Delayed hypersensitivity reaction
Delayed hypersensitivity reaction also called type 4 hypersensitivity reaction or cell-mediated hypersensitivity reaction, is inflammatory reaction initiated by T cells (T-lymphocytes) and antigen-presenting cells (such as macrophages and dendritic cells) that cause an inflammatory reaction to either exogenous or autoantigens, which takes more than 12 hours to develop 1. Typically the maximal reaction time occurs between 48 to 72 hours. The term delayed which appears 48-72 hours after antigen exposure is used to differentiate a secondary cellular response from an immediate hypersensitivity response, which generally appears within 12 minutes of an antigen challenge. Delayed hypersensitivity reactions are mediated by by specific subsets of CD4+ helper T cells (Th-1 and Th-17 cells) or by CD8+ cytotoxic T cells and monocytes/macrophages rather than by antibodies. Delayed hypersensitivity reactions are normal physiological events. Anything that alters these normal events can lead to multiple opportunistic infections. delayed hypersensitivity reaction reactions may include, but are not limited to, contact dermatitis (eg, poison ivy rash), tuberculin skin test reactions, granulomatous inflammation (eg, sarcoidosis, Crohn disease), allograft rejection, graft versus host disease, and autoimmune hypersensitivity reactions. Morbidity and mortality vary (eg, ranging from a self-limited rash to chronic debilitating diseases) based on the active disease present.
Delayed hypersensitivity reaction to exogenous antigens involves T cells and also antigen-presenting cells such as macrophages and dendritic cells, all produce cytokines that stimulate a local inflammatory response in a sensitized individual. Delayed hypersensitivity reaction to autoantigens can be seen in type 1 diabetes mellitus, which is an autoimmune disease that results from autoimmune cell-mediated destruction of insulin-secreting pancreatic beta cells. Delayed hypersensitivity reaction cannot be transferred from an animal to another by mean of antibodies or serum. However, it can be transferred by T cells, particularly CD4 Th1 cells but it is progressively lost in individuals with HIV/AIDS. Antigen-presenting cells such as Langerhans cells engulf process and present antigens to antigen-specific T cells that become sensitized. Cytokines produced by keratinocytes, antigen-presenting cells and T cells recruit antigen-nonspecific T cells and macrophages to participate in a local inflammatory reaction 2.
There are three variants of delayed hypersensitivity as listed below. The three types of delayed hypersensitivity reaction can distinguish one to another according to the skin reactivity they produce once antigens applied epicutaneously or intradermally. The magnitude of the reaction can be assessed in animals by measuring the thickening of the skin, which is local but also systemic such as cytokine synthesis and T-cell division.
- Contact hypersensitivity reaction (48 to 72 hours). In contact dermatitis, small antigens called haptens penetrate the skin and combine with tissue protein and mediate immune reactions. Langerhans cells are the principal antigen-presenting cells involved in recognition of hapten-tissue protein complexes and their presentation to T cells. Also, keratinocytes, which express MHC class II molecules and intercellular adhesion molecule-1 (ICAM-1), make a group of cytokines including IL-1, IL-6, IL-8 among others that help in the establishment of the contact hypersensitivity response 3.
- Tuberculin hypersensitivity reaction (48 to 72 hours). Tuberculin-type hypersensitivity, initially described by Koch, occurs in patients with tuberculosis (TB) or those vaccinated against tuberculosis when they are injected subcutaneously with tuberculin (a product derived from the tubercle bacillus). They react with skin induration, swelling, and redness 4. Other antigens from several pathogens can cause a similar reaction in sensitized individuals including antigens from Leishmania tropica and Mycobacterium leprae.
- Granulomatous hypersensitivity reaction (21 to 28 days). Granulomatous-type hypersensitivity results from the persistence within macrophages of intracellular pathogens or other substances that the cell is unable to process or destroy. It occurs to a variety of antigens including beryllium, talc, silica among other, where macrophages are unable to digest them. In allergic alveolitis, the antigen-presenting cell is unable to process and assimilate the immune complexes, and granuloma develop. Another disease is sarcoidosis, where the antigen is unknown but leads to granuloma formation 5.
