Enterobiasis
Enterobiasis also known as pinworm infection, is caused by a small, thin, white roundworm called Enterobius vermicularis, which is also known as the human pinworm due to the female’s long, pointed tail. Another putative pinworm species, Enterobius gregorii, has been described and reported from humans in Europe, Africa, and Asia. However, further morphologic and molecular evidence suggests Enterobius gregorii likely represents an immature form of Enterobius vermicularis. The rat pinworm, Syphacia obvelata, has also very rarely been reported infecting humans. Although pinworm infection can affect all people, it most commonly occurs among children, institutionalized persons, and household members of persons with pinworm infection. Enterobiasis (pinworm infection) is treatable with over-the-counter or prescription medication, but reinfection, which occurs easily, should be prevented. For best results, the entire family should be treated and thorough washing of pajamas, bed linens and underwear done.
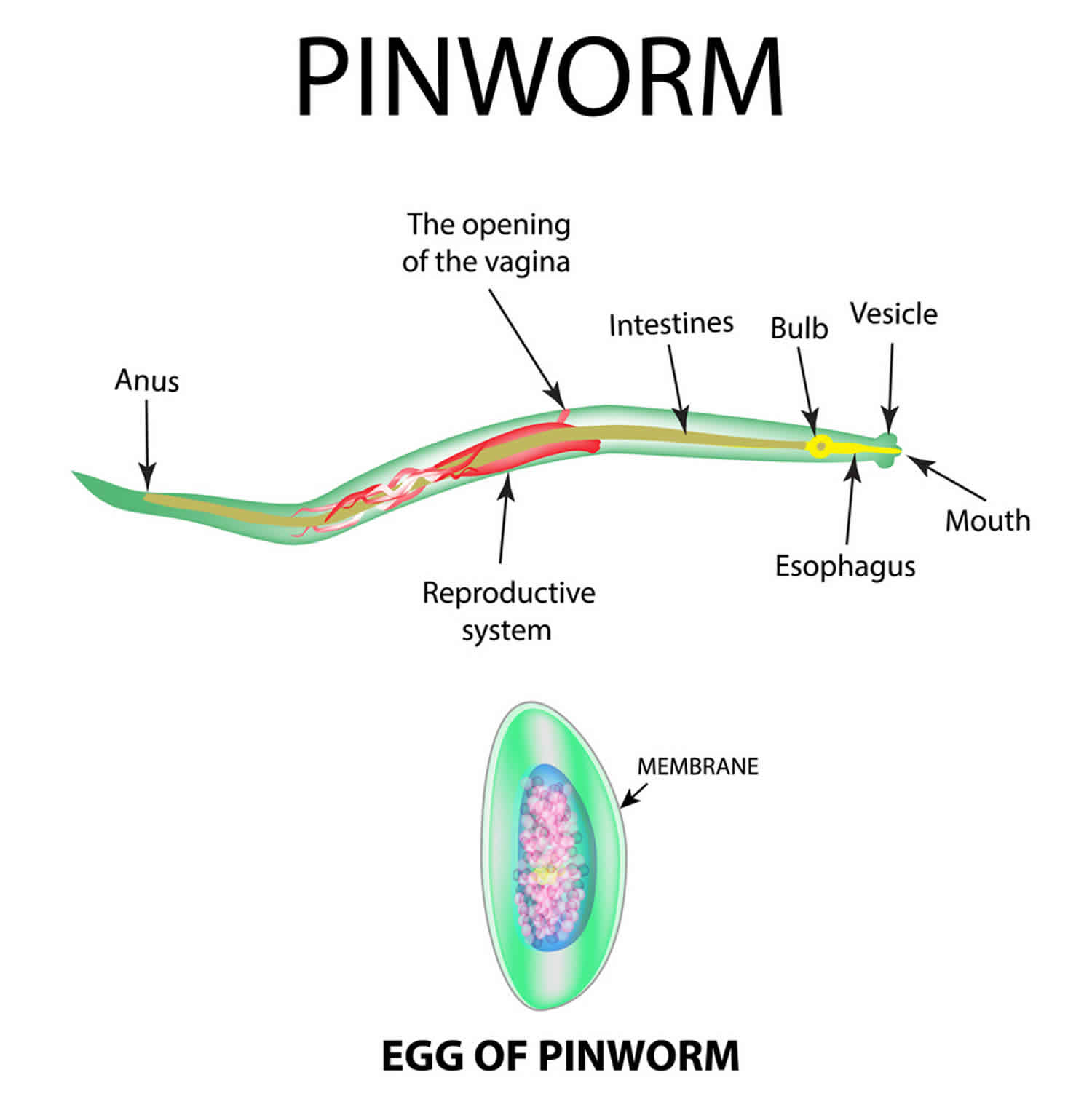
Pinworms are thin and white, measuring about 1/4 to 1/2 inch (about 6 to 13 millimeters) in length. While an infected person sleeps, female pinworms leave the intestine through the anus and deposit their eggs on the surrounding skin. Most people infected with pinworms have no symptoms, but some people experience anal itching and restless sleep.
