What is acne Acne, pimples or zits, is a chronic inflammatory disorder of pilosebaceous (sebaceous gland a small gland in the skin which secretes a lubricating
What is antiperspirant An antiperspirant is a chemical agent that reduces perspiration or sweating. The active ingredients of roll-on, spray and powder formulations are traditionally
Tips for raising children Being a parent can be great fun, with lots of opportunities for love and excitement. It also brings challenges and hard
How to deal with a difficult child Becoming a parent is one of the biggest role you’ll ever take on. It’s one of the few
What is loneliness Loneliness or being lonely is about not feeling connected to others. You can feel lonely in a room full of people. The
How to fix a broken relationship with your girlfriend or boyfriend A relationship can start with you feeling on top of the world, but it
How to deal with a broken heart A broken heart, relationship breakup and divorce are among the toughest life experiences people can face at any
How to deal with divorce as a man or a woman Divorce and separation are among the toughest life experiences people can face. Men and
What to do after a breakup A romantic relationship breakup, separation and divorce are one of the most stressful and emotional experiences in life. People
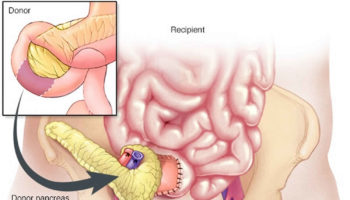
Can you get a pancreas transplant? Yes. More than 50,000 pancreas transplant have been performed worldwide (> 29,000 from the United States and >19,000 from