Caustic ingestion
A wide variety of chemical agents including mineral and organic acids and alkalis, oxidizing agents, denaturants, hydrocarbons and other chemicals may cause corrosive injuries 1. Accidental or intentional ingestion of corrosive substances cause life-threatening injuries to the entire gastrointestinal tract, but most significantly the upper digestive tract, including the oropharyngeal cavity, larynx, esophagus, and stomach. The degree of injury is determined by the nature of the substance (the degree to which it could cause corrosion), the amount consumed or its concentration and state (solid or liquid), and the time of contact with the gastrointestinal mucosa 2. The large majority of caustic agents are liquids. Strong acids and alkali are readily available as household cleaners. Lye is a generic term for the alkali used to make soap, either potassium hydroxide or sodium hydroxide. Acids cause coagulation necrosis, whereas alkali combine with tissue proteins and cause liquefaction necrosis which penetrates deep into tissues. Concentrated alkali ingestion may lead to more serious injury and complications by penetrating tissues and leading to full-thickness damage of the esophageal/gastric wall. Liquid household bleach, although often reported, does rarely cause severe injuries.
Caustic material ingestion injuries are uncommon. Only 5,000 cases are reported in the United States each year and most acute care healthcare facilities admit only a few cases annually 3. The majority (80 %) of cases worldwide involve children as a result of unintentional, accidental ingestion of caustic substances 4. The remainder of cases reported are adults with psychiatric disturbances, some after suicide attempts, or alcoholics 5.
More severe injuries to the esophagus and stomach occur if large quantities of substances are ingested, particularly in persons who attempt suicide 6. However, worldwide estimates report that about 80% of cases occur in children younger than 5 years 4. Also, many of the reported patients who ingested caustic substances have accompanying psychiatric disorders including depression, schizophrenia, adjustment problems, and personality disorders 7. Adult exposures have increased morbidity than childhood exposures because of the often higher volume of the exposure and the presence of possible co-ingestants. Occupational exposures often are more severe than other exposures because industrial products are more concentrated than those found in the home 8.
The alkali drain cleaners and acidic toilet bowl cleaners are responsible for the most fatalities from corrosive agents. In adults, 10% of caustic ingestions result in death 9.
Approximately 10% of caustic ingestions result in severe injury requiring treatment. Approximately 1-2% of caustic ingestions result in stricture formation 9.
Common acid-containing sources include the following:
- Toilet bowl–cleaning products
- Automotive battery liquid
- Rust-removal products
- Metal-cleaning products
- Cement-cleaning products
- Drain-cleaning products
- Soldering flux containing zinc chloride
Common alkaline-containing sources include the following:
- Drain-cleaning products
- Ammonia-containing products
- Oven-cleaning products
- Swimming pool–cleaning products
- Automatic dishwasher detergent
- Hair relaxers
- Clinitest tablets
- Bleaches
- Cement
Corrosive esophageal injury or caustic esophagitis usually occurs from accidental or suicidal ingestion of caustic substances (e.g. lye, household cleaners, bleaches, washing soda), and is harmful to the esophagus due to their alkali medium. The stomach is not affected as the gastric acid can neutralize these substances, however, in cases of acidic corrosives, the esophagus can be spared while the stomach is severely injured. The esophageal damage depends on the concentration, type, and quantity of ingestion of the harmful material and the time of contact between it and the esophagus. It usually affects the middle and lower third of the esophagus.
Caustic ingestion can result in a number of injuries ranging in severity from mild oral burns to minimal mucosal erythema or transmural necrosis of the esophagus and stomach with visceral perforation. Emergency surgery is indicated for hemorrhage, free perforation, mediastinitis or peritonitis. Full thickness esophagogastric necrosis is a severe form of injury associated with considerable morbidity and mortality. It may occur due to ingestion of a large amount or highly concentrated corrosive substance. The injury may extend and involve adjacent viscera such as the duodenum, small intestine, colon, pancreas, and gallbladder. Complications such as hemorrhage, perforation, aorto-enteric fistula, or gastro-colic fistula may occur in patients surviving the initial event during the first 2–3 weeks after ingestion. Patients who have survived severe caustic injury of the foregut are at high risk of luminal strictures. After recovery from the initial injury, collagen deposition and fibrosis continue for months and scar retraction results in esophageal shortening and stricture. The incidence of esophageal stricture following grade 2B and grade 3 esophageal burns is in the range of 50–80 % 10. Concomitant gastric outlet obstruction occurs in up to 30 % of patients with esophageal stricture 11. In the long term, development of pharyngeal, esophageal, or gastric strictures may compromise nutritional outcome. Interestingly, the risk of squamous-cell cancer of the damaged esophagus is estimated to be 1000 times higher than that of the general population, and the latent period for the malignant change is 15–40 years 12.
Currently, in most referral centers therapeutic algorithms for the management of patients with caustic injuries rely on the findings of upper digestive endoscopy. Despite the use of different endoscopic classification systems, therapeutic approaches are similar and include conservative management of patients with mild injuries, while patients with severe injuries undergo emergency surgical exploration.
Airway obstruction may occur secondary to edema, bleeding, and the presence of necrotic material. Because this can develop rapidly, airway protection is paramount following caustic ingestions. Delays in securing a definitive airway can result in increased difficulty due to progressive airway edema.
Esophageal gastric, bowel, airway, or vascular perforation may occur.
Fluid losses from vomiting, third spacing, and gastrointestinal bleeding may lead to hypovolemia and shock. This is particularly true after ingestion of metallic chlorides.
After significant acidic ingestions, the patient may develop metabolic acidosis, hemolysis, and multiorgan failure including acute renal failure.
Hypocalcemia develops precipitously after ingestion of significant amounts of hydrogen fluoride.
Although there are studies describing the short and long-term outcomes of reconstruction for established caustic strictures of the esophagus, there is limited literature on the early and long term outcomes of patients managed in an emergency setting for corrosive induced acute esophagogastric and/or adjacent organ necrosis.
In patients who survive the initial phases of injury, late-developing problems include the following:
- Strictures
- Fistula
- Hypomotility disorders
- Increased risk of gastrointestinal cancers
Caustic substance ingestion
The severity of tissue injury from acidic and alkaline substances is determined by the duration of contact; the amount and state (liquid, solid) of the substance involved; and the substance’s physical properties, such as its pH, concentration, ability to penetrate tissue, and its titratable reserve. The latter reflects the amount of tissue required to neutralize a given amount of the involved substance and is particularly useful for measuring the amount of damage that can be caused by caustics, such as phenol, which have a near-neutral pH.
The pH of a chemical is a measure of how easily the chemical accepts or donates a proton. This relates to the strength of the acidic or alkaline substance, and provides some, but not precise, correlation with the likelihood of injury. Substances with a pH less than 2 are considered to be strong acids; those with a pH greater than 12 are considered to be strong bases.
