Cystoplasty
Cystoplasty also known as bladder augmentation or augmentation cystoplasty, is a surgical procedure to make the bladder larger (increasing the size of the bladder) 1. The urinary bladder can be enlarged or it can be partially or completely replaced, if it is not functioning normally. For many patients, augmentation cystoplasty can provide a safe, functional reservoir that allows for urinary continence and prevention of upper tract deterioration. This is achieved by using part of the bowel to alter the bladder surgically. The bowel is a large organ, so a small part of it can be used safely for this purpose.
There are three different parts of the bowel that can be used to alter the bladder:
- the small bowel called the ileum, which is used in the ileocystoplasty
- the large bowel or colon,which is used in the colocystoplasty
- the large bowel called the cecum, which is used in the cecocystoplasty.
There are two different types of cystoplasty:
- the ‘clam’ cystoplasty
- substitution cystoplasty.
Your doctor will talk to you about which type of cystoplasty will be best for you and which part of the bowel will be used.
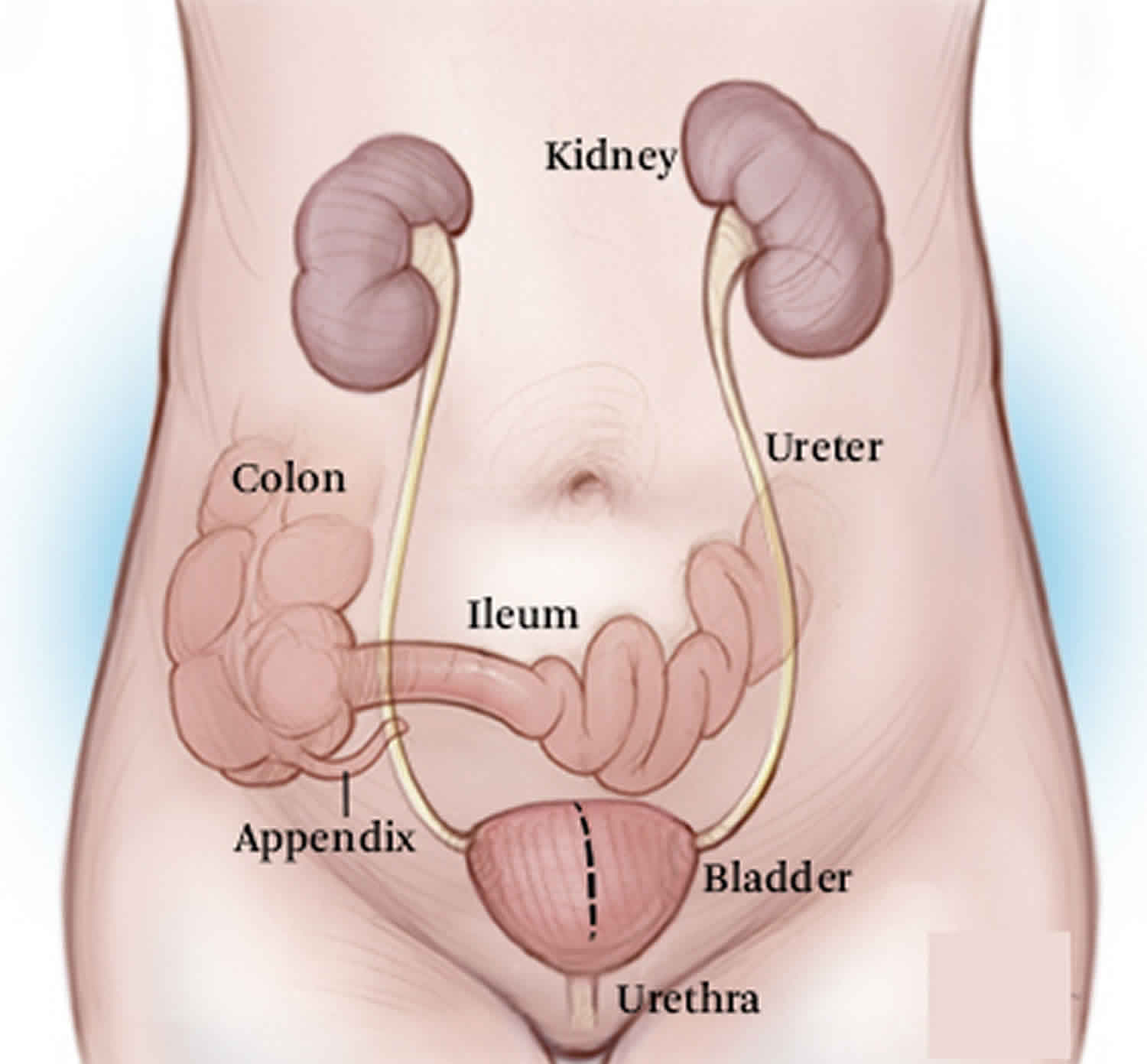
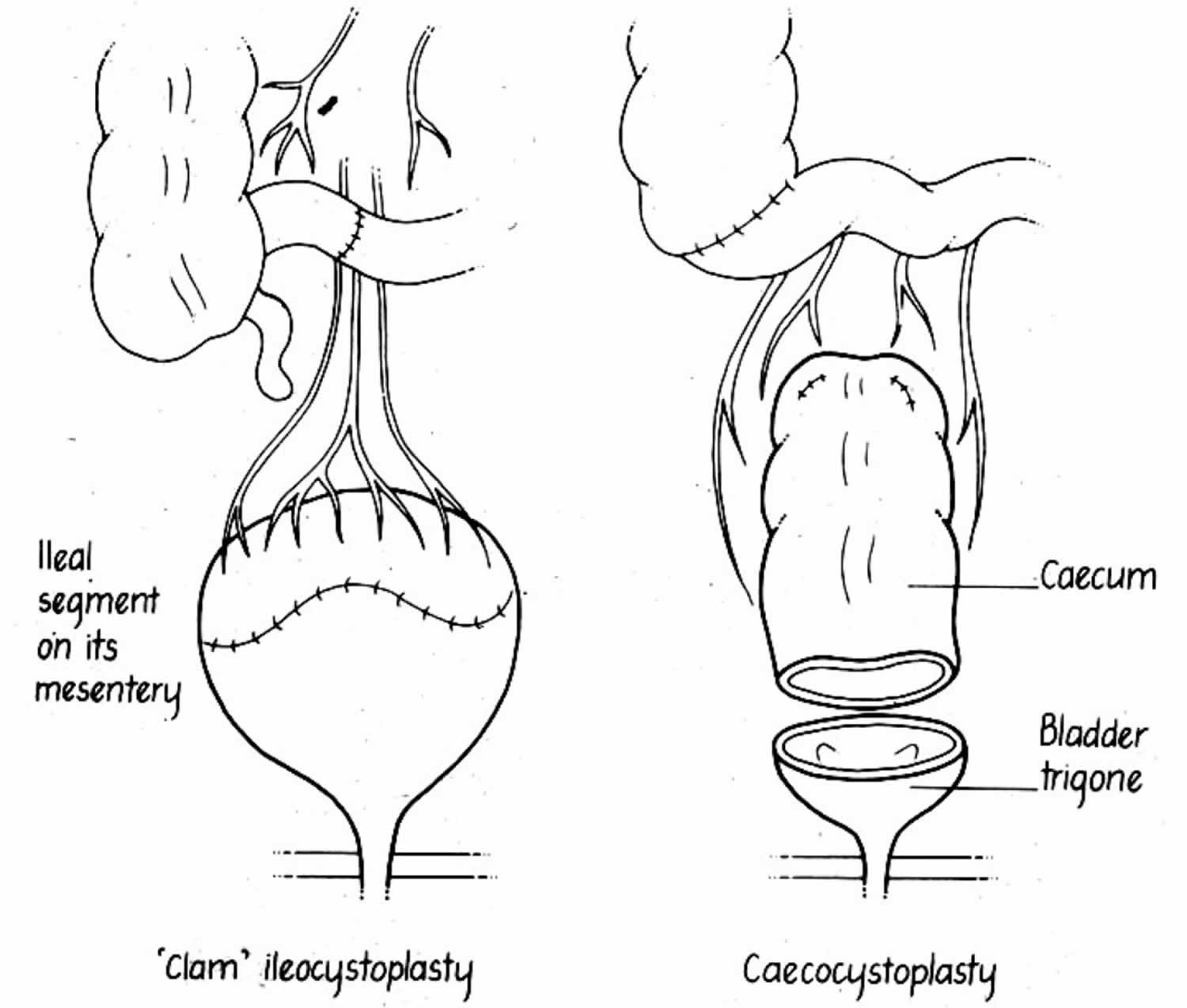
Figure 1. Cystoplasty
Why is bladder augmentation cystoplasty performed?
