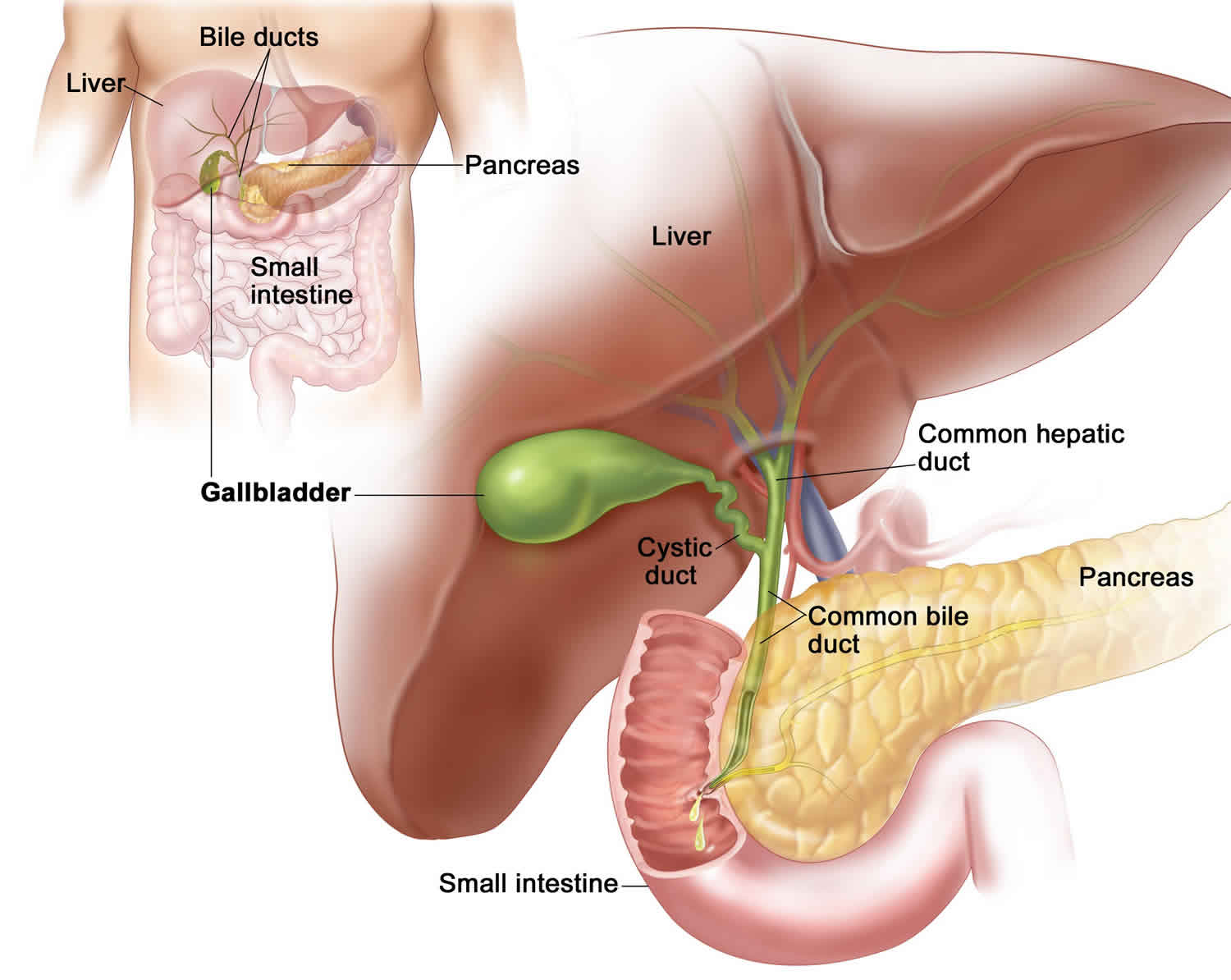
What is adenomyomatosis of the gallbladder
Gallbladder adenomyomatosis also known as adenomyoma or adenomyomatous hyperplasia of the gallbladder, is a benign (non-cancerous) condition characterized by epithelial proliferation and hypertrophy of the muscles of the gallbladder wall 1 with an outpouching of the mucosa into or through the thickened muscular layer, i.e., the Rokitansky-Aschoff sinuses 2. Rokitansky-Aschoff sinuses may contain calculi and/or cholesterol crystals. The gallbladder wall thickening, Rokitansky-Aschoff sinuses, and the calculi and/or cholesterol crystals that are often found in sinuses characterize the imaging appearance of adenomyomatosis 3. Sometimes, particularly when the characteristic imaging findings are not present, adenomyomatosis can be difficult to distinguish from gallbladder cancer based on the diagnostic imaging findings. Adenomyomatosis is often asymptomatic and incidentally detected, requiring no specific treatment 3. Adenomyomatosis also can be associated with right upper quadrant pain. In cases where it is difficult to distinguish adenomyomatosis from gallbladder cancer or when adenomyomatosis is associated with right upper quadrant pain, this condition may be treated with a cholecystectomy 4.
