Gastric distension
Gastric distension is the enlargement of the stomach, and can be due to a number of causes. Physiologic (normal) gastric distension occurs when eating. Distension of the upper stomach stimulates the secretion of stomach acid, while distension of the lower stomach stimulates gastrin secretion 1. Distension of the stomach also stimulates the secretion of ghrelin 2.
Progressive gastric distension is a rare condition, which may lead to gastric wall ischemia and perforation. Gastric distension is often diagnosed late in the course of the illness after complications are already present. Early recognition, prompt referral and intervention has the potential to prevent adverse outcomes.
Gastric distension most commonly occurs as a postoperative complication. Benign causes include diabetes mellitus, trauma, resuscitation, electrolyte derangements, emotional stress, superior mesenteric artery syndrome, gallstone (duodenal bulb obstruction also known as Bouveret syndrome) and others (see causes below) 3. In patients with an eating disorder, the stomach may distend to extremely high volumes.
Ischemia and perforation as a result of gastric distension is extremely rare, as the stomach is well protected against ischemic events due to a generous collateral circulation. Chronicity in gastric distension may also play a protective role. Ischemia and perforation occur as a result of venous insufficiency, with the point of tension needed to cause mucosal ischemia documented as 14 mmHg 4.
Septic shock and multi-organ failure as a result of gastric perforation is invariably fatal 5.
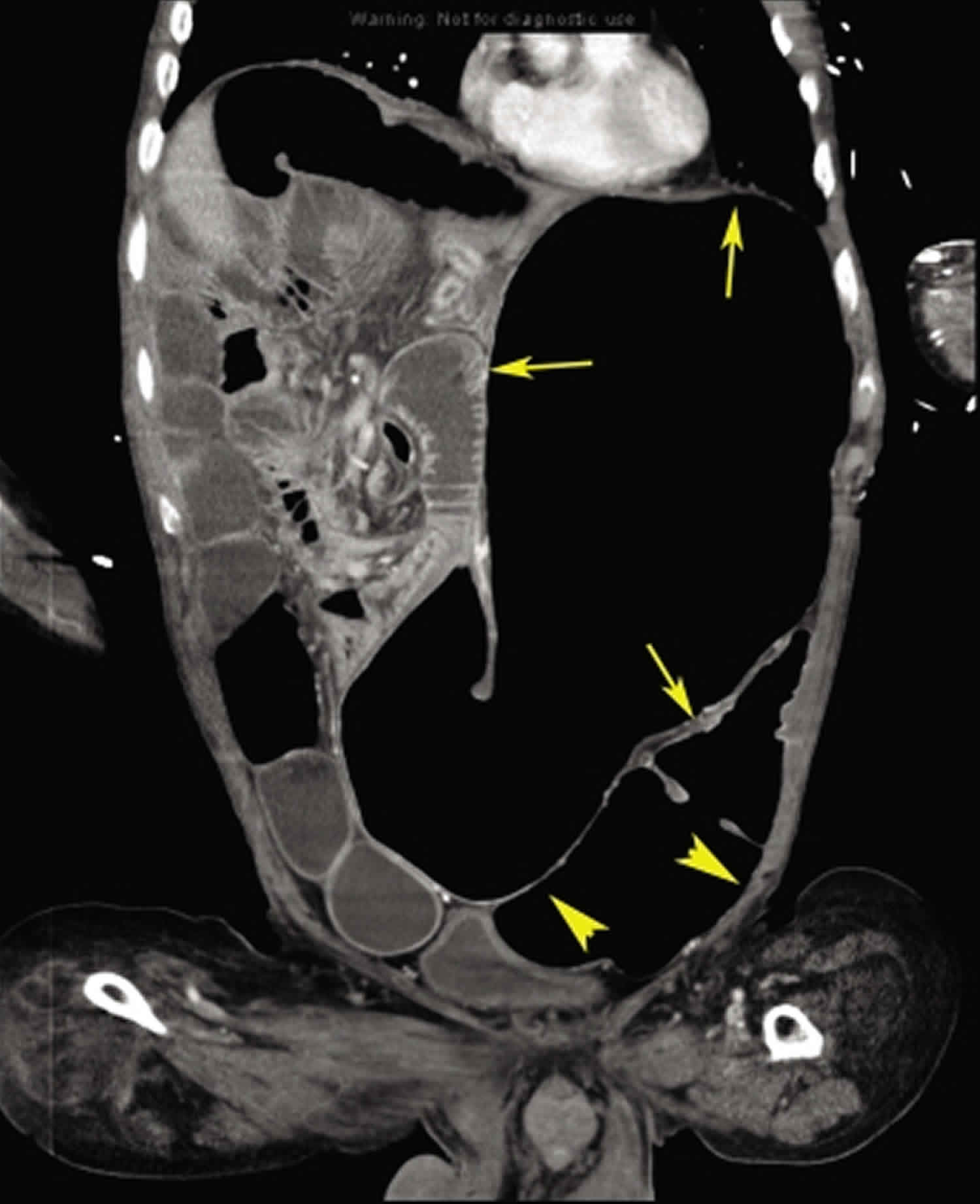
Figure 1. Gastric distension abdominal x-ray
Footnote: Abdominal radiograph showing massive gastric distension outlined by arrows.