Delayed hypersensitivity is a major mechanism of defense against various intracellular pathogens, including mycobacteria, fungi, and certain parasites, and it occurs in transplant rejection and tumor immunity. The central role of CD4+ T cells in delayed hypersensitivity is illustrated in patients with AIDS. Because of the loss of CD4+ cells, the host response against intracellular pathogens such as Mycobacterium tuberculosis is markedly impaired. The bacteria are engulfed by macrophages but are not killed.
If CD4 T-cell function is abnormal, the patient presents with opportunistic infections, including infection with mycobacteria, fungi, parasites, and, often, mucocutaneous candidiasis 6. Undesirable consequences of delayed-type hypersensitivity reactions include illness such as contact dermatitis and allograft rejection. Examples of delayed hypersensitivity reaction are contact dermatitis (eg, poison ivy rash), tuberculin skin test reactions, granulomatous inflammation (eg, sarcoidosis, Crohn disease), allograft rejection, graft versus host disease, and autoimmune hypersensitivity reactions 7. Of note, the Rhus genus of plants, which includes poison ivy, poison oak, and poison sumac, all cause identical rashes.
Delayed hypersensitivity reaction causes
Delayed hypersensitivity reactions are normal physiological events. Anything that alters these normal events can lead to multiple opportunistic infections. Immune deficiencies (congenital or acquired) and immunosuppressive agents can alter this normal response. Some drugs can also cause delayed hypersensitivity reactions or type 4 hypersensitivity reactions. Allopurinol and lamotrigine have a risk of developing delayed hypersensitivity reactions at higher doses.
Mechanism of delayed hypersensitivity reaction
The cellular events that result in delayed hypersensitivity reactions or type 4 hypersensitivity reaction (cell mediated hypersensitivity reaction), primarily involve T-cells and macrophages. First, local immune and inflammatory responses at the site of foreign antigen up-regulate endothelial cell adhesion molecule expression, promoting the accumulation of leukocytes at the tissue site. The antigens involved may be either intracellular pathogens such as Mycobacterium tuberculosis, Listeria monocytogens, Histoplasma capsulatum, Herpes Simplex virus etc. or contact antigens such as Nickel salts, Poison ivy etc. The antigen is engulfed by macrophages and monocytes and is processed and presented to a T-cell that has a specific receptor for that processed antigen. Macrophages secrete interleukin (IL)–1, IL-2, IL-6, and other lymphokines. Cytotoxic T cells can also be activated. Antigen-presenting cells stimulated by T cells are unable to digest the antigens, and they become giant multinucleated cells. In this process, many cytokines are produced, and the most important are TNF-alpha and beta, IL-2, and GM-CSF. The characteristic histologic appearance of the macrophage–T-cell infiltrate is a granuloma. This type of infiltrate in the tissue is called granulomatous inflammation. The presence of granuloma characterizes the delayed hypersensitivity reactions. Diseases caused by delayed hypersensitivity reactions tend to be chronic. Some of them are leprosy, tuberculosis (TB), schistosomiasis, sarcoidosis and Crohn’s disease. A chemical irritant can apply to the epidermis and may result in over-expression of ELAM-1, VCAM-1, and ICAM-1 which mediate inflammatory reactions consistent with a delayed hypersensitivity reaction 8.
