Drop attacks
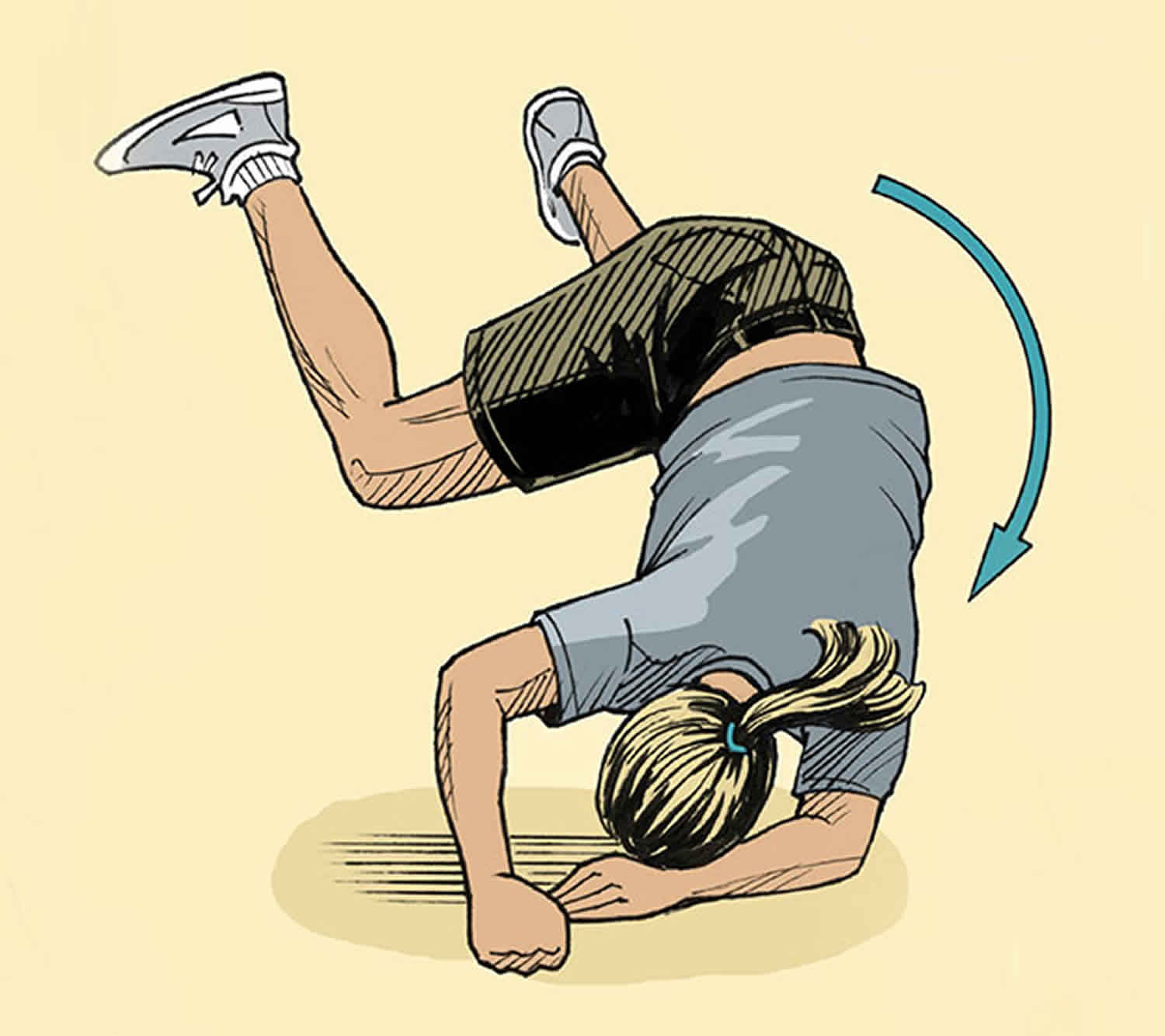
Drop attacks is the medical term for sudden falls to the ground without prodromes, trigger factors (not precipitated by a specific stimulus) or without loss of consciousness (blackout) and with instantaneous recovery to baseline status 1. Drop attack occurs while the patient is standing or walking and comes on abruptly, without warning, and are followed by a rapid return to baseline 2. The patient literally drops to the ground because of the sudden loss of muscle strength. Once fallen, the patient is usually able to get up immediately by himself and continue with his previous activity, with no visible residual of the attack 3. Characteristically, the patient remains fully conscious throughout this experience. Since vision, hearing, and speech remain intact, the patient is surethat there was no alteration of consciousness. Drop attacks are frightening and often lead to injuries, if a person was standing she/he often falls, usually forwards, and may injure the front of their head or face, knees and forearms.
