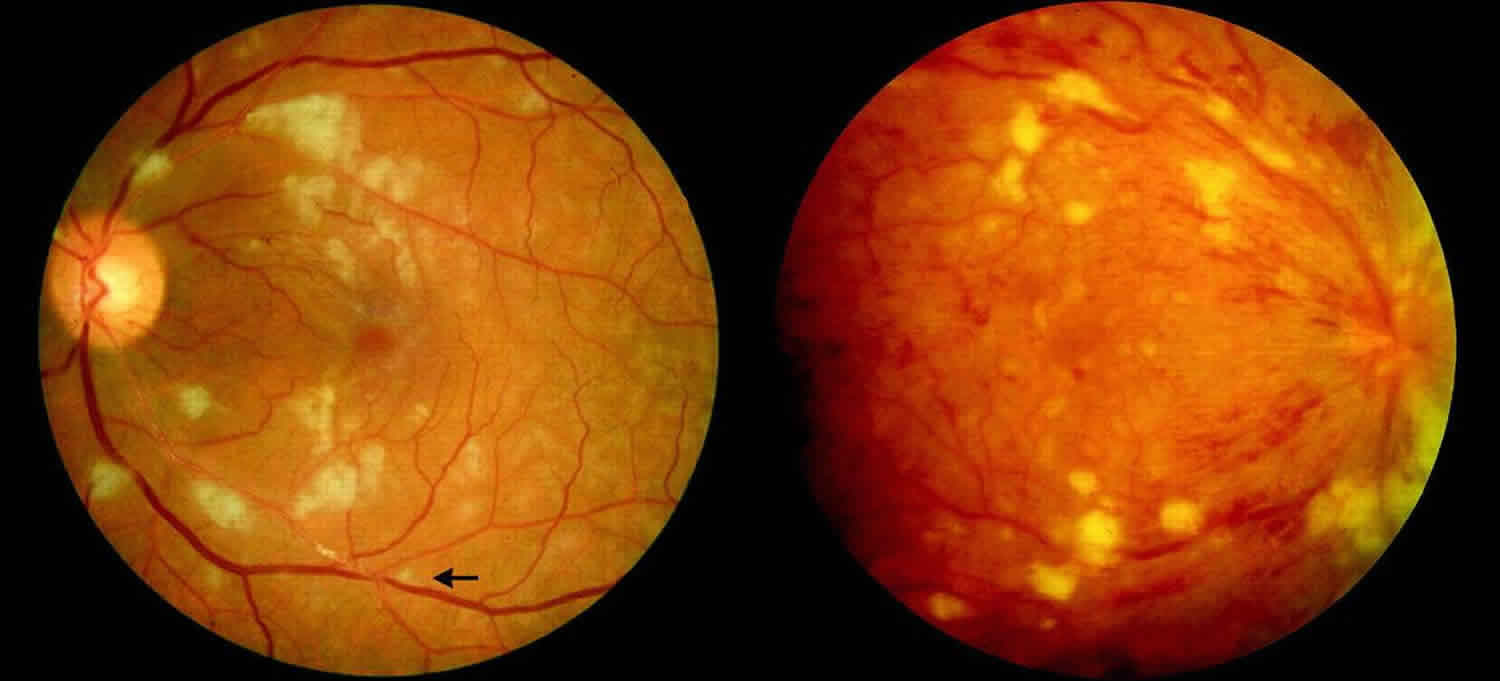
Cotton wool spots
Cotton wool spots are an abnormal finding on fundoscopic exam of the retina in otherwise healthy patients. Cotton wool spots appear as puffy white patches on the retina. Typical cotton wool spots appear as transient gray to white areas with indistinct borders in the retinal nerve fiber layer usually less than 1/3 disc diameter, often adjacent to small retinal vessels 1. A single cotton wool spot in one eye can be the earliest ophthalmoscopic finding in diabetic or hypertensive retinopathy 2. In a series of patients who had cotton-wool spots and no known medical history, diastolic blood pressure equal to or greater than 90 mmHg was detected in 50% of patients, and an elevated blood sugar was found in 20% of patients 3.
Cotton wool spots are believed to occur secondary to ischemia from retinal arteriole obstruction 4. Cotton wool spots is thought to represent nerve fiber layer infarct and pre-capillary arteriolar occlusion. However, factors responsible for focal interruption of axoplasmic flow in the retinal nerve fiber layer may result in similar intra-axonal organelle accumulations 5.
The histological hallmark of cotton wool spots is considered by many authors to be clusters of cytoid bodies which form due to focal obstruction of orthograde or retrograde axonal transport in retinal ganglion cell axons 2. They are named cytoid bodies because they look like cells, however they are eosinophilic segments of ganglion cell axons that are swollen because of defective axoplasmic flow. Cytoid bodies are usually packed with accumulations of mitochondria and other intracellular material 6.
