Cervicocranial syndrome
Craniocervical syndrome also called Barre-Lieou syndrome, craniocervical junction syndrome or posterior cervical sympathetic syndrome, is an entity whose symptoms includes vertigo, cephalea, tinnitus, facial pain, otalgia, dysphagia, pain of the carotid artery are thought to be caused by cervical factors 1. Craniocervical syndrome has not been agreed as a neurological entity 2, but is used as a repository for undiagnosed symptoms including those succeeding acute neck injuries, despite the term chronic originally described. Symptoms alleged are occipital headaches 3, nystagmus on head movement 4, tinnitus, spasms,blurred vision, corneal hyperaesthesia, and corneal ulcers. Other symptoms are anxiety, depression, and memoryand cognitive disorders 5. This non-specific constellation of symptoms has been ascribed to trauma or arthritis of the third and fourth cervical vertebrae or disks, which in turn cause a disturbance of the cervical sympathetic nerves and disordered circulation, in the cranial nuclei V and VIII 6, 7.
According to the National Institute of Health (NIH), the craniocervical syndrome is neurologic syndrome following injury of the spinal sympathetic nerves of the neck. The injury usually results from arthritis or pinching by the adjacent vertebrae. Symptoms include facial pain, chronic allergies, dizziness, neck pain, ear pain and vertigo.
Much of the literature predates 1990 and appears in journals of chiropraxis, acupuncture, and manipulation 2. Although the validity of craniocervical syndrome is not generally accepted 8, the term still appears in the literature. Yang Choen Lie 7 described a sympathetic disorder associated with cervical ‘‘arthritis’’ in his thesis of 1928.
Cervicocranial syndrome causes
The causes of craniocervical syndrome can be congenital or acquired.
Congenital causes
Congenital craniocervical junction abnormalities may be specific structural abnormalities or general or systemic disorders that affect skeletal growth and development. Many patients have multiple abnormalities.
Structural skeletal abnormalities include the following:
- Os odontoideum (anomalous bone that replaces all or part of the odontoid process)
- Atlas assimilation (congenital fusion of the atlas and occipital bone)
- Congenital Klippel-Feil malformation (eg, with Turner syndrome or Noonan syndrome), often associated with atlanto-occipital anomalies
- Atlas hypoplasia
- Platybasia, often with basilar invagination, Chiari malformations (descent of the cerebellar tonsils or vermis into the cervical spinal canal), and other abnormalities
Systemic disorders that affect skeletal growth and development and involve the craniocervical junction include the following:
- Achondroplasia (impaired epiphyseal bone growth, resulting in shortened, malformed bones) sometimes causes the foramen magnum to narrow or fuse with the atlas and thus may compress the spinal cord or brain stem.
- Down syndrome, Morquio syndrome (mucopolysaccharidosis IV), or osteogenesis imperfecta can cause atlantoaxial subluxation or dislocation.
Acquired causes
Acquired craniocervical junction causes include injuries and disorders.
- Rheumatoid arthritis is the most common disease cause
- Injuries may involve bone, ligaments, or both and are usually caused by vehicle or bicycle accidents, falls, and particularly diving; some injuries are immediately fatal.
- Paget disease of the cervical spine can cause atlantoaxial dislocation or subluxation, basilar invagination, or platybasia.
- Metastatic tumors that affect bone can cause atlantoaxial dislocation or subluxation.
- Slowly growing craniocervical junction tumors (eg, meningioma, chordoma) can impinge on the brain stem or spinal cord.
Cervicocranial syndrome symptoms
Symptoms and signs of craniocervical junction abnormalities can occur after a minor neck injury or spontaneously and may vary in progression. Presentation varies by degree of compression and by structures affected.
The most common manifestations are:
- Neck pain, often with headache
- Symptoms and signs of spinal cord compression
Neck pain often spreads to the arms and may be accompanied by headache (commonly, occipital headache radiating to the skull vertex); it is attributed to compression of the C2 root and the greater occipital nerve and to local musculoskeletal dysfunction. Neck pain and headache usually worsen with head movement and can be precipitated by coughing or bending forward. If patients with Chiari malformation have hydrocephalus, being upright may aggravate the hydrocephalus and result in headaches.
Spinal cord compression involves the upper cervical cord. Deficits include:
- Spastic paresis in the arms, legs, or both, caused by compression of motor tracts
- Commonly, impaired joint position and vibration senses (posterior column function)
- Tingling down the back, often into the legs, with neck flexion (Lhermitte sign)
- Uncommonly, impaired pain and temperature senses (spinothalamic tract function) in a stocking-glove pattern
Neck appearance, range of motion, or both can be affected by some abnormalities (eg, platybasia, basilar invagination, Klippel-Feil malformation). The neck may be short, webbed (with a skinfold running approximately from the sternocleidomastoid to the shoulder), or in an abnormal position (eg, torticollis in Klippel-Feil malformation). Range of motion may be limited.
