pain relief with less risk of tissue rupture.
- Extracorporeal shock wave therapy. In this procedure, sound waves are directed at the area of heel pain to stimulate healing. It’s usually used for chronic plantar fasciitis that hasn’t responded to more-conservative treatments. This procedure might cause bruising, swelling, pain, numbness or tingling. Some studies show promising results, but it hasn’t been shown to be consistently effective.
- Tenex procedure. This minimally invasive procedure removes the scar tissue of plantar fasciitis without surgery.
- Surgery. Few people need surgery to detach the plantar fascia from the heel bone. It’s generally an option only when the pain is severe and all else fails. Side effects include a weakening of the arch in your foot.
Lifestyle and home remedies
To reduce the pain of plantar fasciitis, try these self-care tips:
- Maintain a healthy weight. Lose weight if you’re overweight or obese to minimize stress on your plantar fascia.
- Choose supportive shoes. Avoid high heels. Buy shoes with a low to moderate heel, good arch support and shock absorbency. Don’t go barefoot, especially on hard surfaces.
- Don’t wear worn-out athletic shoes. Replace your old athletic shoes before they stop supporting and cushioning your feet. If you’re a runner, buy new shoes after about 400 to 500 miles of use.
- Change your sport. Try a low-impact sport, such as swimming or bicycling, instead of walking or jogging.
- Apply ice. Hold a cloth-covered ice pack over the area of pain for 15 to 20 minutes three or four times a day or after activity. Or try ice massage. Freeze a water-filled paper cup and roll it over the site of discomfort for about five to seven minutes. Regular ice massage can help reduce pain and inflammation.
- Stretch your arches. Simple home exercises can stretch your plantar fascia, Achilles tendon and calf muscles.
Calcaneus fracture
A fracture of the calcaneus, or heel bone, can be a painful and disabling injury. Calcaneus fracture commonly occurs during a high-energy event—such as a car crash or a fall from a ladder—when the heel is crushed under the weight of the body. When this occurs, the heel can widen, shorten, and become deformed. Calcaneus fractures are rare but potentially debilitating injuries 5. Fractures of the tarsal bones account for only about 2% of all adult fractures and only 50-60% of tarsal fractures are calcaneus fractures 5. Historically a burst fracture of the calcaneus was coined a “Lovers Fracture” as the injury would occur as a suitor would jump off a lovers balcony to avoid detection 6.
Most patients with calcaneus fractures are young, with the 20-39 age group the most common. Calcaneus fractures are rare in children. Comorbidities such as diabetes and osteoporosis may increase the risk of all types of fractures.
Calcaneus fractures can be quite severe. A calcaneus fracture may cause the calcaneus bone to widen and shorten. In some cases, a fracture may also enter the subtalar joint in the foot. When this occurs, damage to the articular cartilage covering the joint may cause long-term complications such as chronic pain, arthritis, and loss of motion.
Treatment often involves surgery to reconstruct the normal anatomy of the heel and restore mobility so that patients can return to normal activity. But even with appropriate treatment, some fractures may result in long-term complications, such as pain, swelling, loss of motion, and arthritis.
Calcaneus fracture severity
The severity of a calcaneus injury depends on several factors, including:
- The number of fractures
- The amount and size of the broken bone fragments
- The amount each piece is out of place (displaced) — In some cases, the broken ends of bones line up almost correctly; in more severe fractures, there may be a large gap between the broken pieces, or the fragments may overlap each other
- The injury to the cartilage surfaces in the subtalar joint
- The injury to surrounding soft tissues, such as muscle, tendons, and skin
When the bone breaks and fragments stick out through the skin or if a wound penetrates down to the bone, the fracture is called an “open” fracture. An open fracture often causes more damage to the surrounding muscles, tendons, and ligaments and takes a longer time to heal. Open fractures have a higher risk for infection in both the wound and the bone. Immediate treatment to clean the wound is required to prevent infection.
Calcaneus fracture classification
Calcaneal fractures can be classified into two general categories 7.
- Extraarticular fractures account for 25 % of calcaneal fractures. These typically are avulsion injuries of either the calcaneal tuberosity from the Achilles tendon, the anterior process from the bifurcate ligament, or the sustenaculum tali.
- Intraarticular fractures account for the remaining 75%. The talus acts as a hammer or wedge compressing the calcaneus at the angle of Gissane causing the fracture.
There are two main classification systems of extraarticular fractures.
Essex-Lopresti:
- Joint depression type with a single verticle fracture line through the angle of Gissane separating the anterior and posterior portions of the calcaneus.
- Tongue type which has the same verticle fracture line as a depression type with another horizontal fracture line running posteriorly, creating a superior posterior fragment.
