What is pes cavus
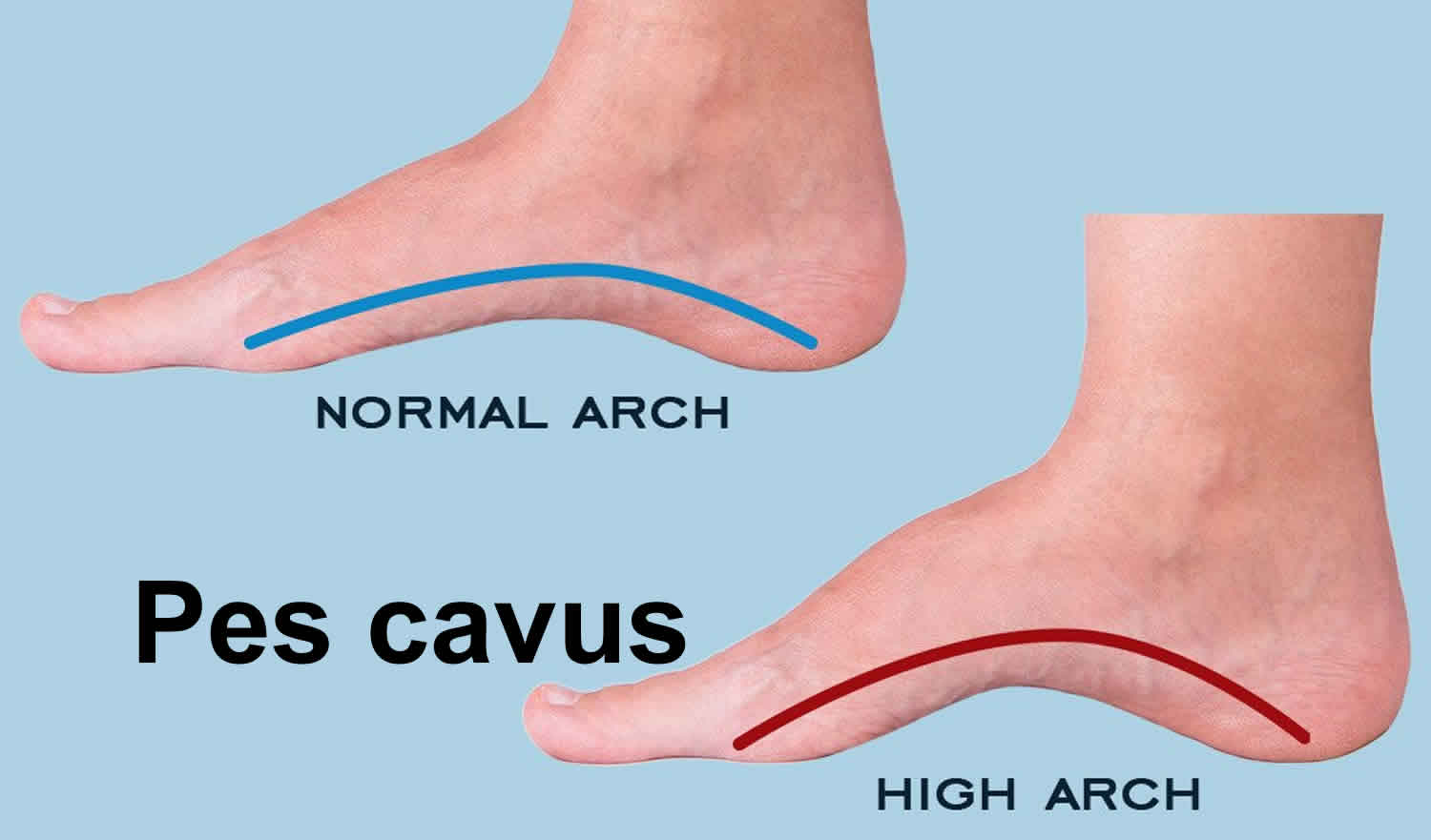
Pes cavus is high arch foot, which is an abnormal elevation of the medial longitudinal arch of the foot. The arch runs from your toes to the heel on the bottom of your foot. Pes cavus is the opposite of pes planus (flat feet). Unlike pes planus (flat feet), pes cavus (highly arched feet) are often more rigid in structure and tend to be painful as the shock absorption function during gait is lost as a result of the inability of the hindfoot to assume a valgus alignment. This is so because more stress is placed on the section of the foot between the ankle and toes (metatarsals). Pes cavus foot is a less efficient shock absorber, while being placed under constant tension. The normal tripod weight-bearing structure of the foot becomes unbalanced in a cavus foot leading to frequent episodes of ankle instability or painful calluses on the sole of the foot. The person would balance on only 3 main areas: the 1st, 5th metatarsal heads, and the heel. A varus hindfoot will lead to calluses on the lateral border of the foot, usually at the base of the fifth metatarsal. Plantar flexion of the forefoot leads to increased pressure on the metatarsal heads. Clawing of the toes may cause calluses on the dorsum of the flexed proximal interphalangeal joints of the toes due to friction in the shoe 1. Pes cavus can make it difficult to fit into shoes. People who have high arches most often need foot support. Pes cavus may cause disability.