In pediatric patients younger than 5 years, consuming caustic substances occurs accidentally; however, in teens and adults, it is mostly intentional with the goal of committing suicide 6. Although many kinds of substances cause caustic injury 13, the most common agent is a strong alkaline substance such as sodium hydroxide (NaOH) or potassium hydroxide (KOH), which usually includes disinfectants used in the home or laundry facilities, and discoid batteries 14. The term “lye” refers to the liquid obtained from the leaching of ashes, including sodium hydroxide (NaOH) or potassium hydroxide (KOH). Highly acidic substances, such as hydrochloric acid, sulfuric acid, and phosphoric acid, are used frequently to remove rust in bathrooms or swimming pools and may be included in car batteries. These acidic materials are used less frequently than alkaline substances as a tool for suicide because they can induce severe pain 15.
A solution of 5% sodium hypochlorite, which is used as bleach, is commonly known as “Rox.” This agent is frequently reported to be ingested, but it rarely injures the esophagus or stomach 16. Button-type batteries contain highly alkaline substances, and if swallowed, serious tissue injury secondary to local current or pressure necrosis may occur. When these batteries are trapped in the esophagus, burns may occur within 4 hours and perforation may occur within 6 hours 14. Therefore, in those cases, the batteries should be removed through emergent endoscopy.
Alkaline ingestions
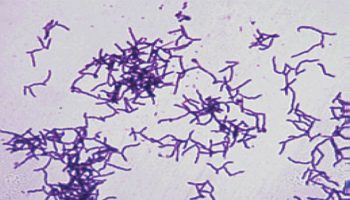
Alkaline ingestions cause tissue injury by liquefactive necrosis, a process that involves saponification of fats and solubilization of proteins. Cell death occurs from emulsification and disruption of cellular membranes. The hydroxide ion of the alkaline agent reacts with tissue collagen and causes it to swell and shorten. Small vessel thrombosis and heat production occurs.
Severe injury occurs rapidly after alkaline ingestion, within minutes of contact. The most severely injured tissues are those that first contact the alkali, which is the squamous epithelial cells of the oropharynx, hypopharynx, and esophagus. The esophagus is the most commonly involved organ with the stomach much less frequently involved after alkaline ingestions. Tissue edema occurs immediately, may persist for 48 hours, and may eventually progress sufficiently to create airway obstruction. Over time, if the injury was severe enough, granulation tissue starts to replace necrotic tissue.
Over the next 2-4 weeks, any scar tissue formed initially remodels and may thicken and contract enough to form strictures. The likelihood of stricture formation primarily depends upon burn depth. Superficial burns result in strictures in fewer than 1% of cases, whereas full-thickness burns result in strictures in nearly 100% of cases. The most severe burns also may be associated with esophageal perforation.
Acid ingestions
Acid ingestions cause tissue injury by coagulation necrosis, which causes desiccation or denaturation of superficial tissue proteins, often resulting in the formation of an eschar or coagulum. This eschar may protect the underlying tissue from further damage. Unlike alkali ingestions, the stomach is the most commonly involved organ following an acid ingestion. This may due to some natural protection of the esophageal squamous epithelium. Small bowel exposure also occurs in about 20% of cases. Emesis may be induced by pyloric and antral spasm.
The eschar sloughs in 3-4 days and granulation tissue fills the defect. Perforation may occur at this time. A gastric outlet obstruction may develop as the scar tissue contracts over a 2- to 4-week period. Acute complications include gastric and intestinal perforation and upper gastrointestinal hemorrhage.
Significant exposures may also result in gastrointestinal absorption of the acidic substances leading to significant metabolic acidosis, hemolysis, acute renal failure, and death.
Corrosive esophageal injury pathophysiology
Ingestion of alkaline substances is known to mainly injure the esophagus rather than the stomach or duodenum, whereas acidic materials injure mainly the stomach rather than the esophagus 17. However, recent reports indicating that extensive esophageal injury or even perforation is not uncommon after ingestion of acids are putting this traditional notion into question 18. In addition, both acidic and alkaline substances can injure the larynx, trachea, and bronchi 14.
Ingestion of alkaline substances leads to liquefaction necrosis due to bonding with tissue protein 14. Therefore, it causes rapid injuries outside the esophagus toward the mediastinal wall. These responses continue until the alkaline substance is neutralized by the tissue fluids. In addition, alkaline fluid has a stronger surface tension and stays in the tissue for a longer period, thereby worsening the injury. Within the stomach, injuries are limited by the partially neutralizing mechanism of gastric acid 19. In the case of extensive injury to the intestinal wall, complications such as perforation, mediastinitis, and peritonitis may occur and result in death. Liquid materials, rather than solid batteries, result in more extensive injuries 14. Liquefaction necrosis occurs for 3 to 4 days and causes intravascular thrombus and mucosal inflammation, in addition to causing local or extensive putrefaction and ulceration. Over a period of 2 weeks, the esophageal wall is thinned with tissue putrefaction, granulation, and fibrosis; the process of reepithelialization takes 1 to 3 months. Therefore, endoscopic procedures should be avoided from 5 to 15 days after the ingestion of alkaline substances 20. Stricture formation, as a chronic complication, is ultimately affected by the depth of the esophageal injury and the degree of collagen accumulation. Therefore, the subsequent possibility of chronic complications or death increases in second- or third-degree injuries 19.
Ingestion of acids usually causes superficial coagulation necrosis, in which formation of thrombi within the vessels and bundling of connective tissue lead to the formation of scar tissue. Therefore, very deep injuries that extend through all layers of the gastrointestinal wall do not commonly develop after the ingestion of acidic substances 21.
Upon swallowing, acids cause severe oropharyngeal pain; thus, they are usually consumed in small volumes compared with the alkaline substances. Acidic substances have less surface tension; therefore, they pass rapidly through the esophagus, resulting in a less frequency and a lower degree of esophageal injuries 14. The ingested acidic substance flows rapidly to the pylorus through the lesser curvature of the stomach, causing widespread injury in the antrum 2. If there is some amount of food inside the stomach, injury can be prevented because of a neutralization effect. Despite this, if large quantities are consumed, esophageal or gastric perforation may occur.
Although, as stated above, caustic injury caused by alkaline substances is more severe, a comparative study revealed that the prognosis was less favorable for those who swallowed a strong acid 22. In this study 22, the acid ingestion group showed a high frequency of severe complications such as perforation or death, a high degree of mucosal injury, and a high frequency of intensive care unit (ICU) admission. This is thought to be because the prognosis of caustic injury is influenced by the quantity ingested and the types of complication after ingestion rather than by the type of the ingested substance (acid or alkaline).
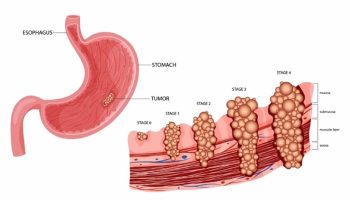
Corrosive esophageal injury grading
The degree of injury from caustic substances can be categorized similarly to that of skin burns 20.
- First-degree injuries are confined to the mucosal surface, and can show diffuse or localized erythema, edema, and bleeding. Scar formation does not ultimately occur.
- Second-degree injuries involve the mucosa and submucosa. Endoscopic examination can show various findings such as exudates or blister formation. Ultimately, scar changes can develop through the formation of granulation and fibrosis.
- Third-degree injuries include the entire wall layer, and are characterized by deep penetrating ulcers, black discoloration, or perforation of the intestinal wall.
