Bishop score
Bishop score or Bishop’s score, is a pre-labor scoring system to assist in predicting whether induction of labor will be required 1. To prepare for labor and delivery, the cervix begins to soften (ripen), thin out, and open. These changes usually start a few weeks before labor begins. Labor and delivery nurses or an obstetricians use the Bishop score to rate the readiness of the cervix for labor. With Bishop scoring system, a number ranging from 0–13 is given to rate the condition of the cervix. A Bishop score of less than 6 means that your cervix may not be ready for labor. However, avoid digital cervical exams in a patient with placenta previa or before establishing a diagnosis of preterm rupture of membranes 2.
The Bishop score reflects the normal changes the cervix undergoes in the process of childbirth (parturition) 2. Extensive cervical remodeling is needed for the cervix to dilate and pass a fetus fully. While human parturition (process of childbirth) is not completely understood, it is a complex system that involves interactions between placental, fetal, and maternal mechanisms. The nonpregnant cervix extracellular matrix is primarily made up of tightly packed collagen bundles. Gradually throughout the pregnancy the composition of the cervix changes with decreased collagen density and an increase in hyaluronic acid and water content. In the days to weeks before delivery, through a cascade of events, inflammatory mediators increase the production of prostaglandins. Prostaglandins invading the cervix mediate the release of metalloproteases that break down collagen and change the cervical structure. Cervical softening and distention results from these extracellular matrix compositional changes, specifically, increased vascularity and stromal and glandular hypertrophy, and are due in part to an increase in collagen solubility.