The long-term impact of a cavus foot is that the person is more vulnerable to certain overuse injuries during sports, exercise and even during their daily activities.
Pes cavus may be due to a plantar-flexion deformity of the forefoot (forefoot equinus) or due to dorsiflexion of the calcaneus. Although the hindfoot is more commonly in varus, it may at times be in valgus alignment. The first ray is typically plantar-flexed and the forefoot is typically in pronation.
The incidence of pes cavus deformity is variable as it is typically related to an underlying neuromuscular disorder or neurological injury.
People with pes cavus should be checked for nerve and bone conditions. Finding these other conditions may help prevent or reduce arch problems.
A detailed neurological examination of the extremities is important, as is a full examination of the spine for deformity or signs of spinal dysraphism. As mentioned above, the clinical progression of a pes cavus foot deformity entails a transition from a flexible to a rigid deformity. In the most common variety, a cavovarus foot, the forefoot is rigidly pronated relative to the hindfoot and the subtalar joint is inverted into varus. The hindfoot deformity is initially flexible but eventually becomes rigid. The Coleman block test is used to evaluate the flexibility of the hindfoot 2. For the test, the patient stands with a rigid block under the lateral border of the foot, allowing the first metatarsal to plantar-flex. A flexible hindfoot varus deformity will correct to valgus alignment indicating the presence of a forefoot-driven flexible hindfoot varus whereas a rigid hindfoot deformity will not correct with this maneuver.
A history of progressive changes in foot shape and function must be sought. A sudden worsening of the deformity in a child with myelomeningocele could represent the effects of a tethered spinal cord. Examination of family members for subtle or not so subtle cavus foot deformity may help reveal the underlying diagnosis. Long standing cavovarus deformities can be associated with patellar instability and recurrent ankle sprains.
People with pes cavus foot problems would need a thorough biomechanical assessment before undergoing any treatment. Any neurological component would suggest a more severe condition; the patient would be advised accordingly and referred to the relevant doctors for further diagnostic investigation. In general, the best preventative treatment is to have children’s feet checked before the age of 8 to ensure they are developing correctly. Conservative treatment often involve custom foot orthotics for realignment and offloading of the feet. These should be designed precisely to the person. Because cavus feet are less adaptable than other foot types, even 1 extra degree of angulation can affect the knees, hips and spine.
Figure 1. Pes cavus
Pes cavus causes
Pes cavus (high arch feet) are much less common than flat feet. Pes cavus are more likely to be caused by a bone (orthopedic) or nerve (neurological) condition. There are different factors that can cause pes cavus foot, including heredity and neurological conditions. Typically, conditions such as Charcot-Marie-Tooth or clubfoot deformity present as high arches.
Unilateral pes cavus causes:
- Scarring of the deep posterior compartment of the leg
- Post-traumatic: calcaneal or talar fractures
- Spinal cord tumor
- Tethered cord
- Peroneal nerve injury
- Poliomyelitis
- Iatrogenic
Bilateral pes cavus causes:
- Charcot Marie Tooth disease
- Friedrich’s ataxia
- Myelodysplasia
- Syringomyelia
- Cerebral palsy
- Muscular dystrophy
- Idiopathic/familial pes cavus
Greater than two-thirds of cavus foot deformities are associated with an underlying neurological disorder causing a muscle imbalance 3. The most common underlying diagnosis is Charcot-Marie-Tooth disease (also known as hereditary motor and sensory neuropathy). Patients with Charcot-Marie-Tooth typically have a weak tibialis anterior and a weak peroneus brevis. These are overpowered by a preservation of the posterior tibialis and peroneus longus, causing hindfoot varus with forefoot equinus and pronation. The less common calcaneocavus deformity is typically seen in children with myelomeningocele or poliomyelitis 4. Bilateral involvement tends to be associated with systemic conditions and unilateral cavus deformity may be due to a more localized cause. Spinal cord pathology such as a tethered cord or spinal cord tumor must be ruled out in cases of new onset unilateral cavus deformity. As established muscle weakness and imbalance are irreversible, even with successful treatment or arrest of a neurological cause, the cavus foot deformity is often progressive. The deformity is typically flexible at first and then becomes rigid.