Augmentation cystoplasty is performed in people who have trouble urinating because of certain health problems or conditions or when other treatments have failed or do not suit your lifestyle. These include the following:
- Incontinence, the inability to hold urine (wetting).
- The muscles of the bladder are not working properly. For instance, the bladder may not stretch normally, which increases pressure in the bladder. This may cause pressure to back up to the kidneys (reflux), which can cause kidney infections and damage the kidneys. Augmentation cystoplasty can decrease pressure in the bladder.
- Spasticity (stiffness) of the bladder.
- Shrinking of the bladder caused by treatments (e.g., radiation) or diseases (e.g., spinal cord injury).
In many cases, augmentation cystoplasty is performed after the patient has performed self-catheterization for a period of time. Self-catheterization is a procedure in which the patient inserts a catheter (a thin, hollow tube) through his or her urethra (the tube through which urine comes out of the body) in order to drain urine.
Bladder enlargement surgery types
Clam cystoplasty
The clam cystoplasty involves enlargement of the bladder through a lower abdominal incision (cut) which can be below the bikini line. The bladder is opened up across the top so it forms two halves joined at the bottom end (the bladder neck). It looks like an open clam shell at this point, giving the operation its name.
The piece of bowel to be used is opened along one side so that it is a flat rectangular piece of tissue instead of a tube. It is still attached to its blood supply, even though it is no longer attached to the rest of the bowel. The prepared bowel can then be attached to the opened bladder like a ‘gusset’.
Substitution cystoplasty
The substitution cystoplasty is done through a lower abdominal incision. The damaged or diseased bladder is removed, leaving behind the bladder neck that contains the sphincter muscle which controls continence and the passage of urine. A completely new bladder can then be formed from part of the bowel which has been prepared as shown in Figure 1. This cup-like structure is then attached to the bladder neck to form the new bladder. This image shows the two types of cystoplasty; a clam ileocystoplasty and a substitution cecocystoplasty.
Bladder augmentation cystoplasty indications
Any patient with marked reduction in bladder capacity or compliance may be a candidate for augmentation cystoplasty. Conservative management for these patients usually consists of intermittent self-catheterization 2 and anticholinergic medications. In general, augmentation cystoplasty is considered when bothersome symptoms impair a patient’s lifestyle despite medical treatment or when high-pressure urinary storage places the upper urinary tracts at risk.
Both neuropathic and non-neuropathic causes for severe bladder dysfunction exist in pediatric and adult populations.
Neuropathic causes include the following:
- Spinal cord injury
- Multiple sclerosis
- Myelodysplasia
- Tethered spinal cord
Neurogenic bladder in the pediatric population is often associated with congenital anomalies, including the following:
- Spina bifida/myelomeningocele 3.
- Posterior urethral valves
- Prune belly syndrome (Eagle-Barrett syndrome)
- Bladder exstrophy
- Cloacal exstrophy
Patients with these conditions most commonly undergo augmentation cystoplasty when, despite behavioral and medical management, they experience continued incontinence, debilitating urgency, enuresis, complicated urinary tract infections (UTIs), vesicoureteral reflux (VUR) or impaired renal growth.