Sanders Classification: Based on reconstituted CT findings.
- Type I fractures: 1 nondisplaced or minimally displaced bony fragment
- Type II fractures: 2 bony fragments involving the posterior facet. Subdivided into types A, B, and C depending on the medial or lateral location of the fracture line.
- Type III fractures: 3 bony fragments including an additional depressed middle fragment. Subdivided into types AB, AC, and BC, depending on the position and location of the fracture lines.
- Type IV fractures: 4 comminuted bony fragments.
Calcaneus fracture cause
Calcaneus fractures most commonly occur during high energy events leading to axial loading of the bone but can occur with any injury to the foot and ankle 8.
The calcaneus is most often fractured during a:
- Fall from a height
- Twisting injury to the ankle
- Motor vehicle collision
Most of the injuries cause the calcaneus bone to flatten, widen, and shorten. Stress fractures may occur with over use or repetitive use, such as running.
The severity of a fracture can vary. For example, a simple twist of the ankle may result in a single crack in the bone. The force of a head-on car collision, however, may result in the bone being shattered (comminuted fracture).
Similar fractures can result from different mechanisms. For example, if you land on your feet from a fall, your body’s weight is directed downward. This drives the talus bone directly into the calcaneus. In a motor vehicle crash, the calcaneus is driven up against the talus if the heel is crushed against the floorboard. In both cases, the fracture patterns are similar. As a rule, the greater the impact, the more the calcaneus is damaged.
In a high-energy fracture, other injuries, such as fractures of the spine, hip, or other heel, can occur.
Calcaneus fracture symptoms
Patients with calcaneus fractures usually experience:
- Pain
- Bruising
- Swelling
- Heel deformity
- Inability to put weight on the heel or walk
With some minor calcaneus fractures, the pain may not be enough to prevent you from walking — but you may limp. This is because your Achilles tendon acts through the calcaneus to support your body weight. If, however, your calcaneus is deformed by the injury, your muscle and tendon cannot generate enough power to support your weight. Your foot and ankle will feel unstable, and you will walk differently.
Calcaneus fracture complications
Complications often occur with calcaneus fractures. Minor complications include:
- Small or temporary areas of delayed wound healing
- Nerve irritation around the incision
- Tendon irritation
- Joint stiffness
- Chronic pain
- Chronic swelling
Major complications include:
- Failure of the wound to heal
- Infection
- Posttraumatic arthritis (with or without surgery)
It is important to tell your doctor if you are a smoker. Smoking affects both bone and wound healing. With or without surgery, your bone may take longer to heal if you smoke.
Additional surgery is usually required in cases of infection or wound healing complications. If all attempts to resolve an infection or a wound healing complication fail, an amputation may be necessary.
Calcaneus fracture diagnosis
It is important that you tell your doctor the circumstances of your injury. For example, if you fell from a ladder, how far did you fall?
It is also important that you tell your doctor if you have any other injuries or medical problems, such as diabetes, or if you take medications or smoke.
Physical Examination
After discussing your symptoms and medical history, your doctor will perform a careful examination. He or she will:
- Examine your foot and ankle to see if your skin was damaged or punctured from the injury.
- Check your pulse at key points of the foot to be sure that there is a good blood supply to the foot and toes.
- Check to see if you can move your toes, and can feel things on the bottom of your foot.
- Determine whether you have injured any other areas of your body by examining the rest of your injured leg, your other leg, pelvis, and spine.
Tests
Imaging studies will help confirm the diagnosis of a calcaneus fracture:
- X-rays. This test is the most common and widely available diagnostic imaging technique. X-rays create images of dense structures, such as bone. An x-ray can show if your calcaneus is broken and whether the bones are displaced.
- Bohler’s Angle may be depressed on plain radiographs. Defined as the angle between two lines drawn on plain film. The first line is between highest point on the tuberosity and the highest point of posterior facet and the second is the highest point on the anterior process and the highest point on the posterior facet. Normal angle is between 20-40 degrees.
- The Critical Angle of Gissane may be increased. Defined as the angle between two lines drawn on plain film. The first along the anterior downward slope of the calcaneus and the second along the superior upward slope. A normal angle is 130-145 degrees.
- Normal Bohlers and Gissane angles do not rule out a fracture.
- Abnormalities of either of these findings should prompt a CT scan for further classification and evaluation of the fracture.
- Computed tomography (CT) scans. Because of the complex anatomy of the calcaneus, a CT scan is routinely ordered after a calcaneus bone fracture has been diagnosed on x-ray. A CT scan will produce a more detailed, cross-sectional image of your foot and can provide your doctor with valuable information about the severity of your fracture. Mondors Sign is a hematoma identified on CT that extends along the sole and is considered pathognomic for calcaneal fracture. This information will help your doctor recommend the best plan for treatment.