Pes cavus symptoms
Pes cavus symptoms include:
- Shortened foot length
- Difficulty fitting shoes
- Foot pain with walking, standing, and running (not everyone has this symptom)
Symptomatic or painful pes cavus (high arch feet) often present with the following:
- Pain along the lateral column of the foot due to joint degeneration, periostitis, capsulitis, tendonitis, bursitis, and neuritis.
- Ankle instability and the tendency to suffer ankle sprains.
- Pain under the 1st metatarsal which may be a sesamoid fracture, sesamoiditis, osteoarthritis, hallux limitus, tendonitis, etc.
- Plantar fasciitis due to constant tension exerted on the plantar fascia and achilles.
- Metatarsal and lateral column stress fractures.
- A collapse of the foot structure due to the high arch becoming flattened.
Pes cavus possible complications
Pes cavus complications may include:
- Chronic pain
- Difficulty walking
Given that cavus foot deformities are typically the result of a neurologic disorder, recurrence is common. Revision surgical intervention is often required. The healing of medially based incisions may be tenuous given the stretching that occurs as part of the correction of the pes cavus foot deformity. Excessive scar formation medially may also impair revision correction of recurrent pes cavus foot deformity.
Pes cavus diagnosis
When the person stands on the foot, the instep looks hollow. Most of the weight is on the back and balls of the foot (metatarsals head).
Your doctor will check to see if the pes cavus is flexible, meaning it can be moved around.
Tests that may be done include:
- X-ray of the feet
- X-ray of the spine
- Electromyography (EMG)
- MRI of the spine
- Nerve conduction studies
- Genetic testing to look for hereditary genes that can pass on to your child
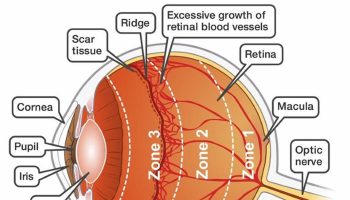
Initial evaluation should include weight-bearing anteroposterior (AP) and lateral radiographs of the feet. Meary’s angle, the Hibbs angle and calcaneal pitch are measured on the lateral view. Meary’s angle is the angle between the axis of the talus and the axis of the first metatarsal on the lateral view 5. It is normally a straight-line relationship but in cavus feet will be angulated apex dorsally. The Hibbs angle is the angle between the first metatarsal and the long axis of the calcaneus on the lateral view. In normal feet it is 150 degrees and it decreases as the cavus deformity worsens and the longitudinal arch becomes more elevated. Calcaneal pitch is also measured on the lateral view and values greater than 30 degrees are consistent with cavus deformity. On the AP radiograph, the angle between the axis of the talus and the calcaneus is normally approximately 30 degrees; this angle lessens and the talus and calcaneus become increasingly parallel with increased hindfoot varus 4.
As Charcot-Marie-Tooth disease is associated with progressive hip subluxation and dysplasia, an AP pelvis radiograph is indicated in those with suspected Charcot-Marie-Tooth disease. As part of the work-up of possible spinal dysraphism or tumor, spine radiographs and/or MRI may be indicated. Complete neurological evaluation by a pediatric neurologist is often appropriate and electromyography or muscle biopsy may be part of the work-up of an underlying neuromuscular disorder.
Pes cavus treatment
People with pes cavus foot problems would need a thorough biomechanical assessment before undergoing any treatment. Treatment of a cavus foot deformity must be considered in the context of the underlying diagnosis. If the cause of the pes cavus foot deformity is treatable (such as a spinal cord tumor or tethered spinal cord) it should be the first focus of treatment even though the resultant foot deformity may still be progressive. The goal of treatment of a patient with a cavus foot deformity is to achieve a painfree, plantigrade, mobile foot with improved muscle balance.