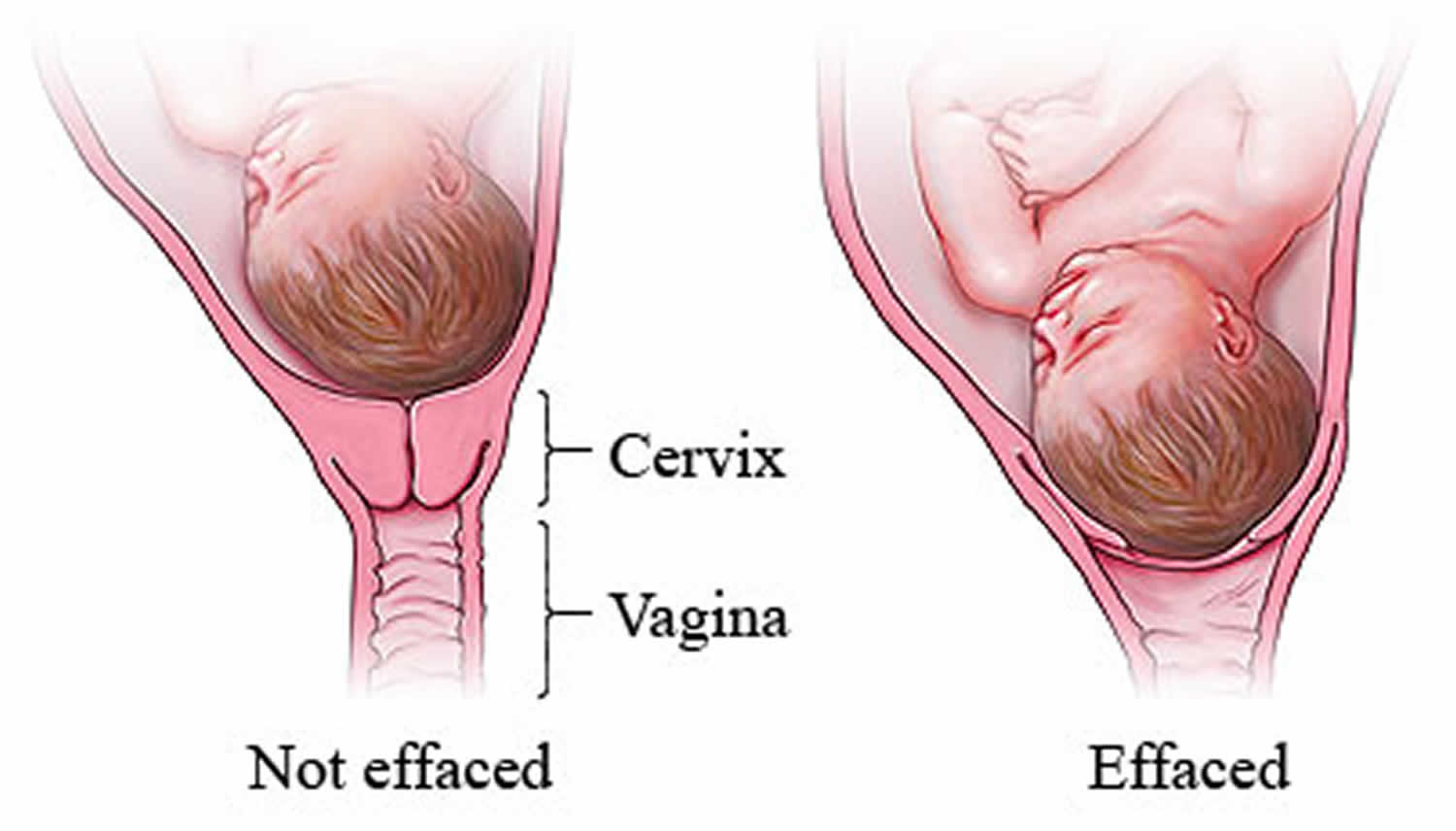
Figure 1. Cervical effacement
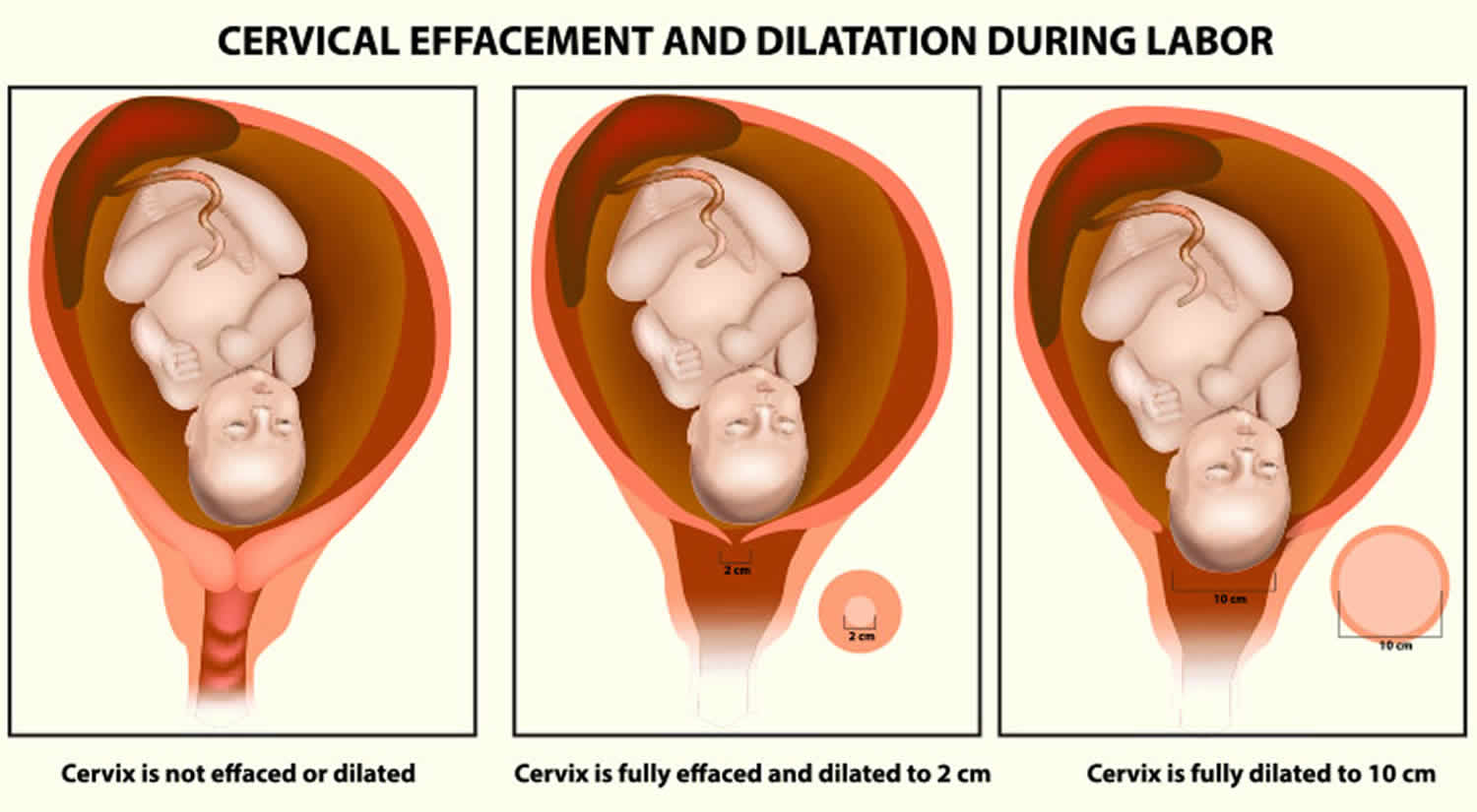
Figure 2. Cervical dilation
Footnote: As labor nears, the fetus’s head drops down into the pelvis and pushes against the cervix. The cervix begins to thin (efface) and open (dilate), sometimes over a few weeks.
What is labor induction?
Induction of labor may be defined as ‘an intervention designed to initiate uterine contractions artificially leading to progressive effacement and dilatation of the cervix and birth of the baby’ 3.
Labor induction is the use of medications or other methods to bring on (induce) labor. Induction of labor is a commonplace obstetric practice. Currently, more than 20% of pregnant women in the United States deliver as a result of labor induction. Predictors for success in induction include many of the similar criteria Bishop set forth in the 1960s 1.
Why is labor induced?
Labor is induced to stimulate contractions of the uterus in an effort to have a vaginal birth. Labor induction may be recommended if the health of the mother or fetus is at risk. In special situations, labor is induced for nonmedical reasons, such as living far away from the hospital. This is called elective induction. Elective induction should not occur before 39 weeks of pregnancy.
What is “ripening the cervix”?
