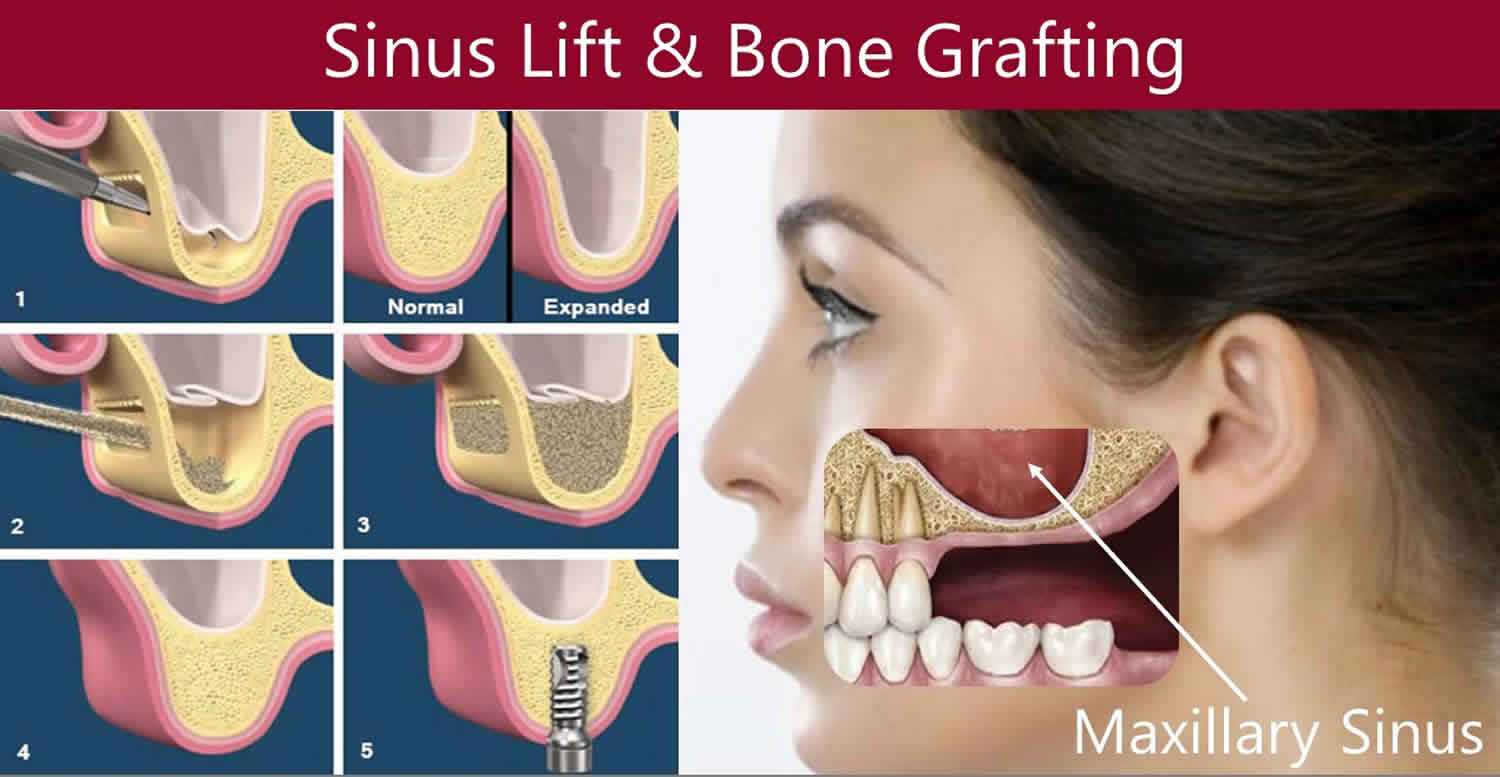
Sinus lift
Sinus lift also called maxillary sinus floor augmentation, sinus graft, sinus augmentation or sinus procedure, is a surgical procedure which aims to increase the amount of bone in the posterior maxilla (upper jaw bone), in the area of the premolar and molar teeth, by lifting the lower Schneiderian membrane (sinus membrane) and placing a bone graft. The sinus lift is one of the most common procedures performed to increase the height of posterior maxilla for placement of dental implants 1. The prime requisite for dental implants is the presence of good bone, thus bone grafting is carried out wherever bone is deficient. There is vast literature which states that sinus expands in the absence of teeth resulting in thin bone incapable of placement of implant placement 2, in such cases bone grafting is done via direct or indirect sinus lift, increasing the height of bone in posterior maxilla.