Some adult patients who underwent urinary diversion for an embryologic urinary defect as a child seek a healthier cosmetic and functional state. In other cases, adults have an acquired condition that is causing bladder dysfunction. Adults may present with symptoms very similar to those of children with congenital abnormalities. Again, surgery is indicated for adults with refractory symptoms and those with risk or progression of upper tract deterioration.
Nonneuropathic causes include the following:
- Detrusor instability
- Chronic cystitis, including tuberculosis and schistosomiasis
- Interstitial cystitis
- Radiation cystitis
- Classic or cloacal exstrophy
- Defunctionalized bladder in a patient who is on dialysis
Decreased bladder capacity or abnormal compliance may manifest as debilitating urgency, frequency, incontinence, recurrent urinary tract infections (UTIs), pyelonephritis, or progressive renal insufficiency.
Bladder augmentation cystoplasty contraindications
Bladder augmentation cystoplasty surgery is not suitable for:
- Patients who are unable to self catheterixe.
- Some patients with severe kidney failure.
- Patients who produce excessive volumes of urine which would mean they would have to catheterize too frequently to manage.
- Patients who produce extremely small volumes of urine.
- Patients with liver failure.
- Patients with bowel disease or who have had large volumes of bowel removed.
- Some patients who have had radiotherapy to their bladder and bowel.
Patients who are unable or unwilling to perform life-long intermittent catheterization should not undergo augmentation cystoplasty, because of the high likelihood that catheterization will ultimately be required.
In addition, patients with inflammatory bowel disease (especially Crohn disease), a short or irradiated bowel, bladder tumors, severe radiation cystitis, or severe renal insufficiency should not undergo augmentation cystoplasty.
Poor surgical candidates and patients with a short life expectancy should consider alternatives to augmentation cystoplasty, such as continued medical management or creation of a less complex, temporizing form of urinary drainage.
How is augmentation cystoplasty performed?
Before augmentation cystoplasty surgery
Before the augmentation cystoplasty is performed, you will have a series of tests and examinations, including:
- Physical exam.
- Examination of the bladder (usually cystoscopy or radiological imaging).
- A test to see how well the you holds urine and how full your bladder is before it starts to leak or transmit pressure to the kidneys.
- Blood tests
- Electrocardiogram (ECG), which provides a printout of your heart rate and rhythm
- MRSA screening (a test for infection).
Before your surgery you will need to fast. Fasting means that you cannot eat or drink anything for six hours before surgery. We will give you clear instructions about when to start fasting. It is important to follow the instructions. If there is food or liquid in your stomach during the anesthetic, it could come back up your throat and damage your lungs. Your doctor will therefore defer or re-schedule your operation until it is safe to proceed if you have not followed the fasting 4 of 7 instructions correctly. Your doctor will also ask about you about any medications you take – please bring them with you to your appointments. You will also perform a bowel prep, in which you drinks a solution that will clean out your bowel before surgery.
During augmentation cystoplasty surgery
Augmentation cystoplasty is a type of abdominal surgery, which means that the surgeon makes an incision (cut) in the patient’s abdomen to get to the bladder.
After making the incision in the abdomen, the surgeon cuts open the bladder at the top to prepare it for enlarging.
The surgeon then removes a section of the small or large intestine; detubularizes (cuts open) that link of bowel and attaches it to the top of the bladder. The bladder and bowel are then sewn together to make the bladder larger (Figure 1).
After the augmentation cystoplasty surgery
The cystoplasty surgery usually takes two to five hours depending on the type of operation.
After the augmentation cystoplasty surgery, you will stay in the hospital, usually for five to seven days. You will probably not be able to eat or drink for a couple days after surgery, and will receive fluids through an intravenous (IV) line.
While in the hospital, you will have at least two and possibly more tubes in your abdomen and bladder. Nurses and physicians will instruct you on how to care for these tubes and irrigate mucous out of the bladder, beginning immediately after surgery. The tubes and drains will be removed on your consultant’s instructions. The following timescales are a guideline:
- Wound drains will usually be removed when they stop draining after about two to three days.
