Acoustic reflex
Acoustic reflex also known as the acoustic middle-ear-muscle reflex or stapedius reflex, is a reflexive or involuntary contraction of the stapedius muscle in response to high-intensity acoustic stimuli (loud sound), leading to changes in the acoustic immittance characteristics of the middle ear 1. The stapedial reflex stiffens the middle ear system, causing a reduction in the transfer of low-frequency energy. The acoustic reflex decreases the transmission of vibrational energy to the cochlea, where it is converted into electrical impulses to be processed by the brain. When presented with an intense sound stimulus, the stapedius and tensor tympani muscles of the ossicles contract. The stapedius stiffens the ossicular chain by pulling the stapes of the middle ear away from the oval window of the cochlea and the tensor tympani muscle stiffens the ossicular chain by loading the tympanic membrane when it pulls the malleus (hammer) in toward the middle ear. The acoustic reflex pathway ascends from the peripheral auditory system to the brainstem and then descend both ipsilaterally and contralaterally, so presentation of a loud sound in one ear results in bilateral contraction of the stapedius muscles. The acoustic reflex is mediated in the lower pons, and, therefore, reflects only a small portion of the central auditory nervous system. The acoustic reflex, however, can provide insight as to central auditory dysfunction in the caudal brainstem.
Measurement of acoustic reflex thresholds has been a standard element of the audiological test battery, valuable especially in the diagnosis of middle-ear and retrocochlear disorders. The acoustic reflex and other audiologic tests (e.g., air and bone conduction thresholds, tympanometry, and reflex decay) can help differentiate middle-ear, cochlear, and 8th cranial nerve problems; however, these tests are not able to differentiate auditory nerve from low brainstem involvement.
The clinical procedure for assessing the acoustic reflex threshold involves presenting a low-frequency probe tone (i.e., 226 Hz) to one ear, presenting high-intensity signals to the same or the other (contralateral) ear, and monitoring a decrease in the acoustic admittance of the probe tone in response to the presentation of the high-level signal. The minimum stimulus level that results in an observable decrease in acoustic admittance is defined as the acoustic reflex threshold. Acoustic reflex thresholds are usually measured from 500-2000 Hz, in both ipsilateral and contralateral modes, for each ear.
For the ipsilateral or uncrossed acoustic reflex, stimulate the ear that is monitored for response. The assessed pathway involves the cochlea, ventral cochlear nucleus, CN VIII, CN VII and its motor nucleus, and the stapedius muscle—all on the side ipsilateral to the stimulus.
For the contralateral or crossed acoustic reflex, present the stimulus to the ear opposite the ear that is monitored for response. The assessed pathway involves the ipsilateral cochlea, ventral cochlear nucleus, and CN VIII; the pathway crosses the trapezoid body and then involves the contralateral medial superior olive, CN VII and its motor nucleus, and the stapedius muscle.
In listeners with normal hearing, the acoustic reflex threshold is elicited at levels approximating 85 dB hearing level (+/− 10 dB). The acoustic reflex is absent if the signal doesn’t reach the cochlea with sufficient intensity, if there is damage affecting any of the structures along the acoustic reflex pathway, or if there is a stiff middle ear system in the probe ear. Examples of conditions in which the acoustic reflex is absent include conductive hearing loss of 25 dB hearing level or greater in the stimulus ear, conductive hearing loss of 10 dB hearing level or greater in the probe ear, sensorineural hearing loss exceeding 75 dB hearing level in the stimulus ear, a lesion of the facial nerve in the probe ear, and a lesion in the auditory brainstem affecting the crossing pathway of the acoustic reflex arc. The acoustic reflex may also be absent with a lesion of the vestibulocochlear nerve in the stimulus ear, depending on the extent of the lesion. The acoustic reflex is expected to be present in cases of mild, moderate, or moderately severe sensorineural hearing loss associated with a cochlear lesion. The acoustic reflex threshold generally increases as a function of pure-tone threshold in these cases 2.
Acoustic reflexes are remarkably sensitive to retrocochlear dysfunction given the ease with which they can be obtained 3. In a study of 30 individuals with surgically confirmed cerebellopontine angle tumours and 30 controls matched for hearing loss, the crossed acoustic reflex was found to have a sensitivity of 83% and a specificity of 97% 4. Similarly, a study of 89 individuals with 8th cranial nerve tumors found the sensitivity of the acoustic reflex to be 84% 5. Acoustic reflexes are also sensitive to auditory neuropathy: In a large multi-site study, acoustic reflexes were either absent or elevated in all individuals with auditory neuropathy that were subjected to the measurement (n = 148) 6.