When a tooth is lost the alveolar process begins to remodel. The vacant tooth socket collapses as it heals leaving a toothless (edentulous) area, termed a ridge. This collapse causes a loss in both height and width of the surrounding bone. In addition, when a maxillary molar or premolar is lost, the floor of the maxillary sinus expands, which further diminishes the thickness of the underlying bone. Overall, this leads to a loss in volume of bone that is available for implantation of dental implants, which rely on osseointegration (bone integration), to replace missing teeth. The goal of the sinus lift is to graft extra bone into the maxillary sinus, so more bone is available to support a dental implant.
Your surgeon will cut the gum tissue where your back teeth used to be. The tissue is raised, exposing the bone. A small, oval window is opened in the bone. The membrane lining the sinus on the other side of the window separates your sinus from your jaw. This membrane is gently pushed up and away from your jaw. Granules of bone-graft material are then packed into the space where the sinus was. The amount of bone used will vary, but usually several millimeters of bone is added above the jaw. Once the bone is in place, the tissue is closed with stitches. Your implants will be placed four to nine months later. This allows time for the grafted material to mesh with your bone. The amount of time depends on the amount of bone needed.
Sinus lift surgery is now widespread, with good results in terms of bone augmentation and implant osseointegration. Nevertheless, the maxillary sinus is a sensitive area which is prone to complications and there is a small proportion of patients who have sinus membrane tear, bleeding, infections, placement of implant in deficient bone height and dislodgement of implant in the sinus cavity with an incidence ranging from 3.5% to 10.5% 3.
Sinus lift surgery indications
Indications of sinus lift surgery include 4:
- Oro-antral fistula treatment
- Reconstruction of palate clefts
- Interpositional graft with Le Fort I fractures
- Less than 10 mm alveolar residual bone height
- Less than 4 mm residual bone width
- No history of any pathology
- In the past, a major sinus disease has not been passed.
Sinus lift surgery contraindications
Local contraindications of sinus lift surgery 4:
- Maxillary sinus infections and pathological lesions
- Chronic sinusitis
- Alveolar scar possibility
- Odontogenic infections
- Allergic rhinitis
- The presence of an irregular alveolar crest
General contraindications of sinus lift surgery:
- High doses of radiation in the head and neck region
- Sepsis
- Advanced medical conditions
- Uncontrolled systemic disturbances
- Excessive smoking, alcohol or substance consumption
- Psychological problems.
Sinus lift surgery procedure
Sinus lift surgery can be entered from four different regions to the sinus area 4:
- Superior-lateral wall (Caldwell-Luc): Entry from the anterior of the zygomatic arch.
- Mid-lateral wall: Entered between alveolar crest and zygomatic arch.
- Inferior-lateral wall: It is entered from alveolar crest level (Lateral window technique/external lifting)
- Krestal osteotomy (closed technique/internal lifting)
The most commonly used methods in the clinic are an inferior-lateral wall and closed sinus lifting methods 4. External technique for creating a bone window in the vestibular wall of the sinus. After that, the sinus epithelium was gently raised to create a space for bone grafting. The healing period took about 6 months. In addition, the one-stage approach was demonstrated, in which sinus augmentation and implantation are performed in one surgery while the two-stage approach had the implantation taking place after several months of sinus augmentation. The above mentioned technique has been known as sinus lifting with the lateral window and is still widely used in modern implant dentistry due to its reliable efficiency.
Lateral window sinus lift
Lateral window sinus lift also called external sinus lifting is often used to reach the maxillary sinus and augment the area; the maxillary elevation of the maxillary sinus floor is obtained by a window-like cavity from the side wall of the maxillary sinus. Nerve blockage is achieved by local anesthesia for this procedure. A vertical incision is made at sagittal, mesial or distal (if necessary
both sides) top of the crest. The lower edge of the window should be 3 mm above the sinus floor, the posterior edge on the tuber, and the anterior edge 3 mm distal from the anterior wall of the sinus 5.