Drop attacks key points 2:
- Drop attacks are sudden falls without loss of consciousness that are not precipitated by a specific stimulus, occur with abrupt onset and without warning, and are followed by a rapid return to baseline.
- The term “drop attack” has subsequently been used to encompass a wide variety of sudden falls with or without existing conditions known to increase the risk of falls, with or without provocation by a specific stimulus, with or without loss of consciousness, and with or without significant baseline abnormalities.
- A range of localizations for drop attacks is possible, but most commonly lower brainstem or spinal cord structures are implicated.
- Drop attacks generally indicate transient impairment of bilateral central nervous system structures involved in maintenance of postural muscle tone and balance.
- Tumarkin otolithic catastrophes (or crises) are drop attacks without associated autonomic or neurologic symptoms in patients with severe vestibular disease, usually due to Meniere’s disease.
People with drop attacks often experience the following:
- A drop attack is a sudden fall to the ground while standing or walking.
- There is usually no specific trigger although some patients do report drop attacks being more likely in certain situations, especially the tops of stairs and busy places like supermarkets. This may be something to do with ‘sensory overload’ that some people get in these situations.
- Patients with functional drop attacks normally can’t remember the fall itself but are aware of the impact on the ground (or within seconds of falling). This is different to a mechanical fall when people often do remember the fall (often in detail). Its also different to a dissociative attack (non-epileptic attack) where there is an actual ‘blackout’.
- Unlike an epileptic seizure or a faint, people with drop attacks can usually get up again quite quickly.
- Injury is a common consequence of drop attacks. In France the condition has been called ‘maladies de genius bleus’ (sickness of the blue knees) because patients with drop attacks so often fall down on their knees, bruising them in the process. Other common injuries include wrist and hand injuries as well as facial injuries. When drop attacks are witnessed, its often noticed that the person just crumples down to the ground rather than toppling over (like a faint)
- Its only natural when you’ve had some unexpected falls that you will worry about going outside. Not only can it be painful to fall down so unexpectedly but many patients report embarrassment, especially when others come to their aid. As with any other cause of sudden ‘attack, people with drop attacks often develop a fear of going outside on their own. This may be important to recognize as part of treatment
“Drop attacks”, first described by Tumarkin in 1936 as “otolithic catastrophe” 4, are characterized by a sudden falling to the ground without loss of consciousness 5. Otolithic crises, also defined as Tumarkin crisis, are abrupt attacks of falling, without loss of consciousness. The attacks last a few seconds. According to Janzen and Russell, Tumarkin himself proposed that the cause was due to otolithic malfunction 6. Usually, drop attack patients have no warning of an attack and know immediately where they are after hitting the ground. Initially these events were described in otherwise healthy elderly people 7, but the term “drop attack” has subsequently been used to encompass a wide variety of sudden falls with or without existing conditions known to increase the risk of falls, with or without provocation by a specific stimulus, with or without loss of consciousness, and with or without significant baseline abnormalities. Diagnosis of drop attack is not always very easy; in typical cases, there is no doubt, in fact, patients usually describe a feeling of being “thrown to the ground” by a force. Since sensorium is preserved, syncope can be excluded. Albeit, in the presence of drop attack, cardiac and neurological causes must be ruled out. The fear of falling, caused by drop attacks, is an important cause of handicap in Meniere’s disease patients; in fact, patients with drop attacks are more dependent on visual and proprioceptive information 8. Moreover, they tend to limit their activity and change their life-style.
Drop attacks are thought to be caused by a sudden shift of otolithic maculae or by a rupture of the peri-lymph/endo-lymph balance. Another explanation is a possible mechanical deformation of the otolith organ which leads to activation of vestibulo-spinal reflexes 9. Drop attacks are more frequent in the late period of Meniere’s disease 10, even if they can also occur in the earlier stages. Black 10 postulated that erroneous information from otolithic maculae cause an incorrect alignment of the body axis relative to vertical gravity; thus the center of gravity is moved outside the platform provided by the feet and consequently the patient falls to the ground 10.
