Hand tremors
Tremor is a type of rhythmic shaking movement that you can’t control that is commonly caused by a neurological condition or a nervous system disorder 1, 2, 3. Hand tremors or shaky hands can have many causes, ranging from temporary factors like stress, caffeine, alcohol or drug withdrawal, some prescription medicines (e.g., anti-epileptics such as phenytoin, and carbamazepine, narcoleptics, tricyclics, lithium, cocaine, alcohol, adrenaline, bronchodilators, theophylline, caffeine, steroids, valproate, amiodarone, thyroid hormones, vincristine) to more serious underlying medical conditions like heavy metals poisoning, metabolic diseases such as overactive thyroid (hyperthyroidism), hypoparathyroidism (a condition where the parathyroid glands produce insufficient parathyroid hormone (PTH), leading to low calcium levels in the blood (hypocalcemia) causing a variety of symptoms such as muscle spasms, tingling sensations, and in severe cases, seizures), liver disease and hypoglycemia (low blood sugar level), peripheral neuropathies (e.g., Charcot-Marie-Tooth disease – a group of inherited progressive disorders that affect the peripheral nerves), essential tremor (the most common cause of adult onset hand tremors with about 50 to 70% of essential tremor cases being inherited although a specific gene hasn’t been identified and the other cases of essential tremor caused by unknown factors), multiple sclerosis (MS), Parkinson’s disease (a neurodegenerative brain condition that causes problems with slowed movements (bradykinesia), poverty of movement (hypokinesia), e.g. loss of facial expression and arm swing, difficulty with fine movements, resting tremors, balance problems, mental health, sleep, pain and other health issues), Wilson’s disease (a genetic disorder where the body can’t properly eliminate copper, causing it to build up in the liver, brain, eyes, and other organs), brain tumors or alcohol abuse disorder. It’s important to find out if your hand tremor is a symptom of a more serious medical condition or just a temporary effect like stress, caffeine, alcohol or drug withdrawal and some prescription medications. The first step is to see an experienced neurologist, and preferably one with additional training in movement disorders for a thorough evaluation.
If you’re experiencing tremor, it’s important to speak with a an experienced neurologist, and preferably one with additional training in movement disorders for a thorough evaluation. As making a proper diagnosis is important for your treatment and future prognosis.
Your neurologist will likely:
- Ask about your medical history and your symptoms
- Perform a physical exam
- Conduct a neurological exam
Your neurologist may also order blood tests or brain imaging to identify for any underlying causes.
Treatment depends on the type of tremor and its severity. If tremor is caused by a different health condition, treating that condition can reduce or stop the tremor. Mild cases may not need treatment, especially if you aren’t bothered by the symptoms. Avoiding excess caffeine and limiting alcohol may help reduce a tremor. Using relaxation techniques, such as massage and meditation, and doing tasks differently, such as paying bills online instead of writing checks, may also help.
- Medication. Certain medications can help slow or suppress symptoms. Botulinum toxin injections can also help certain kinds of tremor.
- Surgery. For severe cases of tremor and when medicines aren’t helping, a doctor may recommend surgical treatment such as deep brain stimulation.
- Therapy. Physical, speech, and occupational therapy can all help control symptoms of tremor and manage daily tasks.
- Assistive devices. Certain assistive tools and technologies can help simplify daily tasks such as eating, writing, or using a computer. Some wearable devices can also help suppress tremor.
Talk with your doctor about trying medications to suppress your tremors or stopping medications that might worsen them.
See a doctor immediately if you:
- Suddenly develop a tremor
- Are under 50 years old
- Also feel confused or weak
- Experience difficulty walking
- Have a fast heart rate.
Make an appointment to see a doctor if you:
- Have a new tremor or one that’s getting worse. If the shaking doesn’t improve or gets worse over time, it’s important to consult a doctor.
- Tremors interfere with daily activities: If the tremors significantly impact your ability to perform everyday tasks.
- Find that your work is affected
- If you suspect tremors might be related to another health issue or underlying medical condition.
What are the different kinds of tremor?
Tremors are categorized by when they happen and what triggers them 4, 5.
- Physiologic tremor. The normal, tiny amount of tremor that’s present in all healthy individuals. We all have a little bit of tremor called a physiologic tremor; it’s natural and not usually noticeable.
- Enhanced physiologic tremor. A more noticeable version of physiologic tremor. This small, fine tremor in the hands and fingers is usually a side effect of certain medications, alcohol withdrawal, stress, fatigue, or some medical conditions such as an overactive thyroid and hypoglycemia (low blood sugar level).