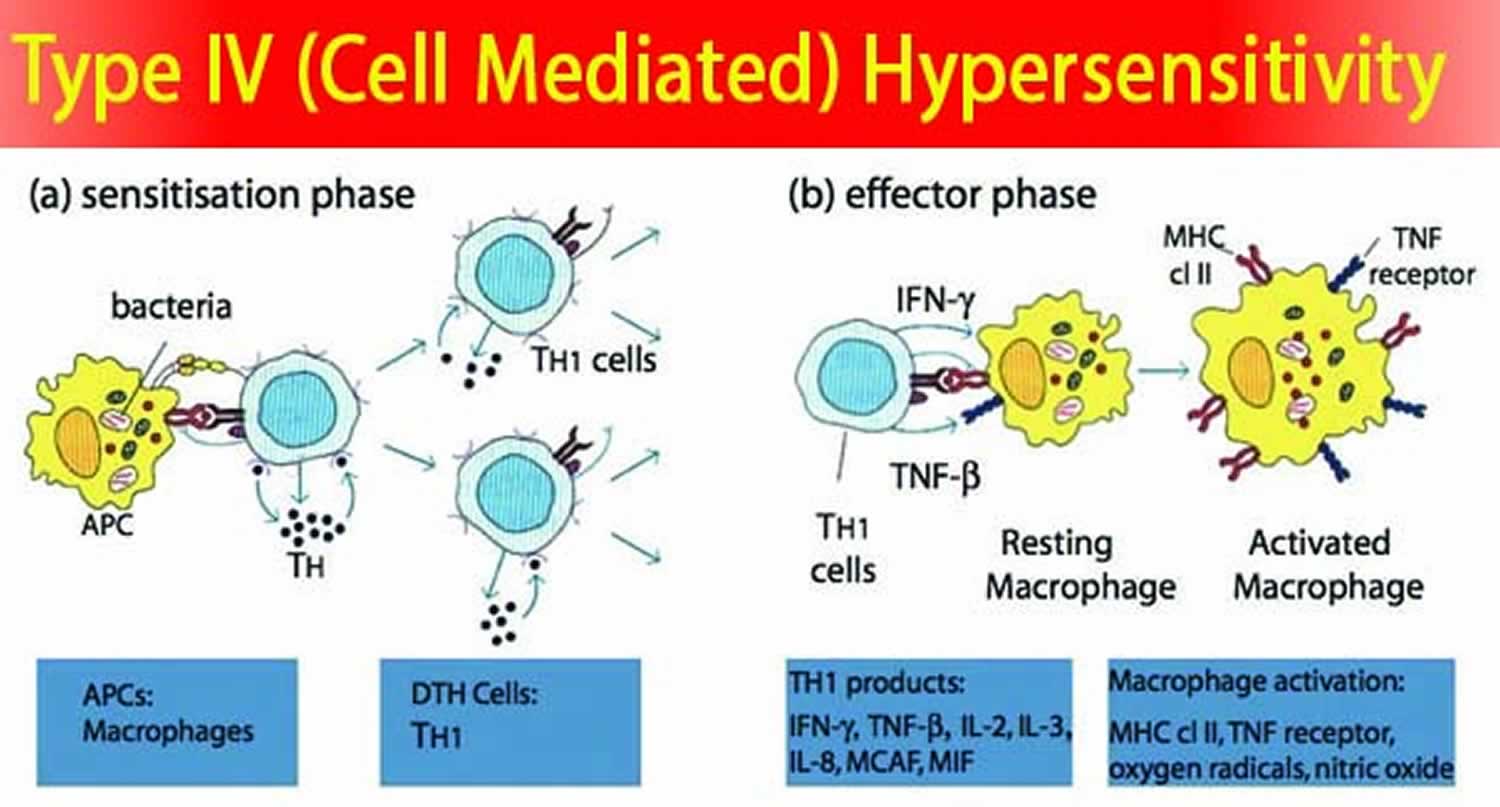
Delayed hypersensitivity reaction is accomplished in two phases: the initial sensitization phase and the later effector phase.
- In the sensitization phase, the primary contact with the antigen is established. During this period, specific Th cells are sensitized and are clonally expanded.
- In the effector phase, a subsequent exposure to the same antigen induces the delayed type hypersensitivity response.
In contact hypersensitivity reactions, there are mononuclear cells infiltrates present in both dermis and epidermis. The last one is pushed outward, and a microvesicle forms within it as a consequence of the edema developed.
In tuberculin-type hypersensitivity reactions, histologically there is a dense dermal infiltrate of leukocytes visualized with Hematoxylin and Eosin (H and E) stain. There is also marked caseation and necrosis within the granuloma.