To predict the treatment outcome and prognosis of patients with caustic injuries, endoscopic categorization of 81 patients was performed, and the subsequent categorization is widely used 20:
- Grade 0 indicates a normal mucosa;
- Grade 1 indicates only slight swelling and redness of the mucosa;
- Grade 2A indicates the presence of superficial ulcers, bleeding, and exudates;
- Grade 2B indicates local or encircling deep ulceration;
- Grade 3A indicates focal necrosis;
- Grade 3B indicates extensive necrosis.
Although further studies are needed to evaluate the validity of this endoscopic categorization, most patients with grade 1 or 2A injuries have good prognoses without sudden deaths, and they do not develop outlet obstruction or stricture of the esophagus. Approximately 70% to 100% of patients with grade 2B and 3A injuries develop stricture. For patients with grade 3B injuries, a mortality of 65% has been reported, and in the majority of cases, esophagectomy and colonic or jejunal replacement surgeries are required. However, several reports have indicated that 12% of gastrectomies and 15% of esophagectomies are unnecessary; therefore, a more accurate standard is required 23.
Caustic ingestion signs and symptoms
The clinical presentations of caustic injuries are very diverse, and initial symptoms do not show deep correlations with the ultimate degree of the injury 24. Crystal or other solid materials easily adhere to the oral mucosa; therefore, they cause more severe injuries to the pharynx and upper airway rather than to the esophagus or stomach. In contrast, liquids can easily pass through the esophagus and stomach; therefore, they can cause extensive injury. The degree of injury is proportional to the mortality. Furthermore, the morbidity of chronic complication is also related to the degree of injury 25. Depending on the injured area, pain may arise in the oropharynx, retrosternum, or epigastrium. Dysphagia, odynophagia, and excessive salivation may also occur. Continuous severe retrosternal or back pain may indicate esophageal perforation or mediastinitis. Perforation may occur up to 2 weeks after ingestion; therefore, strict monitoring is essential 4. In addition, depending on the extent of injury, vomiting, hematemesis, abdominal tenderness, and rebound tenderness may suddenly occur. Although rare, vocal hoarseness, wheezing, and shortness of breath may also occur upon injury to the larynx and epiglottis. Fever, palpitations, and shock indicate extensive damages.
Caustic ingestion diagnosis
Medical history
The physician should try to identify the specific agent ingested, as well as the concentration, pH, and amount of substance ingested. The time, nature of exposure, duration of contact, and any immediate on-scene treatment are important in determining management of toxicity.
The presence or absence of the following symptoms should be determined since the presence of any of these symptoms suggests the possibility of significant internal injury (although their absence does not preclude significant injury):
- Dyspnea (shortness of breath)
- Dysphagia (difficulty swallowing)
- Oral pain and odynophagia (painful swallowing)
- Chest pain
- Abdominal pain
- Nausea and vomiting
Rapidly obtaining reliable information on the particular agent involved is vital. This is particularly true of uncommon caustic agents, some of which have important toxic concerns beyond those of a simple caustic ingestion.
A good example of this is the potential for abrupt, life-threatening hypocalcemia following ingestion of hydrogen fluoride, even in a relatively dilute form such as that found in some rust removers. Case reports of patients surviving such suicidal ingestions underline the value of being able to anticipate and aggressively manage the systemic hypocalcemia, which is unique to hydrogen fluoride, with intravenous calcium. Other examples of caustic agents with unique toxicities include phenol, zinc chloride, and mercuric chloride, all of which can cause significant systemic toxicity and which may require significant changes in management.
Material Safety Data Sheets (MSDS), online databases, and consultations with the local poison center are all ways for a clinician to rapidly familiarize themselves with unfamiliar caustic agents.
Physical examination
As with the history, physical examination findings may be deceptively unremarkable after a significant caustic ingestion, despite the presence of significant tissue necrosis 26.
Signs of impending airway obstruction may include the following:
- Stridor
- Hoarseness
- Dysphonia or aphonia
- Respiratory distress, tachypnea, hyperpnea
- Cough
Other signs of injury may include the following:
- Tachycardia
- Oropharyngeal burns – These are important when identified; however, significant esophageal involvement may occur in the absence of oropharyngeal lesions
- Drooling
- Subcutaneous air
- Acute peritonitis – Abdominal guarding, rebound tenderness, and diminished bowel sounds
- Hematemesis
Indications of severe injury include the following:
- Altered mental status
- Peritoneal signs
- Evidence of viscous perforation
- Stridor
- Hypotension
- Shock
Laboratory tests
Laboratory studies may include the following:
- Laboratory tests should include white blood cell (WBC), hemoglobin, platelet count, C-reactive protein (CRP), pH, and serum levels of Na, K, Cl, Ca, Mg, urea, creatinin, LDH, CPK, AST, ALT, lactates, alcohol. β-HCG levels should be measured in young women.
- pH testing of product: A pH less than 2 or greater than 12.5 indicates greater potential for severe tissue damage 27, but a pH outside of this range does not preclude significant injury
- pH testing of saliva: Unexpected high or low values may confirm ingestion in questionable cases; however, a neutral pH cannot rule out a caustic ingestion
- Complete blood count (CBC) and electrolyte, blood urea nitrogen (BUN), creatinine, and arterial blood gas (ABG) levels may all be helpful as baseline values and as indications of systemic toxicity
- Liver function tests and a disseminated intravascular coagulation (DIC) panel may also be helpful to establish baselines or, if abnormal, confirm severe injury following acid ingestions
- Urinalysis and urine output may help guide fluid replacement
- Blood type and crossmatch are indicated for any potential surgical candidates or those with the potential for gastrointestinal bleeding
- Obtain aspirin and acetaminophen levels as well as an electrocardiogram (ECG) in any patient whose intent may have been suicidal.
- In cases of hydrofluoric acid ingestion, precipitous falls in calcium level may lead to sudden cardiac arrest. Although ionized calcium levels are likely to have too long a turnaround to be clinically useful, cardiac monitoring and serial ECGs may help anticipate this event
Although the results of laboratory tests are not well correlated with the degree of injury, a study suggests that white blood cell counts >20,000 cells/mm³, increase in the C-reactive protein (CRP) level, old age, and the presence of esophageal ulcers are predictive factors that are correlated with mortality 28. Some reports state that an arterial pH <7.22 may indicate esophageal injury requiring surgical management 29. Usually, laboratory results contribute toward setting the direction of monitoring and management of the patient, rather than predicting the mortality 30.
Endoscopy
Some reports suggest that nonsymptomatic pediatric patients who have ingested low-potency substances do not require endoscopy. However, for adult patients who have ingested caustic substances with the intent to commit suicide, most of those substances are very potent, and therefore, emergent endoscopy is recommended for all patients 31.