Suspicion of neural dysfunction clearly warrants electrophysiological assessment and a referral for magnetic resonance imaging, but if acoustic reflexes are not measured in the first place, there may be no grounds for suspicion. Recall that significant threshold asymmetries are only present in about 80–90% of individuals with confirmed lesions (depending on the criteria selected for a identifying a significant asymmetry) 7 and abnormal acoustic reflexes can be found in cases of retrocochlear dysfunction even when thresholds are normal. Abnormal speech scores are present in a still smaller proportion of cases with retrocochlear involvement 3.
Recently, renewed interest in the acoustic reflex has been provoked by the discovery of noise-induced cochlear synaptopathy—the loss of synapses between cochlear inner hair cells and auditory nerve fibers, which can occur without widespread hair cell loss or permanent threshold elevation 8. Detection of synaptopathy in living humans requires noninvasive metrics of auditory nerve function, and the acoustic reflex may be of value. In a mouse model of synaptopathy, acoustic reflex measures correlated more closely with synaptic survival than auditory-brainstem-response measures, with acoustic reflex thresholds proving superior to acoustic reflex amplitude in predicting synapse counts 9. In investigations of tinnitus-related synaptopathy, both acoustic reflex amplitude 10 and acoustic reflex thresholds 11 have been adopted as proxy measures of auditory nerve function.
