What is bowenoid papulosis
Bowenoid papulosis is an uncommon sexually transmitted pre-cancerous skin condition that occurs at both sexes, which is a rare form of intraepithelial neoplasia 1. Bowenoid papulosis presents as single or multiple small, red, brown or flesh-colored spots or patches on the genitals of males and females. In females it is one type of “vulvar intraepithelial neoplasia” (VIN) and in males it is a type of penile intraepithelial neoplasia (PIN) 2. Bowenoid papulosis tends to affect young sexually active people. Sexually active people may be at risk of getting bowenoid papulosis. As in genital warts, human papillomavirus (HPV) transmission is most often passed through direct skin-to-skin sexual contact. Partners of patients with bowenoid papulosis should be screened for other forms of intraepithelial neoplasia (cervical, penile, vulvar and anal). Men and women are equally at risk and the peak incidence is in sexually active persons in their third to the mid-fifth decade with a mean age of 31 years 3. However, bowenoid papulosis can appear at any age and ranges from 3 to 80 years. Both sexes are affected, although recent data showed an increased number in women. There are an estimated 5 cases per 100,000 women 4. The exact prevalence is unknown because bowenoid papulosis lesions are related clinically to genital warts. There is no racial predilection for bowenoid papulosis.
Bowenoid papulosis is clinically characterized by multiple well-demarcated red-brown to violaceous papules, usually less than 1 cm in size. The surface of the lesion can be flat, smooth, papillomatous or verrucous. Some papules may coalesce into large plaques. Sometimes, bowenoid papulosis presents as warty white plaques. The distribution of lesions is commonly discrete; sometimes bowenoid papulosis can have an annular or linear exhibition. In men, bowenoid papulosis lesions primarily involve the penile shaft, but may also involve foreskin, glans, scrotum as well as the anus. Whereas in women, the lesions are usually bilateral and affect labia major, labia minor, clitoris, inside the vagina, inguinal folds, and perianal area. The lesions are generally darker in women than in men. They are usually asymptomatic; occasionally, patients may complain from pruritus and soreness of the affected area. Extragenital bowenoid papulosis is a very rare condition, and it may involve the face, fingers or neck, with or without concomitant genital lesions 5.
The classification of bowenoid papulosis was confusing and including three clinical entities: bowenoid papulosis, Bowen’s disease, and erythroplasia of Queyrat. Now it is recommended that these three entities not be used to describe lesions in the anogenital area 6. But, dermatologists still recognize bowenoid papulosis as a distinct clinical variant. In fact, bowenoid papulosis is induced virally by human papillomavirus (HPV) and presents as solitary or multiple skin-colored papules in the anogenital area. Human papillomavirus (HPV), the cause of genital warts and some genital cancers, has been closely linked to bowenoid papulosis. Although most cases of bowenoid papulosis are benign (harmless) a small percentage may transform into invasive squamous cell carcinoma (penile or vulvar cancer).
Bowenoid papulosis can last from two weeks to several years. Bowenoid papulosis lesions are generally considered benign with a spontaneous regress leaving no sequelae in immunocompetent persons, although a small number may transform into invasive squamous cell carcinoma. Clinically bowenoid papulosis is assimilated to genital warts while histologically it has a close resemblance to squamous cell carcinoma in situ (Bowen’s disease). Treatment is generally conservative.
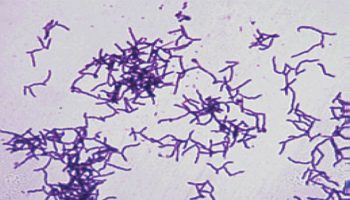
Figure 1. Bowenoid papulosis in females
[Source 7 ]Bowenoid papulosis causes
Bowenoid papulosis is a sexually transmitted condition associated with HPV infection. Most lesions are associated with oncogenic HPV types mainly the HPV 16 genotype but occasionally HPV 18, 31, 33, 34, 35, 39, 42, 48, 51, 52, 53 and 54 are detected 6. Bowenoid papulosis may also occur in immunocompromised individuals such as in organ transplant recipients. Smoking has recognition as a recurrence factor.
Bowenoid papulosis pathophysiology
Detection of papillomavirus common antigen in cases of bowenoid papulosis supports the hypothesis that bowenoid papulosis results from HPV. In fact, E6 and E7 viral oncoproteins of oncogenic HPV types contribute to oncogenesis by inducing over-expression of p16 protein and human telomerase reverse transcription (hTERT).
Bowenoid papulosis histopathology
Histologically, bowenoid papulosis is characterized by acanthosis with full thickness epidermal atypia, known as Bowenoid dysplasia. Multiple metaphase mitoses are usually visible above the basal layer as well as scattered dyskeratotic and multinucleated keratinocytes with pleiomorphism. Histopathologic findings may also show parakeratosis and hypergranulosis. The integrity of the basement membrane is preserved. The dermis contains superficial infiltrate of lymphocytes with perivascular accentuation. Induction of the focal epidermal hyperplasia and dysplasia is viral. Moreover, immunohistochemistry for p16 protein reveals strong in bowenoid papulosis. Staining with an antibody to p16 protein has high specificity and sensitivity to detect this disease.