Cervical ripening refers to softening, effacement (thinning) and dilatation of the cervix 4., which can be assessed with a (modified) Bishop score (< 5 or ≥ 5). Ripening the cervix is a process that helps the cervix soften and thin out in preparation for labor. Medications or devices may be used to soften the cervix so it will stretch (dilate) for labor.
How is cervical ripening performed?
Ripening of the cervix can be done with prostaglandins or with special devices.
What are prostaglandins?
Prostaglandins are drugs that can be used to ripen the cervix. They are forms of chemicals produced naturally by the body. These drugs can be inserted into the vagina or taken by mouth. Some of these drugs are not used in women who have had a previous cesareandelivery or other uterine surgery to avoid increasing the possible risk of uterine rupture (tearing).
Dinoprostone is prostaglandin E2 (available as Prostin® E2 vaginal gel 1 mg and 2 mg OR Cervidil®; 10 mg vaginal pessary) and is currently used for pre-induction cervical ripening.
Onset of labor after dinoprostone gel administration is variable (6 – 18 hours).
What devices are used to ripen and dilate the cervix?
Laminaria (a substance that absorbs water) can be inserted to expand the cervix. A catheter (small tube) with an inflatable balloon on the end also can be inserted to widen the cervix.
What is “stripping the membranes”?
Stripping the membranes is a way to induce labor. The health care professional sweeps a gloved finger over the thin membranes that connect the amniotic sac to the wall of your uterus. This action may cause your body to release prostaglandins, which soften the cervix and may cause contractions.
How can rupturing the amniotic sac bring on labor?
