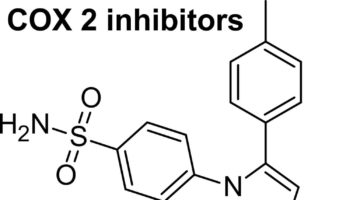
What is a COX-2 inhibitor COX-2 inhibitor is short for cyclooxygenase-2 selective inhibitor, is a non-steroidal anti-inflammatory drug (NSAID) that is the competitive inhibitor of
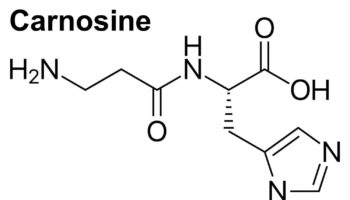
What is carnosine Carnosine (beta-alanyl-L-histidine) is a naturally occurring dipeptide neuropeptide (dipeptide of the amino acids beta-histidine and 3-methyl-L-histidine) found in mammalian tissues ((Hipkiss, A.R.;
What is the Dukan diet The Dukan diet is a low-carb, low-fat and high-protein diet and eating plan that is based on proteins and vegetables,
What is sexsomnia Sexsomnia also called "sleep sex" or "atypical sexual behavior during sleep" or "somnambulistic sexual behavior", refers to sexual acts that are carried
What is overpronation Overpronation or excessive pronation or eversion in frontal plane at ankle joint in heel-toe running, refers to the tendency of the medial
What is pareidolia Pareidolia is the interpretation of previously unseen and unrelated objects as familiar due to previous learning ((Akdeniz G, Toker S, Atli I.
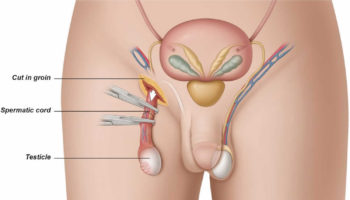
What is orchiectomy Orchiectomy is a surgical procedure to remove one or both testicles. If only one testicle is removed, this is known as unilateral
What is synesthesia Synesthesia is an extraordinary way of perceiving the world, involving experiences of connections between seemingly unrelated sensations, images or thoughts ((Brogaard B.
What are tonsil stones Tonsil stones are also known as tonsilloliths, are small white or yellow lumps of hardened material that can form in the palatine
What is XYY syndrome XYY syndrome is also known as 47XYY syndrome or Jacob's syndrome, is characterized by an extra copy of the Y chromosome