- Functional tremor also called psychogenic tremor can appear as any form of tremor. Its symptoms may vary but often start suddenly and fluctuate widely. The tremor may increase with attention and decrease or disappear when the person is distracted.
- Essential tremor. The most common type of abnormal tremor. It happens without other neurological symptoms. It occurs during movement and usually affects the hands and arms, but it can also impact the head, legs, or voice. This type often runs in families.
- Parkinsonian tremor. A common early sign of Parkinson’s disease, though not everyone with Parkinson’s disease experiences tremor. It is most noticeable when the body is at rest and may look like rolling a pill between the thumb and a finger. Parkinson’s tremor may also affect the chin, lips, face, and legs. Parkinsonian tremor may initially appear in only one limb or on just one side of the body but may spread to both sides as the disease progresses. The tremor is often made worse by stress or strong emotions.
- Dystonic tremor. A tremor that occurs in people with dystonia, a movement disorder in which incorrect messages from the brain cause muscles to be overactive, resulting in abnormal postures or sustained, unwanted movements. The disorder usually appears in young or middle-aged adults and can affect any muscle in the body. Dystonic tremor most commonly affects the neck (cervical dystonia), vocal cords (laryngeal dystonia), or arms/legs (limb dystonia). A person with dystonic tremor can sometimes relieve their tremor by relaxing completely or touching the affected body part or muscle.
- Cerebellar tremor. Cerebellar tremor is typically a slow, big (high amplitude) tremor of the arms, legs, hands, or feet that worsens at the end of a purposeful movement such as pressing a button. Cerebellar tremor is caused by damage to the cerebellum, the part of the brain that controls movement and its pathways to other brain areas. This damage could be caused by a stroke, tumor, injury, an inherited disorder, or from chronic damage due to alcohol use disorder.
- Orthostatic tremor is a rare disorder characterized by rapid muscle contractions in the legs that occur when a person stands up. Orthostatic tremor usually stops when the person sits down or walks. Standing may make the person feel unsteady or unbalanced, causing them to try to sit or walk. Because this type of tremor involves very fast shaking, it may not be visible to the naked eye. Orthostatic tremor can be felt by touching the person’s thighs or calves or when a doctor listens to the muscle activities with a stethoscope. In some cases, the tremor can become more severe over time. The cause of orthostatic tremor is unknown.
- Rest tremor occurs when people are at rest. People with Parkinson’s disease often experience rest tremor.
- Action tremor occurs when a muscle is moved voluntarily. There are several sub-classifications of action tremor, many of which overlap.
- Postural tremor occurs when holding a position against gravity, such as holding the arms outstretched.
- Kinetic tremor is associated with any voluntary movement, such as moving the wrists up and down or closing and opening your eyes.
- Intention tremor starts when the person makes an intended movement toward a target, such as lifting a finger to touch their nose.
- Task-specific tremor only appears when performing goal-oriented tasks such as handwriting or speaking.
- Isometric tremor occurs during a voluntary muscle contraction that is not accompanied by any movement, such as when holding a heavy book in the same position.
Who is more likely to get tremor?
Tremor is most common among middle-aged and older adults, although it can occur at any age. Generally, tremor occurs in men and women equally.
Tremor can occur on its own or be a symptom of other neurological disorders such as Parkinson’s disease, multiple sclerosis, or stroke. Tremor sometimes can be caused by other medical conditions, including but not limited to:
- Medicines. Several drugs can cause tremors, including certain asthma medications, corticosteroids, chemotherapy, and drugs used for certain psychiatric and neurological disorders.
- Heavy metals and other neurotoxins. Exposure to heavy metals (such as mercury, manganese, lead, arsenic, etc.), organic solvents, or pesticides may cause tremors.
- Caffeine. Excessive caffeine may cause temporary tremor or make an existing tremor worse.
- An overactive thyroid (hyperthyroidism) can cause tremors.
- Liver or kidney failure. Liver and kidney failure may cause damage in certain brain areas that leads to tremors or jerky movements.
- Diabetes. High or low blood sugar (hyperglycemia or hypoglycemia, respectively) may cause tremors or other involuntary movements.
- Stress, anxiety, or fatigue may be associated with tremors.
Hand tremors causes
Tremor is usually caused by a problem in the parts of the brain that control movements. Most types have no known genetic cause, although there are some forms that appear to be inherited and run in families.