There are two methods used when creating windows on the sinus wall:
- Incomplete fracture,
- Removed bone wall method.
In the incomplete fracture method, the sinus side wall is folded and placed in the sinus cavity. Thus, there is autogenous bone between the sinus floor and the graft material in the form of bone
ischemia. In the bone wall removal method, the bone marrow is completely removed at the desired border. In both methods, after obtaining the sidewall window, the sinus membrane is removed from the bone using special instruments and carefully positioned if the graft material is to be placed. Thus, a vertical area is obtained between the sinus membrane and the alveolar crest.
Conventional rotary tools or piezoelectric are used while creating the sine sidewall window. According to the study published in 2018 6, the perforation rate of the Schneiderian membrane is 24% in conventional procedures, whereas the rate of perforation in piezoelectric surgery is about 8%.
Many researchers have suggested the placement of membranes after surgery on the sinus lateral wall for the purpose of increasing new bone formation 7.
Internal sinus lift
Krestal osteotomy technique was first described by Summers in 1994 as a less invasive technique of apically compressing the sinus floor in the sinus direction and removing the Schneiderian membrane 8. This technique is a good option for patients with bone heights greater than 5–7 mm 5. Several studies have reported a good survival rate (from 93.5–100%) for implants placed sinus using this technique 9.
After removal of the osteotomy site either by flap removal or by flapless technique, a 2 mm drill is used to remove the bone from the sinus floor up to 1 mm 9. The osteotomy is extended with osteotomy drills of 0.5–1.2 mm from the implant size or a series of osteotomes. The bone particles are inserted into the osteotomy and gently pushed towards the sinus. The breaking of the sinus base can be detected by a change in resistance between the osteotomy and bone or by a change in the sound of the beat. As the membrane increases the risk of puncture, the osteotomy should be avoided from advancing into the sinus 8.
Alveolar crest should be well assessed when the method is determined. Suggestions on this subject are 10:
- 8 mm residual bone height and flat sinus floor: Standard implant placement.
- ≥ 8 mm residual bone height and sinus floor: Elevation of maxillary sinus floor using osteotomy technique without standard implant placement using a short implant or without graft material.
- 5–7 mm residual bone height and relatively flat sinus floor: Elevation of the maxillary sinus floor using osteotomy technique with resorption-resistant graft material.
- 5–7 mm residual bone height and oblique sinus floor: Maxillary sinus floor elevation and simultaneous implant placement using the lateral approach with graft material
- 3–4 mm residual bone height and flat or oblique sinus floor: Elevation of maxillary sinus floor using the lateral approach with graft material.
- 1–2 mm residual bone height and flat or oblique sinus floor: Raising the maxillary sinus floor using a lateral approach with graft material and placement of delayed implant after 4–8 months.
Biomaterials used in maxillary sinus augmentation
Sinus lifting was first described as a surgical technique for creating a bone window in the vestibular wall of the sinus. After that, the sinus epithelium was gently raised to create a space for bone grafting. Bone harvesting was performed in the iliac crest area and then placed in the prepared space. The healing period took about 6 months before implantation. The use of autogenous bone,
allograft and alloplast material for bone grafting during sinus augmentation was suggested 4.
Autogenous bone graft is accepted as the gold standard in terms of osteogenic potential but has some disadvantages due to reasons such as the limitations of obtaining autogenous bone graft from the mouth and morbidity as the donor site 11. Autogenous bone grafts are usually harvested from the oral cavity, iliac crest, tibia, and calvary. When choosing the donor site, the size of the defect and surgical risks should be considered 12.
Demineralized freeze-dried bone began to be used in 1970 due to its osteoconductive properties. It has been observed that the use of periodontal surgeons is good for filling the defect and providing a significant increase in the formation of new attachment 13. Biocoral® in is the main component calcium carbonate, along with aragonite, strontium, fluoride, magnesium, sodium, and potassium 14. Biocoral® has recently been used to treat bone defects that are associated with adult periodontitis 15.