Adenomyomatosis has been found in 1% to 8.7% of cholecystectomy specimens 3. Although there is a wide age range of patients who are diagnosed with adenomyomatosis, patients are most frequently diagnosed in their 50s 3. There are discrepancies in the literature regarding the prevalence of adenomyomatosis in males and females. Specifically, some authors state that adenomyomatosis is more prevalent in women than men (3:1). Other authors state that the prevalence is similar in men and women. There is no known race predilection 5.
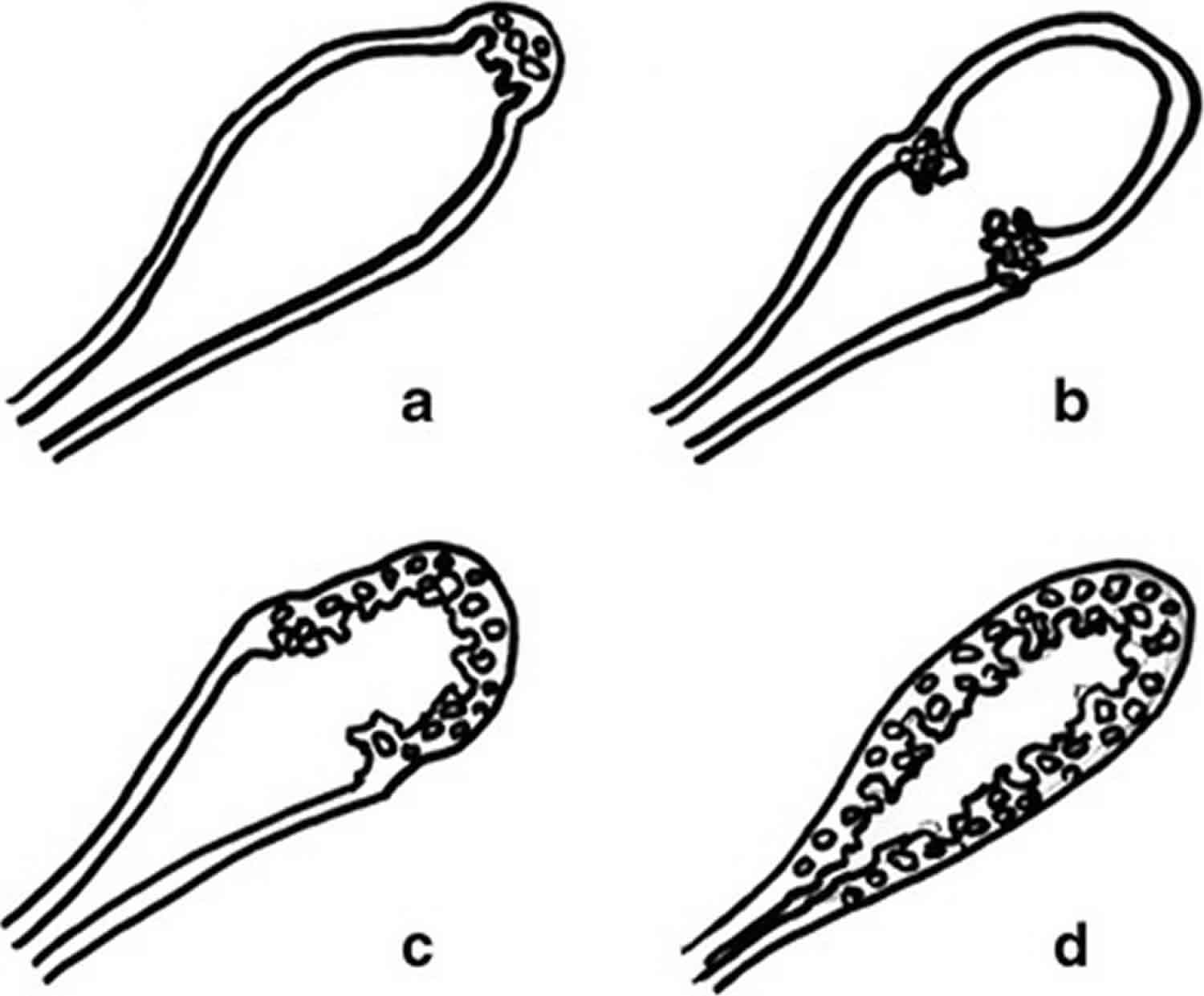
Gallbladder adenomyomatosis has four morphological types according to the localization in the gallbladder wall (see Figure 1) 6: 1) Fundal (localized) type, 2) segmental type, 3) diffuse type and 4) annular type 6.
- Localized gallbladder adenomyomatosis is the most common pattern and is characterized by a focal thickening, usually involving the fundal region (the so-called “fundal gallbladder adenomyomatosis”). The uninvolved gallbladder wall appears physiologically thin and the overall gallbladder shape is usually maintained.
- Segmental gallbladder adenomyomatosis is characterized by the involvement of a larger portion of the gallbladder wall, typically the fundus and the distal third of the body. The involved portion appears contracted, whereas the uninvolved one maintains its normal shape.
- Annular gallbladder adenomyomatosis is characterized by a ring-form thickening of the gallbladder wall, usually involving the middle portion. The gallbladder appears contracted only in the involved portion, changing its global morphology and becoming “hourglass-shaped”. In some cases, epithelial proliferation may be particularly conspicuous and subdivide the gallbladder lumen into two separate compartments. As a consequence, biliary sludge and stones may accumulate into the isolated fundal compartment 7. According to some authors, annular gallbladder adenomyomatosis should be considered a subtype of segmental gallbladder adenomyomatosis 8.
