What is dermatofibroma
Dermatofibroma also called cutaneous fibrous histiocytoma, is a common overgrowth of the fibrous tissue of the skin situated in the dermis (the deeper of the two main layers of the skin). Dermatofibroma is quite harmless and will not turn into a cancer. Dermatofibromas are common, benign skin neoplasms composed of collagen, macrophages (histiocytes), capillaries, and fibroblasts. Dermatofibroma has no known cause. Dermatofibromas can be found anywhere on your body, but they most often develop on the extremities, with the lower legs being the most common place to find them. Dermatofibromas are usually round, brownish to red-purple, and feel like hard lumps under the skin. While dermatofibromas are usually painless, there can be some itching or tenderness to touch.
Dermatofibromas are most commonly seen in females and can occur at any age, with most growths beginning in teens and young adults. They do tend to occur in families; if a child has a dermatofibroma, it is likely that a close relative has at least one as well.
Dermatofibromas are a common skin lesion in almost all populations, with one study reporting that they account for 3% of all dermatopathology laboratory specimens 1. The overall worldwide incidence is difficult to determine, as the vast majority of patients are asymptomatic and therefore many patients may never seek care for these lesions. These lesions are most common in patients in their 20s to their 40s. Most studies indicate a female predominance, with an incidence ranging from equivocal to only slightly higher in females too as high as twice as frequent in females as compared to males 2.
Dermatofibromas are benign lesions, but seek medical evaluation if a lesion begins to increase in size, becomes painful, or if large numbers of dermatofibromas in grouped or linear clusters are seen.
Anyone who develops a new lump in their skin, particularly if it is pigmented, should ask their doctor to have a look at it.
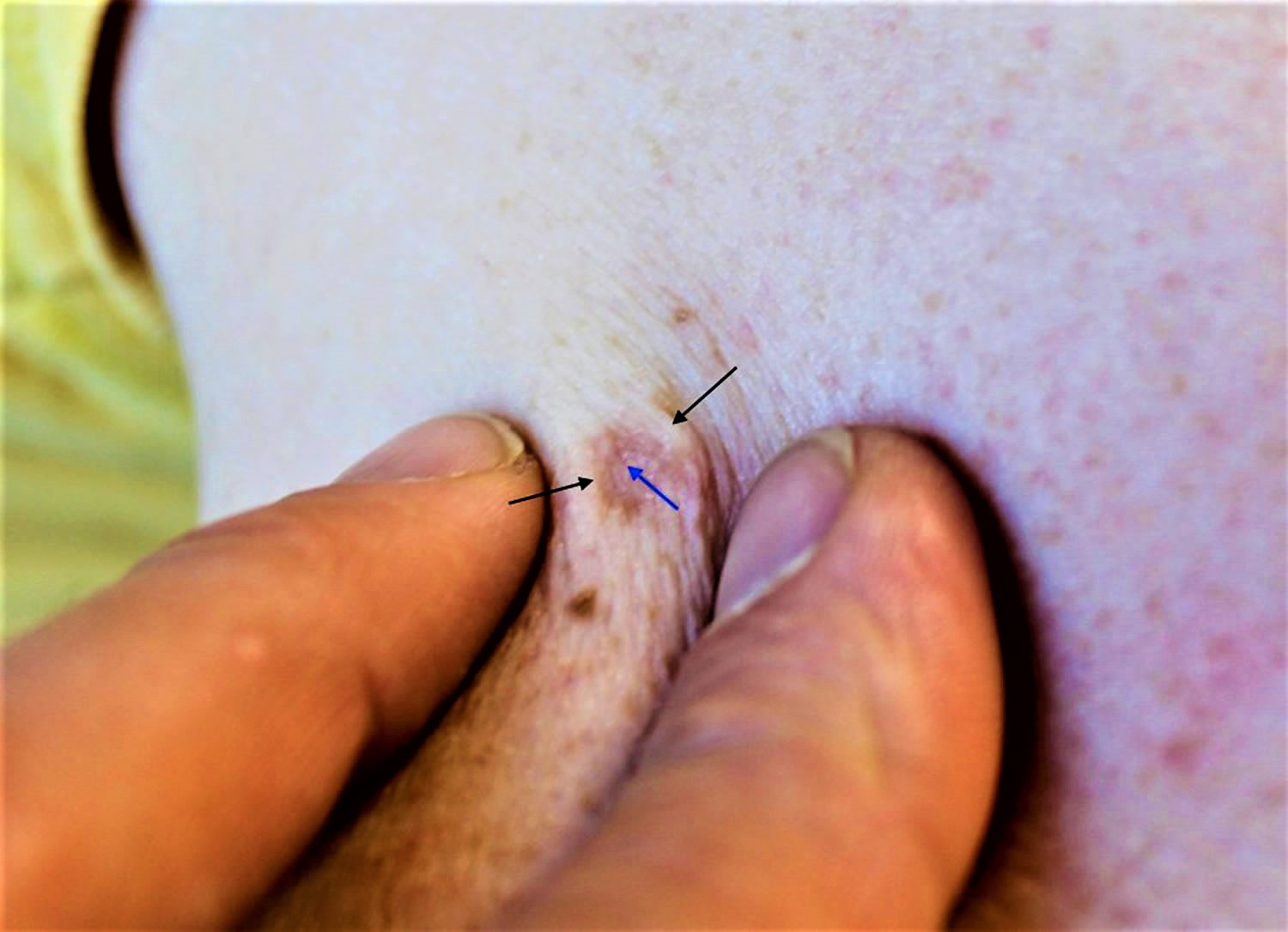
Figure 1. Dermatofibroma pinch test
Are dermatofibromas hereditary?