Bioglass® contains SiO2 (45%), CaO (24.5%), NaO2 (24.5%) and P2O5 (6%). Surface-reactive silica can provide specific physiological responses, including calcium and phosphate groups and alkaline pH levels, at interfaces with tissues, thereby providing high bioactivity and tolerances that are favorable for the formation of a strong implant bond 11.
PepGen P-15 ™ (Dentsply Friadent CeraMed, Lakewood, CO) is the combination of mineral components of the bovine bone. The inorganic bovine bone mineral component provides the calcium phosphate and natural anatomic matrix necessary for osteoconduction 16.
Calcium sulfate is a highly bio-compatible material with one of the simplest of synthetic bone graft materials with the longest clinical history of more than 100 years 17. Calcium sulphate acts directly as a calcium source, and osteoprogenitor is faster to enter the cell than other materials 18.
Bio-Oss® Protein-free sterilized bovine bone. It consists of porosity from 75 to 80% and cortical fragments with a crystal size of about 10 μm 19. According to some studies, Bio-Oss supports osteogenesis and has slow resorption 20.
Fingranule® (Fin-Ceramica, Faenza RA, Italy) is hydroxyapatite made from potato-shaped granules with a diameter ranging from 250 to 600 μm. This hydroxyapatite is characterized by very low density and crystallinity. The specific property of this material is that it has high porosity. The nano-size is between 10 μm and 10 –60 μm 21.
Polymeric Gel; It consists of a special mixture of poloxamers dissolved in water (predominantly poloxamer 407; BASF ChemTrade GmbH, Burgbernheim, Germany). An important feature of this mixture is that it remains liquid at 23°C and becomes denser and more solid at higher temperatures (about 37°C). For this reason, the poloxamer mixture is stably positioned on the surface of the mucous membrane, allowing the sinus membrane to be raised in a stable manner. They are not metabolized in the body and are proven to be non-irritating and non-toxic 22.
One of the most recent methods used in sinus lifting is the hyaluronic acid method. Hyaluronic acid, the application of exogenous hyaluronic acid and hyaluronic acid-based materials has provided good results in manipulating and accelerating the healing process in numerous medical disciplines such as ophthalmology, dermatology, dentistry, and rheumatology 23. Hyaluronic acid is a naturally occurring, non-sulfated glycosaminoglycan 24 normally found in large quantities in extracellular matrices such as basal lamina, connective matrix and synovial fluid. Hyaluronic acid also has osteoconductive properties and accelerates bone regeneration by chemically, proliferating, and rearranging differentiation of
mesenchymal cells.
Scarano et al. 25 compared the biomaterials used in sinus lifting in 2006. Results of this study, In every specimen taken from augmentations made with autogenous bone, it was possible to see that almost all particles of autogenous bone were completely surrounded by newly formed bone, and the material was found to be highly osteoconductive. They compared histomorphometric
analyses of new bone formation: autogenous bone graft 40.1% ± 3.2%, demineralized frozen-dried bone 29% ± 2.3%, Biocoral® 39% ± 3.1%, Bioglass® 31% ± 1.9%, Fisiograft ®, 33% ± 2.1%, PepGen P-15 ™, 37% ± 2.3%, calcium sulfate38% ± 3.2%,, Bio-Oss®% ± 1.6%, hydroxyapatite 39,32% ± 2.5%.
Cossellu et al. 22 used resorbable polymeric thermoreversible gels in place of graft material in their study of 11 patients who required maxillary sinus lift. After 6 months they took biopsies during implant placement and histologically and histomorphologically examined the specimens histologically and histomorphometrically. According to the histological study result, the new bone tissue does not contain fibrous tissue, cell infiltration is not seen. A new bone form, consisting of lamellar and woven bone, ranging from 54–60% was also observed.
Favato et al. 26 found no statistically significant difference in the study of the volume changes of different graft materials in 43 patients with maxillary sinus augmentation. However, endobon is least shrunk graft material in this study.
Dogan et al. 27 performed a comparison using micro-CT and histomorphometry on the early recovery period of collagenized heterolog bone graft (test group)alone and mixed with hyaluronic acid and collagenized heterolog bone graft (control group). Thirteen systemically healthy patients underwent bilateral sinus augmentation and one side was filled with collagenized heterolog bone graft alone while the other side was filled with hyaluronic acid + collagenized heterolog bone graft. Four months later, bone biopsies were obtained at the implant placement stage. According to the micro-CT and histomorphometric results, the test group had a significant difference from the control group in the 4-month improvement in new bone percentage. Micro-CT and histomorphometric analysis showed more bone formation on the side with hyaluronic acid.