As an intact-looking oral cavity or pharynx cannot be used to exclude the possibility of esophageal or gastric injury, upper gastrointestinal endoscopy should be performed within 24 hours of ingestion of caustic substances; however, several reports indicate that it can be safely done up to 96 hours after ingestion 22. Upper gastrointestinal endoscopy can be used to evaluate esophageal and gastric injuries, as well as to predict prognosis and establish a management plan 32. However, it is contraindicated in several patients, such as hemodynamically unstable patients, those suspected to have a perforation, those in severe respiratory distress, and patients with severe laryngo-pharyngeal edema or necrosis. For patients whose injury is focused around the lips and oral cavity, esophageal or gastric injury usually does not exceed the first-degree grading 33.
Guidelines on pediatric gastrointestinal endoscopy
Guidelines on pediatric gastrointestinal endoscopy from the European Society of Gastrointestinal Endoscopy and European Society for Paediatric Gastroenterology Hepatology and Nutrition include the following suggestions and recommendations for management of corrosive ingestion in pediatric patients 34:
- Suggestion: Every child who has ingested a corrosive substance should have a thorough follow-up, with endoscopy dictated only by symptoms; depending on the symptoms, endoscopy should be performed within 24 hours. (Strong recommendation, high quality evidence.)
- Recommendation: Every child with a suspected caustic ingestion and symptoms or signs (eg, oral lesions, vomiting, drooling, dysphagia, hematemesis, dyspnea, abdominal pain) should undergo esophagogastroduodenoscopy (EGD) to identify all consequent digestive tract lesions. (Strong recommendation, high quality evidence.)
- Suggestion: In cases of suspected corrosive ingestion where the child is asymptomatic (no drooling of saliva/other symptoms, no mouth lesions) and adequate follow-up is assured, esophagogastroduodenoscopy may be withheld. (Weak recommendation, moderate quality evidence.)
- Recommendation: In patients with grade IIb esophagitis after corrosive ingestion, high doses of intravenous dexamethasone (1 g/1.73 m² per day) should be administered for a short period (3 days), to prevent the development of esophageal stricture. No evidence of benefit exists for the use of corticosteroids in other grades of esophagitis (I, IIa, III). (Strong recommendation, moderate quality evidence.)
Endoscopic ultrasound
Miniprobe endoscopic ultrasound (EUS) can be used safely, and compared with conventional endoscopy, no differences have been reported for their use in predicting the development of early complications 35. However, a study had indicated that no strictures form later if the muscle layer is intact in endoscopic ultrasound 36. In addition, several studies with radial EUS indicated that if the proper muscle layer is included, the treatment response to balloon dilatation decreases, and subsequent repeated procedures are required; however, additional studies are needed to investigate the role of endoscopic ultrasound in evaluating caustic esophageal injuries.
Radiologic examinations
A simple chest X-ray may be done to observe if there is a gas shadow in the mediastinum or under the diaphragm, indicating esophageal or gastric perforation, respectively. For confirmation, esophagography or upper gastrointestinal series with a water-soluble contrast medium may be attempted carefully.
The diagnostic efficacy of computed tomography (CT) is slightly higher than endoscopy in terms of assessing the depth and boundary of esophageal or gastric injury, and it is effective in diagnosing impending perforation. In a retrospective analysis of 49 patients who underwent CT, a scoring system for the degree of esophageal causticity and injury of peripheral tissues was attempted, and in terms of predicting the degree of stricture, CT showed better results than endoscopy 37.
Caustic ingestion management
No randomized trial has compared various models for the management of caustic esophageal injury in humans. Instead, most of the currently used management procedures are based on animal experiments.
Management algorithm
Airway monitoring and control is the first priority. Airway protection is critical following caustic ingestion if there is any indication of airway compromise. This can develop rapidly and be complicated by multiple factors.
Large-bore intravenous access allows administration of fluids and medications as needed.
Patients with clinical signs of peritonitis and hemodynamic instability require immediate surgical exploration. Although symptoms such as chest pain, dysphagia, odynophagia, drooling, hemorrhage are usually associated with severe injuries after voluntary ingestion, the absence of oropharyngeal damage does not exclude the possibility of severe esophagogastric injuries 1.
Avoid nasogastric tube positioning as their validity to prevent vomiting and stricture formation has never been proven; nasogastric tubes have been reported to increase risks of gastric perforation, gastroesophageal reflux, and pneumonia 1.
Results of laboratory tests such as white blood cell (WBC), platelet count, CRP, pH, AST, ALT, creatinin, and lactate can help decision making in difficult situations 1.
The efficacy of proton-pump inhibitors and H2 blockers in minimizing esophageal injury by suppressing acid reflux has not been proven 1.
The utility of corticosteroid in terms of stricture prevention is controversial and systematic administration is not recommended. Steroids should be reserved for patients with symptoms involving the airway 1.
Administration of broad-spectrum antibiotics should not be done on a systematic basis. Antibiotics are advised in grade 3 injuries if corticosteroids are initiated or if lung involvement is identified 1.
Endoscopy is the cornerstone of management of caustic injuries. Endoscopy is usually performed 3 to 6 hour after ingestion, and injuries are graded according to the Zargar classification 20. Patients with severe (Grade 3B) esophagogastric injuries are considered for surgery while patients with low grade injuries (≤ Grade 3A) are offered non-operative treatment. Endoscopy grading can also predict the risk to develop an esophageal stricture during follow-up. Inability of endoscopy to predict accurately the depth of intramural necrosis may result in either futile surgery, with negative effects on survival, digestive function and management costs, or in patient death due to inappropriate non operative treatment. Moreover, emergency endoscopy is futile in up to 30 % of patients who do not have injuries of the upper digestive tract following ingestion of bleach or corrosive agents other than strong acids or alkali 1.
Computed tomography helps palliate shortcomings of endoscopy based algorithms. The use of CT is helpful in guiding indications for esophagectomy in patients with grade 3B caustic injury. In a recent study CT did better than endoscopy in selecting patients for surgery or non-operative treatment, suggesting that CT can replace endoscopy in the management of caustic injuries. CT criteria of transmural esophageal necrosis include esophageal-wall blurring and periesophageal-fat blurring on unenhanced images, and absence of post-contrast esophageal-wall enhancement; transmural necrosis of the stomach was defined as the absence of post-contrast gastric-wall enhancement 1.
Pre-hospital management
Establish the diagnosis of caustic agent ingestion. Identify the involved agent. Collect the product on the scene and bring it to the emergency department. If difficult product identification try to evaluate pH (<2; > 10), but be aware that some agents cause a pH-independent corrosive injury 1.
Evaluate the ingestion scenario by:
- a) ascertain ingestion;
- b) determine the accidental or voluntary character;
- c) detect co-ingestion of alcohol and/or drugs;
- d) try to evaluate ingested quantity (in adults assess normal sip (30–50 ml) vs. large gulp (60–90 ml);
- e) assess delay from ingestion.
Identification of additional risk factors such as extreme ages (young children, elderly), pregnancy, underlying disease, and the form of the ingested agent (solid, liquid, gel, vapors-concomitant aspiration).
Supportive care rather than specific antidotes is the mainstay of treatment. Secure airway patency and hemodynamic stabilization.
Prevent vomiting, repeat esophageal passage, and aspiration by:
- a) use of antiemetics (metoclopramide);
- b) seated 45° position during transport;
- c) avoid gastric lavage and induced emesis;
- d) avoid diluents (milk, water). Do not dilute acids with water; this would result in excessive heat production. Dilution may be beneficial for ingestion of solid or granular alkaline material if performed within 30 minutes after ingestion using small volumes of water. Because of the risk of emesis, carefully consider the risks versus benefits of dilution.