- Diffuse gallbladder adenomyomatosis is characterized by the involvement of the whole organ that consequently appears contracted, even after fasting.
At present, the main treatment for gallbladder adenomyomatosis is surgery, but it is very important to screen patients and make clear the operation indications, taking the complications after cholecystectomy into consideration. As for asymptomatic gallbladder adenomyomatosis, a conservative treatment is recommended with ultrasound exams twice a year. The fundal type gallbladder adenomyomatosis can be treated by partial laparoscopic cholecystectomy. The segmental and diffuse type should undergo a total laparoscopic cholecystectomy. Females over 60 years of age who present gallbladder stones and segmental type gallbladder adenomyomatosis should undergo surgery 9.
Figure 1. Gallbladder adenomyomatosis patterns
Footnote: Gallbladder adenomyomatosis: patterns of gallbladder wall involvement. Drawings showing localized gallbladder adenomyomatosis (a), annular gallbladder adenomyomatosis (b), segmental gallbladder adenomyomatosis (c) and diffuse gallbladder adenomyomatosis (d)
[Source 6 ]Gallbladder adenomyomatosis cancer risk
Aldridge et al. 10 in 1991 first reported that gallbladder adenomyomatosis was a precancerous lesion. Afterwards, several articles suggested that gallbladder cancer originated from adenomyomatosis and the segmental-type adenomyomatosis had a higher incidence rate 11. However, recently researchers in China and abroad have suggested that adenomyomatosis in the initial stage was unrelated with gallbladder carcinoma (gallbladder cancer) in that it was only proliferation and found in 2.8–5% of all cholecystectomies in China and in 2–5% worldwide 11. Therefore, gallbladder adenomyomatosis relationship with early-stage gallbladder cancer remains unclear 1.