Recent studies have shown that it is not necessary to use graft material in simultaneous implant placement with sinus lifting procedures and that filling the region between the sinus membrane and the bone-implant with the patient’s blood will result in sufficient bone in that region. Thor et al. 28 performed sinus elevation and implant placement without graft material at the same time. Sinus mucosa perforated in 11 of these 27 sinus operations. Sinus surgery was performed in patients with bone height ≤5 mm. The average amount of bone recovered as a result of 1-year follow-up was found to be 6.51 mm.
Sindel et al. 29 performed a study on the application of ring-block autogenous bone graft at implant placement with sinus perforation simultaneously. They prefer symphysis area to harvest autogenous bone graft. After removing the full thickness flap, graft borders were determined with a trephine bur with an inside diameter of 7.5 mm. The implant cavity is prepared according to the diameter and length of the implant to be used on the later determined graft. In the drilling process, 1.5 mm bone tissue was not touched around the implant. After this procedure, a bone graft was removed using the same trephine bur.
The overall survival rate of the implants was 90% over an average of 24.3 months. The nine implanted implants continue to function within normal limits of marginal resorption without any sign of peri-implant disease.
Sinus lift surgery complications
The most common sinus lift complication which can be encountered during the surgery, are summarized as follows 30:
- Intraoperative complications:
- Bleeding,
- Buccal flap tear,
- Infraorbital nerve injury,
- Membrane perforation;
- Early postoperative complications:
- Incision line opening,
- Bleeding,
- Barrier membrane exposure,
- Infraorbital nerve paresthesia;
- Late postoperative complications:
- Graft loss/failure,
- Implant failure,
- Oroantral fistula,
- Implant migration,
- Inadequate graft fill.
Intraoperative complications can arise during any surgical procedure, the most common of which is membrane perforation occurring in about 7-44% of procedures 31. This can further lead to acute or chronic sinus infections, loss of grafting material and the disruption of normal sinus physiology 32. In such cases no grafting procedure should be carried out and the site can be reopened after 2-3 weeks when the membrane has repaired itself. However, few authors advocate grafting even in cases of membrane tear as no association between the membrane perforation and the implant survival has been found 30. Certain anatomical factors such as sinus septa, mucosal swelling, mucoceles, narrow sinus or osteotomy design or an increased lateral wall can increase the risk of membrane perforation. Thus such the site should be free of pathologies before sinus lift.
Bleeding is another common complication, slight bleeding from the surgical site is a normal phenomenon of any surgery, and bleeding from soft tissues is of short duration however, if profuse bleeding occurs one should consider the possibility of damage or severing of the artery or branches of the vascular supply of the lateral wall of the sinus and the surrounding soft tissue or damage
to the posterior lateral nasal artery. All efforts should be done towards control of the bleeding, only when clinician is sure of no hemorrhages, bone grafting procedure can be commenced.
Displacement of dental implants to adjacent anatomic structures is another reported complication. This occurs when proper treatment planning is not done and there is no initial stability of the dental implant placed which occurs in cases of insufficient bone height and quality. Displacement of an implant may further cause serious consequences such as sensory disturbance, maxillary sinusitis, oroantral fistula. The migration of such implants in the ethmoid, sphenoid sinuses, orbit, nose and anterior cranial fossa is much more sporadic 33 other reasons for such displacement are poor surgical skills of the operator, the presence of an uncured perforation, too much implant tapping or the application of an excessive force 34. Another reason could be autoimmune reaction to the peri-implant bone destruction caused by the implant, which leads to the loss
of integration 35. Caldwell-Luc technique has been proposed to retrieve dental implant or any foreign body material from the sinus, however sometimes implant may be embedded further up towards the orbit, causing retrieval difficult. This results in extra surgeries and expenditure for the patient.