Possible causes of hand tremors are many and may be genetic, acquired, or idiopathic 6:
- Neurodegenerative disease
- Essential Tremor: Essential tremor previously also called benign essential tremor or familial tremor is a neurological condition causing involuntary shaking, often most noticeable when hands are in use. Essential tremor is one of the most common adult-onset movement disorders. Essential tremor key feature is a tremor in both hands and arms during action without other neurological signs. Essential tremor also may affect a person’s head, voice, or lower limbs. Although the tremor can start at any age, it most often first appears during adolescence or in middle age between ages 40 and 50. It can be mild and stay mild, or slowly get worse over time. The exact cause of essential tremor is unknown. Studies show essential tremor is accompanied by a mild degeneration of the cerebellum, which is the part of your brain that controls movement coordination. Essential tremor is an inherited condition in 50-70% of cases (referred to as familial tremor). Familial forms often appear early in life.
- Parkinson’s Disease: Tremors, especially at rest, are a common symptom of Parkinson’s disease.
- Multiple system atrophy
- Corticobasal degeneration
- Progressive supranuclear palsy (PSP)
- Genetic disorders: genes causing predominantly parkinsonism
- Genes causing frontotemporal dementia with parkinsonism
- Genes causing predominantly dystonia
- Neuroferritinopathy is a rare, autosomal dominant movement disorder caused by mutations in the FTL1 gene, which encodes the ferritin light chain. This genetic defect leads to abnormal iron accumulation in the brain, primarily in the basal ganglia, resulting in progressive movement problems and other neurological symptoms.
- Spinocerebellar ataxias are a group of inherited, progressive neurological disorders characterized by loss of balance and coordination, and other movement problems. They are caused by genetic mutations that affect the brain and spinal cord. While there is no cure, treatments focus on managing symptoms and improving quality of life.
- Genes causing Fahr’s disease also known as familial idiopathic basal ganglia calcification, is a rare neurological disorder characterized by abnormal calcium deposits in the brain, particularly in the basal ganglia. These calcifications can lead to various neurological symptoms, including movement disorders and cognitive impairments. The condition is often inherited, either dominantly or recessively
- Genes causing peripheral neuropathies that produce tremor
- Wilson’s disease
- X-linked dystonia parkinsonism/Lubag
- Lesch-Nyhan’s syndrome
- Fragile X–associated tremor or ataxia syndrome
- Spinal muscular atrophy
- Chromosomal aneuploidy
- XYY, XXY (Klinefelter’s syndrome), and XXYY syndromes
- Mitochondrial genetic disorders
- Leigh’s syndrome also called Leigh disease is a rare, inherited neurological disorder primarily affecting infants and young children, caused by defects in the energy-producing process within the mitochondria. It leads to progressive loss of mental and movement abilities (psychomotor regression) and typically results in death within a few years, often due to respiratory failure.
- Mitochondrial polymerase gamma mutations. Mutations in the gene encoding mitochondrial DNA polymerase gamma (POLG), the enzyme that synthesises mitochondrial DNA (mtDNA), have been associated with a mitochondrial disease—autosomal dominant or recessive progressive external ophthalmoplegia—and multiple deletions of mtDNA. It typically affects multiple organs, primarily the brain, nerves, muscles, and liver, and can affect vision due to involvement of brain structures 7. It is also one of the most common inherited mitochondrial disease.
- Infectious and inflammatory diseases
- Human immunodeficiency virus (HIV)
- Tuberculosis
- Syphilis
- Measles
- Typhus is a group of infectious diseases caused by rickettsial bacteria and transmitted by fleas, lice, chiggers, or ticks. The main types are epidemic typhus (louse-borne), murine typhus (flea-borne), and scrub typhus (chigger-borne). Symptoms include fever, headache, and sometimes a rash. Typhus is treatable with antibiotics, but untreated can be fatal.
- Neuroborreliosis also known as Lyme neuroborreliosis is a neurological complication of Lyme disease caused by the bacteria Borrelia burgdorferi, which can affect the nervous system. It’s a tick-borne disease that can manifest with a variety of symptoms, including facial nerve palsy, radiculitis, and meningitis.
- Bacterial encephalitis
- Viral encephalitis
- Endocrine and metabolic disorders
- Kidney failure
- Liver failure
- Hyperthyroidism (overactive thyroid)
- Deficiencies in vitamins B1 (thiamine), B6 (pyridoxine), and B12 (cobalamin) can contribute to tremors.
- Hypoglycemia (Low Blood Sugar): This can lead to shaking due to nerve and muscle dysfunction.