Ear hearing anatomy
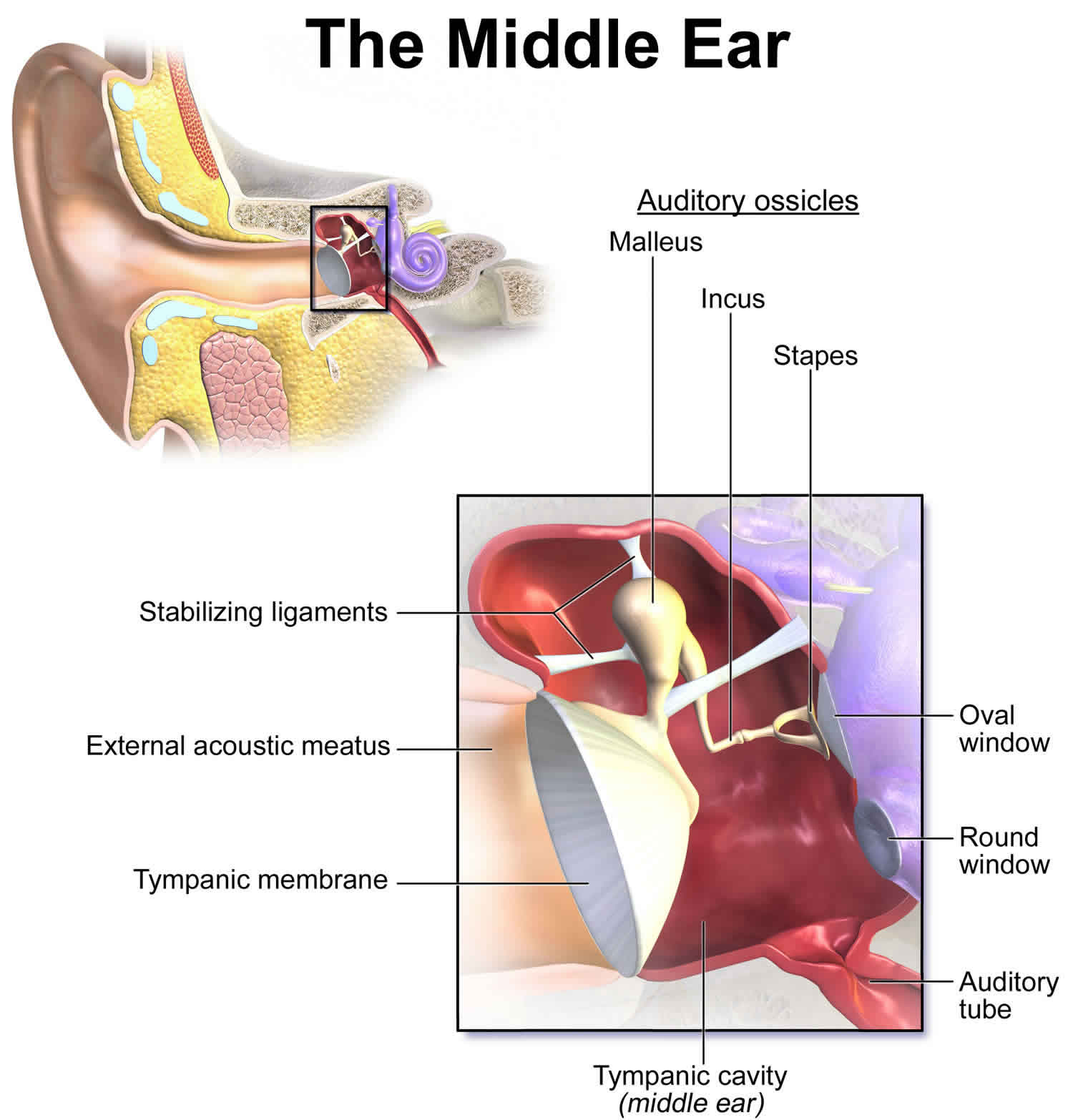
The primary functionality of the middle ear (tympanic cavity) is that of bony conduction of sound via transference of sound waves in the air collected by the auricle to the fluid of the inner ear. The middle ear inhabits the petrous portion of the temporal bone and is filled with air secondary to communication with the nasopharynx via the auditory (eustachian) tube.
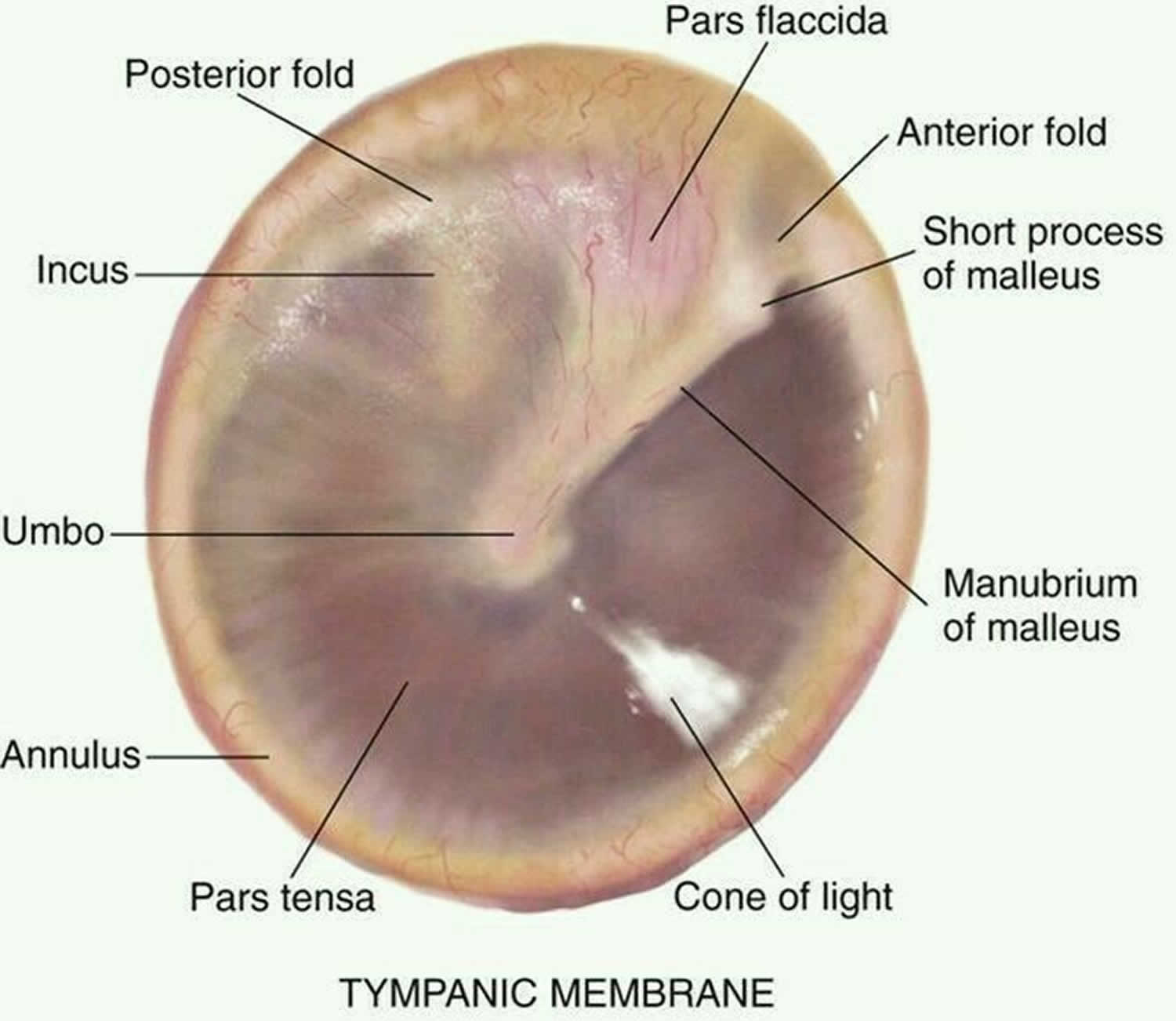
The tympanic membrane is an oval, thin, semi-transparent membrane that separates the external and middle ear (tympanic cavity). The tympanic membrane is divided into 2 parts: the pars flaccida and the pars tensa. The manubrium of the malleus is firmly attached to the medial tympanic membrane; where the manubrium draws the tympanic membrane medially, a concavity is formed. The apex of this concavity is called the umbo. The area of the tympanic membrane superior to the umbo is termed the pars flaccida; the remainder of the tympanic membrane is the pars tensa.
Figure 1. Ear anatomy

Figure 2. Middle ear anatomy

Figure 3. Tympanic membrane (right ear)
Acoustic reflex arc
Much of what is currently known about the human acoustic reflex arc is based on the work of Borg on rabbits 12 with considerable contributions from Møller 13. The acoustic reflex is mediated by the stapedius muscle in the middle ear, which contracts in response to moderate-to-loud acoustic stimulation, reducing the admittance of the ossicular chain. The lowest level of acoustic energy needed to produce a significant change in admittance, generally defined as at least 0.02 mmho, is called the acoustic reflex threshold. The reflex is consensual, so that when one ear is stimulated, both pathways respond. Therefore there are two recording conditions possible: an ipsilateral condition where the stimulus is presented to the same ear in which the measurement probe is monitoring immittance, and a contralateral condition where the sound is presented contralaterally to the ear in which immittance is being monitored. The general practice is use pure tone stimuli at 500, 1000 and 2000 Hz, although 4000 Hz is sometimes also used. There may be times when broadband noise is used as the stimulus, which can be compared to pure tone reflex data to provide objective information about the status of the cochlea 14. Normative data for acoustic reflex thresholds are available for normal hearing and for varying degrees of cochlear hearing loss, and range from 75 to 90 dB hearing level. Generally the intensity needed to elicit a response increases with increasing levels of cochlear hearing loss.