Based on available evidence, gallbladder adenomyomatosis cannot be regarded as a precancerous lesion 1. Gallbladder adenomyomatosis is a benign epithelial proliferation while stones and cholecystitis secondary to gallbladder adenomyomatosis may lead to dysplastic changes and cancer 1. Most patients with gallbladder adenomyomatosis do not have typical symptoms and usually present chronic cholecystitis and vague abdominal pain, which complement histological examination of cholecystectomy specimens 12. The increasing gallbladder intramural pressure may indicate that gallbladder decompression delays the adenomyomatosis progress.
Gallbladder adenomyomatosis causes
The cause of adenomyomatosis is unknown, although some have proposed that it is a response to chronic inflammation of the gallbladder. Since patients are most frequently diagnosed in their 50s, the idea of chronic inflammation as the etiology seems plausible 13.
Gallbladder adenomyomatosis symptoms
Most cases of adenomyomatosis of the gallbladder are thought to be asymptomatic. Right upper quadrant pain has been seen in association with adenomyomatosis. Some patients have coexistent cholelithiasis (gallstones), which can be symptomatic 3.
Gallbladder adenomyomatosis diagnosis
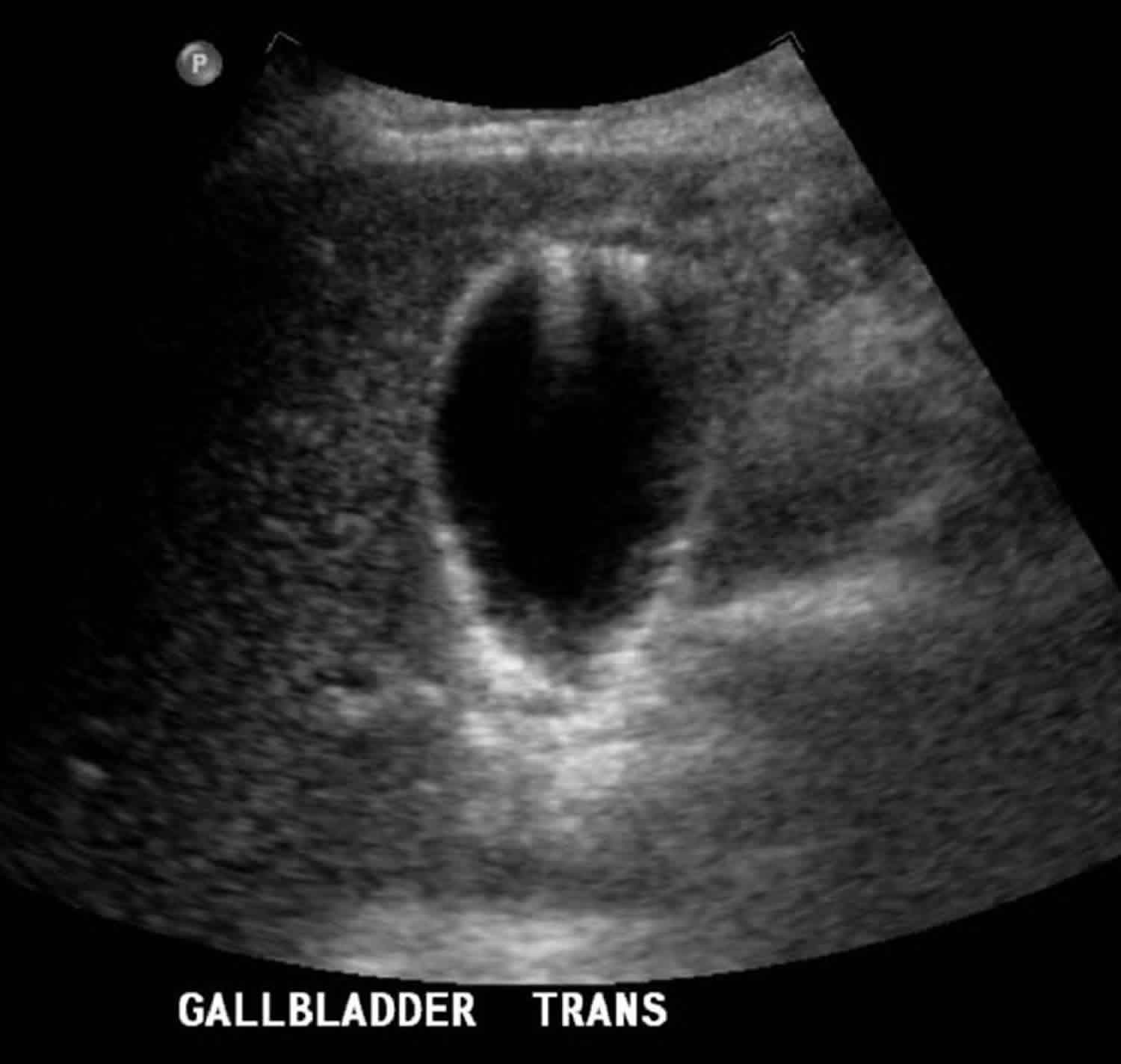