- Stress fractures such as those seen in runners would be best evaluated with a bone scan or MRI scan.
Your doctor may share both your x-rays and CT scans with you to help you better understand the nature and severity of your injury.
Calcaneus fracture treatment
There is no universal agreement among experts as to the best treatment method for calcaneus fractures. No single method works the same for everyone.
Your doctor will consider several factors in planning your treatment, including:
- The cause of your injury
- Your overall health
- The severity of your injury
- The extent of soft tissue damage
Because most calcaneus fractures cause the bone to widen and shorten, the goal of treatment is to restore the normal anatomy of the heel. In general, patients whose normal heel anatomy is restored have better outcomes. In most cases, recreating the normal heel anatomy involves surgery. Your doctor will discuss the different treatment options with you.
Nonsurgical treatment
Nonsurgical treatment may be recommended if the pieces of broken bone have not been displaced by the force of the injury.
Immobilization. A cast, splint, or brace will hold the bones in your foot in proper position while they heal. You may have to wear a cast for 6 to 12 weeks — or possibly longer. During this time, you will not be able to put any weight on your foot until the bone is completely healed.
Surgical treatment
If the bones have shifted out of place (displaced), your doctor may recommend surgery.
Surgery to repair a calcaneus fracture can restore the normal shape of the bone but is sometimes associated with complications, such as wound healing problems, infection, and nerve damage. Nonsurgical treatment of some fractures, however, can also lead to long-term complications, such as pain, arthritis, and a limp. Your doctor will review the details of your injury and talk with you about the risks and benefits of surgical versus nonsurgical treatment.
Timing of surgery
If the skin around your fracture has not been broken, your doctor may recommend waiting until swelling has gone down before having surgery. Elevating your leg and keeping it immobilized for several days will decrease swelling. It will also give stretched skin a chance to recover. Waiting before the operation may improve your overall recovery from surgery and decrease your risk of infection.
Open fractures, however, expose the fracture site to the environment and must be treated immediately. They require surgery to clean the wound and remove damaged tissue
Early surgery is also often recommended for an avulsion fracture. Although uncommon, a piece of the calcaneus can be pulled off when the Achilles tendon splits away from the bone (avulsion). For this type of fracture, emergent surgery can decrease the risk of injury to the skin around the Achilles tendon.
Surgical procedure
The following procedures are used for various types of calcaneus fractures:
- Percutaneous screw fixation. If the bone pieces are large, they can sometimes be moved back into place without making a large incision. Special screws are then inserted through small incisions to hold the fracture together.
- Open reduction and internal fixation. During this operation, an open incision is made to reposition (reduce) the bones into their normal alignment. They are held together with wires or metal plates and screws.
Bones have a remarkable capacity to heal. The more severe your injury, however, the longer your recovery may be. Patients with more severe fractures are also more likely to suffer some degree of permanent loss of function, regardless of treatment.
Pain management
After surgery, you will feel some pain. This is a natural part of the healing process. Your doctor and nurses will work to reduce your pain, which can help you recover from surgery faster.
Medications are often prescribed for short-term pain relief after surgery. Many types of medicines are available to help manage pain, including opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and local anesthetics. Your doctor may use a combination of these medications to improve pain relief, as well as minimize the need for opioids.
Be aware that although opioids help relieve pain after surgery, they are a narcotic and can be addictive. Opioid dependency and overdose has become a critical public health issue in the U.S. It is important to use opioids only as directed by your doctor. As soon as your pain begins to improve, stop taking opioids. Talk to your doctor if your pain has not begun to improve within a few days of your surgery.
Rehabilitation
Whether your treatment is surgical or nonsurgical, your rehabilitation will be very similar. The time it takes to return to daily activities will vary depending on the type and severity of the fracture and whether you have other injuries.
Some patients can begin weight-bearing activities a few weeks after injury or surgery; others may need to wait 3 months or more before putting weight on the heel. Most patients are able to begin partial weight bearing between 6 and 10 weeks after injury or surgery.
- Early motion. Many doctors encourage motion of the foot and ankle early in the recovery period. For example, you may be instructed to begin moving the affected area as soon as your pain allows. If you have had surgery, you may be instructed to begin moving the affected area as soon as the wound heals to your doctor’s satisfaction.
- Physical therapy. Specific exercises can help improve the range of motion in your foot and ankle, and strengthen supporting muscles. Although they are often painful at the beginning and progress may be difficult, exercises are required in order for you to resume normal activities.
