What is melioidosis
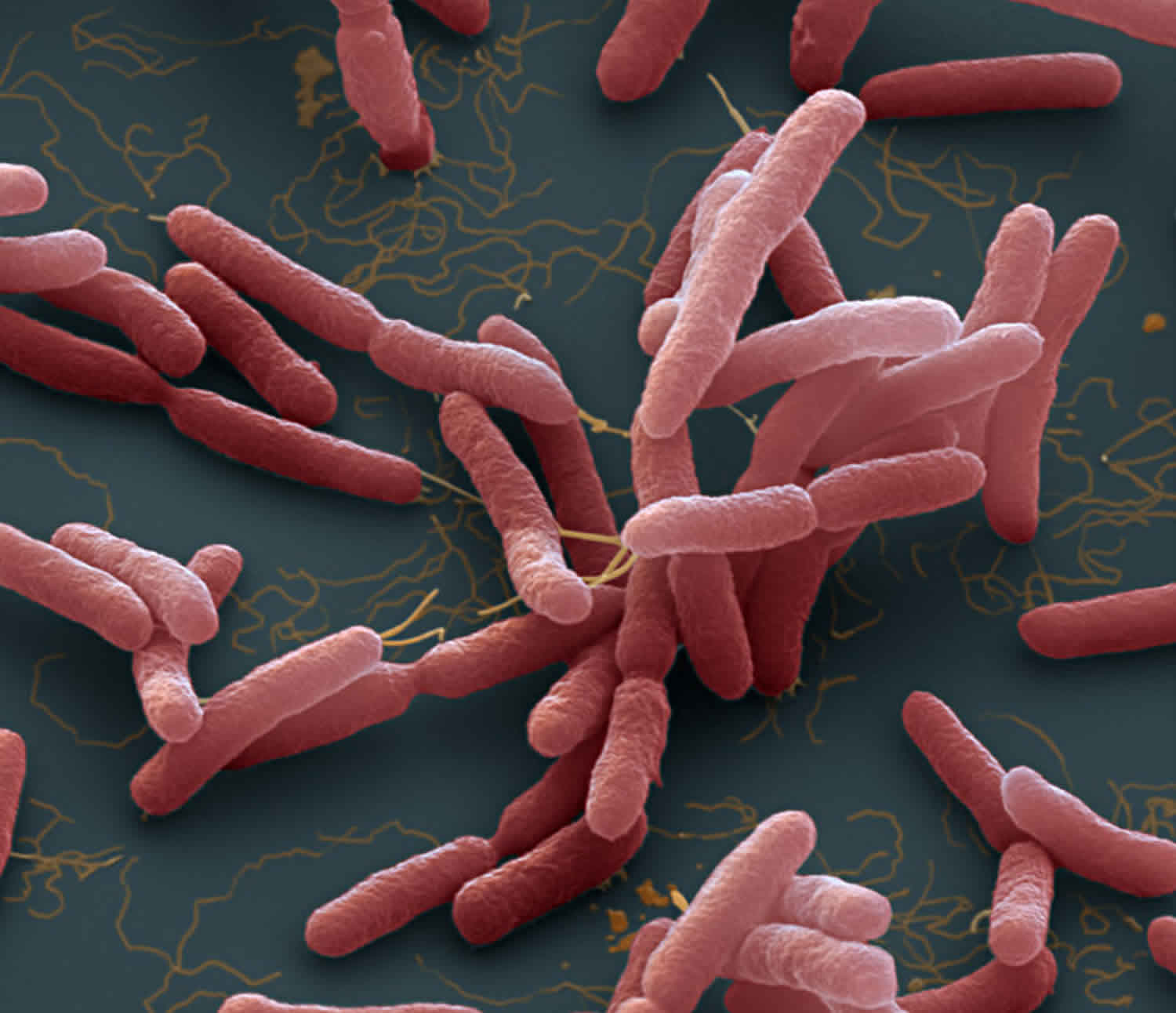
Melioidosis also called Whitmore’s disease, is an infectious disease caused by the bacteria Burkholderia pseudomallei that are commonly found in the soil and water, that can infect humans or animals 1. Melioidosis is a rare disease in the United States, but it is common in tropical or subtropical areas of the world, including Southeast Asia, Africa, and northern Australia where it is widespread 2.