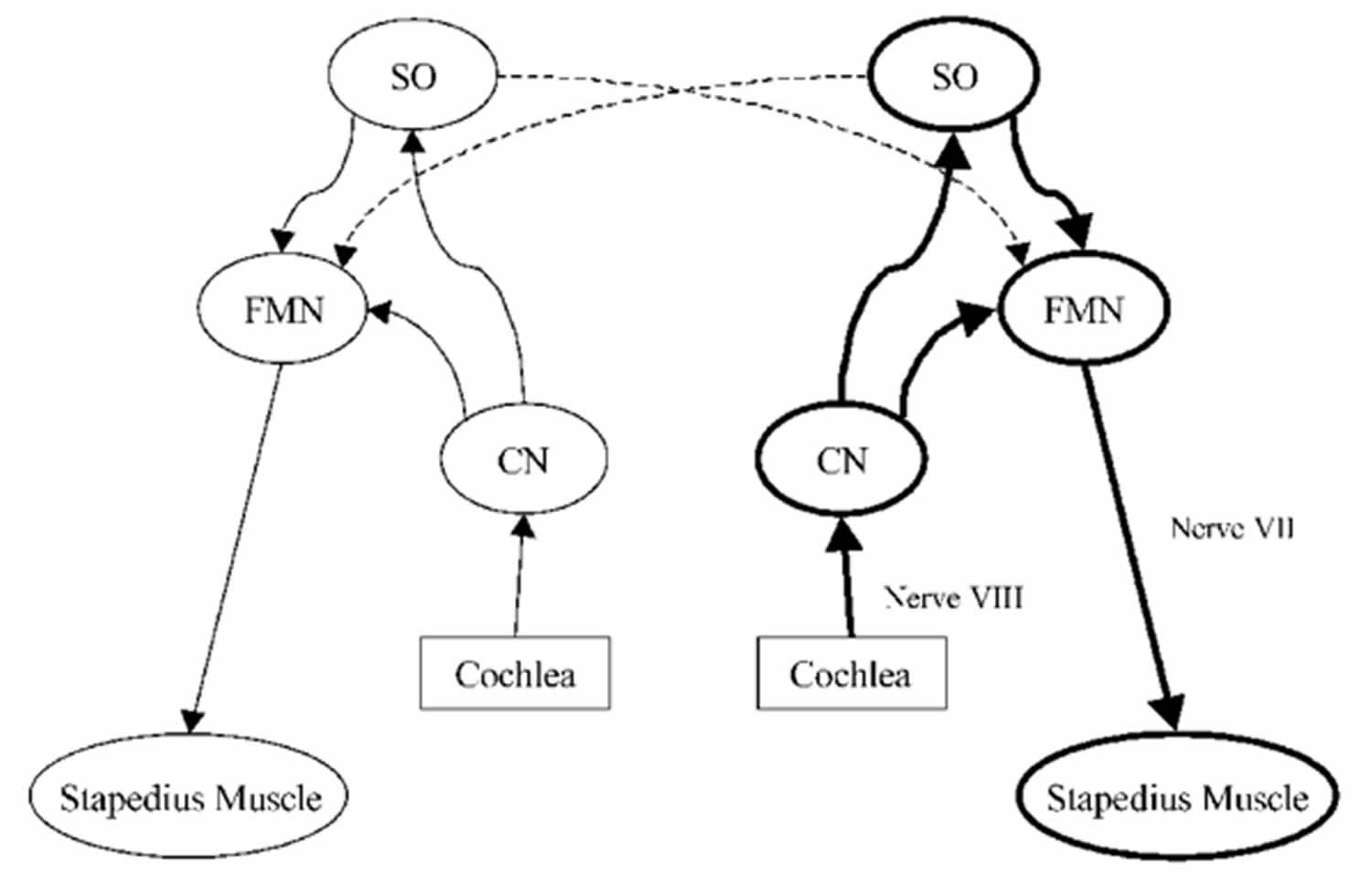
The acoustic reflex is triggered when an ear is stimulated with a moderately intense signal that reaches the ventral cochlear nucleus and is projected via one of two tracts: one leading directly to the facial nerve nucleus on the same side and another that crosses the midline of the brainstem and connects with the contralateral superior olivary complex. The cochlear nucleus also sends a tract to the ipsilateral superior olivary complex which connects to its partner in the contralateral field, as well as both facial nerve nuclei, both ipsilaterally and contralaterally. The efferent portion of the pathway from the facial nerve nucleus to the facial nerve runs through the internal auditory meatus and into the middle ear where it connects with the stapedius muscle 15. Because of the complexity of the acoustic reflex arc and its involvement with both peripheral and central mechanisms, it can be impacted by outer, middle, and inner ear pathologies, as well as by pathology of the auditory nerve and lower brainstem. Acoustic reflexes are typically not present for conductive hearing losses.
The reflex is triggered when an ear is stimulated with a moderately intense signal that reaches the ventral cochlear nucleus (CN) and is projected via one of two tracts: one leading directly to the facial nerve nucleus on the same side and another that crosses the midline of the brainstem and connects with the contralateral superior olivary complex (SOC). The cochlear nucleus also sends a tract to the ipsilateral SOC which connects to its partner in the contralateral field, as well as both facial nerve nuclei, both ipsilaterally and contralaterally. The efferent portion of the pathway from the facial nerve nucleus to the facial nerve runs through the internal auditory meatus and into the middle ear where it connects with the stapedius muscle.7 Because of the complexity of the arc and its involvement with both peripheral and central mechanisms, it can be impacted by outer, middle, and inner ear pathologies, as well as by pathology of the auditory nerve and lower brainstem. Reflexes are typically not present for conductive hearing losses.