Can my family become infected with pinworms from swimming pools?
Enterobiasiss are rarely spread through the use of swimming pools. Enterobiasiss occur when a person swallows pinworm eggs picked up from contaminated surfaces or fingers. Although chlorine levels found in pools are not high enough to kill pinworm eggs, the presence of a small number of pinworm eggs in thousands of gallons of water (the amount typically found in pools) makes the chance of infection unlikely.
My little kids like to co-bathe – could this be how they are becoming infected?
During this treatment time and two weeks after final treatment, it is a good idea to avoid co-bathing and the reuse or sharing of washcloths. Showering may be preferred to avoid possible contamination of bath water. Careful handling and frequent changing of underclothing, night clothes, towels, and bedding can help reduce infection, reinfection, and environmental contamination with pinworm eggs. These items should be laundered in hot water, especially after each treatment of the infected person and after each usage of washcloths until infection is cleared.
Did my pets give me pinworms / can I give pinworms to my pets?
No. Humans are considered to be the only hosts of Enterobius vermicularis which is also known as the human pinworm.
Enterobiasis causes
Enterobiasis is spread by the fecal-oral route, that is by the transfer of infective pinworm eggs from the anus to someone’s mouth, either directly by hand or indirectly through contaminated clothing, bedding, food, or other articles.
Pinworm eggs become infective within a few hours after being deposited on the skin around the anus and can survive for 2 to 3 weeks on clothing, bedding, or other objects. People become infected, usually unknowingly, by swallowing (ingesting) infective pinworm eggs that are on fingers, under fingernails, or on clothing, bedding, and other contaminated objects and surfaces. Because of their small size, pinworm eggs sometimes can become airborne and ingested while breathing.
Once swallowed, the eggs hatch in the intestines and mature into adult worms within a few weeks.
Female pinworms move to the anal area to lay their eggs, which often results in anal itching. When you scratch the itchy area, the eggs cling to your fingers and get under your fingernails. The eggs then get transferred to other surfaces, such as toys, bed linens or toilet seats. The eggs can also be transferred from contaminated fingers to food, liquids, clothes or other people.
Pinworm eggs can survive for two to three weeks on surfaces.
Enterobiasis occurs worldwide and affects persons of all ages and socioeconomic levels. It is the most common worm infection in the United States. Enterobiasis occurs most commonly among:
- school-aged and preschool-aged children,
- institutionalized persons, and
- household members and caretakers of persons with pinworm infection.
Enterobiasis often occurs in more than one person in household and institutional settings. Child care centers often are the site of cases of pinworm infection.
Risk factors for enterobiasis
Risk factors for pinworm infection include:
- Being young. Pinworm infections are most likely to occur in children ages 5 to 10. The microscopic eggs are easily spread to family members, caregivers, or other children at school or child care centers. Pinworm infections are uncommon in children younger than age 2.