- The nasogastric tube will be removed when you can drink without feeling nauseated.
- The drip in your arm or neck will be removed when you are drinking and your bowels are working again.
- Two very small tubes called stents, which you may have to keep the ureters open, usually stay in for seven to ten days.
- The clips or sutures (stitches) will be removed from the wound site after seven to ten days. Some sutures may be soluble so will not need to be removed.
- If you have a catheter in your abdominal wall (a supra pubic catheter), this will remain in place for six weeks.
- The urethral catheter, if in place, is usually removed after three to seven days.
Because the bowel is now in contact with the bladder system, you should expect that your urine will have mucus in it. You will have to irrigate this mucus on a regular basis (usually every morning) for the remainder of your life. If it is not irrigated out, the mucus can form stones and you will need additional operations to remove these stones. Retained mucus will also lead to a greater risk for infections in the urinary tract. Your nurse will do this for the first few days and then you will be shown how to perform this yourself. The frequency of the bladder washouts will be agreed with you and is different from person to person. Before going home you must feel confident in washing out your reservoir or bladder, so please ask if you are unsure.
Three weeks after the surgery, you will have a radiology test to make sure that the new, larger bladder is not leaking. If that test is deemed okay, then the tubes will be removed and you will be instructed on self-catheterization and irrigation in the clinic. You should be able to resume normal activities, including returning to work, approximately 6 weeks after the surgery.
Because your new bladder is only partially made of bladder muscle, you should expect to not be able to empty your bladder by voiding (urinating) alone after surgery. You will most likely require self-catheterization for the remainder of your life to empty your bladder. In some cases, a new channel is created during bladder augmentation surgery so that you may pass a catheter through you belly button to empty. Patients are usually taught how to do this 3 weeks after surgery.
Bladder augmentation cystoplasty recovery
On leaving hospital
Although you should allow time to rest after you have left hospital, you should also do some gentle exercise, such as a short daily walk, and gradually increase the amount and the intensity of exercise over the following few weeks. You should not do anything too strenuous or lift anything heavy, such as full shopping bags, for six to eight weeks. You should aim to be back to the same level of activity as before your operation within about three months.
Diet and fluids
There is no need to follow any special diet but it is a good idea to eat a healthy nutritious diet including fruit and vegetables. If your surgeon has used a part of your bowels to make a reservoir or to alter your bladder surgically, you may find it takes time for your bowels to return to their usual pattern. If bowel movements are still a problem, please discuss this at your next appointment or talk to your doctor.
Fluid intake is very important – you must drink at least eight to ten cups of fluid a day. This will help prevent the build-up of mucus, which not only blocks the catheters but also acts as a medium on which bacteria can grow, causing infection.
Supplies
When you leave hospital your surgical team will arrange for all the supplies you need to be delivered to your home. This will include drainage bags and equipment to carry out bladder washouts. Your surgical team will give you clear instructions on how to order more supplies. Your surgical team will also refer you to a district nurse. The district nurse will look after your wound sites and offer general advice. The catheters should not be changed or removed by anyone apart from the your surgical team unless instructed by your doctor. If you have any specific questions, please contact the nurse specialist or your surgical team.
Activities
Your doctor will advise you to refrain from sex for at least six weeks after surgery to allow for healing and to prevent infection and pain. After this time you can resume your sex life when you feel comfortable. If you have any concerns, please discuss them with your surgeon or nurse specialist. Please speak to your surgeon before resuming any sports.
If you experience any problems catheterizing, please do not hesitate to contact your doctor. Contact your nurse, your doctor, or the hospital if:
- you think you have a urine infection (urine becomes thick or smelly, you have a fever or feel unwell, or there is blood in your urine)
- your operation scar becomes hard, red, oozes or becomes inflamed
- you have persistent abdominal (tummy) or back pain
- you have persistent nausea or vomiting.
Will I have to wash out my bladder?