In granulomatous-type hypersensitivity reactions, histology shows a typical epithelioid-cell granuloma. Also, giant cells are visible in the center of the lesion, which is surrounded by a cuff of lymphocytes. The reaction is due to the persistence of the mycobacterial antigen. Mature tissue macrophages can surround the granuloma and are visualized by antibody staining techniques 9.
Delayed hypersensitivity reaction symptoms
The clinical history of delayed hypersensitivity reactions differs depending on the cause. Delayed hypersensitivity diseases can develop in humans due to mycobacteria, protozoa, and fungi, although in another granulomatous disease such as Crohn’s disease, no infectious microbes have been found. Some of the most critical diseases include leprosy, tuberculosis, schistosomiasis, sarcoidosis and Crohn’s disease 10. The inability to mount an adequate delayed hypersensitivity response results in a poor outcome in diseases such as leprosy and tuberculosis.
Leprosy
Leprosy is divided clinically into three essential types: tuberculoid, borderline, and lepromatous. In tuberculoid leprosy, the affected skin has a few, well-defined, hypopigmented patches that show epithelioid infiltrate with no microorganisms. In lepromatous shows, multiple confluent skin lesions characterized by numerous bacilli. Borderline leprosy shows physical findings of the two anterior.
Tuberculosis
Tuberculosis in the lungs causes a granulomatous reaction that leads to cavitation and the spread of bacteria. There are extensive areas of fibrosis that can see in the chest x-ray. This lesion is typically granulomatous.
Schistosomiasis
Schistosomiasis causes by schistosomes, once the body is sensitized by a granulomatous reaction developed in the parasitized tissue mediated by Th2 lymphocytes.
Sarcoidosis
Sarcoidosis is a chronic and idiopathic disease in which activated macrophage and granuloma accumulate in many tissues along with fibrosis. The condition can be characterized by the presence of enlarged lymph nodes, which may be identified in chest radiographs. This disease is associated with depression of cell-mediated immunity both in vivo and in vitro. A tuberculin test is negative in this disease. The clinical manifestations include granuloma development in the lungs, lymph nodes, nervous system, bones, and skin and are associated with fever, malaise, and shortness of breath due to lung fibrosis.
Crohn’s disease
Crohn’s disease is another granulomatous disease that is not caused by a microorganism. Granulomas are prominent. It is a chronic disease that affects ileum and colon, and where T-helper cells and antigen-presenting cells accumulate in all layers of the intestines.
Contact hypersensitivity (ie, allergic contact dermatitis). Patients often report being in wooded areas or having made contact with poison ivy or poison oak, which caused a rash, itching, or both. The exposure occurs 48-72 hours before the development of symptoms.
Tuberculin hypersensitivity reactions
Many times during a routine health screening, patients have a positive Mantoux test result and are asymptomatic. In these cases, patients may recall being exposed to someone with TB or with a chronic cough. In many cases, patients do not recall a possible exposure.
The Mantoux test itself is a delayed hypersensitivity reaction 11. Thus, 48-72 hours following the intradermal administration of purified M tuberculosis protein derivative, patients who have been exposed to the bacteria develop a delayed hypersensitivity reaction manifested by inflammation and edema in the dermis 12. A positive Mantoux test is the result of the recruitment of several types of mononuclear leukocytes and the release of several cytokines that promote the delayed hypersensitivity reaction inflammatory reaction. Measurement by the QuantiFERON test of interferon production by peripheral blood mononuclear cells has been used as an in vitro surrogate for the Mantoux test.
The physical examination findings can be normal, or they can reveal the signs and symptoms of the specific disease.
- Contact hypersensitivity reactions: Examination usually reveals edematous and erythematous epidermal tissue with microvesicles. If the offending antigen is from the Rhus genus of plants, the involved area usually appears in a linear fashion. If the offending antigen is nickel (eg, jewelry), then the involved area is oriented in a fashion consistent with the area of contact. Long-term nickel exposure results in an eczematous dermatitis with lichenification of the skin.