Early post-operative complications such swelling or slight bleeding from the surgical site are common and transient. Complications such as exposure of the underlying membrane due to opening of suture line mainly occur due to excessive swelling. Thus post operative instructions should be clearly given and should be reinforced on the patient. Late complications of the surgery include loss of the graft causing implant failure. This may also lead to implant migration in other anatomical structures as aforementioned and oroantral fistula. According to the literature, acute postoperative sinusitis occurs as a complication in up to 4.7% of sinus graft procedures 36. Rhino-sinusitis is a well-known complication associated with the sinus lift procedures where surgical treatment is required to further stop the spread of infection 37. Most often the infection appears after more than one week of the surgery. According to the literature it has been shown that 3-20% of patients who have predisposing factor for sinusitis are at risk of developing postoperative transient sinusitis.
- Mahesh, Lanka & Kurtzman, Gregori. (2019). COMPLICATIONS OF THE SINUS LIFT PROCEDURE.[↩]
- Bhaskar SN. Orban’s oral histology and embryology (11th ed). St Louis, Mo: CV Mosby; 239-59.[↩]
- Candotto, Valentina & Gallusi, Gianni & Piva, A & Baldoni, M & Girolamo, M. (2020). Complications in sinus lift. Journal of biological regulators and homeostatic agents. 34. 139-142. [↩]
- Bagis, Nilsun & Barbaros, R. (2018). Maxillary Sinus Lifting. International Journal of Experimental Dental Science. 7. 91-97. 10.5005/jp-journals-10029-1181.[↩][↩][↩][↩][↩]
- Tarnow DP, Wallace SS, Froum SJ, et al. Histologic and clinical comparison of bilateral sinus floor elevations with and without barrier membrane placement in 12 patients: Part 3 of an ongoing prospective study. Int J Periodontics Restorative Dent 2000;20(2):117-125.[↩][↩]
- Jordi C, Mukaddam K, Lambrecht JT, et al. Membrane perforation rate in lateral maxillary sinus floor augmentation using conventional rotating instruments and piezoelectric device—a meta-analysis. Int J Implant Dent 2018;4:3.[↩]
- Wallace SS, Mazor Z, Froum SJ, et al. Schneiderian membrane perforation rate during sinus elevation using piezosurgery: clinical results of 100 consecutive cases. Int J Periodontics Restorative Dent 2007;27(5):413-419.[↩]
- Summers RB. Sinus floor elevation with osteotomes. J Esthet Dent 1998;10(3):164-171.[↩][↩]
- Pjetursson BE, Lang NP. Sinus floor elevation utilizing the transalveolar approach. Periodontol 2000. 2014;66(1):59-71.[↩][↩]
- Lindhe J, Lang, NP. Clinical periodontology and implant dentistry. 2008; 6th edition Oxford: Blackwell Munksgaard[↩]
- Wang M. Developing bioactive composite materials for tissue replacement. Biomaterials 2003;24(13):2133-2151.[↩][↩]
- Clavero J, Lundgren S. Ramus or chin grafts for maxillary sinus inlay and local onlay augmentation: comparison of donor site morbidity and complications. Clin Implant Dent Relat Res 2003;5(3):154-160.[↩]
- Bowers G, Felton F, Middleton C, et al. Histologic comparison of regeneration in human intrabony defects when osteogenin is combined with demineralized freeze-dried bone allograft and with purified bovine collagen. J Periodontol 1991;62(11):690-702.[↩]
- Pollick S, Shors EC, Holmes RE, et al. Bone formation and implant degradation of coralline porous ceramics placed in bone and ectopic sites. J Oral Maxillofac Surg 1995;53(8):913-915.[↩]
- Yukna RA, Yukna CN. A 5-year follow-up of 16 patients treated with coralline calcium carbonate (Biocoral) bone replacement grafts in intrabony defects. J Clin Periodontol 1998;25:1036-1040.[↩]
- Qian JJ, Bhatnagar RS. Enhanced cell attachment to anorganic bone mineral in the presence of a synthetic peptide related to collagen. J Biomed Mater Res 1996;31(4):545-554.[↩]