No.
Can a dermatofibroma be cured?
Yes, by removal under local anaesthetic with a small margin of surrounding normal skin. This reduces the chance of the dermatofibroma locally recurring.
Dermatofibroma causes
Dermatofibroma cause is unknown and remains a controversial topic 1. However, dermatofibromas often seem to appear after a minor injury to the skin such as a prick from a thorn or an insect bite. More often, there is no inciting event or trauma, and the dermatofibroma develops spontaneously 1. Interestingly, although they will develop spontaneously, spontaneous regression is not commonly observed, which may support an argument against a primarily reactive process in favor of a clonal or neoplastic model 1.
Dermatofibromas are firm, skin-colored or slightly pigmented papules or nodules. Dermatofibromas may be tender or pruritic (itchy) and they often persist for life. They are most common on the legs of women and usually appear in young adulthood. They may heal as depressed scars after several years.
Histologically, dermatofibromas represent a well-circumscribed proliferation of fibrohistiocytic spindle-shaped cells interspersed among thickened dermal collagen bundles. The epidermis may show some acanthosis with basal layer hyperpigmentation. Immunohistochemistry typically reveals positive staining with factor XIIIa.
Dermatofibromas are often solitary, though any individual may have more than one. Rarely, multiple eruptive dermatofibromas may occur in patients. MEDF is arbitrarily defined as the presence of a minimum of anywhere from 5 to 15 or more dermatofibromas developing in less than a 4-month period. Multiple eruptive dermatofibromas has been reported to occur in the setting of human immunodeficiency virus (HIV) infection; autoimmune disease, most frequently systemic lupus erythematosus; and neoplastic disease. Multiple clustered dermatofibroma is an entity where 15 or more dermatofibromas cluster together to form a plaque, most often on the lower half of the body in the first to third decades.
Dermatofibroma histopathology
Dermatofibromas have many histologic variants including cellular, epithelioid, lipidized, aneurysmal, monster cell, and atypical (to name only a few); but the most frequently diagnosed is the common fibrous histiocytoma or common dermatofibroma.
The common dermatofibroma is characterized histopathologically by a localized proliferation of spindle-shaped fibrous cells admixed with histiocytoid cells within the dermis. This proliferation is usually nodular in appearance, with spiculated, but moderately defined, borders that may have a pushing appearance in regards to the surrounding tissue. The spindle cells will form focally what is referred to as a “storiform” pattern, which describes a multi-centric whorling appearance of the elongated nuclei. There may be intermixed capillaries and lymphocytes or multinucleated giant cells. These proliferations are usually contained within the dermis, but it is not uncommon to observe a small portion of the lesion dipping down into the subcutaneous tissue along septal lines. A helpful and distinguishing characteristic is the presence of trapped collagen bundles or “collagen balls” within and between the fascicles of spindled fibrous cells. These entrapped collagen collections are more commonly found forming at the periphery of the lesion.
The overlying epidermis is usually separated by a clearly delineated and unaffected zone of separation, the “Grenz zone.” Typical reactive epidermis changes include hyperkeratosis and acanthosis. The epidermis also will often exhibit elongated rete ridges diving into the dermis with hyperpigmented basal keratinocytes, which is referred to as the “dirty feet” sign.