Abdominal ultrasound is the suggested diagnostic imaging test when a patient presents with right upper quadrant pain. Sometimes the ultrasound findings are characteristic of adenomyomatosis, and a confident diagnosis can be made. However, if gallbladder wall thickening is seen on ultrasound but cannot be well characterized, a magnetic resonance imaging (MRI) scan of the abdomen may be helpful for further characterization. If gallbladder wall thickening is seen incidentally on a computed tomography (CT) scan, an ultrasound and/or an MRI scan may be helpful for further characterization. Regardless of the modality used, the appearance of adenomyomatosis on imaging is related to the presence of characteristic gallbladder wall thickening, Rokitansky-Aschoff sinuses, and the calculi and/or cholesterol crystals that are often found in sinuses. By ultrasound, adenomyomatosis is seen as gallbladder wall thickening, intramural cystic spaces, and echogenic intramural foci (cholesterol crystals in the Rokitansky-Aschoff sinuses) that show comet tail artifacts. In most cases, all of the characteristic findings are not present 14.
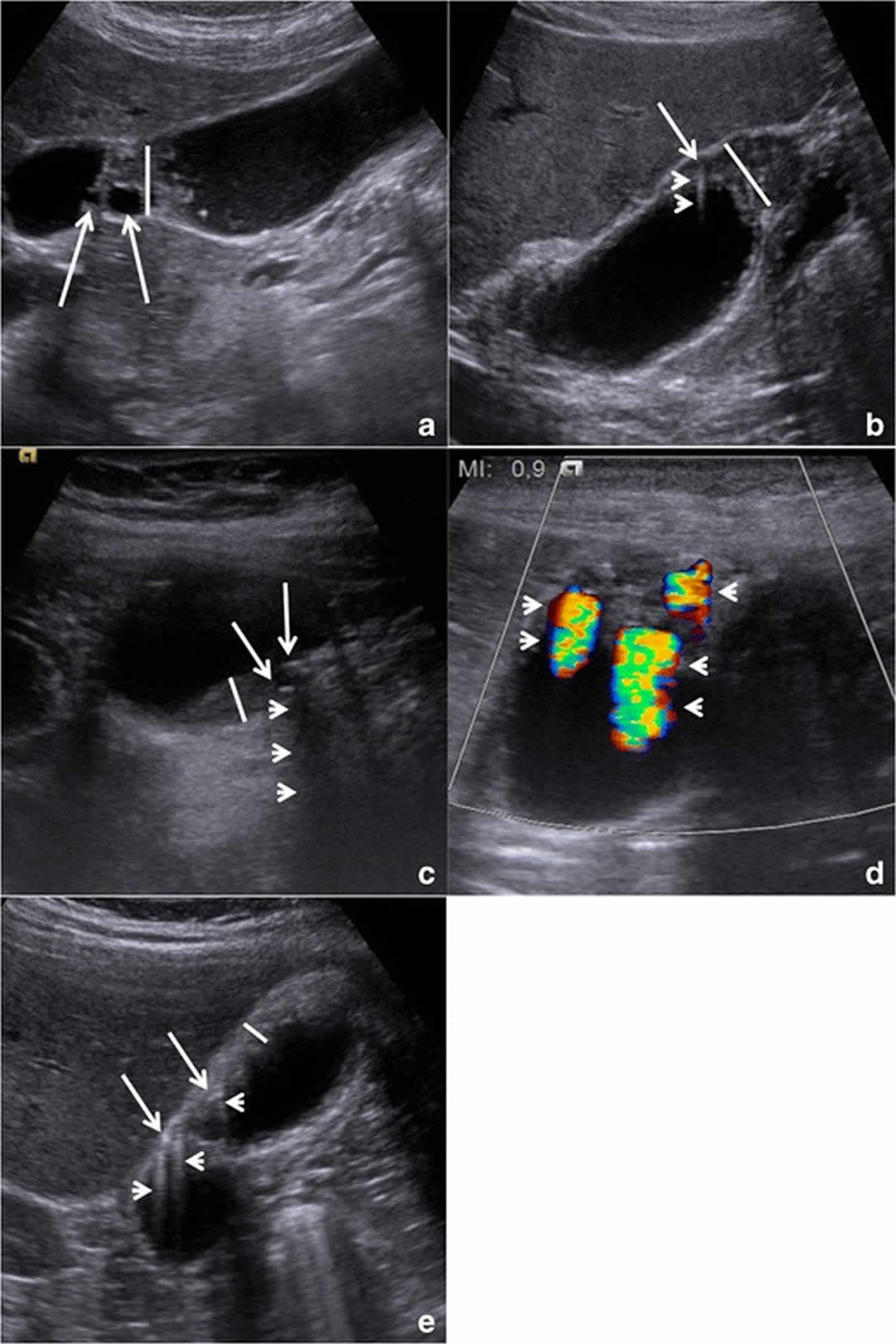
Of the ultrasound findings described, the echogenic foci with associated V-shaped comet tail artifacts have been described as specific for adenomyomatosis (Figure 2). On MRI, adenomyomatosis shows gallbladder wall thickening and T2 hyperintense intramural cystic spaces. Calculi are seen as signal voids. The T2 hyperintense cystic spaces can align in a curvilinear fashion, producing a “pearl necklace sign.” On CT imaging, nonspecific gallbladder wall thickening and