As already mentioned, Meniere’s disease involves the whole inner ear; when the lateral canal is destroyed and the patient still complains of dizziness and vertigo, it is tempting to suspect that the latter are caused by the remaining function in vertical canals and otolithic organ 11. Unfortunately, it is difficult to confirm this condition due to the lack of specific tests and to the difficulty in examining the patient during a drop attack. Undoubtedly, for drop attacks to develop, some vestibular function must be preserved 10.
The incidence of drop attack is unknown, even if some authors have estimated that the attacks occur in about 6% of Meniere’s disease patients 10 Others have reported similar values 12, while others report very high values 8. This difference is possibly due to different diagnostic criteria.
Spontaneous resolution of drop attacks is common but, in severe cases, aggressive treatment is necessary. Drop attacks secondary to otologic causes must be recognized because, in severe cases, ablative surgery is curative 10.
What is the risk of stroke or death in persons with drop attacks?
The stroke rate in persons with drop attacks is 0.5%/year. This rate is not significantly different than the general population 13.
Persons with drop attacks have far more fractures than the general population 13.
Drop attacks causes
There are many causes of drop attacks, and many neurologic and non-neurologic causes. Symptomatic drop attacks causes include simple falls, low blood pressure (hypotension), cataplexy 14, epilepsy (atonic seizure – where the person’s muscles suddenly relax and they become floppy) 15, leg weakness, sudden falls in parkinsonian syndromes including those due to freezing, transient ischemic attacks (TIAs), epilepsy, myoclonus, startle reactions (hyperekplexia), paroxysmal dyskinesias, structural central nervous system lesions, and hydrocephalus 16. Syncope and cardiovascular disease account for non-neurologic causes. About 12% are due to the heart (a variant of syncope), 8% due to poor circulation to the brain, 8% due to problems with both the heart and brain, 7% due to seizures, 5% due to the inner ear (Menieres disease — called the otolithic crisis of Tumarkin), and 1%, due to psychological problems. Rarely, drop attacks are exaggerated startle reactions. Idiopathic drop attacks usually appear between the ages of 40 and 59 years, the prevalence increasing with advancing age (Stevens and Matthews, 1973), and are a common cause of falls and fractures in elderly people 7. In the majority (64%) of drop attack cases, the cause of drop attacks is not clearly established 17.
Drop attacks from Meniere’s disease are more “active” — the person involved actually ends up participating in the fall (because they feel as if they are flipped). Most other drop attacks are slower and are more of a “collapse” than an actively driven fall. The mechanism for drop attacks in Meniere’s disease is likely a “popping” of a dimpled inner ear membrane as pressure changes in the ear 18. Saccule testing such as the vestibular evoked myogenic potential (VEMP) is reported to be abnormal in this situation, but the unusual type of vestibular evoked myogenic potential required is not one that is commonly encountered in clinical laboratories 19.
More dubious causes of drop attacks:
There are a number of “one off” reports of entities within the ventricles such as colloid cysts 20, and choroid plexus cysts 21. These are diagnosed with MRI scans.
Extremely unusual situations include chorea 22, rare genetic disorders 23.
There are occasional patients with Chiari who reportedly have drop attacks 24.
A small number of drop attacks may be due to superior canal dehiscence syndrome 25. It is difficult to see how superior canal dehiscence syndrome could cause an abrupt drop attack. Superior canal dehiscence syndrome is diagnosed with a vestibular evoked myogenic potential (VEMP) and a CT scan of the temporal bone (if the vestibular evoked myogenic potential is abnormal).
Rare patients fall due to cataplexy 26. Cataplexy is another cause of symptomatic drop attacks that does not fit the categories listed previously. Patients with cataplexy fall suddenly without loss of consciousness but with inability to speak during an attack. There is a precipitating trigger, usually laughter or a sudden emotional stimulus. The patient’s muscle tone is flaccid and remains this way for many seconds. Cataplexy is a variant of narcolepsy. Cataplexy is usually just one feature of the narcolepsy syndrome; other features include sleep paralysis and hypnagogic hallucinations, in addition to the characteristic feature of sudden, uncontrollable falling asleep. Narcolepsy is diagnosed with a sleep study and the multiple sleep latency test. Some experts think this is roughly 1/100’th as common as Meniere’s disease drop attacks.
Vives-Rodriguez 27 reported drop attacks in a case of “LG11 encephalitus”. This is a “super zebra”.
Drop attacks are reported in Migraine 28 which of course can cause nearly any neurologic symptom reported in the literature as well.
