Terrien’s marginal degeneration
Terrien’s marginal degeneration is a rare painless and slowly progressive non-inflammatory thinning of the peripheral corneal stroma 1. Terrien’s marginal degeneration is usually bilateral but may be asymmetric. As opposed to other causes of peripheral corneal thinning, there is typically no inflammation and the corneal epithelium remains intact. Characteristic features of Terrien’s marginal degeneration include peripheral stromal thinning that typically begins superiorly with intact epithelium, overlying pannus (superficial vascularization) and a leading edge of lipid deposition. The thinning classically has a steep central edge and a gradually sloping peripheral edge. The thinning may create against-the-rule or oblique astigmatism due to its relaxing effect on the corneal curvature and patients may experience corneal perforation with mild trauma.
Terrien’s marginal degeneration typically occurs in males 40 years and older (men than women 3:1), although it may present in childhood 2. Patients normally report an absence of eye pain, photophobia, or tearing 2. However, a painful variant presenting in younger individuals has also been described 3.
Two types of Terrien’s marginal degeneration have been documented. The first occurring in the older population and is asymptomatic and slowly progressive. The second more inflammatory type occurs in young to middle-aged men (75%) and occurs in the second or third decade of life. It has also been reported in patients with posterior polymorphous dystrophy, anterior basement membrane dystrophy and erythema elevatum diutinum.
Corneal thinning can be localized or involve extensive proportions of the peripheral cornea 4. Degeneration typically begins superiorly with mild, punctuate subepithelial and/or anterior stromal opacities and leaves a clear area between the opacities and the limbus. Opacification is followed by the development of a peripheral, superficial, fine vascular pannus, which progresses over the years to include subepithelial opacity at the advancing edge, without the overlying edge characteristic of Mooren’s ulcer. The thinning spreads circumferentially, rarely involves the inferior limbus, and leaves the epithelium intact. The central wall