wall enhancement are sometimes seen. The “rosary sign” can be present, which is caused by a thin layer of enhancing epithelium lining the intramural diverticula, which is surrounded by hypo-enhancing hypertrophied muscularis, causing the gallbladder wall to resemble a rosary.
Figure 2. Adenomyomatosis gallbladder ultrasound
Figure 3. Adenomyomatosis gallbladder ultrasound findings
Footnote: Gallbladder adenomyomatosis: typical ultrasound findings in annular type (a), fundal type (b and d), segmental type (c) and diffuse type (e). Gallbladder wall thickening (line) is always seen in gallbladder adenomyomatosis, but it is non-specific. On b-mode images, Rokitansky–Aschoff sinuses (arrows) typically appear anechoic (a), but they can also appear hyperechoic if cholesterine crystals or calcifications are present (b and c). Comet-tail reverberation artefacts (Figures b and e, arrowheads) or acoustic shadowing (c, arrowheads) are usually observed profoundly in Rokitansky–Aschoff sinuses. On colour Doppler images (d), twinkling artefacts (arrowheads) may be observed profoundly in Rokitansky–Aschoff sinuses.
[Source 6 ]Gallbladder adenomyomatosis treatment
In cases where it is difficult to distinguish adenomyomatosis from gallbladder cancer or when adenomyomatosis is associated with right upper quadrant pain, adenomyomatosis may be treated with a cholecystectomy. If adenomyomatosis is found incidentally and is asymptomatic, no treatment is recommended 15.