Yes, especially because it is made out of bowel. Your doctor or nurse will teach you how to do this and tell you how often to do it before you leave the hospital. You will need to perform washouts via the catheter up to 3 times a day to clear any mucus produced by the bowel. Often, when your body is healing after the operation, the bladder needs to be washed more frequently to prevent blockage with mucous or debris. In time you may not need to do it as often. If you leave hospital with a catheter or tube, your doctor or nurse may advise you to perform wash-outs if you feel the tube is blocked and urine is not draining out. If urine stops draining and you cannot get it to flow again, please call your doctor immediately for advice.
You will need to self catheterize every 2-3 hours initially and 1-2 times overnight. Gradually with time you should be able to increase the intervals between passing the catheter to a maximum of every 4-5 hours as the bladder and bowel patch gradually stretches over time and more urine can be held. The bladder capacity usually continues to improve for up to a year afterwards.
What if I don’t catheterize as often as required?
- The bladder can rupture or burst which can be serious and even fatal.
- You can get; kidney failure, urine infections, or stones forming in the bladder or kidneys.
- A build up of mucus in the bladder that can cause blockages.
Follow-up appointment
You will be given a follow-up appointment usually six weeks after leaving hospital. If you need to return to the hospital to have catheters or tubes removed, your doctor will arrange this before you leave. You may wish to wear a medical information bracelet or necklace as a safety precaution if you are ever taken to hospital in an emergency and are unable to communicate. A medical alert bracelet or necklace will alert staff to your condition, enabling them to provide you with the specialist care you need.
Life long follow up is required
- Blood test for kidney function and urine test for infection every 3 months for the first year
- An IVP X-Ray is sometimes required at 6 weeks.
- Review appointment at 6 weeks, 3 months, 6 months and then annually thereafter.
- Ultrasound of kidneys annually.
- Vitamin B12 levels if indicated and replacement injections if deficient.
- Flexible cystoscopy every 1-2 years after 10 years.
How will the new bladder work?
The bladder’s continence mechanism is not affected by the bladder enlargement surgery. This means that, assuming that your bladder worked properly before surgery, it should not leak urine and can often be emptied in the normal way. However, some patients find they are unable to empty out their bladder adequately or at all. This can happen immediately after surgery or later on. The only way to empty the bladder in these cases is to pass a catheter intermittently in to the bladder and drain urine.
Your doctor will give you detailed instructions on how to do this before surgery. If there are problems passing a catheter this way, an alternative will be discussed with you.
Bladder augmentation complications
All treatments and procedures carry some level of risk. The most common complications that can occur after a cystoplasty are:
- Urine infection.
- Mucous build up which may cause bladder or kidney stones to form.
- The blood becoming too acidic (acidosis) due to increased amounts of some salts being lost in the urine. This rarely causes symptoms and can be treated with bicarbonate supplement tablets.
- Inability to empty the bladder completely, which means you would have to start self-catheterization.
- Urine incontinence.
Potential risks and complications:
- Death is rare, < 1/1000.
- There is a small risk of a major event like a heart attack, stroke, heart failure, leg vein clots and pulmonary embolus, (clots dislodging to the lungs), or pneumonia .
- Damage to adjacent organs such as: ureters, (tubes from kidney to bladder), bowel, blood vessels or nerves which may require further surgery to correct.
- Inability to use the bowel segment as planned and an alternative bowel segment is used or rarely being unable to perform the procedure at all.
- Bleeding; 5% risk of needing a blood transfusion.
- Wound infection, wound breakdown or infection within the abdomen.
- Ileus – a delay in the return of bowel activity requiring gastric drainage via a nasogastric tube, intravenous fluids, nil by mouth and even intravenous feeding, sometimes requiring re-exploration of the abdomen by returning to surgery.
- A small bowel obstruction; this can occur up to many years later and may require an operation/laparotomy and further bowel resection/removal.
- A leak of urine from the bladder requiring prolonged catheter/tube drainage or even return to theatre.