- e) avoid increasing damage by exothermic reaction: attempts at pH neutralization with either a weak alkali or acid are prohibited.
Do not administer a weak acid in alkaline ingestions or a weak alkaline agent in acid ingestions. There is a risk of heat production resulting from this exothermic reaction. In addition, the risk of emesis makes this a hazardous intervention.
General management
If a person is suspected to have ingested large quantities of acidic or alkaline substances according to history taking, physical examination, and upper endoscopy (higher than grade 2B), admission to a medical or surgical ICU is mandatory. By using this management approach, the development of serious complications, if any, can be rapidly treated, and the formation of strictures after recovery can be reduced. However, clinical signs may vary between patients; therefore, strict individual evaluation is necessary. It should be considered that the presence of a symptom or sign alone cannot be used to predict the degree of injury.
Endoscopy is not necessary if there are no symptoms and if unintentional ingestion of small volumes of acid or alkaline substances can be confirmed on the basis of history taking. The patient can be followed at the outpatient clinic after discharge 14.
Other patients should be admitted and kept nil per os, and chest and abdominal X-ray scans should be taken to assess for perforation. In addition, an intravenous (IV) line must be kept for fluid resuscitation in patients with hypotension. To prevent stress ulcers and additional damage to the esophagus from the regurgitated gastric acid, IV proton pump inhibitors can be administered 38. If patients experience pain, it should be controlled with adequate administration of narcotic anesthetics. Perforation, mediastinitis, and peritonitis are indications for emergent surgery. For the treatment of patients with injuries higher than grade 3 that are observed by using endoscopy or those suspected to have esophageal perforation, broad-spectrum IV antibiotics such as third-generation cephalosporins should be administered. In patients with respiratory difficulties, laryngoscopic observation is required to evaluate for the need for a tracheostomy. In patients with accompanying oropharyngeal injury, careful management considering airway obstruction is necessary. If there is swelling of the larynx or epiglottis, the airway should be maintained by performing tracheotomy rather than tracheal intubation.
Several methods for the management of caustic esophageal injuries must be avoided before their evaluation, which include administering drugs that may induce vomiting. This is because such methods may reexpose the esophagus to the caustic substances residing in the stomach. Neutralizers must also be avoided because the heat generated from the neutralization reaction may worsen the tissue injury. Furthermore, nasogastric tubes must also be avoided, as they may induce vomiting and reexpose the esophagus to the caustic substances; the pressure generated during vomiting may also increase the risk of perforation.
Gastric emptying and decontamination
- Do not administer emetics because of risks of re-exposure of the vulnerable mucosa to the caustic agent. This may result in further injury or perforation.
- Gastric lavage by traditional methods using large-bore orogastric Ewald tubes are contraindicated in both acidic and alkaline ingestions because of risk of esophageal perforation and tracheal aspiration of stomach contents.
- In large-volume liquid acid ingestions, nasogastric tube (NGT) suction may be beneficial if performed rapidly after ingestion. Pyloric sphincter spasm may prolong contact time of the agent to the gastric mucosa for up to 90 minutes. Nasogastric tube suction may prevent small intestine exposure. Esophageal perforation is rare. Nasogastric tube suction may be of particular value following ingestion of zinc chloride, mercuric chloride, or hydrogen fluoride, unless signs of perforation are present. This should be done after consulting with a regional poison control center.
- Activated charcoal is relatively contraindicated in caustic ingestions because of poor adsorption and endoscopic interference.
Upper GI endoscopy
As described above, upper GI endoscopy to evaluate the degree of injury must be performed within 24 hours. Patients with grade 0 injuries can be discharged immediately, and those with grade 1 or 2A injuries do not require specific treatment. Patients can consume liquids, and advance to regular food within 24 to 48 hours. Patients with grade 2B or 3 injuries can be given liquids through a nasogastric tube 24 hours after the ingestion of caustic substances, and may drink water if they are able to swallow saliva after 48 hours. Patients with grade 3 injuries must be carefully observed for perforation symptoms for at least 1 to 2 weeks after the ingestion.
Nutritional approach
Caustic ingestion can induce systemic inflammatory response syndrome (SIRS) or sepsis with a severe hypermetabolic and catabolic response. Negative nitrogen balance and weight loss are related to injury severity. (Level 3–4)
Use as soon as possible the gastrointestinal tract for nutrition. Patients with low grade injuries should resume oral alimentation as soon as they are able to swallow. In patients with severe burns, enteral feeding through jejunostomy or nasojejunal tube is recommended rather than a gastrostomy due to the possibility of a hidden gastric outlet obstruction (Level 5)
Surgery
Esophagectomy is required for patients with severe stricture 39; however, this may result in negative long-term consequences concerning the survival rate or functional capacity 23. Emergent surgery is required for patients with perforation, mediastinitis, and peritonitis. If performed by an experienced surgeon, minimally invasive thoracoscopic and laparoscopic procedures result in better outcomes than conventional methods 40. The most important factors to ensure successful recovery include vascular supply and low tension of the anastomotic site. In patients with damage to both the esophagus and stomach, the colon is usually used as a source of replacement tissue. On the other hand, in patients with damage to only the esophagus, the stomach is pulled up toward the mediastinum to replace the esophagus.
Emergency surgery for caustic injuries
Emergency surgery is eventually required in a small number of patients with transmural necrosis to avoid involvement of adjacent organs and death. Laparotomy is usually performed but laparoscopic exploration has been reported as feasible and safe 1.
Transhiatal esophagectomy and total gastrectomy are the most frequently employed surgical procedures in the acute setting. Meanwhile, esophagectomy with gastric preservation and total gastrectomy with esophagojejunostomy can be performed if transmural necrosis is limited to the esophagus or the stomach, respectively 1.
Feeding jejunostomy should be systematically constructed at the end of the operation, regardless of the type of surgical procedure performed 1.
Extended surgery (beyond esophagogastrectomy) should be attempted in case of existing injuries on other abdominal organs. All injured organs should be resected during the first operation as caustic lesions invariably progress. Mortality rates are high, but surgery may be only choice for these patients 1.
If the patient’s conditions allow, immediate biliary and pancreatic reconstruction should be attempted after pancreatoduodenectomy for caustic necrosis 1.
Transmural esophageal necrosis may lead to subsequent tracheobronchial extension in a small number (<10 %) of patients. Preoperative bronchoscopy should be performed in all patients considered for surgery. In the presence of tracheobronchial necrosis, esophagectomy should be performed by a right thoracic approach. Tracheobronchial necrosis can be successfully treated with pulmonary patch technique 1.
Massive intestinal necrosis should be a reason for the surgeon to stop due to inability of later reconstruction and nutrition 1.
Mortality rates are high, but surgery may be only choice for these patients. Factors which have a negative impact on outcome include advanced age, tracheobronchial injuries, emergency esophagectomy, need for extended resections and severe modifications of laboratory tests (pH < 7.2, AST > 2 N, renal failure, etc.) 1.