Rupturing the amniotic sac can start contractions. It also can make them stronger if they have already begun. The health care professional makes a small hole in the amniotic sac with a special tool. This procedure, called an amniotomy, may cause some discomfort.
When is amniotomy done?
Amniotomy is done to start labor when the cervix is dilated and thinned and the fetus’s head has moved down into the pelvis. Most women go into labor within hours after the amniotic sac breaks (their “water breaks”).
What is oxytocin?
Oxytocin is a hormone that causes contractions of the uterus. It can be used to start labor or to speed up labor that began on its own. Contractions usually start about 30 minutes after oxytocin is given.
What are the risks associated with labor induction?
With some methods, the uterus can be overstimulated, causing it to contract too frequently. Too many contractions may lead to changes in the fetal heart rate, umbilical cord problems, and other problems.
Other risks of cervical ripening and labor induction include the following:
- Infection in the mother or fetus
- Uterine rupture
- Increased risk of cesarean birth
- Fetal death
Medical problems that were present before pregnancy or occurred during pregnancy may contribute to these complications.
Is labor induction always effective?
Sometimes labor induction does not work. A failed attempt at induction may mean that you will need to try another induction or have a cesarean delivery. The chance of having a cesarean delivery is greatly increased for first-time mothers who have labor induction, especially if the cervix is not ready for labor.
Bishop scoring system
The Bishop scoring system is based on a digital cervical exam of a patient with a zero point minimum and 13 point maximum 2. The Bishop scoring system utilizes cervical dilation, position, effacement (thinning), consistency of the cervix, and fetal station. Cervical dilation, effacement, and station are scored 0 to 3 points, while cervical position and consistency are scored 0 to 2 points (see Table 1 below) 5.
The total Bishop score is achieved by assessing the following five components on vaginal examination:
- Cervical dilatation: Cervical dilation is the measure of how dilated the cervix is in centimeters. This is performed by estimating the average diameter of the open cervix.
- Cervical effacement: Cervical effacement is the thinning or shortening of the cervix expressed as a percentage of the whole cervix. Zero percent effacement means the cervix is a normal, pre-labor length. Fifty percent effaced means the cervix is at half of the expected length. If the cervix is 100% effaced, it is paper thin.
- Cervical consistency: Cervical consistency of the cervix refers to the feel of the cervix on the exam. A firm cervix has a consistency similar to the tip of the nose, while a soft cervix has a consistency similar to the lips of the oral cavity.
- Cervical position: Cervical position refers to the position of the cervix relative to the fetal head and maternal pelvis.
- Fetal station: Fetal station is the position of the fetal head relative to the ischial spines of the maternal pelvis. The ischial spines are halfway between the pelvic inlet and outlet. At zero station, the fetal head is at the level of the ischial spines. Above and below this level are divided into thirds, by which station is denoted with negative numbers above and positive numbers below the zero station. As a fetal head makes its descent, the station changes from -3, -2, -1, 0, +1, +2, +3. In 1989, the American College of Obstetrics and Gynecology redefined fetal station from -5 to +5, using centimeters instead of thirds as a measurement from the ischial spines. The Bishop score, however, uses the -3 to +3 system.
Each components is given a Bishop score of 0-2 or 0-3. The highest possible total Bishop score is 13. A Bishop score of 5 or more is considered significant for cervical ripening and favorable for induction of labor, while a score of 9 or greater suggests ripening is completed.
Table 1. Bishop score for induction of labor
| Parameter\Score | 0 | 1 | 2 | 3 |
|---|---|---|---|---|
| Position of cervix | Posterior | Mid position | Anterior | – |
| Cervical Consistency | Firm | Medium | Soft | – |
| Cervical Effacement (%) | 0-30% | 40-50% | 60-70% | 80% |
| Cervical Dilation (cm) | Closed | 1-2 cm | 3-4 cm | 5-6 cm |
| Fetal station (-3 to +3) | -3 | -2 | -1, 0 | +1, +2 |
Bishop score interpretation
A Bishop score of 8 or greater is considered to be favorable for induction, or the chance of a vaginal delivery with induction is similar to spontaneous labor. A score of 6 or less is considered to be unfavorable if an induction is indicated cervical ripening agents may be utilized.