- Neuropathies and spinal muscular atrophies
- Kennedy’s syndrome, also known as Spinal and Bulbar Muscular Atrophy (SBMA), is a rare, inherited neuromuscular disorder primarily affecting men, causing progressive weakness and wasting of muscles. It’s characterized by the degeneration of lower motor neurons, leading to symptoms like muscle weakness, atrophy, and muscle twitches (fasciculations)
- Guillain-Barré syndrome (GBS) is a rare autoimmune disorder where the body’s immune system attacks the peripheral nervous system, causing muscle weakness and sometimes paralysis. Guillain-Barré syndrome often follows a viral or bacterial infection, though the specific trigger is unknown.
- Gammopathy-induced neuropathies refer to nerve damage caused by the presence of monoclonal proteins, often in conditions like monoclonal gammopathy of undetermined significance (MGUS) or Waldenstrom’s macroglobulinemia. These proteins can directly damage the peripheral nerves or trigger the formation of antibodies that target nerve components, leading to a variety of neurological symptoms.
- Demyelinating diseases such as multiple sclerosis (MS)
- Encephalitis lethargica, subacute sclerosing panencephalitis,
- Antineuronal antibody disease
- Neurotoxins and heavy metals
- Drugs
- Anticonvulsants: valproate, carbamazepine, phenytoin
- Tetrabenazine, antidepressants, sympathomimetics, bronchodilators, beta-2 agonists
- Lithium
- Neuroleptics, metoclopramide
- Amiodarone
- Thyroid hormone replacement
- Anticancer drugs: vincristine, cisplatin, paclitaxel, doxorubicin, cytosine arabinoside, ifosfamide, tacrolimus, 5-fluorouracil, methotrexate
- Drug and alcohol withdrawal
- Others
- Brain tumors
- Brain injury: head trauma, brain surgery, and electrical injury
- Vascular: ischemia, hemorrhage, and arteriovenous malformations
- Anxiety and stress
- Fatigue
- Cooling
- Trauma of peripheral tissues
- Human immunodeficiency virus (HIV).
Hand tremors signs and symptoms
Many diseases or conditions cause tremors:
- Enhanced physiologic tremor. Caffeine use, an overactive thyroid, stress, fatigue, or sleep deprivation can intensify physiologic tremor. This tremor may show up as a postural tremor.
- Medication-induced tremor. Some medications can cause tremors, such as the antidepressant bupropion (Wellbutrin) and the anti-arrhythmic drug amiodarone (Cordarone). The resulting tremor is often postural.
- Parkinsonian tremor. This resting, pill-rolling tremor can occur with or without the degenerative neurological condition Parkinson’s disease.
- Essential tremor. This is a benign tremor that causes involuntary shaking in various body parts, including the hands, head, and voice box. A person with essential tremor may have a postural hand tremor or an intention tremor or both.
- Cerebellar tremor. This is an intention tremor caused by damage to the cerebellum in the back of the brain, often from a stroke or multiple sclerosis. The cerebellum helps coordinate movement, like reaching out to grasp a doorknob. Cerebellar damage can cause your hand to miss the doorknob.
- Post-stroke tremor. After a stroke, a person can have a variety of tremors. If there’s damage to the cerebellum there can be an intention tremor. If the damage is in the basal ganglia, the person can have a resting tremor.
- Withdrawal tremor. People suffering alcohol withdrawal can experience postural tremors.
Hand tremors that occur with activity are described based on when they appear:
- Postural tremor occurs when your hands are outstretched, and gravity is pulling them down. You can’t keep the hands completely steady while they’re outstretched.
- Intention tremor starts when you’re reaching for a target, like a keyhole as you unlock your door.
- Task-specific tremor occurs when performing an activity, such as when you’re writing.
Symptoms that could indicate your tremor is essential tremor include:
- Shaking in your hands.
- Head nodding or shaking.
- Quivering voice.
- Tremors worsen with emotional stress.
- Tremors worsen with purposeful movement.
- Rest helps to relieve tremors.
The key symptom of essential tremor is shaking — usually your hands — when you’re trying to use them. That shaking can take different forms and usually happens under certain circumstances.
- Action tremor: This is a form of essential tremor that happens during actions, such as reaching for an object.
- Postural tremor: This is shaking that happens when you hold part of your body in a specific pose, such as holding a hand outstretched and keeping it at the same height.
Essential tremor signs and symptoms:
- Begin gradually. They usually are more noticeable on one side of the body.
- Worsen with movement
- Usually occur in the hands first, affecting one hand or both hands
- Can include a “yes-yes” or “no-no” double nodding or shaking motion of the head.
- Quivering voice
- Tremors worsen with purposeful movement
- Rest helping to relieve tremors.
- Tremors may be aggravated by emotional stress, fatigue, caffeine, certain medications, low blood sugar, or temperature extremes.