- Weight bearing. When you begin walking, you may need to use crutches, a cane, or a walker and/or wear a special boot. It is very important to follow your doctor’s instructions for walking on your foot. If you put weight on your foot too soon, the bone pieces may move out of place and you might require surgery. If you have had surgery, the screws might loosen or break and the bone may collapse. This may not occur the first time you walk on it but, if the bone is not healed and you continue to bear weight, the metal will eventually break.
Calcaneus fracture recovery time
Some patients can begin weight-bearing activities a few weeks after injury or surgery; others may need to wait 3 months or more before putting weight on the heel. Most patients are able to begin partial weight bearing between 6 and 10 weeks after injury or surgery. If your calcaneus fracture is severe, however, it may take from 1 to 2 years before recovery is complete.
Patients whose x-rays show good healing and normal heel anatomy often have ongoing symptoms after treatment. On the other hand, the calcaneus can look quite deformed on an x-ray, but the patient may have few, if any, symptoms.
Studies have compared results in patients whose fractures were treated with and without surgery. Some studies show a significant benefit of surgery, while other studies show less benefit for certain patients. Researchers continue to look for ways to improve the outcomes of treatment for different types of calcaneus fractures, as well as for patients who smoke or have other health considerations. Your doctor will talk with you about the best treatment options in your case.
Calcaneus fracture prognosis
If your injury is minor, such as a crack in the calcaneus bone with little muscle damage, you may be able to resume normal activities from 3 to 4 months after surgery. If your calcaneus fracture is severe, however, it may take from 1 to 2 years before recovery is complete.
Despite the best efforts of the doctor and patient, normal foot and ankle motion is rarely regained after a severe fracture and patients do not typically resume their pre-injury level of function. A patient who is not very active might tolerate a foot that is not normal. On the other hand, a patient whose job or recreational activities require a lot of walking or climbing will notice more.
Common problems
Common problems that may persist after recovery include:
- Skin irritation. Footwear can irritate the skin or tendons in the affected area.
- Altered gait. In some cases, the arch of the foot has not been restored, or the Achilles tendon has not healed at its normal distance from the ankle. Full motion between the talus and the calcaneus is rarely regained in these cases, and this can change the way you walk. You may have problems walking on uneven ground, such as grassy surfaces or hills.
- Pain. Following a fracture, you may experience continued subtalar pain and limited motion. Even if the heel anatomy is perfectly restored, you may still have discomfort. This can happen because of injured soft tissues, persistent fracture displacement, or limited ankle and subtalar range of motion. Although relatively uncommon, pain can also be caused by irritation from the plates or screws.
Further treatment
If you have chronic pain or experience other complications, you may need further treatment. This may include:
- Orthotics. A simple shoe modification may help some chronic problems. You may need to wear a heel pad, lift, or shoe cup, as well as special shoes with extra depth in the toe compartment.
- Additional surgery. Sometimes, another major operation is required. If the bone has healed in a deformed position, or if the subtalar joint becomes arthritic, the joint between the talus and the calcaneus may need to be fused. The goal of this procedure is to help the talus and the calcaneus grow together to form one bone.
Fusion means that no more motion can occur between the two bones. If the bone is badly deformed, your doctor may attempt to correct some or all of the deformity along with the fusion.
- Keener BJ, Sizensky JA. The anatomy of the calcaneus and surrounding structures. Foot Ankle Clin. 2005 Sep;10(3):413-24.[↩][↩]
- Hall RL, Shereff MJ. Anatomy of the calcaneus. Clin. Orthop. Relat. Res. 1993 May;(290):27-35[↩]
- Gupton M, Terreberry RR. Anatomy, Bony Pelvis and Lower Limb, Calcaneus. [Updated 2018 Dec 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519544[↩]
- Keener BJ, Sizensky JA. The anatomy of the calcaneus and surrounding structures. Foot Ankle Clin. 2005 Sep;10(3):413-24[↩]
- Davis D, Newton EJ. Calcaneus Fractures. [Updated 2019 Mar 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430861[↩][↩]
- Adams MR, Koury KL, Mistry JB, Braaksma W, Hwang JS, Firoozabadi R. Plantar Medial Avulsion Fragment Associated With Tongue-Type Calcaneus Fractures. Foot Ankle Int. 2019 Mar 06;:1071100719830948[↩]
- Jiménez-Almonte JH, King JD, Luo TD, Aneja A, Moghadamian E. Classifications in Brief: Sanders Classification of Intraarticular Fractures of the Calcaneus. Clin. Orthop. Relat. Res. 2019 Feb;477(2):467-471[↩]
- Hordyk PJ, Fuerbringer BA, Roukis TS. Clinical Management of Acute, Closed Displaced Intra-Articular Calcaneal Fractures. Clin Podiatr Med Surg. 2019 Apr;36(2):163-171.[↩]