The most common modification to the Bishop score is a simplified scoring system that just takes into account dilation, effacement, and station (each scored 0 to 3 points). In this shortened modification, a score of more than 5 is considered favorable.
While, originally, the Bishop score was designed for multiparous patients, it applies to nulliparous patients undergoing induction as well. Increasing maternal parity is a strong indicator of the likelihood of successful vaginal delivery and a predictor of shorter length of labor. Fetal size, gestational age, maternal age, provider patience, and decision to induce versus expectantly manage can be correlated to differing success rates. Maternal body mass index can play a role as well, with the increased length of labor and cesarean delivery rates. The Bishop score is still widely in use to determine whether or not a cervix is “favorable” and to assess whether or not cervical ripening is needed. While Bishop score has been found to be useful for predicting vaginal delivery with sensitivity around 75% (similar between the full and modified scores) as well as a positive predictive value 83% to 84%, it has poor specificity and negative predictive value.
If a cervix is favorable, induction of labor is likely to result in vaginal delivery, and any method of induction tends to work well. In the scenario of a favorable cervix, labor induction is normally undertaken with oxytocin and/or amniotomy.
If a cervix is considered to be unfavorable, no method is highly effective for induction so that patient is a candidate for cervical ripening. Cervical ripening is a process that helps prepare the cervix for labor and can result in a more favorable cervix. There are two main types of cervical ripening, prostaglandin use and mechanical methods. Prostaglandins are a medication that can be given vaginally, buccally, or orally to a patient with an unscarred uterus that can help the cervix progress to a more favorable Bishop score in 12 to 24 hours. Mechanical methods such as a balloon catheter and hygroscopic dilators can be used as well. Mechanical methods, such as a balloon catheter, have shown to have similar outcomes to prostaglandins. Mechanical methods can be used in conjunction with prostaglandins in certain clinical scenarios.
A recent study examining over 5,600 nulliparous women undergoing induction of labor found that a simplified Bishop score, including only cervical dilation, effacement, and station, was equally as predictive as the traditional Bishop score in predicting vaginal delivery 6.
Emerging evidence suggests that ultrasound assessment of the cervix helps distinguish patients at increased risk of preterm labor. In an meta analysis, Crane and Hutchens evaluated more than 300 studies, including 14 articles involving more than 2200 women in their final analysis. They found that ultrasound is a strong predictor of preterm birth among asymptomatic women at less than 35 weeks’ gestation 7.
Detection of fetal fibronectin in cervicovaginal secretions has also been used. Fetal fibronectin is a glycoprotein found in amniotic fluid and at the chorionic decidual interface. The absence of this protein in cervicovaginal secretions predicts prolongation of pregnancy. Fetal fibronectin is also predictive of response to prostaglandin application to the cervix at term in order to induce cervical ripening and labor. Currently, evaluation of fetal fibronectin is used predominantly in the assessment and triage of patients for preterm labor.
Modified Bishop score
According to the Modified Bishop’s pre-induction cervical scoring system, cervical effacement has been replaced by cervical length in cm, with scores as follows: 0 for >4 cm, 1 for 2-4 cm, 2 for 1-2 cm, 3 for <1 cm 8. Cervical length may be easier and more accurate to measure and have less inter-examiner variability.