Often, tremors are the only symptom you have when you have essential tremor. Other conditions that cause tremors come with other symptoms.
Essential tremor almost always affects both sides of your body but often affects one side more than the other. In addition to your hands, tremors can affect other parts of your body such as your head, voice, face and trunk.
The tremor itself isn’t dangerous, but it can cause problems with everyday activities as the condition worsens. Eventually, people with essential tremor may have trouble with activities such as eating with utensils and drinking from a glass, dressing themselves and writing.
Hand tremors diagnosis
Diagnosing hand tremor involves a review of your medical history, family history and symptoms, and a physical examination. Your doctor will want to know what it looks like and if there are any associated features. Is there balance impairment, stiffness, or slowness of movement as in Parkinson’s disease? Was there a stroke? Is there a brain lesion? Is the person taking a certain kind of medication? Does the person consume a lot of caffeine or have any other underlying conditions. It may be necessary to order lab work to check for thyroid disease or get an image of the brain to check for signs of a past stroke.
There are no medical tests to diagnose essential tremor. Diagnosing it is often a matter of ruling out other conditions that could be causing symptoms. To do this, your doctor may suggest the following tests.
Neurological examination
In a neurological examination, your doctor surveys your nervous system functioning, including checking your:
- Tendon reflexes
- Muscle strength and tone
- Ability to feel certain sensations
- Posture and coordination
- Gait
Laboratory tests
Your blood and urine may be tested for several factors, including:
- Thyroid disease
- Metabolic problems e.g. Wilson’s disease
- Drug side effects
- Alcohol levels
- Levels of metals like lead or manganese that may cause tremor
- Genetic testing. This tests for gene changes if there is a known family history of Parkinson’s disease or if you have familial tremor.
- Alpha-synuclein test. Alpha-synuclein test also called an alpha-synuclein seed amplification assay, detects Parkinson’s disease before symptoms begin. Alpha-synuclein clumps are a hallmark sign of Parkinson’s disease. Doctor can test for Parkinson’s disease in the skin or spinal fluid. Alpha-synuclein is found in Lewy bodies. It forms clumps that the body can’t break down. The clumps spread and damage brain cells. In a 2023 study, researchers tested the spinal fluid of more than 1,000 people to look for clumps of the protein alpha-synuclein. The alpha-synuclein test accurately identified people with Parkinson’s disease 87.7% of the time. Alpha-synuclein test also was highly sensitive for detecting people at risk of Parkinson’s disease. This study of the alpha-synuclein seed amplification assay was the largest so far. Some researchers say the study may be a breakthrough for Parkinson’s disease diagnosis, research and treatment trials. But larger studies are needed. There’s hope among researchers that in the future, the alpha-synuclein test could be done using blood samples rather than spinal fluid.
Imaging tests
These imaging tests can help rule out other conditions:
- Computerized tomography (CT) scan. A head CT (computed tomography) scan, also known as a CAT scan, is a medical imaging technique that uses X-rays to create detailed 3D images of the brain, skull, and surrounding structures, helping to diagnose various conditions like strokes, tumors, and injuries. These scans provide a more detailed view than a regular X-ray and can be used to diagnose a wide range of conditions.
- Magnetic resonance imaging (MRI). An head MRI (Magnetic Resonance Imaging) scan is a non-invasive medical imaging technique that uses strong magnetic fields and radio waves to create detailed images of the body’s internal structures. Your doctor can order MRI of your brain and surrounding nerve tissue inside your head using MRI.
- Positron emission tomography (PET) scan. A positron emission tomography (PET) scan is a nuclear medicine imaging technique that uses radioactive tracers to visualize and measure changes in metabolic processes within the body. These scans can help diagnose diseases, monitor treatment effectiveness, and assess organ function. Your doctor may order a PET scan to check for signs of brain disorders such as brain tumors, epilepsy, dementia and Alzheimer’s disease.
- A specific single-photon emission computerized tomography (SPECT) scan called a dopamine transporter (DAT) scan. This can help support the suspicion that you have Parkinson’s disease and help identify different types of tremor. But it is your symptoms and the results of your neurological exam that determine your diagnosis. Most people do not require a DAT scan.
Performance tests
To evaluate the tremor itself, your doctor may ask you to:
- Drink from a glass
- Hold your arms outstretched
- Write
- Draw a spiral
If your doctor is still unsure if your tremor is essential tremor or Parkinson’s disease, he or she might order a dopamine transporter scan (DaTscan). This can tell the difference between the two types of tremor. A special picture or scan of the brain that measures the uptake of dopamine, such as DaTscan, can help to differentiate between essential tremor and Parkinson’s disease tremor. Dopamine is depleted in patients with Parkinson’s disease but not in patients with essential tremor; therefore, scans showing depletion in dopamine are most likely Parkinson’s disease and normal scans would suggest a more likely diagnosis of essential tremor. These scans are used as a tool to help the physician make an accurate diagnosis in difficult cases.