In the United States, confirmed cases reported in previous years have ranged from zero to five and have occurred among travelers and immigrants coming from places where the disease is widespread.
Moreover, it has been found among troops of all nationalities that have served in areas with widespread disease.
The greatest numbers of melioidosis cases are reported in:
- Thailand
- Malaysia
- Singapore
- Northern Australia
Though rarely reported, cases are thought to frequently occur in:
- Papua New Guinea
- Most of the Indian subcontinent
- Southern China
- Hong Kong
- Taiwan
- Vietnam
- Indonesia
- Cambodia
- Laos
- Myanmar (Burma)
Outside of Southeast Asia and Australia, cases have been reported in:
- The South Pacific (New Caledonia)
- Sri Lanka
- Mexico
- El Salvador
- Panama
- Ecuador
- Peru
- Guyana
- Puerto Rico
- Martinique
- Guadeloupe
- Brazil
- Parts of Africa and the Middle East
Melioidosis is spread to humans and animals through direct contact with the contaminated contaminated water and soil.
Melioidosis signs and symptoms can vary greatly and may mimic those of tuberculosis (TB) or common forms of pneumonia 3. Signs and symptoms may include pain or swelling, fever, abscess, cough, high fever, headache, trouble breathing, and more. Although healthy people can also experience signs and symptoms of the disease, people with certain conditions like diabetes, liver disease, kidney disease, lung disease, thalassemia, cancer, or certain autoimmune diseases are more severely affected. Melioidosis diagnosis is made by collecting blood, sputum, urine, or pus samples and growing the bacteria 4. Current treatment is divided into two stages: an intravenous (IV) antibiotic stage and oral antibiotic maintenance stage to prevent recurrence 4.
Melioidosis transmission
While melioidosis infection has taken place all over the world, Southeast Asia and northern Australia are the areas in which it is primarily found. People can get Melioidosis through direct contact with contaminated soil and surface waters.
Humans and animals are believed to acquire the infection by inhalation of contaminated dust or water droplets, ingestion of contaminated water, and contact with contaminated soil, especially through skin abrasions.
It is very rare for people to get the disease from another person. While a few cases have been documented, contaminated soil and surface water remain the primary way in which people become infected.
Besides humans, many animal species are susceptible to melioidosis, including:
- Sheep
- Goats
- Swine
- Horses
- Cats
- Dogs
- Cattle
Risk factor for melioidosis
Although healthy people may get melioidosis, the major risk factors are:
- Diabetes
- Liver disease
- Renal disease
- Thalassemia
- Cancer or another immune-suppressing condition not related to HIV
- Chronic Lung disease (such as cystic fibrosis, chronic obstructive pulmonary disease (COPD), and bronchiectasis).
Melioidosis prevention
In areas where the melioidosis disease is widespread, contact with contaminated soil or water can put people at risk for melioidosis.
However, in these areas, there are things that certain groups of people can do to help minimize the risk of exposure:
- Persons with open skin wounds and those with diabetes or chronic renal disease are at increased risk for melioidosis and should avoid contact with soil and standing water.
- Those who perform agricultural work should wear boots, which can prevent infection through the feet and lower legs.
- Health care workers can use standard contact precautions (mask, gloves, and gown) to help prevent infection.
Melioidosis symptoms
There are several types of melioidosis infection, each with their own set of symptoms.
However, it is important to note that melioidosis has a wide range of signs and symptoms that can be mistaken for other diseases such as tuberculosis or more common forms of pneumonia.