is steep, and the peripheral wall slopes gradually. A yellow line of lipid deposits appears at the leading edge of the pannus (central edge of the furrow). Vessels transverse the furrow and pass beyond it. Spontaneous perforation is rare, although perforation can occur easily with minor trauma. Spontaneous ruptures in Descemet’s membrane can result in interlamellar fluid or even a corneal cyst.
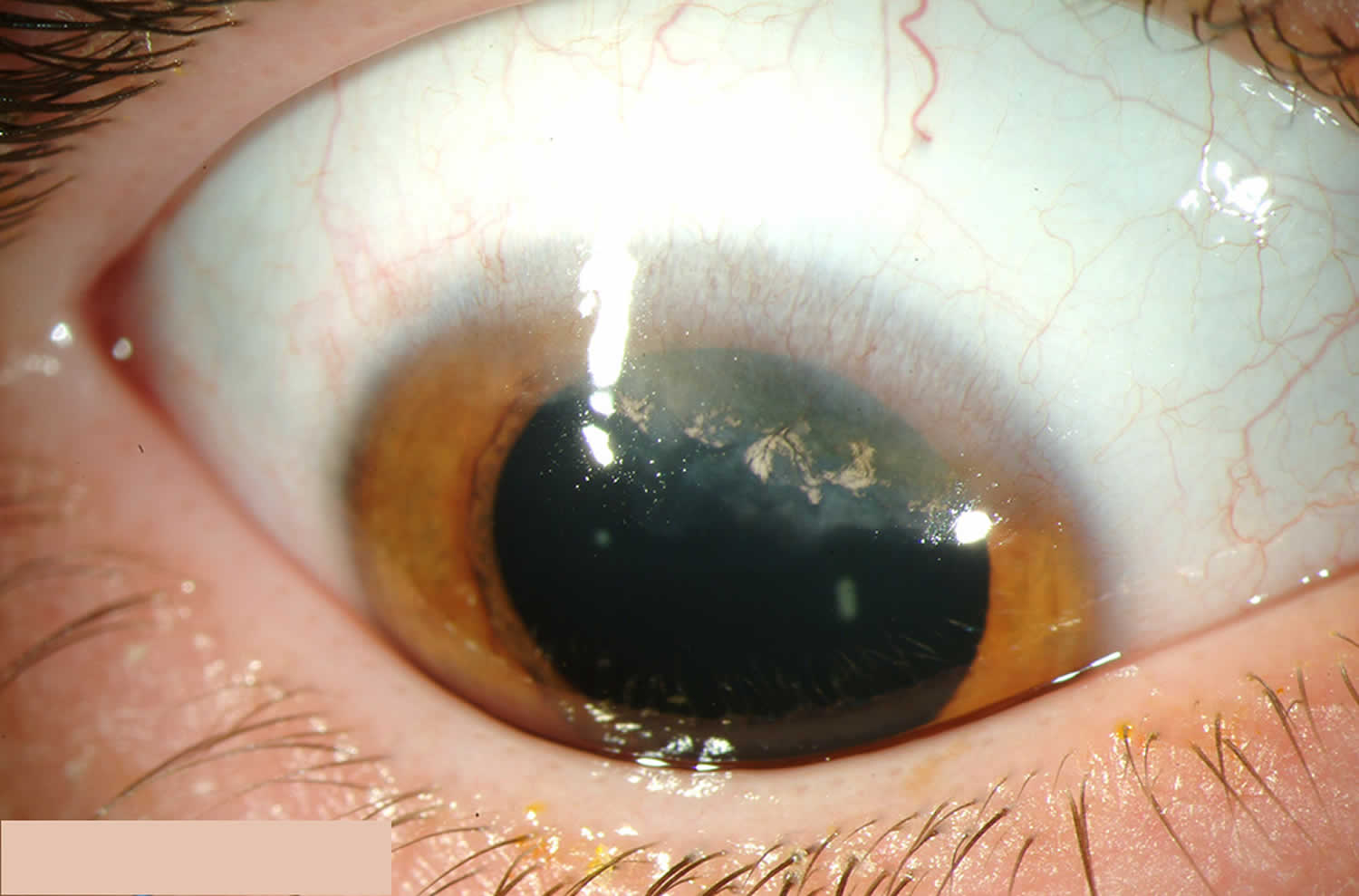
Figure 1. Terrien marginal degeneration
Footnote: Patient with Terrien marginal degeneration displaying superior stromal thinning with intact epithelium, overlying pannus, and lipid at the leading edge.
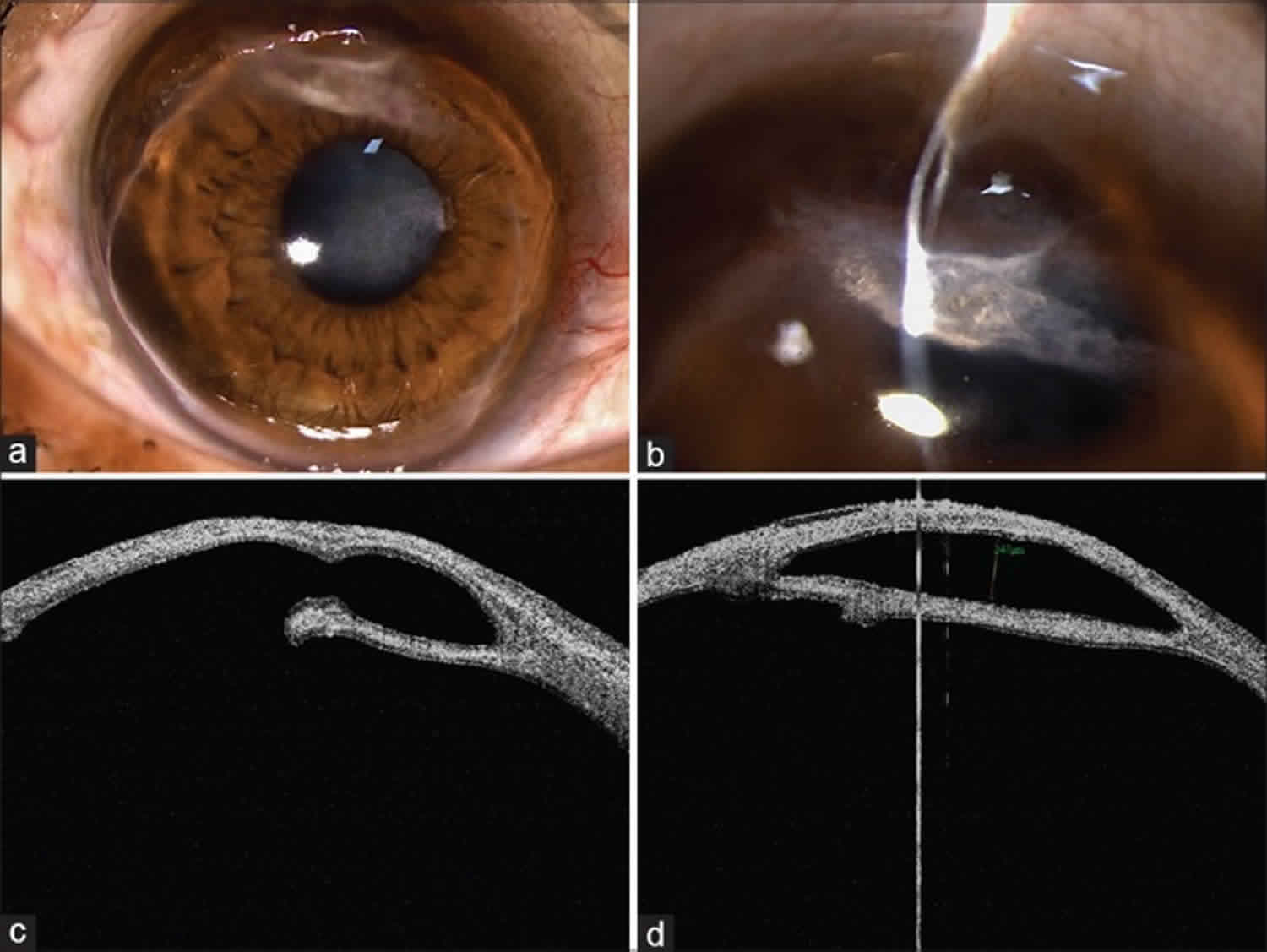
Figure 2. Terrien’s marginal degeneration
Footnote: A case of bilateral Terrien’s marginal degeneration with intrastromal cyst. (a) Slit lamp photograph showing 360° peripheral thinning with superficial vascularization and lipid deposition. (b) Slit lamp photograph showing an intrastromal cyst with scarring. (c and d) Corresponding photographs of anterior segment optical coherence tomography showing the intrastromal cyst and peripheral thinning.