Hand tremors treatment
Hand tremors treatment depends on the underlying cause of your hand tremors. Some tremors can be eliminated or dramatically reduced. For example, for enhanced physiologic tremor you may just need to cut back on caffeine or manage stress. Tremors caused by overactive thyroid or alcohol withdrawal may be reduced by treating those conditions. Medication-induced tremors may be resolved by switching to a different type of medication.
If you have mild essential tremor symptoms, you don’t need any treatment and early treatment does not stop or slow essential tremor symptomatic progression. But if your essential tremor is making it difficult for you to work or perform daily activities, discuss treatment options with your doctor. Only consider starting medication treatment when the tremor affects your daily activities or causes problems for you. Essential tremor is often treated with medications such as the beta blocker propranolol (Inderal) or the antiseizure drug primidone (Mysoline).
People with Parkinson’s disease or Parkinsonian tremors will need medicines such as carbidopa-levodopa to help control their symptoms. Medicines often work very well. When medicine is no longer helping, some people with Parkinson’s disease may have surgery called deep brain stimulation to help control parts of their brain. This surgery may help lessen symptoms. Deep brain stimulation has been approved to treat many stages of Parkinson’s disease. Electrodes are inserted in your brain, and electrical impulses are sent to stimulate it. In addition to medicine, your doctor may also recommend exercise or physical therapy that focuses on balancing and stretching, and speech therapy. These can help you control your movements better.
Tremors from multiple sclerosis, strokes, and brain tumors are not typically reversible.
Because hand tremors can interfere with eating and other tasks, it may help to use weighted eating utensils and to work with an occupational therapist for help with fine motor skills, such as buttoning clothes.
Essential tremor medications
- Beta blockers. Normally used to treat high blood pressure, beta blockers such as propranolol (Inderal) help relieve tremors in some people. This is the most common medication used for treatment of essential tremor. Multiple studies have shown that propanolol improves the symptoms ranging from 50-70% of the patients. However, no long term study has been conducted regarding the effect of propanolol in essential tremor. Other beta-blockers include atenolol, metoprolol, sotalol and nadolol. Beta blockers may not be an option if you have asthma or certain heart problems. Side effects may include fatigue, lightheadedness or heart problems.
- Anti-seizure medications. Epilepsy drugs, such as primidone (Mysoline), may be effective in people who don’t respond to beta blockers. The exact mechanism is unknown. Other medications that might be prescribed include gabapentin (Gralise, Neurontin) and topiramate (Topamax, Qudexy XR). However most of these anticonvulsants are not well studied – only small and short trials have been done to evaluate their effectiveness. Side effects include drowsiness and nausea, which usually disappear within a short time.
- Tranquilizers (benzodiazepines). Doctors may use drugs such as alprazolam (Xanax) and clonazepam (Klonopin) to treat people for whom tension or anxiety worsens tremors. Side effects can include fatigue or mild sedation. These medications should be used with caution because they can be habit-forming (addictive).
- OnabotulinumtoxinA (Botox) injections. Botulinum toxin is injected into the muscles that cause the tremor, temporarily weakening the muscle to reduce the tremor. Botox injections might be useful in treating some types of tremors, especially head and voice tremors. Botox injections can improve tremors for up to three months at a time. However, if Botox is used to treat hand tremors, it can cause weakness in your fingers. If it’s used to treat voice tremors, it can cause a hoarse voice and difficulty swallowing.
Essential tremor natural remedies
Lifestyle changes are often recommended to prevent the tremor from getting worse. Your doctor will ask you to avoid caffeine, cold medicines and certain other medicines if they seem to make your tremor worse. These medicines won’t make your tremor go away. However, the medicine may control the tremor enough to allow you to do normal activities without frustration or embarrassment.
To reduce or relieve tremors:
- Avoid caffeine. Caffeine and other stimulants can increase tremors.
- Use alcohol sparingly, if at all. Some people notice that their tremors improve slightly after they drink alcohol, but drinking isn’t a good solution. Tremors tend to worsen once the effects of alcohol wear off. Also, increasing amounts of alcohol eventually are needed to relieve tremors, which can lead to alcoholism.
- Learn to relax. Stress and anxiety tend to make tremors worse, and being relaxed may improve tremors. Although you can’t eliminate all stress from your life, you can change how you react to stressful situations using a range of relaxation techniques, such as massage or meditation.
