Child Pugh classification
Child-Pugh scoring system also known as the Child‐Turcotte‐Pugh score, is a major prognostic scoring systems in patients with chronic liver disease and liver cirrhosis 1. However, the Model for End-Stage Liver Disease (MELD) score is now used for allocation in liver transplantation waiting lists, replacing Child‐Turcotte‐Pugh score 2. Liver transplantation is now a standard of care therapy for well selected patients with end-stage liver disease, acute liver failure, acute on chronic liver failure and hepatocellular carcinoma (HCC) 3.
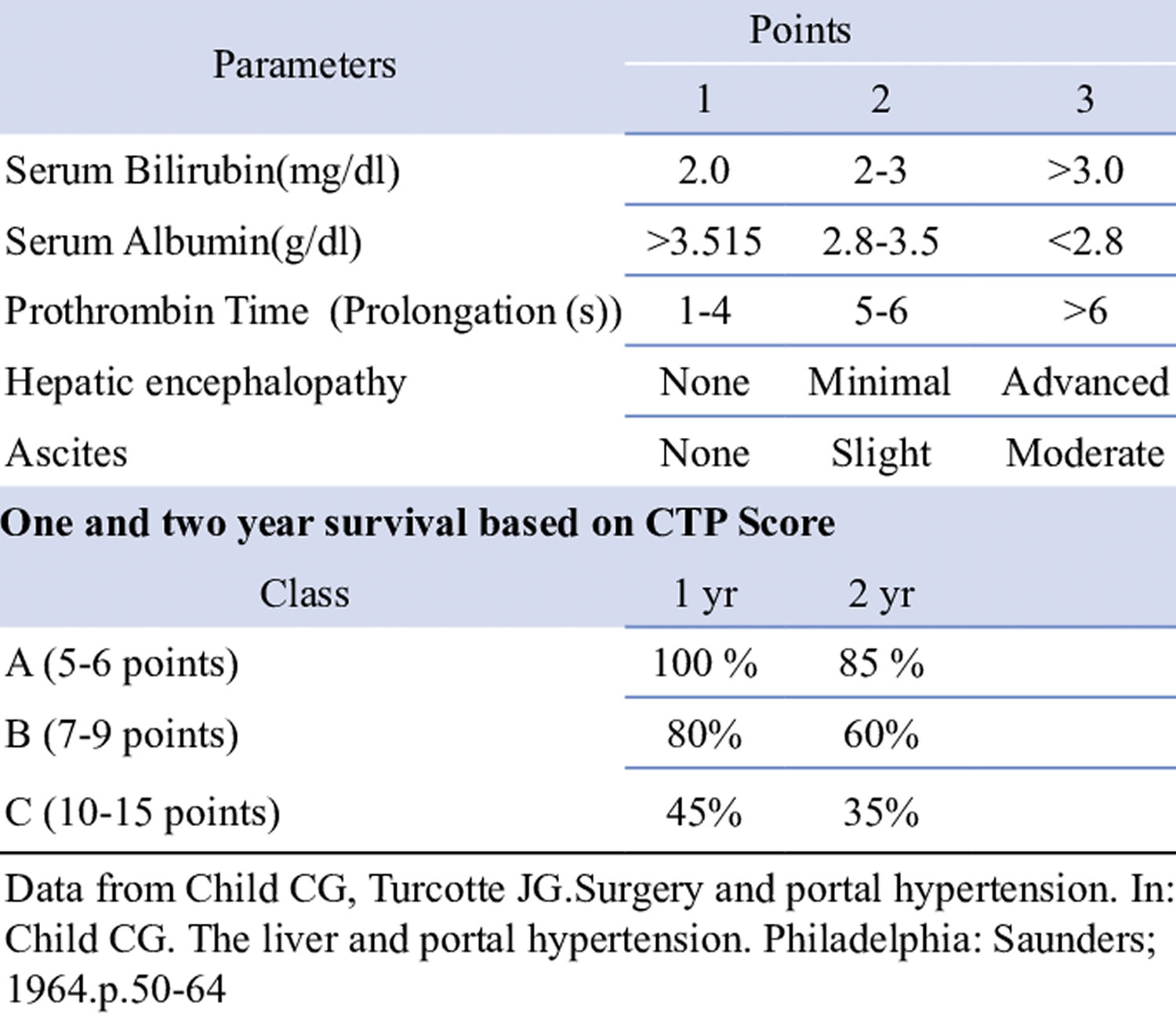
In 1964, Child and Turcotte 4 published a classification to assess the operative risk in cirrhotic patients who recovered from variceal bleeding, undergoing portosystemic shunt surgery. Child-Turcotte score included two continuous variables (bilirubin and albumin) and three discrete variables (ascites, encephalopathy, and nutritional status) which were empirically selected because they were felt to have their own influence on the prognosis in this context 5. Child-Turcotte score classifies patients in class A, B or C in relation to best (A), moderate (B), or worse (C) prognosis.