One of the most common methods to characterize different patterns of acoustic reflex activation in relation to site of lesion was developed by Jerger8,9 (see Hall and Swanepoel6 for further information), and includes five patterns based on both ipsilateral and contralateral measures: “vertical” (reflexes absent in one probe/measurement ear), “diagonal” (reflexes absent in one stimulus ear), “horizontal” (both contralateral reflexes absent), “inverted L” (both contralateral reflexes absent and one unilateral reflex absent) and “uni-box” (one reflex absent). Along with audiometric and tympanometric results, acoustic reflex recordings that typify these five patterns can be used to provide an initial estimate of the site of lesion.
Figure 4. Acoustic reflex arc
Footnote: Reflex arc of the middle ear acoustic reflex: nerve VIII = auditory nerve; nerve VII = facial nerve; CN = cochlear nucleus; SO = superior olive; FMN = facial motonucleus.
Acoustic reflex thresholds
The acoustic reflex threshold is the sound pressure level (SPL) from which a sound stimulus with a given frequency will trigger the acoustic reflex. The acoustic reflex threshold is a function of sound pressure level and frequency. Acoustic reflex threshold is a middle ear measurement of stapedius muscle response to higher intensity and adequate duration sounds for individual frequencies. Consider the softest sound that elicits a reflex contraction of the stapedius muscle as the acoustic reflex threshold. When the stapedius muscle contracts in response to a loud sound, that contraction changes the middle ear immittance. This change in immittance can be detected as a deflection in the recording.
Tympanometry records changes in middle ear immittance, while air pressure is varied in the ear canal and acoustic reflexes are recorded at a single air pressure setting (ie, the pressure setting that provided the peak immittance reading for that particular ear on the tympanogram). Ear canal pressure is maintained at that specific setting, while tones of various intensities are presented into the ear canal and immittance is recorded. A significant change in middle ear immittance immediately after the stimulus is considered an acoustic reflex.
A stapedial muscle contraction in response to an intense signal occurs bilaterally in normal ears with either unilateral or bilateral stimulation. This reaction occurs because the stapedial reflex pathway has both ipsilateral and contralateral projections. Acoustic reflex thresholds generally are determined in response to stimuli of 500, 1000, 2000, and 4000 Hz. For screening purposes, or for a general check of the pathway’s integrity, usually test at 1000 Hz.
People with normal hearing have an acoustic reflex threshold around 70–100 dB sound pressure level (SPL). People with conductive hearing loss (i.e. bad transmission in the middle ear) may have a greater or absent acoustic reflex threshold 16.
The acoustic reflex threshold is usually 10–20 dB below the discomfort threshold. However the discomfort threshold is not a relevant indicator of the harmfulness of a sound: industry workers tend to have a higher discomfort threshold, but the sound is just as harmful to their ears 17.
The acoustic reflex threshold can be decreased by the simultaneous presentation of a second tone (facilitator). The facilitator tone can be presented to either ear. This facilitation effect tends to be greater when the facilitator tone has a frequency lower than the frequency of the elicitor (i.e. the sound used to trigger the acoustic reflex) 18.
Variability of acoustic reflex thresholds
Thresholds vary according to individual hearing sensitivity and retrocochlear function. The range for acoustic reflexes in individuals with normal hearing averages 70-100 decibel (dB) sound pressure level (SPL). The greater the hearing loss, the higher the acoustic reflex threshold for conductive hearing loss. For sensorineural hearing loss, acoustic reflex thresholds may be within the normal range, particularly for mild-to-moderate hearing losses with recruitment.
Elevated or absent acoustic reflex thresholds (ie, >100 dB sound pressure level) for any given frequency may suggest sensorineural or conductive hearing loss, facial nerve disorder, or middle ear disorder. Reflexes usually are absent or cannot be recorded if the patient has type B tympanograms; therefore, acoustic reflexes generally are not tested in these ears.
For example, if the ear canal is occluded with cerumen, a type B tympanogram with low volume will be recorded. In this case, acoustic reflexes cannot be measured because middle ear immittance is not being measured. (Cerumen blocks the signal.)