- Tuberculin hypersensitivity reactions: Approximately 48-72 hours following the intradermal administration of purified Mycobacterium tuberculosis protein, patients who have been sensitized to Mycobacterium tuberculosis by previous exposure develop an area of erythema and induration.
- Granulomatous hypersensitivity reactions: The physical examination findings differ depending on the underlying disease. For example, if the patient has active tuberculosis (TB), then a chronic cough, malaise, night sweats, weight loss, and pyrexia are present.
Other diseases that can include among delayed hypersensitivity reactions or type 4 hypersensitivity reactions:
- Autoimmune myocarditis
- Type 1 diabetes mellitus
- Peripheral neuropathies
- Hashimoto’s thyroiditis
- Multiple sclerosis
- Rheumatoid arthritis
In all of them, Th1 cells play a role in responding to autologous antigens leading to autoimmune disease and inflammation.
Delayed hypersensitivity reaction complications
Complications of Tuberculosis
- Back pain and stiffness
- Tuberculous arthritis
- Heart, liver, and kidney diseases
- Meningitis
Complications of Leprosy without treatment
- Permanent damage to skin, nerves, nose, and limbs
- Claw-like hands
- Nosebleeds
Complications of Schistosomiasis
- Gastrointestinal (GI) bleeding and obstruction
- Nephropathy
- Hematuria
- Hemospermia
Complications of Sarcoidosis
- Pneumonia
- Eye problems (cataracts, glaucoma, and blindness)
- Kidney failure
- Neurosarcoidosis (bilateral facial palsy)
- Hypercalcemia
Complications of Crohn’s disease
- Obstruction of the small intestine or colon
- Intestine perforation
- Intestinal abscesses and fistulae
- Intestinal bleeding
Delayed hypersensitivity reaction diagnosis
Delayed hypersensitivity reactions can be diagnosed by skin test of delayed hypersensitivity using antigens and confirmed by history and clinical presentation. For example, the tuberculin test in a patient with pulmonary tuberculosis can give an overwhelming reaction, but this would not occur in a patient with sarcoidosis. A patient should be tested with an array of allergens to prove which of them is causing the problem. The culture of microorganisms can be useful in demonstrating the cause of the delayed hypersensitivity disorder, especially for tuberculosis (sputum culture). Histopathology can be of chief importance in making a diagnosis of a delayed hypersensitivity reaction or disease. The suspected tissue can be biopsied to prove the nature of the disease and treated accordingly. Immunological testing should be carried out routinely and include complete blood cell count (CBC), T-cell subpopulation, radioallergosorbent test (RAST) and other test include serology, chest x-ray, body radiographs, and also diagnostic ultrasound and CT scan 13.
Delayed hypersensitivity reaction treatment
Treatment of delayed hypersensitivity reactions or type 4 hypersensitivity reactions involves treatment of the elicitating cause 13.
The treatment of contact dermatitis varies depending on the severity of the disease. The best advice is to avoid the offending antigen. Pharmaceutical treatment varies, including over-the-counter corticosteroid preparations, prescription corticosteroid preparations, injectable corticosteroids, oral corticosteroids, and Burow solution.
Tuberculin hypersensitivity skin reactions treatment is rarely needed, because this response is usually short-lived and self-limited. Topical corticosteroid preparations can be applied as needed. On rare occasions, the reaction to a delayed hypersensitivity skin test may be extreme and result in axillary lymphadenopathy and fever. Such reactions are self-limited and may be treated with an antipyretic medication such as aspirin or ibuprofen.
The most common drugs to treat tuberculosis include isoniazid, rifampin, ethambutol, and pyrazinamide. For drug-resistant TB (tuberculosis), a combination of antibiotics such as amikacin, kanamycin, or capreomycin for 20 to 30 months should be used.
The most common drugs to treat leprosy include rifampicin and clofazimine in combination with dapsone for multibacillary leprosy. A single dose of antimicrobial combination to cure single lesion paucibacillary leprosy comprises ofloxacin (400 mg), rifampicin (600 mg), and minocycline (100 mg).