In 1973, Pugh et al. 6 used a modified version of Child-Turcotte classification for patients undergoing surgical transection for esophageal varices. They replaced nutritional status with prothrombin time and assigned a score ranging from 1 to 3 to each variable. Subsequently, this classification was used to predict the outcome of surgery in cirrhotic patients in general, and more recently, to stratify patients on the waiting list for liver transplantation. Similar to the original Child and Turcotte’s grading, neither the division of the grades nor the scoring system was validated statistically. However, a limitation comes from the fact that prothrombin time can also be expressed as either a percentage of normal (prothrombin index) or as international normalized ratio (INR), this latter being now the reference in many countries. The original cut-off values of 4 and 6 seconds for prothrombin time prolongation correspond approximately to a prothrombin index of 50% and 40%, respectively 7. These same values roughly correspond to an INR of 1.7 and 2, respectively. Child-Pugh score corresponds to the total of points for each item. According to the sum of these points, patients can be categorized into Child-Pugh grades A (5 to 6 points), B (7 to 9 points), or C (10 to 15 points). The variables included in Child-Pugh score are not specific markers of the synthesis (albumin and prothrombin) and elimination (bilirubin) functions of the liver. Indeed, changes in serum albumin may be also related to increased vascular permeability 8, especially in cases of sepsis, and large-volume ascites 9. Similarly, bilirubin can be increased as a consequence of impaired renal function, hemolysis, or sepsis 10. Prolonged prothrombin time can be a consequence of an intravascular activation of coagulation during sepsis 11. Overall, the individual components of the Child-Pugh score encompass a broader spectrum of conditions than the single impairment of “liver function.” Child-Pugh score as a whole is also a marker of the multiorgan changes resulting from cirrhosis.
Table 1. Child Pugh classification
| Parameter | Points | ||
|---|---|---|---|
| 1 | 2 | 3 | |
| Albumin (g/dL) | >3.5 | 3.5–2.8 | <2.8 |
| Bilirubin (mg/dL) | <2 | 2–3 | >3 |
| Ascites | Absent | Slight | Moderate |
| Encephalopathy | None | Glasgow Coma Scale 1–2 | Glasgow Coma Scale 3–4 |
| Prothrombin time (PT) (INR) | <1.7 | 1.8–2.3 | >2.3 |
| Child-Pugh score | A | B | C |
| Points | 5–6 | 7–9 | 10–15 |
Child-Pugh score interpretation
Child-Turcotte-Pugh score is widely used to prognosticate patients with cirrhosis (see Tables 1 and 2). Although empirically derived, the Child-Turcotte-Pugh score has been shown to accurately predict outcomes in patients with cirrhosis and portal hypertension 12. The Child-Turcotte-Pugh score scoring system incorporates five parameters: serum bilirubin, serum albumin, prothrombin time, ascites, and grade of encephalopathy 13. Based on the sum of the points from these five parameters, the patients are categorized into one of three Child-Turcotte-Pugh score classes: A, B, or C. Studies involving cirrhotic patients have shown that a patients’ Child-Turcotte-Pugh score score can estimate risk of death at 3-months and 1-year and 2-year survival. The two year survival of cirrhotic patients in Child-Turcotte-Pugh score class A, B, and C are 90%, 70% and 35% respectively 13. American Association for the Study of Liver Diseases recommends referral for liver transplantation evaluation in patients with cirrhosis and a Child-Turcotte-Pugh score of more than 7 14.
Over many years, the routine use of these classifications have revealed some problems. First, both the degree of ascites and encepahlopathy are subjective assessments evaluated by physical examination alone 15. The widespread use of ultrasonography has led to more sensitive detection of ascites, but it is unclear how ascites diagnosed by ultrasonography alone is being categorized by various authors. Hepatic encephalopathy is often assessed by psychometric testing or slowing of frequency on an electroencephalography (EEG). It is not clear how these abnormalities are fitted into Child‐Turcotte‐Pugh classification 15. Secondly, both ascites and hepatic encephalopathy can be influenced by therapy such as diuretics, albumin infusion and lactulose and it is not clear if ascites and hepatic encephalopathy are scored at their best, or worst, or independent of specific therapy.