For a type B tympanogram with normal volume (as in otitis media) no pressure peak for immittance is obtained. The pressure between the ear canal and middle ear are not equilibrated, and acoustic reflexes cannot be recorded.
For a type B tympanogram with high volume (as in the presence of patent pressure equalization tubes or perforated tympanic membranes), an open exchange of air occurs between the ear canal and middle ear; thus, any contraction of the stapedius muscle cannot be measured.
- Guest H, Munro KJ, Couth S, et al. No Effect of Interstimulus Interval on Acoustic Reflex Thresholds. Trends Hear. 2019;23:2331216519874165. doi:10.1177/2331216519874165 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6852360[↩]
- Silman, S., and Gelfand, S.A. (1981). The relationship between magnitude of hearing loss and acoustic reflex threshold levels. Journal of Speech and Hearing Disorders , 46(3), 312-316.[↩]
- Bergenius J, Borg E, Hirsch A. Stapedius reflex test, brainstem audiometry and opto-vestibular tests in diagnosis of acoustic neurinomas. Acomparison of test sensitivity in patients with moderate hearing loss. Scand Audiol 1983;12:3–9.[↩][↩]
- Olsen WO, Bauch CD, Harner SG. Application of Silman and Gelfand (1981) 90th percentile levels for acoustic reflex thresholds. J SpeechHear Dis 1983;48:330–32.[↩]
- Godey B, Morandi X, Beust L, et al. Sensitivity of auditory brainstem response in acoustic neuroma screening. Acta Otolaryngol;118:501–504.[↩]
- Berlin CI, Hood LJ, Morlet T, et al. Multi-site diagnosis and management of 260 patients with auditory neuropathy/dys-synchrony (auditoryneuropathy spectrum disorder). Int J Audiol 2010;49:30–43.[↩]
- Cheng TC, Wareing MJ. Three-year ear, nose, and throat cross-sectional analysis of audiometric protocols for magnetic resonance imagingscreening of acoustic tumors. Otolaryngol Head Neck Surg 2012;146:438–447.[↩]
- Liberman M. C., Kujawa S. G. (2017) Cochlear synaptopathy in acquired sensorineural hearing loss: Manifestations and mechanisms. Hearing Research 349: 138–147. doi:10.1016/j.heares.2017.01.003[↩]
- Valero M. D., Hancock K. E., Maison S. F., Liberman M. C. (2018) Effects of cochlear synaptopathy on middle-ear muscle reflexes in unanesthetized mice. Hearing Research 363: 109–118. doi:10.1016/j.heares.2018.03.012[↩]
- Wojtczak M., Beim J. A., Oxenham A. J. (2017) Weak middle-ear-muscle reflex in humans with noise-induced tinnitus and normal hearing may reflect cochlear synaptopathy. ENeuro 4(6): ENEURO.0363-17.2017. doi:10.1523/ENEURO.0363-17.2017[↩]
- Guest H., Munro K. J., Plack C. J. (2019. a) Acoustic middle-ear-muscle-reflex thresholds in humans with normal audiograms: No relations to tinnitus, speech perception in noise, or noise exposure. Neuroscience, 407, 75–82.. doi:10.1016/j.neuroscience.2018.12.019[↩]
- Borg E. On the neuronal organization of the acoustic middle ear reflex: A physiological and anatomical study. Brain Res 1973;49:101–23.[↩]
- Møller AR. Hearing; Anatomy, Physiology, and Disorders of the Auditory System. San Diego: Plural Publishing; 2012.[↩]
- Hall JW, Swanepoel deW. Objective Assessment of Hearing. San Diego: Plural Publishing; 2010.[↩]
- Musiek F, Baran J. The Auditory System: Anatomy, Physiology and Clinical Correlates. Boston: Pearson, Allyn & Bacon; 2007.[↩]
- Impedance Audiometry. https://emedicine.medscape.com/article/1831254-overview[↩]
- W. Niemeyer (1971). “Relations between the Discomfort Level and the Reflex Threshold of the Middle Ear Muscles”. International Journal of Audiology. 10 (3): 172–176. doi:10.3109/00206097109072555[↩]
- Kawase, Tetsuaki; Takasaka, Tomonori; Hidaka, Hiroshi (June 1997). “Frequency summation observed in the human acoustic reflex”. Hearing Research. 108 (1–2): 37–45. doi:10.1016/s0378-5955(97)00039-7[↩]