- Dying of the bowel patch requiring its removal and possibly replacement with another bowel patch at that time or at a later date.
- Failure to give adequate bladder capacity or contractions of the bowel segment or bladder resulting in continuing incontinence. Contractions may require ongoing medical therapy with anticholinergic medication, Imodium or even a second augmentation cystoplasty.
- Development of stress incontinence.
- Vitamin B12 deficiency due to ileum segment removal requiring lifelong Vitamin B12 replacement injections.
- Removal of a bowel segment can result in a change in bowel habit and even chronic diarrheoa in some patients.
- Kidney infections; 11%.
- Urine infections are common but only need treating if symptomatic.
- Mucus production usually reduces over time. Some patients continue to require regular washouts via a catheter to prevent mucus causing infections, stone formation or blockage which could result in bladder rupture.
- Stones requiring surgery to remove occur in up to 50% of patients.
- Metabolic disturbances may require ongoing medication and can cause osteoporosis. Rarely are they severe enough to require removal of the augmentation.
- Bleeding or discomfort passing urine
- Delayed rupture, <5% may be due to mucus blockage, infection, chronic bladder over distension. It requires laparotomy to repair with subsequent increased risk of another rupture.
- Sometimes complete replacement of the augment is required.
- Cancer – rare; 1.5% risk. The average time to cancer is > 20 years. It occurs at the join of the bladder to the bowel. After 10 years a screening cystoscopy is required every 1-2 years for the rest of your life.
Bladder rupture
- This usually results from overfilling of the bladder but could also result from chronic infection or a blow to the lower abdomen.
- The symptoms are abdominal pain, nausea, vomiting or abdominal distension and eventually sepsis.
- Immediate presentation to a hospital emergency department is required.
- Treatment is surgery to repair the rupture. Sometimes replacement of the augment is required.
Your surgeon will discuss any potential complications with you before surgery and you will be able to ask questions. As with any surgery, there are risks with having a general anesthetic. You should have received a copy of our leaflet having an anesthetic which goes into more detail. If you have not, please ask your doctor for one.
Augmentation cystoplasty outcomes
The likelihood of the bladder augmentation surgery working 4:
- 75% of patients have an excellent result
- 20% are improved
- 5% have major ongoing problems
- 13% have incontinence but only half of these require surgery
- 16% chance of needing revision surgery over next 3-5 year.
Urine incontinence
- This occurs in about 13% of patients and is more common at night or if patients don’t catheterize often enough.
- Some patients have stress incontinence as well as urge incontinence. Patients with stress incontinence may require another procedure for this done at the same time as the augmentation cystoplasty or done at a later date.
In addition to accepting the need to catheterize afterwards it essential patients also realize that following this procedure they will need lifelong follow-up and further surgical procedures are often required.
In properly selected patients, augmentation cystoplasty is an excellent procedure that provides a safe and effective way of improving urinary storage. Bladder emptying is almost universally impaired, and the patient must be prepared to perform lifelong intermittent catheterization. The patient and physician must recognize the need for surveillance to identify potential problems. Stones, metabolic and nutritional abnormalities, renal insufficiency, and malignancy are best treated through early recognition and prompt therapy 5.
Herschorn et al 6, using a survey to address complications and patient satisfaction in an augmentation cystoplasty population, found that at a mean of 6 years after surgery, 41% of the patients had 1 or more complications, with 36% of all patients requiring intervention. Most took medications (eg, anticholinergics, antidiarrheals, or antibiotics). Of 59 patients, 56 required clean intermittent catheterization at a mean interval of 4.6 hours; 18% had postoperative bowel dysfunction, and 7% had preoperative dysfunction.
Schlomer et al 7 analyzed 1622 augmentation cytoplaties performed on children between 2000 and 2009. A complication was identified in 30% of patients. Longer hospital stays and increased risk for having complications were associated with older age and bladder exstrophy-epispadias complex diagnosis.