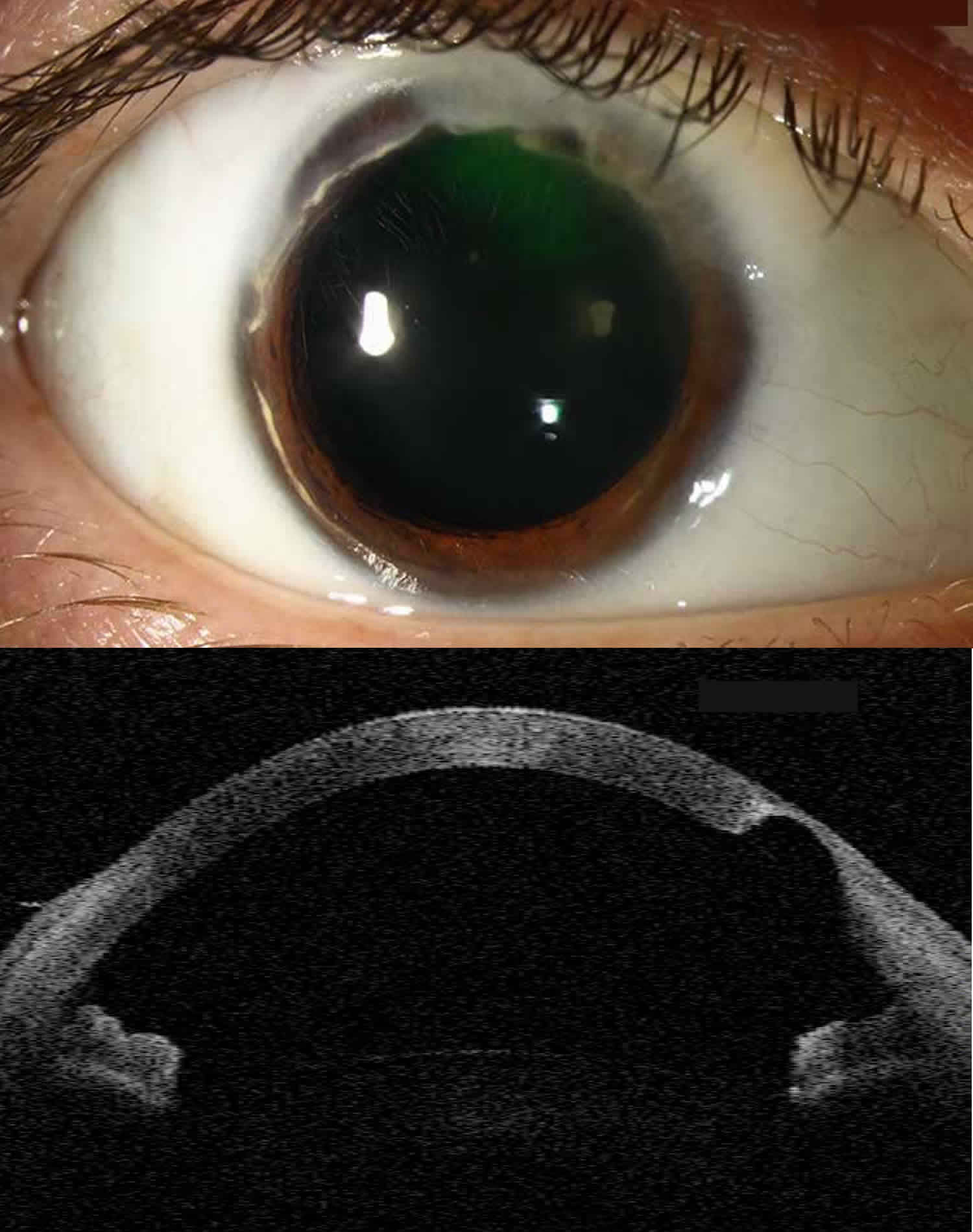
[Source 5 ]Figure 3. Terrien marginal corneal degeneration
Footnote: This patient with Terrien’s marginal degeneration has characteristic findings in the right eye. The severe superior stromal thinning is visible on anterior segment OCT and is creating a characteristic against-the-rule pattern of astigmatism. The patient was filtering aqueous through the area of superior thinning resulting in positive Seidel testing and creation of an adjacent conjunctival bleb. The patient underwent a crescentic lamellar keratoplasty to repair the defect.
Terrien’s marginal degeneration causes
Terrien’s marginal degeneration cause is currently unknown. The epithelium may be normal, thickened or thinned. Bowman’s membrane is typically absent or degenerated. Thinning and occasional breaks may be seen in Descemet’s membrane. Subepithelia fibrillar collagen degeneration has been seen with light microscopy. Electron microscopy demonstrates collagen precursors, stromal ground substance, and possibly lipid phagocytized by histiocytic cells with high lysosomal activity. Histocytes with a high degree of lysosomal activity are responsible for the destruction of collagen fibrils.