Several studies have shown that Child-Pugh score is an independent prognostic marker in the settings of ascites 16, ruptured esophageal varices 17, alcoholic cirrhosis 18, hepatitis C virus- (HCV-) related cirrhosis 19, primary biliary cirrhosis (PBC) 20, primary sclerosing cholangitis 21, and Budd-Chiari syndrome 22. Child-Pugh score, which can be easily calculated at the bedside, has been widely used for selecting candidates for resection of hepatocellular carcinoma 23 and nonhepatic surgery 24.
Attempts have been made to improve the accuracy of Child-Pugh score by incorporating other markers of liver function (such as the clearance of galactose, indocyanine green, aminopyrine, and lidocaine) 25. However, these additional markers had a limited value. The incorporation of conventional markers of nutritional status to Child-Pugh score also had a limited value 26.
Since the five variables of Child-Pugh score were selected empirically, it can be anticipated that not all are independent predictors of prognosis. For example, albumin and prothrombin time are somewhat redundant. Including both variables in a single score may result in overweighting their own influence.
The cut-off value for each variable has been empirically selected. There is no evidence that moving from one class to the next one translates into a proportional change in mortality risk. As an example, patients with serum bilirubin above 100 μmol/L may be under-scored with Child-Pugh, because the limit for the upper class of bilirubin is only 51 mmol/L. This ceiling effect of discrete classes does not exist with continuous variables. In addition, the limits for qualitative variables (ascites and encephalopathy) are still vague. They may be influenced by subjective interpretation.
The five variables of Child-Pugh score are empirically given the same weight, which is also questionable. Multivariate analysis has shown that the proper weight of predictive factors is quite variable. For example, the weight of INR is three times as high as that of bilirubin in the Model for End-Stage Liver Disease (MELD) score 27.
Child-Pugh score does not take into account specific variables, serum creatinine in particular, which have been shown to have a determinant impact on the prognosis of cirrhosis 16. Similarly, it has been shown that the addition of markers of portal hypertension, such as esophageal varices, portal blood velocity, and hepatic venous pressure gradient, would improve the accuracy of Child-Pugh score 28.
Finally, Child-Pugh score does not take into account the cause of cirrhosis and the possibility of stopping (or slowing) the damaging process to the liver. This limitation is especially relevant in patients with alcoholic cirrhosis or with hepatitis B virus- (HBV-) related cirrhosis with viral replication.
Table 2. Child-Turcotte-Pugh score
[Source 29 ]- D’Amico G., Garcia-Tsao G., Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: A systematic review of 118 studies. J. Hepatol. 2006;44:217–231. doi: 10.1016/j.jhep.2005.10.013 https://doi.org/10.1111/j.1365-2036.2005.02691.x[↩]
- Kim WR, Biggins SW, Kremers WK, et al. Hyponatremia and mortality among patients on the liver-transplant waiting list. N Engl J Med. 2008;359(10):1018–1026. doi:10.1056/NEJMoa0801209 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4374557[↩]
- Fox AN, Brown RS Jr. Is the patient a candidate for liver transplantation? Clin Liver Dis. 2012; 16(2):435-48.[↩]
- Child C, Turcotte J. The liver and portal hypertension. In: Child CI, ed. Surgery and Portal Hypertension. Philadelphia, USA: W. B. Saunders, 1964: 50–8.[↩]
- Durand F, Valla D. Assessment of the prognosis of cirrhosis: Child-Pugh versus MELD. J Hepatol 2005;42(suppl):S100-S107[↩]
- Pugh R, Murray‐lyon I, Dawson J. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg 1973; 60: 646–9.[↩]
- Assessment of Prognosis of Cirrhosis. https://www.medscape.com/viewarticle/572659_3[↩]