- Make lifestyle changes. Use the hand less affected by tremor more often. Find ways to avoid writing with the hand affected by tremor, such as using online banking and debit cards instead of writing checks. Try voice-activated dialing on your cellphone and speech-recognition software on your computer.
Physical therapy
Doctors might suggest physical or occupational therapy. Physical therapists can teach you exercises to improve your muscle strength, control and coordination.
Occupational therapists can help you adapt to living with essential tremor. Therapists might suggest adaptive devices to reduce the effect of tremors on your daily activities, including:
- Heavier glasses and utensils
- Wrist weights
- Wider, heavier writing tools, such as wide-grip pens.
Nerve stimulation devices
A wearable electronic peripheral nerve stimulation device (Cala Trio, Cala kIQ) is a newer treatment option for people with essential tremor. The device is worn as a wristband for 40 minutes twice a day. It works by stimulating nerves and muscles to create a muscle response that reduces tremors. Studies have found that the device can bring some improvement for tremors.
Focused ultrasound thalamotomy
Focused ultrasound thalamotomy is a non-invasive neurosurgical procedure that uses focused ultrasound waves that travel through the skin and skull to target and destroy specific areas of the thalamus, a part of the brain involved in motor control, to reduce or eliminate tremors, particularly those associated with essential tremor or Parkinson’s disease 8, 9. During a focused ultrasound thalamotomy procedure a surgeon uses Magnetic Resonance Imaging (MRI – a medical imaging technique that uses strong magnetic fields and radio waves to create detailed, cross-sectional images of the body’s internal structures) to target the correct area of the brain and to be sure the sound waves are generating the exact amount of heat needed for the procedure.
Focused ultrasound thalamotomy is done on one side of the brain. The surgery affects the other side of the body from the one where it’s done. For example, focused ultrasound thalamotomy on the right thalamus affects the left side of your body. This is due to a phenomenon called contralateral control, where nerve pathways cross over in the brainstem, connecting the brain hemispheres to the opposite sides of the body where the left side of your brain generally controls the right side of your body, and the right side of your brain controls the left side of your body.
Focused ultrasound thalamotomy creates a lesion that can result in permanent changes to brain function. Some people have experienced altered sensation, trouble with walking or difficulty with movement. However, most complications go away on their own or are mild enough that they don’t interfere with quality of life.
Surgery
Deep brain stimulation (DBS) might be an option if your tremors are severely disabling and you don’t respond to medications. The surgical procedures are stereotactic thalamotomy or thalamic deep brain stimulation. Excellent results have been reported from these surgeries.
In deep brain stimulation, doctors insert a long, thin electrical probe into the portion of your brain that causes your tremors (thalamus). A wire from the probe runs under your skin to a pacemaker-like device (neurostimulator) implanted in your chest. This device transmits painless electrical pulses to interrupt signals from your thalamus that may be causing your tremors.
Side effects of surgery can include equipment malfunction; problems with motor control, speech or balance; headaches; and weakness. Side effects often go away after some time or adjustment of the device.
Figure 1. Deep brain stimulation
Coping and support
For many people, essential tremor can have serious social and psychological consequences. If the effects of essential tremor make it difficult to live your life as fully as you once did, consider joining a support group like International Essential Tremor Foundation (https://www.essentialtremor.org/).
Support groups aren’t for everyone, but you might find it helpful to have the encouragement of people who understand what you’re going through. Or see a counselor or social worker who can help you meet the challenges of living with essential tremor.
Hand tremors prognosis
Hand tremors prognosis depends on the underlying cause and severity of your hand tremors. Hand tremors, particularly in the context of essential tremor, typically have a progressive nature, meaning they tend to worsen over time. However, the progression is often slow, and the tremors might stabilize or remain stable in some individuals. While essential tremor is not life-threatening, it can significantly impact daily life and activities
Survival in essential tremor does not differ from the general population 1, 10. Although there is no associated death rate, it can cause significant inconvenience to the patients and the overall quality of life can be significantly impaired with essential tremor 10. This is due to the social and functional embarrassment that usually occur in activities of daily living such as employment, normal outing activities such as difficulty writing, eating, and drinking, attending parties, shopping alone, etc. As much as 85% of the patients with essential tremor reported that this condition affected their lifestyle in certain ways. Essential tremor symptoms are typically progressive and potentially disabling, often forcing patients to change jobs or seek early retirement 11, 12, 13, 14.