Terrien’s marginal degeneration symptoms
Terrien’s marginal degeneration typically presents as painless progressive blurred vision. Patients normally report an absence of eye pain, photophobia, or tearing 2. However, a painful variant presenting in younger individuals has also been described 3.
Terrien’s marginal degeneration diagnosis
The diagnosis of Terrien’s Marginal Degeneration is primarily clinical, based on history and slit lamp examination of the eye.
Physical examination reveals a leading edge of lipid deposition, steep central edge, sloping peripheral edge, intact epithelium and superficial vascularization. Patients have a high against-the-rule or oblique astigmatism from the progressive flattening of the vertical meridian.
Terrien’s marginal degeneration may be differentiated from other peripheral corneal thinning disorders by the lack of inflammation, presence of superficial vascularization, advancing linear deposition of lipid, lack of epithelial defect and slow progressive course. It can present with recurrent painful episodes of inflammation. Collagen vascular diseases should be excluded. No known systemic associations. Rarely, it may present as a pseudo-pterygium with a broad, flat, leading edge that arises in an oblique axis. This variant may be the same as Fuchs’ superficial marginal keratitis.
Diagnostic procedures
Corneal topography reveals flattening of the peripheral thinned cornea, with steepening of the corneal surface approximately 90° away from the midpoint.
Differential diagnosis
- Marginal furrow degeneration
- Dellen
- Collagen vascular disease
- Pellucid marginal degeneration
- Sclerokeratitis
- Keratoconjunctivits sicca
- Staphylococcal marginal keratitis
- Infectious corneal ulcer
Terrien’s marginal degeneration is generally easy to differentiate from Mooren’s because there is no pain or inflammation, the epithelium is intact and there is no overlying edge. Inflammatory Staphylococcal lesions usually have a lucid interval between the limbus and the infiltrate and only rarely cause thinning. Marginal furrow degeneration is bilateral and avascular with only minimal, if any, thinning.
Terrien’s marginal degeneration treatment
Generally no treatment is required for Terrien’s marginal degeneration, unless perforation or impending perforation occurs. Initial conservative management for the severe astigmatism includes the use of spectacles or rigid gas-permeable contact lenses. Underlying corneal thinning should be monitored carefully.
Medical therapy
Most common medical therapy is contact lenses to address the corneal astigmatism.
Surgery
Surgical correction is indicated when perforation is imminent due to progressive thinning or when astigmatism significantly limits visual acuity. Crescent-shaped lamellar or full-thickness corneoscleral patch grafts may be used. These grafts have been reported to arrest progression of severe against-the-rule astigmatism for up to 20 years. Annular lamellar keratoplasty grafts may be required in severe cases of 360° marginal degeneration.
Terrien’s marginal degeneration prognosis
Most patients with do not progress to corneal perforation and can be managed successfully with glasses or contact lenses. Because there is typically no epithelial defect the risk of infectious keratitis and acute corneal thinning is low, but these patient should be monitored regularly.
- Vejdani AH, Khakshoor H, McCaughey MV, Moshirfar M. Partial and Total Descemet’s Detachments in a Patient with Severe Terrien’s Marginal Degeneration and Juvenile Idiopathic Arthritis. Case Rep Ophthalmol Med. 2014;2014:279491. doi:10.1155/2014/279491 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4131067[↩]
- Bouchard CS. Noninfectious keratitis. In: Yanoff M, Duker J, editors. Ophthalmology. 3rd edition. Mosby; 2008. p. p. 1552.[↩][↩][↩]
- Austin P, Brown SI. Inflammatory Terrien’s marginal corneal disease. American Journal of Ophthalmology. 1981;92(2):189–192.[↩][↩]
- Terrien’s Marginal Degeneration. https://eyewiki.org/Terrien%27s_Marginal_Degeneration[↩]
- Singhal D, Roop P, Maharana PK. Intrastromal cyst in Terrien’s marginal degeneration. Indian J Ophthalmol. 2019;67(9):1475. doi:10.4103/ijo.IJO_2097_18 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6727702[↩]