Arguably the most important entity to distinguish dermatofibromas from is the similar appearing, but much more worrisome, dermatofibrosarcoma protuberans (DFSP). These lesions are more typically much more cellular, have a more marked development of the storiform pattern, and will invade and involve the subcutis much more deeply, often entrapping fat as it dives and proliferates along the subcutaneous septae 3.
Dermatofibroma signs and symptoms
Dermatofibromas usually have no symptoms, but some people may be concerned about how they look.
Dermatofibromas are most often found on the arms and legs of women. They are small brown or reddish-brown mobile nodules, and they feel quite firm. They may be tender to touch. Many lesions demonstrate a “dimple sign,” where the central portion puckers as the lesion is compressed on the sides. They generally do not change in size. Occasionally they itch or hurt when touched or knocked. If they are on the legs, shaving the skin over them can cause bleeding.
What do dermatofibromas look like?
- Dermatofibromas are firm bumps that feel like small rubbery buttons lying just under the surface of the skin. They are seldom more than 1 cm across. They lie within the skin and so move with it. A dimple may appear over them when they are pinched.
- Size varies from 0.5–1.5 cm diameter; most lesions are 7–10 mm diameter.
- Their color ranges from pink to light brown in white skin, and dark brown to black in dark skin; some appear paler in the center.
- Dermatofibromas can crop up anywhere, but are most common on the lower legs of young or middle-aged adults and on the upper arms of women.
- Most people with a dermatofibroma will have only one; some people will have several; this may happen in individuals that have a disease that causes immune suppression (lupus, HIV, some cancers).
- Women get them more often than men.
- People may have 1 or up to 15 lesions.
- The skin dimples on pinching the lesion.
- They do not usually cause symptoms, but they are sometimes painful or itchy.
Dermatofibroma diagnosis
A doctor can usually identify a dermatofibroma easily by the way it looks. However, if there is doubt about the diagnosis, or worries over the possibility of skin cancer, the bump can be removed under a local aaesthetic and looked at under the microscope.
The most important evaluation is biopsy with histopathologic examination. These lesions can be reliably diagnosed through this method along with the correlated clinical exam. If these lesions are evaluated prior to biopsy by sonography, they should appear as an avascular lesion within the dermis which will often have superficial subcutis involvement and spiculated margins that are not well defined. The size and margins of these lesions correlate well on the histopathologic exam with sonographic findings 4.
Dermatofibroma treatment
Dermatofibroma is benign; therefore, reassurance is often all that is needed. Dermatofibromas may spontaneously go away, although in many cases they can last indefinitely. However, as they are harmless and cause little trouble, no treatment is usually needed apart from an accurate diagnosis and reassurance.
- Often symptomatic, protruding dermatofibromas can be reduced in size by freezing with liquid nitrogen (cryotherapy) but it will leave a scar and the lesion may recur or steroid injections to the lesion. In darker-skinned individuals, freezing with liquid nitrogen and steroid injection of may cause pigmentary change that is usually temporary.
- Surgical excision can be performed, but due to the high incidence of recurrence, the use of topical steroids or steroid injections into the lesion post-excision is often necessary. Excision (surgical removal) under local anesthetic will always leave a scar, which may be as obvious as the original lesion.
- Dermatofibromas can improve slightly (get flatter) with intra-lesional steroid injections (steroid injections into the lesion).
- Some lasers, including carbon dioxide lasers (which work to flatten the lesion) and pulsed dye lasers (which target the blood supply to the lesion) have shown good results but may also scar.
Complications of dermatofibroma are primarily related to surgical removal, including bleeding, infection, scar/disfigurement, and need for further procedures.
- Myers DJ, Fillman EP. Dermatofibroma. [Updated 2019 Feb 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470538[↩][↩][↩][↩]
- Buehler D, Weisman P. Soft Tissue Tumors of Uncertain Histogenesis: A Review for Dermatopathologists. Clin. Lab. Med. 2017 Sep;37(3):647-671[↩]
- Agarwal A, Gopinath A, Tetzlaff MT, Prieto VG. Phosphohistone-H3 and Ki67: Useful Markers in Differentiating Dermatofibroma From Dermatofibrosarcoma Protuberans and Atypical Fibrohistiocytic Lesions. Am J Dermatopathol. 2017 Jul;39(7):504-507[↩]
- Kelati A, Aqil N, Baybay H, Gallouj S, Mernissi FZ. Beyond classic dermoscopic patterns of dermatofibromas: a prospective research study. J Med Case Rep. 2017 Sep 20;11(1):266.[↩]