Brain compression (eg, due to platybasia, basilar invagination, or craniocervical tumors) may cause brain stem, cranial nerve, and cerebellar deficits. Brain stem and cranial nerve deficits include:
- Sleep apnea
- Internuclear ophthalmoplegia (ipsilateral weakness of eye adduction plus contralateral horizontal nystagmus in the abducting eye with lateral gaze)
- Downbeat nystagmus (fast component downward)
- Hoarseness
- Dysarthria
- Dysphagia
- Cerebellar deficits usually impair coordination.
Vertebrobasilar ischemia can be triggered by changing head position. Symptoms may include:
- Intermittent syncope
- Drop attacks
- Vertigo
- Confusion or altered consciousness
- Weakness
- Visual disturbance
Syringomyelia (cavity in the central part of the spinal cord) is common in patients with Chiari malformation. It may cause:
- Segmental flaccid weakness and atrophy, which first appear or are most severe in the distal upper extremities
- Loss of pain and temperature senses in a capelike distribution over the neck and proximal upper extremities
However, light touch is preserved.
Cervicocranial syndrome diagnosis
A craniocervical abnormality is suspected when patients have pain in the neck or occiput plus neurologic deficits referable to the lower brain stem, upper cervical spinal cord, or cerebellum. Lower cervical spine disorders can usually be distinguished clinically (based on level of spinal cord dysfunction) and by neuroimaging.
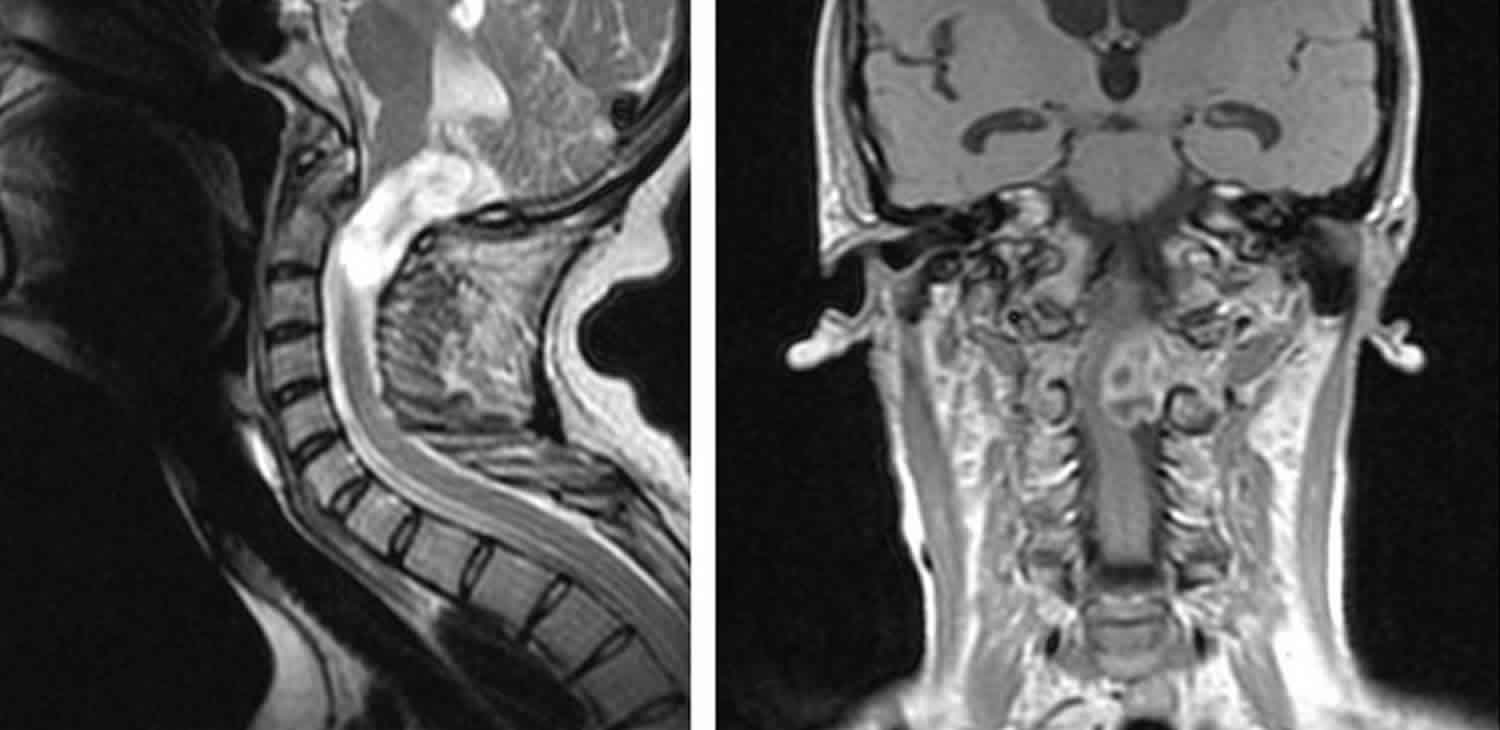
Neuroimaging
If a craniocervical abnormality is suspected, MRI or CT of the upper spinal cord and brain, particularly the posterior fossa and craniocervical junction, is done. Acute or suddenly progressive deficits are an emergency, requiring immediate imaging. Sagittal MRI best identifies associated neural lesions (eg, medulla, pons, cerebellar, spinal cord, and vascular abnormalities; syringomyelia) and soft-tissue lesions. CT shows bone structures more accurately than MRI and may be done more easily in an emergency.