The need to perform emergency surgery for caustic injuries has a persistent long-term negative impact both on survival and functional outcome. Moreover, esophageal resection is an independent negative predictor of survival after emergency surgery 1.
Endoscopic treatment of esophageal stricture
Esophageal caustic strictures are frequently complex, i.e. long (>2 cm), angulated, irregular, and multiple. In addition, the “remodeling time”, i.e. the time to stricture stabilization ranges between 6 months to 3 years. As a consequence, the reported success rate of dilatation is lower than for other benign esophageal strictures. The optimum time for dilatation is after healing of the acute injury, usually in the 3rd week. Late management is usually associated with marked esophageal wall fibrosis and collagen deposition, which requires more endoscopic sessions for adequate dilatation. This is a crucial issue in developing countries, where late presentations are more than 50 %.
Dilatation can be carried out with balloon dilators or Savary bougies. A prospective randomized study has shown no clear advantage of each method in peptic esophageal strictures. Savary dilators are considered more reliable and effective than balloon dilators in consolidated strictures. Moreover, Savary bougies offer the advantage of “feeling” the resistance to dilatation under the operator’s hands.
“Rules of the thumb”:
- To begin with dilators that are one or two French sizes smaller than the estimated diameter of the stricture,
- Not to dilate more than two to three sizes larger than the size of the first dilator meeting resistance.
The perforation rate after dilatation for caustic strictures ranges from 0.4 to 32 %, higher than for other benign strictures. Fluoroscopy during dilatation may help in difficult cases. Although comparative trials are not available, selective use of fluoroscopy is supported by extensive clinical experience.
The interval between dilatations varies from less than 1 week to 2–3 weeks. Although three or four sessions may provide durable results, the number of dilatation required is unpredictable and the endoscopic treatment may continue for years. A cut-off value for stopping dilatations is not clear and is influenced by patient, physician and geographic factors. In adult studies, the maximal esophageal wall thickness at CT scan and the involvement of muscolaris propria at endoscopic ultrasound were found to be significant predictors of stricture development, more difficult dilatations, and recurrent stricture. Gastroesophageal reflux and alterations in esophageal motility due to esophageal wall fibrosis can contribute to persistent dysphagia, in spite of apparently successful dilatations.
A sustained esophageal lumen patency is not the only therapeutic goal: especially in children, an associated improvement in nutritional status should be considered an important end-point.
Gastrostomy feeding may be life-saving, especially in developing countries. Moreover, gastrostomy allows a retrograde approach for dilatation. In challenging strictures, a nylon thread left between the nose and the gastrostomy maintains luminal access and facilitates further dilatations.
Use of intralesional steroids and Mitomycin C applied endoscopically have been evaluated in several studies. Apparently, intralesional steroids favour a longer symptom-free time interval between dilatations but seem less effective in caustic strictures. Overall, there is no convincing evidence of the efficacy of these procedures.
There is no convincing evidence that intraluminal stenting as an alternative to repeat dilatations is beneficial. Early stenting has been proposed to prevent stricture in uncontrolled studies. The number of dilatations and the duration of treatment were reduced. Notably, 50 % of children in whom a home-made stent was placed after the first dilatation, did not require further treatment.
Long-term outcomes of stent placement for refractory benign esophageal strictures are poor. Partially covered Self Expanding Metallic Stents (SEMS) are almost abandoned, in spite of their superior anchoring capacity, because of the associated hyperplastic ingrowth or overgrowth, with consequent difficult removal and recurrent dysphagia. Fully covered Self Expanding Polyflex Stents (SEPS) and Self Expanding Metallic Stents (SEMS) show a reduced reactive hyperplasia at a price of a higher migration rate. Biodegradable stents begin to degrade after 4–5 weeks and to dissolve within 2–3 months. Although the migration rate is reduced owing to the uncovered design, biodegradable stents are only temporarily effective and sequential stenting has been suggested to avoid serial dilations. Moreover, hyperplastic tissue reactions have emerged as a significant problem. A recent systematic review of patients with a benign esophageal stricture (25 % caustic) treated by Self Expanding Polyflex Stents (SEPS) showed that only 52 % of the patients were dysphagia-free after a median follow-up of 13 months. A recent publication evaluated the results of stenting in benign strictures from twelve prospective studies. The stent was successfully placed in 98.7 %, but the overall clinical success rate was 24.2 %.
Management of gastric outlet obstruction
Grade three injury to the stomach is an independent risk factor for gastric outlet obstruction that can occur from a few days up to 6 years after caustic ingestion. Distal obstructions account for 60–100 % of the lesions and are located in the prepyloric area. Endoscopic balloon dilatation is safe and successful in the management of a subgroup of patients with gastric outlet obstruction. Progressive endoscopic dilatation can safely be initiated even at 2 weeks from ingestion, especially in short strictures (<25 mm).
There is no clear evidence supporting the use of stents in the management of gastric outlet obstruction.
Early surgery seems to decrease morbidity and mortality, but elective surgery earlier than 3 months is considered risky because of the poor nutritional status, adhesions, edematous gastric wall, difficult assessment of the extent of gastric resection due to ongoing fibrosis.
Pyloroplasty may be performed in patients with moderate/localized strictures, but the risk of recurrent stricture is high.
Gastrojejunostomy is indicated in the presence of extensive perigastric adhesions, unhealthy duodenum, and poor general condition; marginal ulcerations are reported. In selected patients the operation can safely be performed through a laparoscopic approach.
The indication for gastric resection as prophylaxis against malignancy has been probably overstated in the literature. Partial gastric resection seems preferred by most surgeons. The type of surgery should be chosen according to local and general conditions.
Esophageal reconstruction
When esophageal dilatation is not possible or fails to provide an adequate esophageal caliber in the long-term, esophageal replacement by retrosternal stomach or, preferably, colonic interposition should be considered.
A laryngoscopic examination is mandatory prior to all esophageal reconstructions for caustic injuries.
The surgical bypass should be performed at least 6 months after caustic ingestion or emergency surgery since the “remodeling time”, i.e. time to stricture stabilization, is rather long.
Removal of the native esophagus in adult patients is largely debated. It seems advisable in children because of the higher risk of cancer in the long-term.
No randomized studies address the issue of which type of esophagoplasty is preferable. There are pros and cons for either right or left colon. An expert surgeon should do what he/she is used to do.
One-stage esophageal resection and replacement with a gastric conduit, instead of a bypass, is feasible and safe in patients with isolated distal esophageal strictures.
Minimally invasive/hybrid surgical techniques have been used with favourable results in selected patients.
Angiographic study of the vascular pedicle is not routinely recommended before colon interposition or bypass, with the exception of patients with previously failed surgical attempts.
Surgical revision is effective in patients who present with redundancy of the interposed colon years after retrosternal or mediastinal reconstruction.