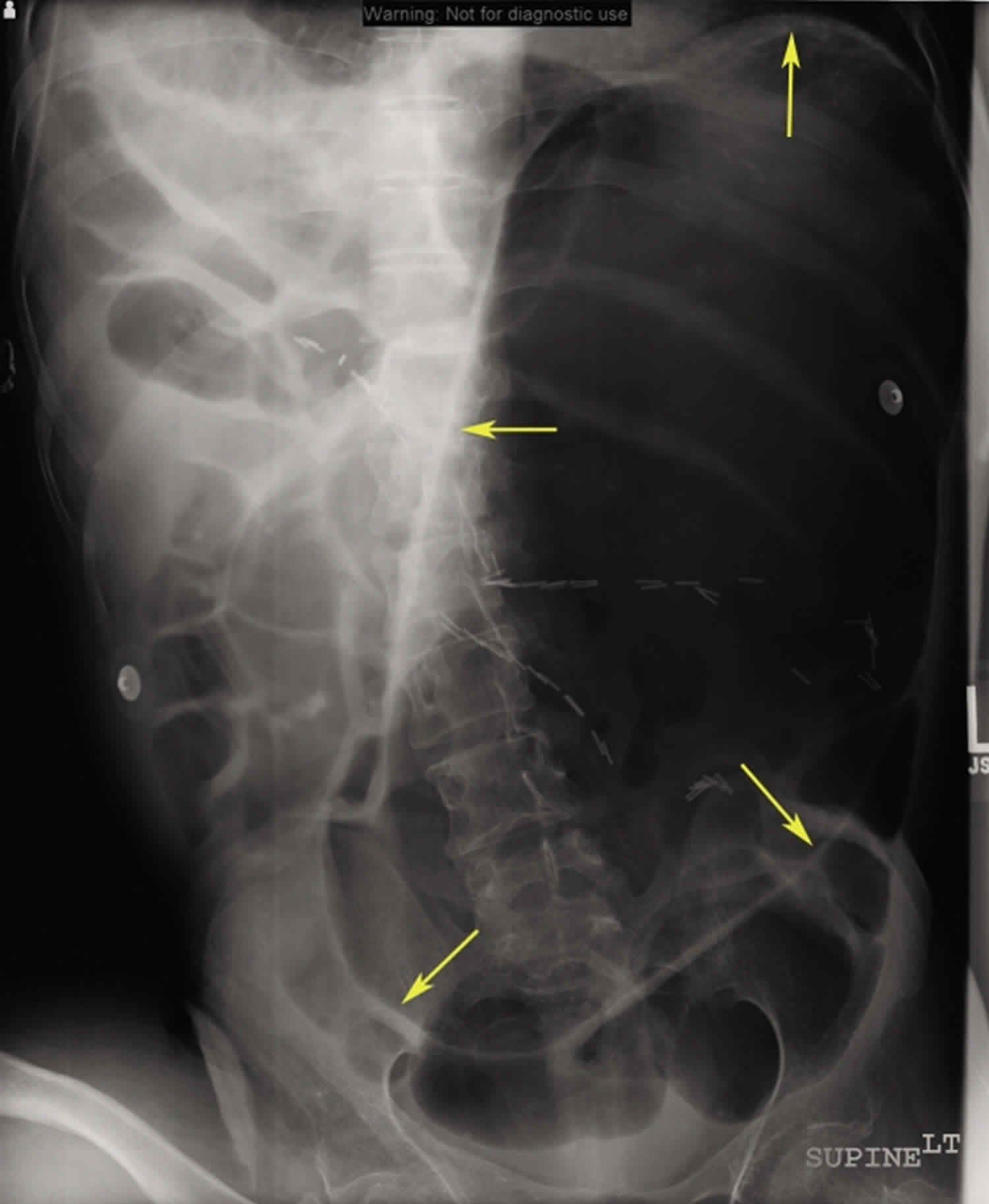
[Source 6 ]Figure 2. Gastric distension CT scan
Footnote: Coronal computed tomography demonstrating the massively dilated stomach (arrows) and dilated bowel loops (arrowheads).