Non-operative management options should be attempted when appropriate before advancing to surgical options. Pes cavus, particularly ones that are flexible or well cared for, may not need any treatment. Corrective shoes may help relieve pain and improve walking. This includes changes to the shoes, such as an arch insert and a support insole.
Associated tightness in the heel cord and plantar fascia may be managed with a stretching program. Weakness in dorsiflexion and eversion may be addressed with an exercise program. Orthotic management including a lateral heel wedge for the flexible hindfoot or a well molded supramalleolar orthosis or ankle foot orthosis may improve balance and help prevent recurrent ankle instability. Symptoms of plantar callosities may be improved with appropriate arch support or metatarsal pads 1.
Surgery to flatten the foot is sometimes needed in severe cases. Any nerve problems that exist must be treated by specialists.
Pes cavus surgery
Indications for surgical intervention include progressive deformity, painful callosities and hindfoot or ankle instability. Many operative procedures have been described to correct the individual deformities and balance the muscle forces in a cavus foot (a full description of these is beyond the scope of this discussion). An important classification that should guide treatment is the flexibility of the segmental deformities. Soft tissue and plantar fascia releases may be used for a flexible deformity whereas an osteotomy or multiple osteotomies are required for a fixed deformity. Plantar fascia release is a standard component of cavus foot procedures. Open release rather than percutaneous release is preferable and should include release of the intrinsic muscles of the foot and the origin of the abductor hallucis. Muscle balancing procedures to help the first ray imbalance are typically considered next, including the peroneus longus to brevis transfer and the transfer of the extensor hallucis longus to the first metatarsal head with interphalangeal joint fusion of the great toe (Jones transfer). Lesser toe imbalance may be addressed by transfer of the extensor digitorum longus tendons to the metatarsal necks (Hibbs transfer) with proximal interphalangeal joint fusion, with or without flexor tenotomy. Correction of the claw toe deformities frequently requires dorsal capsulotomy of the metatarsophalangeal joint in addition to the described tendon transfers and interphalangeal joint fusion.
A rigid plantar flexion deformity of the first ray requires a corrective osteotomy. Advantages of a plantar-based opening-wedge osteotomy of the medial cuneiform are its stability and its location at the apex of the cavus deformity. An osteotomy of the first metatarsal places the physis at risk for arrest and is less stable. Midfoot osteotomies remove a dorsally based wedge from the tarsal bones, preserving the talonavicular joint and calcaneal cuboid joints. This approach results in a short foot and does not address hindfoot varus. A lateral closing wedge (Dwyer type) osteotomy of the calcaneus or a calcaneus lateral slide (Koutsougiannis-Pridie type) will correct an associated varus deformity of the hindfoot. Calcaneo-cuboid-cuneiform osteotomies have been advocated for correction of the deformity as well. Triple arthrodesis should be reserved as a salvage procedure for feet near or at skeletal maturity with advanced rigid deformity with associated degenerative changes. It has been associated with poor long-term results, particularly in patients with progressive deformity and sensory impairment 6.
Pes cavus prognosis
Pes cavus outlook depends on the condition causing high arches. In mild cases, wearing proper shoes and arch supports may provide relief.
- Kasser JR. (2006). The Foot. In Lovell & Winter’s Pediatric Orthopaedics, Sixth Edition, Ed. Morrissy RT and Weinstein SL; Lippincott Williams & Wilkins, Philadelphia, PA[↩][↩]
- Coleman SS, Chesnut WJ. A simple test for hindfoot flexibility in the cavovarus foot. Clin Orthop Relat Res. 1977; 123:60-62.[↩]
- Mosca VS. The cavus foot. J of Pediatr Orthop. 2001; 21: 423-424.[↩]
- Mosca VS. (2014). The Foot. In Lovell & Winter’s Pediatric Orthopaedics, Seventh Edition, Ed. Weinstein SL and Flynn JM; Lippincott Williams & Wilkins, Philadelphia, PA.[↩][↩]
- Meary R. On the measurement of the angle between the talus and the first metatarsal. Symposium: Le Pied Creux Essential. Rev Chir Orthop. 1967; 53: 389.[↩]
- Schwend RM, Drennan JC. Cavus foot deformity in children. J Am Acad Orthop Surg. 2003; 11: 201-211.[↩]