Drop attacks diagnosis
Basically this narrows down to heart, brain, ear, and psychological problems.
- Drop attacks due to cardiac disorders are similar to brief fainting episodes. They are best diagnosed with “ambulatory event monitoring”. These people don’t actively fall, they slump to the ground.
- Drop attacks due to seizures and related problems are diagnosed with EEG test and its variants. Drop attacks due to sudden loss of postural tone. This is called “negative myoclonus” 29, and is a variant of the seizure type of drop attack.
- Drop attacks due to Meniere’s disease, also called “Otolithic Crises of Tumarkin”, are diagnosed with an audiogram, ECOG and ENG. These people actively fall.
- Drop attacks due to psychological problems are very difficult to confirm but sometimes this can be established via inpatient EEG monitoring. Here, any pattern is possible, but generally people do not do self-harm. I.e. no broken bones.
Drop attacks treatment
Drop attacks are very serious as they often result in falls and breakage of bones. Treatment is individualized according to the diagnosis of the underlying cause. Because in many instances, no diagnosis is established, no treatment may be advocated.
Drop Attack most effective treatment:
- Cardiac disorders: Medication or pacemaker
- Seizures: Anticonvulsant
- Meniere’s disease: Surgery or medication to destroy labyrinth (especially low dose gentamicin)
Treatment of drop attacks in Meniere’s disease is still controversial 5. Janzen et al. 6 suggest conservative management in a drop attack patient with Meniere’s disease, on account of the high rate of spontaneous resolution. In their opinion, surgery is indicated when drop attacks in Meniere’s disease become incapacitating, due to frequency, or severely affect the patient’s life style 6. Other authors suggest a first line treatment with drugs (diuretics, etc.); in disabling cases, surgery or gentamicin treatment are further options 30. Vestibular ablation is highly efficacious for controlling disabling vertigo or falls secondary to Meniere’s disease 31. Trans-tympanic gentamicin is an effective alternative in such cases 12; good control of drop attacks has been reported in only about 60% of patients with drop attack 32. Surgical treatment (labyrinthectomy or nerve section) can be effective also in older patients with Meniere’s disease; it has been reported that the elderly show good compensation after ablative surgery 33. Shunt procedures seem to be less effective in Meniere’s disease drop attack patients 10. It should be borne in mind that, in older patients, co-morbidity plays an important role in the compensation mechanism. The older the patient, the more important the continuation of exercises for months/years after treatment. Another golden rule is that in older patients with drop attacks, the search for a possible cause rather than Meniere’s disease, must to be performed very carefully.
- Lladó AC, Malheiro R, Estriga AR. Drop attacks: an unexpected diagnosis. BMJ Case Rep. 2014;2014:bcr2013202551. Published 2014 Mar 14. doi:10.1136/bcr-2013-202551 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3962866[↩]
- Drop attacks. https://www.medlink.com/article/drop_attacks[↩][↩]
- KUBALA MJ, MILLIKAN CH. Diagnosis, Pathogenesis, and Treatment of “Drop Attacks”. Arch Neurol. 1964;11(2):107–113. doi:10.1001/archneur.1964.00460200003001[↩]
- Tumarkin A. The otolith catastrophe: a new syndrome. BMJ 1936;1:175-7.[↩]
- Dallan I, Bruschini L, Nacci A, Bignami M, Casani AP. Drop attacks and vertical vertigo after transtympanic gentamicin: diagnosis and management. Acta Otorhinolaryngol Ital. 2005;25(6):370–373. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2639899[↩][↩]
- Janzen V, Russell R. Conservative management of Tumarkin’s otolithic crisis. J Otolaryngol 1988;7:359-61.[↩][↩][↩]
- Sheldon JH. On the natural history of falls in old age. BMJ 1960:2;1685-90[↩][↩]