If MRI and CT are unavailable, plain x-rays—lateral view of the skull showing the cervical spine, anteroposterior view, and oblique views of the cervical spine—are taken.
If MRI is unavailable or inconclusive and CT is inconclusive, CT myelography (CT after intrathecal injection of a radiopaque contrast agent) is done. If MRI or CT suggests vascular abnormalities, magnetic resonance angiography or vertebral angiography is done.
Cervicocranial syndrome treatment
If neural structures are compressed, treatment consists of reduction (traction or changes in head position to realign the craniocervical junction and thus relieve neural compression). After reduction, the head and neck are immobilized. Acute or suddenly progressive spinal cord compression requires emergency reduction.
For most patients, reduction involves skeletal traction with a crown halo ring and weight of up to about 4 kg. Reduction with traction may take 5 to 6 days. If reduction is achieved, the neck is immobilized in a halo vest for 8 to 12 wk; then x-rays must be taken to confirm stability.
If reduction does not relieve neural compression, surgical decompression, using a ventral or a dorsal approach, is necessary. If instability persists after decompression, posterior fixation (stabilization) is required. For some abnormalities (eg, due to rheumatoid arthritis), external immobilization alone is rarely successful; if it is unsuccessful, posterior fixation or anterior decompression and stabilization are required.
Several different methods of instrumentation (eg, plates or rods with screws) can be used for temporary stabilization until bones fuse and stability is permanent. In general, all unstable areas must be fused.
Radiation therapy and a hard cervical collar often help patients with metastatic bone tumors.
Calcitonin, mithramycin, and bisphosphonates may help patients with Paget disease.
- Terrahe K. Das zervikokraniale Syndrom in der Praxis des HNO-Arztes [The cervico-cranial syndrome in the practice of the otorhinolaryngologist]. Laryngol Rhinol Otol (Stuttg). 1985;64(6):292-299.[↩]
- Pearce JM. Barré-Liéou “syndrome”. J Neurol Neurosurg Psychiatry. 2004;75(2):319. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1738935/pdf/v075p00319.pdf[↩][↩]
- Del Torto U. Considerations and suggestions on a new treatment for Barre-Lieou syndrome.Chir Organi Mov2001;86(4):249–52.[↩]
- Tamura T. Cranial symptoms after cervical injury. Aetiology and treatment ofthe Barre-Lieou syndrome.J Bone Joint Surg Br1989;71:283–7.[↩]
- Neri V. Sindrome cerebrale del simpaticus cervicale.Bol Soc Med, Bologna1924;96:382.[↩]
- Barre ́JA. Sur un syndrome sympathique cervical poste ́rieur et sa causefrequente, l’arthrite cervicale.Revue Neurologique, Paris 1926;1:1246–8.[↩]
- Lie ́ou YC.Syndrome sympathique cervical poste ́rieur et arthrite cervicalechronique de la colonne verte ́brale cervicale. E ́tude clinique et radiologique.The`se. Strasbourg, 1928.[↩][↩]
- Serre H, Labauge R, Simon L,et al.Does the posterior cervical sympatheticsyndrome, so-called‘‘Barre-Lieou syndrome’’, exist? Sem Hop1970;46:1567–86.[↩]