Gallbladder adenomyomatosis prognosis
Apart from the right upper quadrant abdominal pain that some patients experience, gallbladder adenomyomatosis is a benign condition and carries a good prognosis. Not all patients are symptomatic. In fact, adenomyomatosis is often asymptomatic and detected incidentally. It is important to note that gallbladder cancer can have a similar appearance to adenomyomatosis on imaging, and gallbladder carcinoma has a much worse prognosis than adenomyomatosis. Therefore, it is important to ensure that the imaging diagnosis of adenomyomatosis is confident before dismissing this abnormality.
- Pang L, Zhang Y, Wang Y, Kong J. Pathogenesis of gallbladder adenomyomatosis and its relationship with early-stage gallbladder carcinoma: an overview. Braz J Med Biol Res. ;51(6):e7411. doi:10.1590/1414-431×20187411 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6002143[↩][↩][↩][↩]
- Jutras A, Levesque HP. Adenomyoma and adenomyomatosis of the gallbladder. Radiol Clin North Am. 1966;4:483–500.[↩]
- Joshi JK, Kirk L. Adenomyomatosis. [Updated 2018 Dec 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482244[↩][↩][↩][↩][↩]
- Yang HK, Lee JM, Yu MH, Lee SM, Park J, Han NY, Lee K, Jang JY, Han JK. Correction to: CT diagnosis of gallbladder adenomyomatosis: importance of enhancing mucosal epithelium, the “cotton ball sign”. Eur Radiol. 2019 Feb;29(2):1060[↩]
- Golse N, Lewin M, Rode A, Sebagh M, Mabrut JY. Gallbladder adenomyomatosis: Diagnosis and management. J Visc Surg. 2017 Oct;154(5):345-353[↩]
- Bonatti M, Vezzali N, Lombardo F, et al. Gallbladder adenomyomatosis: imaging findings, tricks and pitfalls. Insights Imaging. ;8(2):243–253. doi:10.1007/s13244-017-0544-7 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5359147[↩][↩][↩][↩]
- A literature review of radiological findings to guide the diagnosis of gallbladder adenomyomatosis. Hammad AY, Miura JT, Turaga KK, Johnston FM, Hohenwalter MD, Gamblin TC. HPB (Oxford). 2016 Feb; 18(2):129-135.[↩]
- MR imaging of the gallbladder: a pictorial essay. Catalano OA, Sahani DV, Kalva SP, Cushing MS, Hahn PF, Brown JJ, Edelman RR. Radiographics. 2008 Jan-Feb; 28(1):135-55; quiz 324.[↩]
- Gallbladder adenomyomatosis: Diagnosis and management. Golse N, Lewin M, Rode A, Sebagh M, Mabrut JY. J Visc Surg. 2017 Oct; 154(5):345-353.[↩]
- Adenomyomatosis of the gallbladder. A premalignant lesion? Aldridge MC, Gruffaz F, Castaing D, Bismuth H. Surgery. 1991 Jan; 109(1):107-10.[↩]
- Actual status of clinical diagnosis in patients with primary gallbladder cancer associated with adenomyomatosis. Kai K, Irie H, Ide T, Masuda M, Kitahara K, Miyoshi A, Miyazaki K, Noshiro H, Tokunaga O. Indian J Gastroenterol. 2013 Nov; 32(6):386-91.[↩][↩]
- Poonam Y, Ashu S, Rohini G. Clinics in diagnostic imaging (121). Gallbladder adenomyomatosis. Singapore Med J. 2008;49:262–264[↩]
- Agrusti A, Gregori M, Salviato T, Codrich D, Barbi E. Adenomyomatosis of the Gallbladder as a Cause of Recurrent Abdominal Pain. J. Pediatr. 2018 Nov;202:328-328.e1[↩]
- Martin E, Gill R, Debru E. Diagnostic accuracy of transabdominal ultrasonography for gallbladder polyps: systematic review. Can J Surg. 2018 Jun;61(3):200-207[↩]
- Morikawa T, Okabayashi T, Shima Y, Sumiyoshi T, Kozuki A, Saisaka Y, Tokumaru T, Sui K, Iwata J, Matsumoto M, Morita S, Nishioka Y. Adenomyomatosis Concomitant with Primary Gallbladder Carcinoma. Acta Med. Okayama. 2017 Apr;71(2):113-118[↩]