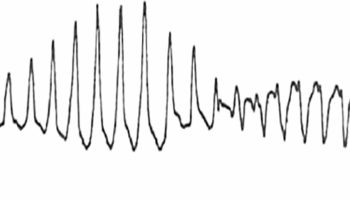
Although prospective longitudinal data are limited, the usual course of essential tremor is one of slow, gradual progression 15, 1. The average rate that arm or hand tremors get worse is between 1.5% and 5% a year. As essential tremor progresses, tremor frequency (number of repetitions per second) may decrease; however, tremor amplitude (magnitude/strength) may increase. Increased amplitude is associated with a decreased ability to manage fine, discrete motor tasks. Essential tremor starts small and usually only affects your hands at first. Over time, usually many years, the tremors may spread to affect your arm and head. As the condition progresses, you may begin to struggle with certain activities and may need help to do them.
Essential tremor may remain stable in a minority of patients. However, a stable course should raise suspicion for an alternative diagnosis such as an enhanced, physiologic tremor or drug-induced tremor rather than an essential tremor 1. While prospective data are limited, essential tremors may be associated with an increased risk for developing Parkinson disease 1.
- Agarwal S, Biagioni MC. Essential Tremor. [Updated 2023 Jul 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499986[↩][↩][↩][↩][↩]
- Santos, P.S.A., Santos, E.G.R., Monteiro, L.C.P. et al. The hand tremor spectrum is modified by the inertial sensor mass during lightweight wearable and smartphone-based assessment in healthy young subjects. Sci Rep 12, 16808 (2022). https://doi.org/10.1038/s41598-022-21310-4[↩]
- Abdo WF, van de Warrenburg BP, Burn DJ, Quinn NP, Bloem BR. The clinical approach to movement disorders. Nat Rev Neurol. 2010 Jan;6(1):29-37. doi: 10.1038/nrneurol.2009.196[↩]
- Tremor. https://www.ninds.nih.gov/health-information/disorders/tremor[↩]
- A quick guide to understanding tremor. https://magazine.medlineplus.gov/article/a-quick-guide-to-understanding-tremor[↩]
- Bhatia KP, Bain P, Bajaj N, Elble RJ, Hallett M, Louis ED, Raethjen J, Stamelou M, Testa CM, Deuschl G; Tremor Task Force of the International Parkinson and Movement Disorder Society. Consensus Statement on the classification of tremors. from the task force on tremor of the International Parkinson and Movement Disorder Society. Mov Disord. 2018 Jan;33(1):75-87. doi: 10.1002/mds.27121[↩]
- What is PolG? https://umdf.org/polg/[↩]
- Parkinson’s Disease. https://www.fusfoundation.org/diseases-and-conditions/parkinsons-disease[↩]
- Focused Ultrasound for Parkinson’s and Essential Tremor. https://www.barrowneuro.org/treatment/focused-ultrasound-thalamotomy[↩]
- Essential Tremor: Essential Facts for Patients. https://www.movementdisorders.org/MDS-Files1/Resources/PDFs/Essentialtremorpatientleaflet.pdf[↩][↩]
- Pahwa R, Dhall R, Ostrem J, Gwinn R, Lyons K, Ro S, Dietiker C, Luthra N, Chidester P, Hamner S, Ross E, Delp S. An Acute Randomized Controlled Trial of Noninvasive Peripheral Nerve Stimulation in Essential Tremor. Neuromodulation. 2019 Jul;22(5):537-545. doi: 10.1111/ner.12930[↩]
- Prasad S, Bhalsing KS, Jhunjhunwala K, Lenka A, Binu VS, Pal PK. Phenotypic Variability of Essential Tremor Based on the Age at Onset. Can J Neurol Sci. 2019 Mar;46(2):192-198. doi: 10.1017/cjn.2018.384[↩]
- Brogley JE. DaTQUANT: The Future of Diagnosing Parkinson Disease. J Nucl Med Technol. 2019 Mar;47(1):21-26. doi: 10.2967/jnmt.118.222349[↩]
- Iacono MI, Atefi SR, Mainardi L, Walker HC, Angelone LM, Bonmassar G. A Study on the Feasibility of the Deep Brain Stimulation (DBS) Electrode Localization Based on Scalp Electric Potential Recordings. Front Physiol. 2019 Jan 4;9:1788. doi: 10.3389/fphys.2018.01788[↩]
- Putzke JD, Whaley NR, Baba Y, Wszolek ZK, Uitti RJ, Essential tremor: predictors of disease progression in a clinical cohort, J. Neurol. Neurosurg. Psychiatry 77 (2006) 1235–1237, 10.1136/jnnp.2006.086579[↩]