Alternative approaches
McGuire et al 8 compared patients treated with augmentation cystoplasty to patients treated with autoaugmentation and determined that whereas autoaugmentation causes less morbidity, commonly reduces symptoms, and routinely improves bladder compliance, the gains in bladder capacity were much less than those seen with augmentation cystoplasty.
This study 8 stratified patients by etiology of bladder dysfunction and compared urodynamic and symptomatic improvement. Patients with myelomeningocele did not fare as well with autoaugmentation because of the smaller increases in bladder capacity, and augmentation cystoplasty was more beneficial in these patients. Reportedly, autoaugmentation was unsuccessful in 27% of the patients who required augmentation cystoplasty.
Hedican et al 9 used laparoscopy to mobilize the intestine in complex pediatric procedures, including augmentation cystoplasty. They found laparoscopy useful in mobilizing the right colon and in isolating the appendix for a continent catheterizable stoma. A smaller lower-midline or Pfannenstiel incision can be used for surgery on the bladder or for re-establishment of bowel continuity.
Laparoscopic autoaugmentation has also been shown to be technically feasible. Braren and Bishop 10 performed laparoscopic autoaugmentation in 7 pediatric female patients aged 3 months to 15 years; bladder capacity increased 55-95%, all 7 patients showed symptomatic improvement, and 6 of the 7 were completely dry.
With the advent of robotic instruments with increased range of motion and the facilitation of intracorporeal suturing, many reconstructive procedures including bladder augmentation have become more amenable to fully laparoscopic procedures 11. These procedures may decrease morbidity, reduce intra-abdominal adhesions, and improve body self-image.
Will I still need anticholinergic medication afterwards?
This may be required to inhibit bladder contractions or contractions of the bowel patch.
- Dahl DM, McDougal WS. Use of Intestinal Segments in Urinary Diversion. Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA. Campbell-Walsh Urology. 9. Philadelphia, PA: Saunders Elselvier; 2007. Ch. 80.[↩]
- Lapides J, Diokno AC, Silber SJ, Lowe BS. Clean, intermittent self-catheterization in the treatment of urinary tract disease. J Urol. 1972 Mar. 107(3):458-61.[↩]
- Kokorowski PJ, Routh JC, Borer JG, Estrada CR, Bauer SB, Nelson CP. Screening for malignancy after augmentation cystoplasty in children with spina bifida: a decision analysis. J Urol. 2011 Oct. 186(4):1437-43.[↩]
- Flood, H.D., et al., Long-term results and complications using augmentation cystoplasty in reconstructive urology. Neurourol Urodyn, 1995. 14(4): p. 297-309.[↩]
- Gurung PM, Attar KH, Abdul-Rahman A, Morris T, Hamid R, Shah PJ. Long-term outcomes of augmentation ileocystoplasty in patients with spinal cord injury: a minimum of 10 years of follow-up. BJU Int. 2011 Aug 18.[↩]
- Herschorn S, Hewitt RJ. Patient perspective of long-term outcome of augmentation cystoplasty for neurogenic bladder. Urology. 1998 Oct. 52(4):672-8.[↩]
- Schlomer BJ, Saperston K, Baskin L. National trends in augmentation cystoplasty in the 2000s and factors associated with patient outcomes. J Urol. 2013 Oct. 190(4):1352-7.[↩]
- Leng WW, Blalock HJ, Fredriksson WH, English SF, McGuire EJ. Enterocystoplasty or detrusor myectomy? Comparison of indications and outcomes for bladder augmentation. J Urol. 1999 Mar. 161(3):758-63.[↩][↩]
- Hedican SP, Schulam PG, Docimo SG. Laparoscopic assisted reconstructive surgery. J Urol. 1999 Jan. 161(1):267-70.[↩]
- Braren V, Bishop MR. Laparoscopic bladder autoaugmentation in children. Urol Clin North Am. 1998 Aug. 25(3):533-40.[↩]
- Challacombe B, Dasgupta P. Reconstruction of the lower urinary tract by laparoscopic and robotic surgery. Curr Opin Urol. 2007 Nov. 17(6):390-5.[↩]