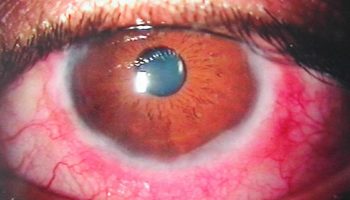
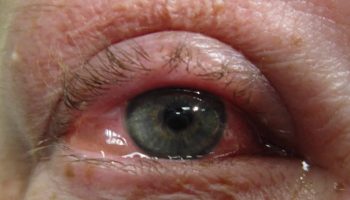
Localized Infection:
- Localized pain or swelling
- Fever
- Ulceration
- Abscess
Pulmonary Infection:
- Cough
- Chest pain
- High fever
- Headache
- Anorexia
Bloodstream Infection:
- Fever
- Headache
- Respiratory distress
- Abdominal discomfort
- Joint pain
- Disorientation
Disseminated Infection:
- Fever
- Weight loss
- Stomach or chest pain
- Muscle or joint pain
- Headache
- Seizures
The time between an exposure to the Burkholderia pseudomallei bacteria that causes melioidosis disease and the emergence of symptoms is not clearly defined, but may range from one day to many years; generally symptoms appear two to four weeks after exposure.
Melioidosis diagnosis
Microbiological culture remains the standard method for the diagnosis of melioidosis, but this method is not optimal because the sensitivity may be as low as 60% 5. Culture specimens should be obtained from blood, throat, urine, respiratory secretions, pus, and surface lesions as appropriate, for all patients with suspected cases. Any positive culture is considered diagnostic for melioidosis because B. pseudomallei is not considered to be a member of the colonizing microbiota. PCR to detect Burkholderia pseudomallei and Burkholderia mallei in clinical samples has been described, but is less sensitive than culture 6.
Gram staining and examination under light microscopy of clinical specimens or bacterial colonies can identify gram-negative bacilli with a granular or safety pin appearance, but this appearance is not specific for Burkholderia pseudomallei. Gram-negative organisms that are oxidase positive, gentamicin- and colistin-resistant, and susceptible to amoxicillin/clavulanic acid, also known as co-amoxiclav, should be strongly suspected to be Burkholderia pseudomallei. During a public health emergency, or where Burkholderia pseudomallei may be of high prevalence in the community, a selective medium such as Ashdown agar 7 that will suppress overgrowth of normal microbiota in nonsterile specimens (e.g., throat swabs) should be used for suspected cases. However, rare gentamicin-susceptible Burkholderia pseudomallei isolates exist (1 in 1,000), which will not grow on Ashdown agar 8.
Commercial Burkholderia cepacia agar is a good alternative if Ashdown agar is not available 9. Bacterial colonies are usually visible after 24 hour. Colonies grown on Ashdown agar might have a violet or purple rugose, cornflower-like appearance. Colonies on nonselective media can vary in appearance and can be rugose or smooth. After positive identification is established, isolates should be collected for strain characterization and epidemiologic information as well as to aid forensic data investigations.
Biochemical tests such as the API 20NE (bioMérieux Inc., Durham, NC, USA) and Vitek II (bioMérieux Inc.) might help with confirmation, but misidentifications by both systems have been reported 10. Bacterial identification methods that use assays with polyclonal or monoclonal antibodies against B. pseudomallei and B. mallei have been described, e.g., a direct immunofluorescence assay that can be applied directly to clinical specimens and has been reported to have a sensitivity of 66% 11 and a latex agglutination assay that can be used to identify colonies (20). Both of these assays use in-house reagents developed in Thailand that are not commercially available but would be useful during a public health emergency for which there is a need to quickly distinguish between melioidosis and other illnesses that produce similar signs and symptoms.
Time to positive culture result (which is correlated with the level of bacteremia) is a prognostic indicator of death. Melioidosis results in a mortality rate of 74% if blood cultures show positive results within 24 h, compared with 41% mortality rate if >24 h pass before blood cultures become positive 12.
Melioidosis treatment
When a melioidosis infection is diagnosed, the disease can be treated with the use of appropriate medication.
The type of infection and the course of treatment will impact long-term outcome. Treatment generally starts with intravenous (within a vein) antimicrobial therapy for 10-14 days, followed by 3-6 months of oral antimicrobial therapy.