Pharyngeal strictures are difficult to manage and require special expertise. Endoscopic laser therapy of pharyngo-laryngeal adhesions may prove useful in selected patients before definitive surgical treatment. Colopharyngoplasty for strictures involving the pharynx is a safe and effective procedure. In such circumstances, the restoration of upper digestive tract continuity requires concomitant esophageal and pharyngeal reconstruction with resection of all scar tissue. Treatment of pharyngeal and laryngeal injuries should be done at the same surgical session. Supraglottic laryngectomy and suprahyoid pharyngectomy are required if the epiglottis and/or the base of the tongue are involved.
Temporary tracheostomy is mandatory during the rehabilitation training period after colopharyngoplasty. The postoperative re-education process is long and difficult and requires full cooperation from a psychiatric stable patient.
Advanced age has a negative impact on esophageal reconstruction. Patients older than 55 years are likely to experience severe complications, worse functional outcomes, and decreased long-term survival. For these reasons colopharyngoplasty should not be offered after this age limit.
Use of myocutaneous flaps and free jejunal grafts should be considered for salvage cervical esophageal reconstruction and restoration of alimentary transit after previously failed surgical attempts.
Prevention of strictures
The use of corticosteroids to prevent the formation of strictures is controversial. Usually, it is not recommended because corticosteroids increase the adverse effects without actually preventing stricture formation, as stricture formation is determined by the initial depth of the injury 41. Grade 3 injuries especially are not affected by the use of corticosteroids. Intralesional injection of triamcinolone has been attempted; however, there are no clear data on the effectiveness, appropriate dosage, and frequency of administration that is required to prevent stricture formation 42.
There is an old study that has shown that antibiotic use significantly helps in preventing strictures 43. However, the efficacy has not been proven in patients without infection. Currently, the use of antibiotics is not recommended for preventing strictures in patients who are not being treated with corticosteroids.
Nasogastric tube insertion can cause infection, acid reflux, and long strictures; therefore, its unique use is not currently recommended. However, a report suggested that nasogastric tube insertion can be used to provide enteral nutrition; therefore, it can be used selectively 44.
Several reports stated that intramucosal injection of mitomycin-C, a chemotherapeutic agent with DNA cross-linking activity, was helpful to prevent strictures 45; however, patients should be observed carefully because systemic absorptions can cause serious adverse effects. A recent meta-analysis indicated positive long-term results; however, additional prospective studies are needed to determine the appropriate concentration, administration period, and frequency of administration, as theoretically, malignant tumors can develop 45. Therefore, this therapeutic method should be used with caution.
Several reports have shown the usefulness of a specially designed stent (silicone rubber or Polyflex stent) for preventing stricture formation 46, 47. However, their low efficacy (<50%) and high expulsion rate (>25%) were problematic. Recently, researchers of a study on the use of a polytetrafluoroethylene stent reported an efficacy of 72% during a period of 9 to 14 months, and researchers of another study on a biodegradable stent reported a 45% efficacy during 53 months, indicating the development of various stent models with varying efficacies. Bougie dilatation has been recommended; however, its efficacy is unclear and additional studies are required.
Apart from the treatment models described above, antioxidants (such as 5-fluorouracil and vitamin E), phosphatidylcholine, octreotide, and interferon-α-2b are being studied for their utility in preventing stricture formation in animal models; however, they are not yet at a stage where they can be used to treat humans. More time may be needed before antioxidants could be used for treatment.
Once a stricture develops, balloon dilatation can be attempted carefully 48.
Caustic ingestion prognosis
The most important prognostic factors include the degree of tissue injury and the underlying condition of the patient. Most deaths occur because of complications such as mediastinitis and peritonitis; therefore, strict management in the initial stage is crucial to avoid the occurrence of complications. The most representative chronic complications include stricture, squamous cell carcinoma, and a decrease in lower esophageal sphincter pressure, which leads to reflux esophagitis, esophageal motility disorder, intractable pain, gastric outlet obstruction, acidity, and protein losing enteropathy. Acid reflux may be an aggravating factor that cause refractory stricture of the esophagus; therefore, regular observation and aggressive anti-acid therapy is necessary in patients with corrosive esophagitis 35.
- Bonavina L, Chirica M, Skrobic O, et al. Foregut caustic injuries: results of the world society of emergency surgery consensus conference. World J Emerg Surg. 2015;10:44. Published 2015 Sep 26. doi:10.1186/s13017-015-0039-0 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4583744[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Park KS. Evaluation and management of caustic injuries from ingestion of Acid or alkaline substances. Clin Endosc. 2014;47(4):301-307. doi:10.5946/ce.2014.47.4.301 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4130883[↩][↩]
- Kluger Y, Ishay OB, Sartelli M, et al. Caustic ingestion management: world society of emergency surgery preliminary survey of expert opinion [published correction appears in World J Emerg Surg. 2015;10:56]. World J Emerg Surg. 2015;10:48. Published 2015 Oct 16. doi:10.1186/s13017-015-0043-4 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4609064[↩]
- Gumaste VV, Dave PB. Ingestion of corrosive substances by adults. Am J Gastroenterol. 1992;87:1–5.[↩][↩][↩]
- Watson WA, Litovitz TL, Rodgers GC, Klein-Schwartz W, Reid N, Youniss J, et al. 2004 annual report of the american association of poison control centers toxic exposure surveillance system. Am J Emerg Med. 2005;23:589–666. doi: 10.1016/j.ajem.2005.05.001[↩]
- Riffat F, Cheng A. Pediatric caustic ingestion: 50 consecutive cases and a review of the literature. Dis Esophagus. 2009;22:89–94.[↩][↩]
- Yeom HJ, Shim KN, Kim SE, et al. Clinical characteristics and predisposing factors for complication of caustic injury of the upper digestive tract. Korean J Med. 2006;70:371–377.[↩]