[Source 6 ]Gastric distension causes
Causes of gastric distension 7:
Obstruction
- Luminal: bezoar, ingested foreign body, hyperphagia, gallstone
- Mural: Gastric tumors, Crohn stricture, tuberculosis, iatrogenic (slipped gastric banding, anastomotic stricture)
- Extrinsic: Lymphoma, other intraperitoneal tumors or metastases, annular pancreas, superior mesenteric artery syndrome
Dysmotility
- Autonomic neuropathy (diabetes mellitus, Parkinson disease), ileus, eating disorders.
- Radiation enteritis
- Drugs such as clonidine, opiates,
- Hypothyroidism
- Amyloidosis
- Scleroderma
- Multiple sclerosis
- Chronic intestinal pseudo-obstruction (CIPO) 6. Chronic intestinal pseudo-obstruction (CIPO) is a rare disorder of gastrointestinal motility characterized by repetitive/chronic symptoms of bowel obstruction in the absence of a mechanical or metabolic cause of obstruction 8. Abnormalities in the integrity of intestinal neural pathways, interstitial cells of Cajal, and smooth muscle cells of the gastrointestinal tract have been implicated in the causation of CIPO.
Gastric distension signs and symptoms
Common presenting symptoms include progressive abdominal distension and increasing abdominal pain accompanied by nonbilous vomiting. Hypotension, metabolic alkalosis and respiratory compromise may occur 9. If the stomach perforates, signs of generalised peritonitis may be obvious. A case has been reported of a patient with a massively distended stomach causing compromised blood flow in the abdominal aorta and leading to absent pulses in the lower limbs 10.
Gastric distension complications
Complications of gastric distension include massive dehydration with hypochloremic metabolic alkalosis and prerenal failure, and perforation with resultant sepsis, multi-organ failure and death. Complications are more likely in the elderly and already frail patients.
Gastric distension diagnosis
Diagnosis of gastric distension from clinical signs can be a challenge in the clinical setting, as symptoms may overlap those of several other conditions including bowel perforation and blood or fluid collections. A plain abdominal X-ray may show a distended stomach. An abdominal computed tomography (CT) scan may reveal a markedly distended stomach extending to the pelvic brim with compression of the small bowel.
Gastric distension treatment
The most important step in the initial management of patient with gastric distension is to promptly decompress the stomach with a nasogastric tube (NGT). This will halt venous congestion and potential ischemia and prevent aspiration. Fluid resuscitation with crystalloid should be initiated and titrated according to the patient’s volume status, degree of renal impairment and electrolyte depletion. An urgent referral should be made to a surgical unit. Consultation with a gastroenterologist may also be required and the potential for the need for a referral to an intensive care unit should be considered early.
- Brunicardi, Charles (2015). Schwartz’s Principles of Surgery (10 ed.). McGraw-Hill. pp. ch 26.[↩]
- Sleisenger and Fordtran’s Gastrointestinal and Liver Disease (10 ed.). Saunders. 2016. pp. 130–147.[↩]
- Kashyap AS, Chopra D, Anand KP, Arora S, Kashyap S. Acute gastric dilatation. Emerg Med J 2009;26:326.[↩]
- Todd SR, Marshall GT, Tyroch AH. Acute gastric dilatation revisited. Am Surg 2000;66:709–10.[↩]
- Arie E, Uri G, Bickel A. Acute gastric dilatation, necrosis and perforation complicating restrictive-type anorexia nervosa. J Gastrointest Surg 2008;12:985–7.[↩]
- Denazareth AG, Alla VM, Lanspa SJ. Massive gastric distension from chronic intestinal pseudo-obstruction. West J Emerg Med. 2012;13(1):106–107. doi:10.5811/westjem.2011.2.6734 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3298222[↩][↩][↩]
- Cox A, Marks DJB. Acute gastric dilatation causing respiratory distress. JRSM Short Rep 2011;2:41.[↩]
- Antonucci A, Fronzoni L, Cogliandro L, et al. Chronic intestinal pseudo-obstruction. World J Gastroenterol. 2008;14:2953–2961.[↩]
- Osmund WE, Copeland J. Gastric dilatation as a cause of respiratory distress. Can Fam Physician 2010;56:151– 2.[↩]
- Gyurkovics E, Tihanyi B, Szijarto A, et al. Fatal outcome from extreme acute gastric dilatation after an eating binge. Int J Eat Disord 2006;39:602–5.[↩]