Another modification for the Bishop’s score is the modifiers. Points are added or subtracted according to special circumstances as follows:
One point is added to the total score for:
- Existence of pre-eclampsia
- Each previous vaginal delivery
One point is subtracted from the total score for:
- Postdate/post-term pregnancy
- Nulliparity (no previous vaginal deliveries)
- PPROM; preterm premature (prelabor) rupture of membranes
Table 2. Modified Bishop cervical score system
| Characteristic | 0 | 1 | 2 | 3 |
|---|---|---|---|---|
| Position of cervix | Posterior | Middle or anterior position | – | – |
| Cervical Consistency | Firm | Medium | Soft | – |
| Cervical Length (cm) | >4 cm | 2-4 cm | 1-2 cm | <1 cm |
| Cervical Dilation (cm) | Closed | 1-2 cm | 3-4 cm | >4 cm |
| Fetal station (-3 to +3) | -3 | -2 | -1, 0 | +1, +2 |
Women with a cervical score ≥ 5 generally labor more easily than those with a cervical score < 5
- Women with a low cervical score (nulliparous and parous) experience higher rates of unsuccessful induction and cesarean section 9.
- Randomized trials comparing induction of labor to waiting have shown that, for a number of indications e.g. maternal diabetes at 38+0 weeks, term PROM and gestation > 41+0 weeks
- Induction of labor increases the number of epidural and operative vaginal deliveries
- There is no increase in caesarean section rate 10
- A policy of labor induction at 41+0 weeks or later compared to awaiting spontaneous labor either indefinitely or at least one week is associated with fewer perinatal deaths 11
- Studies on breast (nipple) stimulation are too small to evaluate the efficacy and safety of this practice. The medical expert consensus is that breast stimulation should not be recommended as a means of stimulating cervical ripening or inducing labor in high risk pregnancies 12.
- Bishop EH. 1964. Pelvic scoring for elective induction. Obstetrics and Gynecology 24:266.[↩][↩]
- Wormer KC, Williford AE. Bishop Score. [Updated 2019 Jan 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470368[↩][↩][↩][↩]
- National Institute for Health and Clinical Excellence (NICE). Induction of labour. National Collaborating Centre for Women’s and Children’sHealth. Commissioned by the National Institutefor Health and Clinical Excellence. London: RCOG Press;2008. https://www.nice.org.uk/guidance/CG70[↩]
- Maul H, Mackay L, Garfield RE. Cervical ripening: Biochemical, molecular, and clinical considerations. Clin Obstet and Gynecol 2006; 49: 551-63[↩]
- Pez V, Deruelle P, Kyheng M, Boyon C, Clouqueur E, Garabedian C. [Cervical ripening and labor induction: Evaluation of single balloon catheter compared to double balloon catheter and dinoprostone insert]. Gynecol Obstet Fertil Senol. 2018 Jul – Aug;46(7-8):570-574.[↩]
- Laughon SK, Zhang J, Troendle J, Sun L, Reddy UM. Using a simplified Bishop score to predict vaginal delivery. Obstet Gynecol. 2011 Apr. 117(4):805-11.[↩]
- Crane JM, Hutchens D. Transvaginal sonographic measurement of cervical length to predict preterm birth in asymptomatic women at increased risk: a systematic review. Ultrasound Obstet Gynecol. 2008 May. 31(5):579-87.[↩]
- Dutta DC. Text Book of Obstetrics. 6ed. New Central Book Agency. 2001. ISBN 978-81-7381-142-5[↩]
- Enkin M, Keirse MJNC, Neilson J, Crowther C, Duley L, Hodnett E, et al. A guide to effective care in pregnancy and childbirth, 3rded. Oxford: Oxford University Press; 2000[↩]
- Royal College of Obstetricians and Gynaecologists (RCOG). Induction of labour, Evidence-based Clinical Guideline Number 9. RCOG Clinical Effectiveness Support Unit, London: RCOG Press; 2001.[↩]
- Mandruzzato G, Alfirevic Z, Chervenak F, Gruenebaum A, Heimstad R, Heinonen S, Levene M, Salvesen K, Saugstad O, Skupski D, Thilaganathan B. Guidelines for the management of postterm pregnancy. J Perinat Med2010; 38: 111-9[↩]
- Kavanagh, J. , Kell, A. and Thomas, J. (2005), Breast Stimulation for Cervical Ripening and Induction of Labour. Birth, 32: 323-324. doi:10.1111/j.0730-7659.2005.00391.x[↩]