- Kentala E, Havia M, Pyykko I. Short-lasting drop attacks in Meniere’s disease. Otolaryngol Head Neck Surg 2001;124:526-30.[↩][↩]
- Ishiyama G, Ishiyama A, Jacobson K, Baloh RW. Drop attacks in older patients secondary to an otologic cause. Neurology 2001;57:1103-6[↩]
- Black FO, Effrom M, Burns D. Diagnosis and management of drop attacks of vestibular origin: Tumarkin’s otolithic crisis. Otolaryngol Head Neck Surg 1982;90:256-62.[↩][↩][↩][↩][↩][↩][↩]
- Bergenius J, Odkvist LM. Transtympanic aminoglycoside treatment of Meniere’s Disease. In: Baloh RW, Halmagyi JM, editors. Disorders of the Vestibular System. New York, NY: Oxford University Press; 1996. p. 575.[↩]
- Baloh RW, Jacobson K, Winder T. Drop attacks with Meniere’s syndrome. Ann Neurol 1990;28:384-7.[↩]
- Drop Attacks. https://www.dizziness-and-balance.com/disorders/central/drop.html[↩][↩]
- Egel RT, Lee A, Bump T, Javois A. Isolated cataplexy in the differential diagnosis of drop attacks: a case of successful clinical diagnosis and treatment. Case Rep Neurol Med. 2012;2012:757586. doi:10.1155/2012/757586 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3420411[↩]
- Atonic Seizures. https://www.epilepsy.com/learn/types-seizures/atonic-seizures[↩]
- Clinical overview and phenomenology of movement disorders. Principles and Practice of Movement Disorders 2nd Edition, 2011. ISBN 978-1-4377-2369-4 https://doi.org/10.1016/C2009-0-44357-5[↩]
- Meissner I, Wiebers DO, Swanson JW, O’Fallon WM. The natural history of drop attacks. Neurology. 1986;36(8):1029–1034.[↩]
- Ozeki, H., et al. (2008). “Vestibular drop attack secondary to Meniere’s disease results from unstable otolithic function.” Acta Otolaryngol 128(8): 887-891.[↩]
- Timmer, F. C., et al. (2006). “Vestibular evoked myogenic potential (VEMP) in patients with Meniere’s disease with drop attacks.” Laryngoscope 116(5): 776-779.[↩]
- Zohrevandi, B., et al. (2015). “Third Ventricle Colloid Cyst as a Cause of Sudden Drop Attacks of a 13-Year-Old Boy.” Emerg (Tehran) 3(4): 162-164.[↩]
- Bansal, A., et al. (2015). “Lateral ventricular cystic choroid plexus papilloma presenting with recurrent drop attacks: A rare manifestation of a rare variant.” Neurol India 63(4): 619-621.[↩]
- Rosati, A., et al. (2015). “Recurrent drop attacks in early childhood as presenting symptom of benign hereditary chorea caused by TITF1 gene mutations.” Dev Med Child Neurol 57(8): 777-779.[↩]
- Toelle, S. P., et al. (2014). “Sensory stimulus-sensitive drop attacks and basal ganglia calcification: new findings in a patient with FOLR1 deficiency.” Epileptic Disord 16(1): 88-92.[↩]
- Straus, D., et al. (2009). “Chiari drop attacks: surgical decompression and the role of tilt table testing.” Pediatr Neurosurg 45(5): 384-389.[↩]
- Brandtberg K, Ishiyama A, Baloh RW. Drop attacks secondary to superior canal dehiscence syndrome. Neurology 2005:64:2126-2128[↩]
- Egel, R. T., et al. (2012). “Isolated cataplexy in the differential diagnosis of drop attacks: a case of successful clinical diagnosis and treatment.” Case Rep Neurol Med 2012: 757586.[↩]
- Vives-Rodriguqes et al. Drop attacks: A clinical manifestation of LG11 encephalitus. Neurology Clinical Practice, 2017, 440-442[↩]
- Ishiyama, G., et al. (2003). “Drop attacks and vertigo secondary to a non-meniere otologic cause.” Arch Neurol 60(1): 71-75.[↩]
- Rubboli G et al. Negative myoclonus: an overview of its clinical features, pathophysiological mechanisms and management. Neurophysiol Clin Neurophysiol 2006:36:337-343[↩]
- Odkvist LM, Bergenius J. Drop attacks in Meniere’s disease. Acta Otolaryngol 1988(Suppl);455:82-5.[↩]
- Ishiyama G, Ishiyama A, Jacobson K, Baloh RW. Drop attacks in older patients secondary to an otologic cause. Neurology 2001;57:1103-6.[↩]
- Kaasinen S, Pyykko I, Ishizaki H, Aalto H. Intratympanic gentamicin in Meniere’s Disease. Acta Otolaryngol (Stockh) 1995;118:294-8.[↩]
- Langman AW, Lindeman RC. Surgical labyrinthectomy in the older patient. Otolaryngol Head Neck Surg 1998;118:739-42.[↩]