- Sottosanti JS. Calcium sulfate-aided bone regeneration: a case report. Periodontal Clin Investig 1995;17(2):10-15.[↩]
- Piattelli A, Scarano A, Piattelli M, et al. Bone regeneration using Bioglass: an experimental study in rabbit tibia. J Oral Implantol 2000;26(4):257-261.[↩]
- Berglundh T, Lindhe J. Healing around implants placed in bone defects treated with Bio-Oss. An experimental study in the dog. Clin Oral Implants Res. 1997;8(2):117-124.[↩]
- Rodriguez A, Anastassov GE, Lee H, et al. Maxillary sinus augmentation with deproteinated bovine bone and platelet rich plasma with simultaneous insertion of endosseous implants. J Oral Maxillofac Surg 2003;61(2):157-163.[↩]
- Nanci A, Zalzal S, Fortin M, et al. Incorporation of circulating bone matrix proteins by implanted hydroxyapatite and at bone surfaces: Implications for cement line formation and structuring of biomaterials. In: Davies JE, ed. Proceedings of the International Workshop on Bone Engineering. Toronto, Canada: Em Squared Inc.; 2000:305-311.[↩]
- Cossellu G, Farronato G, Farronato D, et al. Space-maintaining management in maxillary sinus lifting: a novel technique using a resorbable polymeric thermo-reversible gel. Int J Oral Maxillofac Surg 2017;46(5):648-654.[↩][↩]
- Laurent TC, Fraser JR. Hyaluronan. FASEB J 1992;6(7):2397-2404.[↩]
- Benedetti L, Cortivo R, Berti T, et al. Biocompatibility and biodegradation of different hyaluronan derivatives (Hyaff) implanted in rats. Biomaterials 1993;14(15):1154-1160.[↩]
- Scarano A, Degidi M, Iezzi G, et al. Maxillary sinus augmentation with different biomaterials: a comparative histologic and histomorphometric study in man. Implant Dent 2006;15(2):197-207.[↩]
- Favato MN, Vidigal BCL, Cosso MG, et al. Impact of human maxillary sinus volume on grafts dimensional changes used in maxillary sinus augmentation: a multislice tomographic study. Clin Oral Implants Res 2015;26(12):1450-1455.[↩]
- Dogan E, Dursun E, Tosun E, et al. Evaluation of hyaluronic matrix efficacy in sinus augmentation: a randomized-controlled histomorphometric and micro-computed tomography analysis. Int J Oral Maxillofac Surg 2017;46(7):931-937[↩]
- Thor et al. Sinus Lift and Immediate Implant Installation. J Oral Maxillofac Surg 2007.[↩]
- Sindel A, Ozarslan MM, Ozalp O. Intrasinusal locking technique: a novel use of the ring block technique at sinus perforations for simultaneous implant placement. Int J Oral Maxillofac Surg 2018;47(4):499-504.[↩]
- Schwartz-Arad D, Herzberg R, Dolev E. The prevalence of surgical complications of the sinus graft procedure and their impact on implant survival. J Periodontol 2004;75:511-16.[↩][↩]
- Levin L, Herzberg R, Dolev E, et al. Smoking and complications of onlay bone grafts and sinus lift operations. Int J Oral Maxillofac Impla 2004;19:369-373.[↩]
- Shlomi B, Horowitz I, Kahn A, et al. The effect of sinus membrane perforation and repair with Lambone on the outcome of maxillary sinus floor augmentation: a radiographic assessment. Int J Oral Maxillofac Impla 2004;19:559-562.[↩]
- Griffa A, Viterbo S, Boffano P. Endoscopic-assisted removal of an intraorbital dislocated dental implant. Clin Oral Impla Res 2010;778-780.[↩]
- Varol A, Turker N, Goker K, et al. Endoscopic retrieval of dental implants from the maxillary sinus. Int J Oral maxillofac Impla 2006;21:801-804.[↩]
- Regev R, Smith RA, Perrott DH, et al. Maxillary sinus complications related to endosseous implants. Int J Oral maxillofac Impla 1995;10:451-461.[↩]
- Jensen SS, Terheyden H. Bone augmentation procedures in localized defects in the alveolar ridge: Clinical results with different bone grafts and bonesubstitute materials. Int J Oral Maxillofac Implants 2009;24(suppl):218-236.[↩]
- Carmeli G, Artzi Z, Kozlovsky A, et al. Antral computerized tomography preoperative evaluation: relationship between mucosal thickening and maxillary sinus function. Clinical Oral Implant Research. 2010;78-82.[↩]