- Chang JM, Liu NJ, Pai BC, Liu YH, Tsai MH, Lee CS, et al. The role of age in predicting the outcome of caustic ingestion in adults: a retrospective analysis. BMC Gastroenterol. 2011 Jun 14. 11:72.[↩]
- Rollin M, Jaulim A, Vaz F, Sandhu G, Wood S, Birchall M, et al. Caustic ingestion injury of the upper aerodigestive tract in adults. Ann R Coll Surg Engl. 2015 May. 97 (4):304-7.[↩][↩]
- Cheng HT, Cheng CL, Lin CH, Tang JH, Chu YY, Liu N, et al. Caustic ingestion in adults: the role of endoscopic classification in predicting outcome. BMC Gastroenterol. 2008;8:1. doi: 10.1186/1471-230X-8-1[↩]
- Knezevic JD, Radovanovic NS, Simic AP, Kotarac MM, Skrobic OM, Konstantinovic VD, et al. Colon interposition in the treatment of esophageal caustic strictures: 40 years of experience. Dis Esophagus. 2007;20(6):530–534. doi: 10.1111/j.1442-2050.2007.00694.x[↩]
- Appelqvist P, Salmo M. Lye corrosion carcinoma of the esophagus: a review of 63 cases. Cancer. 1980;45(10):2655-2658. doi:10.1002/1097-0142(19800515)45:10<2655::aid-cncr2820451028>3.0.co;2-p[↩]
- Jung IS, Kim JS. A case of corrosive gastritis caused by salt-fermented Northern Sand Lance. Korean J Gastrointest Endosc. 2011;42:366–368.[↩]
- Contini S, Scarpignato C. Caustic injury of the upper gastrointestinal tract: a comprehensive review. World J Gastroenterol. 2013;19:3918–3930.[↩][↩][↩][↩][↩][↩][↩]
- Goldman LP, Weigert JM. Corrosive substance ingestion: a review. Am J Gastroenterol. 1984;79:85–90.[↩]
- Wasserman RL, Ginsburg CM. Caustic substance injuries. J Pediatr. 1985;107:169–174.[↩]
- Kim HG, Han KH, Lee SI, et al. A case of corrosive gastritis caused by hydrochloric acid. Korean J Gastrointest Endosc. 1988;8:19–23.[↩]
- Arévalo-Silva C, Eliashar R, Wohlgelernter J, Elidan J, Gross M. Ingestion of caustic substances: a 15-year experience. Laryngoscope. 2006;116:1422–1426.[↩]
- Zargar SA, Kochhar R, Nagi B, Mehta S, Mehta SK. Ingestion of strong corrosive alkalis: spectrum of injury to upper gastrointestinal tract and natural history. Am J Gastroenterol. 1992;87:337–341.[↩][↩]
- Zargar SA, Kochhar R, Mehta S, Mehta SK. The role of fiberoptic endoscopy in the management of corrosive ingestion and modified endoscopic classification of burns. Gastrointest Endosc. 1991;37:165–169.[↩][↩][↩][↩]
- Fisher RA, Eckhauser ML, Radivoyevitch M. Acid ingestion in an experimental model. Surg Gynecol Obstet. 1985;161:91–99.[↩]
- Poley JW, Steyerberg EW, Kuipers EJ, et al. Ingestion of acid and alkaline agents: outcome and prognostic value of early upper endoscopy. Gastrointest Endosc. 2004;60:372–377.[↩][↩][↩]
- Chirica M, Resche-Rigon M, Bongrand NM, et al. Surgery for caustic injuries of the upper gastrointestinal tract. Ann Surg. 2012;256:994–1001.[↩][↩]
- Gaudreault P, Parent M, McGuigan MA, Chicoine L, Lovejoy FH., Jr Predictability of esophageal injury from signs and symptoms: a study of caustic ingestion in 378 children. Pediatrics. 1983;71:767–770.[↩]
- Salzman M, O’Malley RN. Updates on the evaluation and management of caustic exposures. Emerg Med Clin North Am. 2007;25:459–476.[↩]
- Caustic Ingestions Clinical Presentation. https://emedicine.medscape.com/article/813772-clinical#b4[↩]
- Riffat F, Cheng A. Pediatric caustic ingestion: 50 consecutive cases and a review of the literature. Dis Esophagus. 2009. 22(1):89-94.[↩]
- Rigo GP, Camellini L, Azzolini F, et al. What is the utility of selected clinical and endoscopic parameters in predicting the risk of death after caustic ingestion? Endoscopy. 2002;34:304–310.[↩]
- Cheng YJ, Kao EL. Arterial blood gas analysis in acute caustic ingestion injuries. Surg Today. 2003;33:483–485.[↩]
- Katzka DA. Caustic injury to the esophagus. Curr Treat Options Gastroenterol. 2001;4:59–66.[↩]
- Celik B, Nadir A, Sahin E, Kaptanoglu M. Is esophagoscopy necessary for corrosive ingestion in adults? Dis Esophagus. 2009;22:638–641.[↩]
- Cabral C, Chirica M, de Chaisemartin C, et al. Caustic injuries of the upper digestive tract: a population observational study. Surg Endosc. 2012;26:214–221.[↩]
- Aronow SP, Aronow HD, Blanchard T, Czinn S, Chelimsky G. Hair relaxers: a benign caustic ingestion? J Pediatr Gastroenterol Nutr. 2003;36:120–125.[↩]
- [Guideline] Tringali A, Thomson M, Dumonceau JM, Tavares M, Tabbers MM, et al. Pediatric gastrointestinal endoscopy: European Society of Gastrointestinal Endoscopy (ESGE) and European Society for Paediatric Gastroenterology Hepatology and Nutrition (ESPGHAN) Guideline Executive summary. Endoscopy. 2017 Jan. 49 (1):83-91.[↩]
- Chiu HM, Lin JT, Huang SP, Chen CH, Yang CS, Wang HP. Prediction of bleeding and stricture formation after corrosive ingestion by EUS concurrent with upper endoscopy. Gastrointest Endosc. 2004;60:827–833.[↩][↩]
- Kamijo Y, Kondo I, Kokuto M, Kataoka Y, Soma K. Miniprobe ultrasonography for determining prognosis in corrosive esophagitis. Am J Gastroenterol. 2004;99:851–854.[↩]
- Ryu HH, Jeung KW, Lee BK, et al. Caustic injury: can CT grading system enable prediction of esophageal stricture? Clin Toxicol (Phila) 2010;48:137–142.[↩]
- Cakal B, Akbal E, Köklü S, Babali A, Koçak E, Taş A. Acute therapy with intravenous omeprazole on caustic esophageal injury: a prospective case series. Dis Esophagus. 2013;26:22–26.[↩]
- Bothereau H, Munoz-Bongrand N, Lambert B, Montemagno S, Cattan P, Sarfati E. Esophageal reconstruction after caustic injury: is there still a place for right coloplasty? Am J Surg. 2007;193:660–664.[↩]
- Zhou JH, Jiang YG, Wang RW, et al. Management of corrosive esophageal burns in 149 cases. J Thorac Cardiovasc Surg. 2005;130:449–455.[↩]
- Fulton JA, Hoffman RS. Steroids in second degree caustic burns of the esophagus: a systematic pooled analysis of fifty years of human data: 1956-2006. Clin Toxicol (Phila) 2007;45:402–408.[↩]
- Siersema PD, de Wijkerslooth LR. Dilation of refractory benign esophageal strictures. Gastrointest Endosc. 2009;70:1000–1012.[↩]
- Krey H. On the treatment of corrosive lesions in the oesophagus; an experimental study. Acta Otolaryngol Suppl. 1952;102:1–49.[↩]
- Kochhar R, Poornachandra KS, Puri P, et al. Comparative evaluation of nasoenteral feeding and jejunostomy feeding in acute corrosive injury: a retrospective analysis. Gastrointest Endosc. 2009;70:874–880.[↩]
- Berger M, Ure B, Lacher M. Mitomycin C in the therapy of recurrent esophageal strictures: hype or hope? Eur J Pediatr Surg. 2012;22:109–116.[↩][↩]
- De Peppo F, Zaccara A, Dall’Oglio L, et al. Stenting for caustic strictures: esophageal replacement replaced. J Pediatr Surg. 1998;33:54–57.[↩]
- Broto J, Asensio M, Vernet JM. Results of a new technique in the treatment of severe esophageal stenosis in children: poliflex stents. J Pediatr Gastroenterol Nutr. 2003;37:203–206.[↩]
- Lee SI, Shn SH, Park IS, Choi HJ. Dilatation of severe corrosive esophageal stricture guided by right coronary artery catheter. Korean J Gastrointest Endosc. 1991;11:77–80.[↩]