Cotton wool spots usually fade over a few weeks following initial presentation and have only recently been associated with lasting retinal or disc damage 7. Most cotton wool spots will appear in the posterior fundus without any loss of visual acuity unless the central macula is involved 1. Traditional assumptions held that following the resolution of a cotton wool spots there were no pathological sequelae. Subsequent investigation with scanning laser ophthalmoscopy has shown localized loss of nerve fiber layer thickness corresponding with prior cotton wool spots 7. Therefore, cotton wool spots are not as innocuous as previously assumed. The incidence of cotton wool spots has rarely been reported in association with glaucoma 8 and subsequent co-localized pathologic examination following resolution of cotton wool spots has not previously been reported.
Cotton wool spots causes
Cotton wool spots causes can be categorized into:
- Ischemic: hypertension, diabetes, ocular ischemic syndrome (cotton wool spots is less common), retinal vein occlusion, anemia, hyperviscosity state, hypercoagulable state, radiation, acute blood loss.
- Immune and inflammatory conditions: systemic lupus erythematosus (SLE), dermatomyositis, scleroderma, polyarteritis nodosa, giant cell arteritis.
- Infectious: HIV retinopathy, cat-scratch disease, rocky mountain spotted fever, leptospirosis, onchocerciasis, bacteremia, fungemia.
- Embolic: carotid emboli, cardiac emboli, cardiac valvular disease, endocarditis, rheumatic heart disease, deep venous emboli, Purtscher-like retinopathy, foreign-body emboli.
- Neoplastic: lymphoma, leukemia, metastasis.
- Medication induced: interferon retinopathy.
- Miscellaneous: trauma, epiretinal membrane, high-altitude retinopathy, papilledema, papillitis, Purtscher retinopathy.
- Idiopathic 4
Cotton wool spots symptoms
Cotton wool spots in general are visually asymptomatic, however, a patient may present with vision loss if the fovea is involved 4. Systemic symptoms of the underlying cause may be present.
Cotton wool spots diagnosis
Diagnosis is usually achieved by a complete ocular examination, including a detailed dilated fundus exam. However, fluorescein angiography may reveal areas of capillary nonperfusion near cotton wool spots3. On the other hand, additional work up may be needed to detect the underlying etiology.
On ophthalmic fundus exam, cotton wool spots may appear as small, yellow-white (or grayish-white), slightly elevated lesions, which look like clouds with a fimbriate border in the superficial retina. Usually they are less than 1/3 disc areas in diameter, and are commonly found in the posterior pole of the funds 4.
Differential diagnosis of other yellow-white retinal lesions may include: myelinated nerve fibers, hard exudate, retinal infiltrate, retinal drusen, chorioretinal atrophy, intraluminal plaque and early endogenous chorioretinitis.
Cotton wool spots treatment
Work up and treatment are directed towards the underlying cause. Cotton wool spots classically disappear in 6–12 weeks, however in diabetic retinopathy they may persist for longer 3.
- Bhatt A, Nguyen C, Mosaed S, Minckler D. Clinical and pathological correlation of cotton wool spots in secondary angle closure glaucoma. Am J Ophthalmol Case Rep. 2018;10:192–195. Published 2018 Feb 28. doi:10.1016/j.ajoc.2018.02.028 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5956715[↩][↩]
- Schmidt D. The mystery of cotton-wool spots-a review of recent and historical descriptions. Eur J Med Res. 2008;13(6):231.[↩][↩]
- Adam T. Gerstenblith, Michael P. Rabinowitz. Wills Eye Manual, The: office and emergency room diagnosis and treatment of eye disease, 6th edition. Lippincott Williams & Wilkins, 2012.[↩][↩][↩]
- Purnima S. Patel, SriniVas R. Sadda. “Retinal Artery Obstructions.” In Retina (Fifth Edition), by Stephen J. Ryan, 1012-1025. Elsevier Inc., 2012.[↩][↩][↩][↩]
- D. McLeod, D. McLeod, E. M. Kohner and A. C. Bird. “The role of axoplasmic transport in the pathogenesis of retinal cotton-wool spots.” Br J Ophthalmol 61 (1977): 177-191.[↩]
- Jr, Ralph C. Eagle. Eye pathology an atlas and text . 2nd edition. Philadelphia: Lippincott Williams & Wilkins, 2011.[↩]
- Gomez M.L., Mojana F., Bartsch D.U., Freeman W.R. Imaging of long-term retinal damage after resolved cotton wool spots. Ophthalmol Times. 2009;116(12):2407–2414.[↩][↩]
- Wolter J.R. Pathology of a cotton-wool spot. Am J Ophthalmol. 1959;48(4):473–485.[↩]