Bowenoid papulosis signs and symptoms
Bowenoid papulosis may look like small red, brown or flesh-colored flat or warty lesions appear most commonly on the shaft of the penis or labia of females. Bowenoid papulosis may also be present on other parts of the genitals as well as in and around the anus. Bowenoid papulosis is usually symptomless but occasionally lesions may become inflamed, itchy and painful. The diagnosis is usually made by skin biopsy.
Bowenoid papulosis tends to spontaneously disappear within several months and if a young woman is pregnant when it is diagnosed it will often disappear after delivery. If it is persistent this is an indication for active treatment because of the chance of developing skin cancer.
Once infected with HPV you may become a lifelong carrier of the virus and recurrence of bowenoid papulosis or other intraepithelial cancers in the genital area is possible.
Bowenoid papulosis complications
Transformation into invasive squamous cell carcinoma is rare and occurs in less than 1 % of cases, especially in immunocompromised individuals. Females with BP lesions and sexual partners of male patients are at high risk of cervical or vulvar carcinomas because of the infection with a potentially oncogenic HPV.
Bowenoid papulosis diagnosis
Bowenoid papulosis may be diagnosed by its typical clinical appearance, especially with the aid of dermoscopy, or by skin biopsy. Squamous cell carcinoma in situ pathology is diagnostic on skin biopsy.
HPV subtyping may also be a recommended next step. Microscopic findings show typical a feature of Bowen’s disease with only a few differentiating features. The distinction rests in the circumscribed plaque-like pattern, the multiplicity of lesions, the age of the patient, and less dyskeratosis and atypia and more dilated vessels in the dermis in pathology 5. Hence the diagnosis of bowenoid papulosis is based on clinical grounds and histopathological correlation. Furthermore, a skin biopsy is recommended in case of recalcitrant lesions to standards therapies to rule out malignancy.
An extensional assessment of HPV infection is mandatory, including examination of the oral, genital, and anal area. Besides, anoscopy should be performed in the case of receptive anal sex. All this must be performed for the patient as well as the partner.
Bowenoid papulosis treatment
Because bowenoid papulosis usually runs a benign course with many cases spontaneously regressing, treatment is often unnecessary. Without treatment, bowenoid papulosis lesions may regress in an average of 8 months. Lesions should be re-examined every 3 to 6 months so that any changes may be picked up early.
If the lesions are persistent, treatment of bowenoid papulosis is the same as for genital warts. Treatment modalities include locally ablative or destructive therapies such as carbon dioxide (CO2) laser vaporization, cryotherapy, electrocoagulation, 5-aminolevulinic acid-mediated photodynamic therapy (ALA-PDT), excisional surgery, and 5 fluorouracil (5FU). Moreover, topical imiquimod cream 5% once a day on an alternate day for one month has proven good results on limited lesions of bowenoid papulosis with viral clearance in some cases. However, relapse often occurs with all treatment modalities 4.
Furthermore, there are prophylactic vaccines to prevent infection with oncologic HPV subtypes. Moreover, prevention from recurrence correlates with cessation of cigarette smoking.
Regular checks are necessary after treatment to ensure the condition has completely resolved.
Bowenoid papulosis prognosis
Bowenoid papulosis has a variable course. Lesions may regress spontaneously or persist for several years with older persons or immunocompromised patients. It may rarely transform into Bowen’s disease or invasive squamous cell carcinoma 8.
- Chamli A, Zaouak A. Bowenoid Papulosis. [Updated 2019 Apr 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539887[↩]
- McCalmont TH. Whither bowenoid papulosis? J. Cutan. Pathol. 2013 Feb;40(2):209-10.[↩]
- Chamli A, Zaouak A. Bowenoid Papulosis. [Updated 2019 Apr 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539887 [↩]
- Wang XL, Wang HW, Guo MX, Huang Z. Combination of immunotherapy and photodynamic therapy in the treatment of Bowenoid papulosis. Photodiagnosis Photodyn Ther. 2007 Jun;4(2):88-93.[↩][↩]
- Hoverson AR, Lundell RB, Cooper VL, Bridges AG. Oral bowenoid papulosis. Cutis. 2018 Nov;102(5):E27-E29.[↩][↩]
- Deen K, Burdon-Jones D. Imiquimod in the treatment of penile intraepithelial neoplasia: An update. Australas. J. Dermatol. 2017 May;58(2):86-92.[↩][↩]
- Penis and scrotum dysplasia / carcinoma in situ. http://www.pathologyoutlines.com/topic/penscrotumbowenoid.html[↩]
- Takayama A, Ishiguro N, Kawashima M. Coexistence of Bowenoid papulosis and Bowen’s disease in a patient with systemic lupus erythematosus. J. Dermatol. 2012 Jul;39(7):646-9.[↩]