Praziquantel can be useful for treating infections caused by all Schistosoma species.
Hydroxychloroquine and chloroquine can use in the therapy of sarcoidosis involving the skin, lungs, and the nervous system.
The use of anti-TNF monoclonal antibodies such as adalimumab and certolizumab have been approved for Crohn’s disease.
Delayed hypersensitivity reaction prognosis
The prognosis of tuberculosis is better if the disease can diagnose and promptly treat with the antimicrobials. Leprosy can also be a curable disease, but it depends on the stage of this disease and patient compliance with multidrug therapy (MDT). Some skin lesions may persist after treatment. Schistosomiasis is associated with high morbidity both as acute and chronic illness. The prognosis of sarcoidosis is guarded, and the overall death rate is less than 7%. Some patients may require treatment if a complication such as pneumonia and nephropathy develops. Crohn’s disease has a reserved prognosis; it cannot be cured.
- Justiz Vaillant AA, Zulfiqar H, Ramphul K. Delayed Hypersensitivity Reactions. [Updated 2019 Jun 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519023[↩]
- Barailler H, Milpied B, Chauvel A, Claraz P, Taïeb A, Seneschal J, Darrigade AS. Delayed hypersensitivity skin reaction to hydroxychloroquine: Successful short desensitization. J Allergy Clin Immunol Pract. 2019 Jan;7(1):307-308.[↩]
- Mahler V, Geier J, Schnuch A. Current trends in patch testing – new data from the German Contact Dermatitis Research Group (DKG) and the Information Network of Departments of Dermatology (IVDK). J Dtsch Dermatol Ges. 2014 Jul;12(7):583-92.[↩]
- Pelzer PT, Mutayoba B, Cobelens FGJ. BCG vaccination protects against infection with Mycobacterium tuberculosis ascertained by tuberculin skin testing. J. Infect. 2018 Oct;77(4):335-340.[↩]
- Thangaraju P, Venkatesan S. Leprosy in Children: Needs for Active Intervention. Chin. Med. J. 2018 Jun 05;131(11):1385.[↩]
- Malajian D, Belsito DV. Cutaneous delayed-type hypersensitivity in patients with atopic dermatitis. J Am Acad Dermatol. 2013 Apr 11.[↩]
- Delayed Hypersensitivity Reactions. https://emedicine.medscape.com/article/136118-overview[↩]
- Galvan-Blasco P, Guilarte M, Cardona V, Labrador-Horrillo M, Sala-Cunill A, Gil-Serrano IJ, Luengo O. Delayed drug hypersensitivity to bortezomib: Desensitization and tolerance to its analogue carfilzomib. Allergy. 2019 Feb 09.[↩]
- Gong W, Huang F, Sun L, Yu A, Zhang X, Xu Y, Shen Y, Cao J. Toll-like receptor-2 regulates macrophage polarization induced by excretory-secretory antigens from Schistosoma japonicum eggs and promotes liver pathology in murine schistosomiasis. PLoS Negl Trop Dis. 2018 Dec;12(12):e0007000[↩]
- Tedijanto C, Hermans S, Cobelens F, Wood R, Andrews JR. Drivers of Seasonal Variation in Tuberculosis Incidence: Insights from a Systematic Review and Mathematical Model. Epidemiology. 2018 Nov;29(6):857-866.[↩]
- Bansal R, Sharma PK. Exaggerated Mantoux reaction in a case of latent tuberculosis infection (LTBI). Indian J Tuberc. 2012 Jul. 59(3):171-3.[↩]
- Facktor MA, Bernstein RA, Fireman P. Hypersensitivity to tetanus toxoid. J Allergy Clin Immunol. 1973 Jul. 52(1):1-12.[↩]
- Wen WL, Tsai KB, Lin YH, Hwang SJ, Hsiao PJ, Shin SJ, Hung WW. Successful management of type IV hypersensitivity reactions to human insulin analogue with injecting mixtures of biphasic insulin aspart and dexamethasone. J. Formos. Med. Assoc. 2019 Apr;118(4):843-848.[↩][↩]