- Fleck A, Raines G, Hawker F, et al. Increased vascular permeability: a major cause of hypoalbuminaemia in disease and injury. Lancet 1985;1:781-784[↩]
- Henriksen JH, Parving HH, Christiansen L, et al. Increased transvascular escape rate of albumin during experimental portal and hepatic venous hypertension in the pig: relation to findings in patients with cirrhosis of the liver. Scand J Clin Lab Invest 1981;41:289-299[↩]
- Moseley RH. Sepsis and cholestasis. Clin Liver Dis 2004; 8:83-94[↩]
- Plessier A, Denninger MH, Consigny Y, et al. Coagulation disorders in patients with cirrhosis and severe sepsis. Liver Int 2003;23:440-448[↩]
- Pugh RN, Murray-Lyon IM, Dawson JL, et al. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg 1973; 60(8):646–9.[↩]
- Yu AS, Keeffe EB. Liver transplantation. In: Zakim D, Boyer TD, editors. Hepatology: a textbook of liver disease. 4th edition. Philadelphia: Elsevier; 2003. p. 1617–56.[↩][↩]
- Martin et al. Evaluation for Liver Transplantation in Adults: 2013 Practice Guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. HEPATOLOGY 2014; 59(3):1144-65.[↩]
- CHOLONGITAS, E. , PAPATHEODORIDIS, G. V., VANGELI, M. , TERRENI, N. , PATCH, D. and BURROUGHS, A. K. (2005), Systematic review: the model for end‐stage liver disease – should it replace Child‐Pugh’s classification for assessing prognosis in cirrhosis?. Alimentary Pharmacology & Therapeutics, 22: 1079-1089. doi:10.1111/j.1365-2036.2005.02691.x https://doi.org/10.1111/j.1365-2036.2005.02691.x[↩][↩]
- Fernandez-Esparrach G, Sanchez-Fueyo A, Ginès P, et al. A prognostic model for predicting survival in cirrhosis with ascites. J Hepatol 2001;34:46-52[↩][↩]
- Merkel C, Bolognesi M, Sacerdoti D, et al. The hemodynamic response to medical treatment of portal hypertension as a predictor of clinical effectiveness in the primary prophylaxis of variceal bleeding in cirrhosis. Hepatology 2000;32:930-934[↩]
- Gluud C, Henriksen JH, Nielsen G. Prognostic indicators in alcoholic cirrhotic men. Hepatology 1988;8:222-227[↩]
- Planas R, Balleste B, Alvarez MA, et al. Natural history of decompensated hepatitis C virus-related cirrhosis: a study of 200 patients. J Hepatol 2004;40:823-830[↩]
- van Dam GM, Gips CH, Reisman Y, et al. Major clinical events, signs and severity assessment scores related to actual survival in patients who died from primary biliary cirrhosis: a long-term historical cohort study. Hepatogastroenterology 1999;46:108-115[↩]
- Shetty K, Rybicki L, Carey WD. The Child-Pugh classification as a prognostic indicator for survival in primary sclerosing cholangitis. Hepatology 1997;25:1049-1053[↩]
- Zeitoun G, Escolano S, Hadengue A, et al. Outcome of Budd-Chiari syndrome: a multivariate analysis of factors related to survival including surgical portosystemic shunting. Hepatology 1999;30:84-89[↩]
- Bruix J, Sherman M. Management of hepatocellular carcinoma. Hepatology 2005;42:1208-1236[↩]
- Friedman LS. The risk of surgery in patients with liver disease. Hepatology 1999;29:1617-1623[↩]
- Testa R, Valente U, Risso D, et al. Can the MEGX test and serum bile acids improve the prognostic ability of Child-Pugh’s score in liver cirrhosis? Eur J Gastroenterol Hepatol 1999;11:559-563[↩]
- Merli M, Riggio O, Dally L. Does malnutrition affect survival in cirrhosis? PINC (Policentrica Italiana Nutrizione Cirrosi). Hepatology 1996;23:1041-1046[↩]
- Malinchoc M, Kamath PS, Gordon FD, et al. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology 2000;31:864-871[↩]
- Salerno F, Borroni G, Moser P, et al. Prognostic value of the galactose test in predicting survival of patients with cirrhosis evaluated for liver transplantation: a prospective multicenter Italian study. AISF Group for the Study of Liver Transplantation. Associazione Italiana per lo Studio del Fegato. J Hepatol 1996;25:474-480[↩]
- Panackel, Charles & Ganjoo, Naveen & Saif, Rehan & Jacob, Mathew. (2016). Decompensated Liver Disease: Liver Transplantation is the Best Option, Not the Last Option ORIGINAL RESEARCH. Kerala Medical Journal. 9. 17. [↩]