Antimicrobial agents that have been effective against melioidosis include:
- Intravenous therapy consists of:
- Ceftazidime administered every 6-8 hours
OR - Meropenem administered every 8 hours
- Ceftazidime administered every 6-8 hours
- Oral antimicrobial therapy consists of:
- Trimethoprim-sulfamethoxazole taken every 12 hours
OR - Amoxicillin/clavulanic acid (co-amoxiclav) taken every 8 hours
- Trimethoprim-sulfamethoxazole taken every 12 hours
Patients with penicillin allergies should notify their doctor, who can prescribe an alternative treatment course.
In 2010, HHS convened a workshop with internationally recognized leaders in the field of Burkholderia species (the species of germ that causes melioidosis, glanders and other related infections) and clinicians with expertise in treating Burkholderia. Workshop attendees recommended treatment regimens for and post-exposure prophylaxis for melioidosis and glanders. More details on the recommendations can be found in the summary, published in CDC’s Emerging Infectious Diseases journal 13.
- This Germ Can Live Decades In Distilled Water, Kill Humans In 48 Hours. https://www.npr.org/sections/goatsandsoda/2016/01/11/462416728/this-germ-can-live-decades-in-distilled-water-kill-humans-in-48-hours[↩]
- Melioidosis. https://www.cdc.gov/melioidosis[↩]
- Melioidosis Signs and Symptoms. https://www.cdc.gov/melioidosis/symptoms/index.html[↩]
- Melioidosis. http://www.checkorphan.org/diseases/meliodosis[↩][↩]
- Limmathurotsakul D, Jamsen K, Arayawichanont A, Simpson JA, White LJ, Lee SJ, Defining the true sensitivity of culture for the diagnosis of melioidosis using Bayesian latent class models. PLoS ONE. 2010;5:e12485[↩]
- Bowers JR, Engelthaler DM, Ginther JL, Pearson T, Peacock SJ, Tuanyok A, BurkDiff: a real-time PCR allelic discrimination assay for Burkholderia pseudomallei and B. mallei. PLoS ONE. 2010;5:e15413[↩]
- Ashdown LR. An improved screening technique for isolation of Pseudomonas pseudomallei from clinical specimens. Pathology. 1979;11:293–7[↩]
- Trunck LA, Propst KL, Wuthiekanun V, Tuanyok A, Beckstrom-Sternberg SM, Beckstrom-Sternberg JS, Molecular basis of rare aminoglycoside susceptibility and pathogenesis of Burkholderia pseudomallei clinical isolates from Thailand. PLoS Negl Trop Dis. 2009;3:e519[↩]
- Peacock SJ, Chieng G, Cheng AC, Dance DA, Amornchai P, Wongsuvan G, Comparison of Ashdown’s medium, Burkholderia cepacia medium, and Burkholderia pseudomallei selective agar for clinical isolation of Burkholderia pseudomallei. J Clin Microbiol. 2005;43:5359–61[↩]
- Amornchai P, Chierakul W, Wuthiekanun V, Mahakhunkijcharoen Y, Phetsouvanh R, Currie BJ, Accuracy of Burkholderia pseudomallei identification using the API 20NE system and a latex agglutination test. J Clin Microbiol. 2007;45:3774–6[↩]
- Wuthiekanun V, Desakorn V, Wongsuvan G, Amornchai P, Cheng AC, Maharjan B, Rapid immunofluorescence microscopy for diagnosis of melioidosis. Clin Diagn Lab Immunol. 2005;12:555–6[↩]
- Tiangpitayakorn C, Songsivilai S, Piyasangthong N, Dharakul T. Speed of detection of Burkholderia pseudomallei in blood cultures and its correlation with the clinical outcome. Am J Trop Med Hyg. 1997;57:96–9[↩]
- Workshop on Treatment of and Postexposure Prophylaxis for Burkholderia pseudomallei and B. mallei Infection, 2010. Volume 18, Number 12—December 2012 https://wwwnc.cdc.gov/eid/article/18/12/12-0638_article[↩]