- Living in crowded spaces. People who live in institutions are at higher risk of developing pinworm infections.
Enterobiasis life cycle
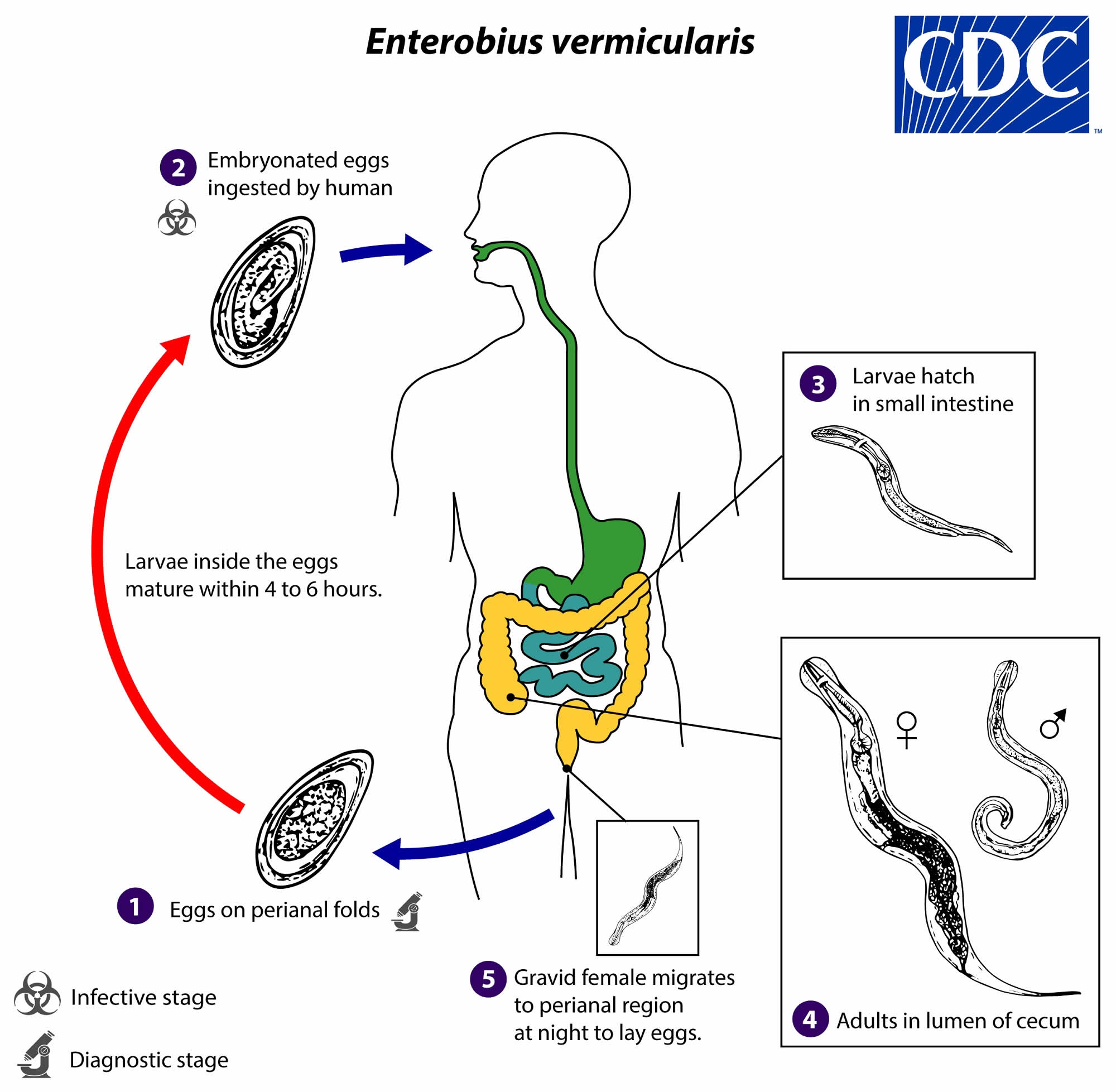
Gravid adult female Enterobius vermicularis deposit eggs on perianal folds (number #1). Infection occurs via self-inoculation (transferring eggs to the mouth with hands that have scratched the perianal area) or through exposure to eggs in the environment (e.g. contaminated surfaces, clothes, bed linens, etc.) (number #2). Following ingestion of infective eggs, the larvae hatch in the small intestine (number #3) and the adults establish themselves in the colon, usually in the cecum (number #4). The time interval from ingestion of infective eggs to oviposition by the adult females is about one month. At full maturity adult females measure 8 to 13 mm, and adult males 2 to 5 mm; the adult life span is about two months. Gravid females migrate nocturnally outside the anus and oviposit while crawling on the skin of the perianal area (number #5). The larvae contained inside the eggs develop (the eggs become infective) in 4 to 6 hours under optimal conditions (number #6).
Rarely, eggs may become airborne and be inhaled and swallowed. Retroinfection, or the migration of newly hatched larvae from the anal skin back into the rectum, may occur but the frequency with which this happens is unknown.
Figure 1. Enterobiasis life cycle
Enterobiasis prevention
Pinworm eggs can cling to surfaces, including toys, faucets, bedding and toilet seats, for two weeks. So besides regular cleaning of surfaces, methods to help prevent the spread of pinworm eggs or to prevent reinfection include:
- Wash in the morning. Because pinworms lay their eggs at night, washing the anal area in the morning can help reduce the number of pinworm eggs on your body. Showering may help avoid possible recontamination in bath water.
- Change underwear and bed linen daily. This helps remove eggs.
- Launder in hot water. Wash bedsheets, nightclothes, underwear, washcloths and towels in hot water to help kill pinworm eggs. Dry on high heat.
- Don’t scratch. Avoid scratching the anal area. Trim your child’s fingernails so there’s less space for eggs to collect. Discourage nail biting.
- Strict observance of good hand hygiene is the most effective means of preventing pinworm infection. This includes washing hands with soap and warm water after using the toilet, changing diapers, and before handling food. Keep fingernails clean and short, avoid fingernail-biting, and avoid scratching the skin in the perianal area. Teach children the importance of washing hands to prevent infection.
Daily morning bathing and changing of underclothes helps remove a large proportion of pinworm eggs and can help prevent infection and reinfection. Showering may be preferred to avoid possible contamination of bath water. Careful handling (avoid shaking) and frequent laundering of underclothes, night clothes, towels, and bed sheets using hot water also helps reduce the chance of infection and reinfection by reducing environmental contamination with eggs.
Also, infected people should comply with good hygiene practices such as washing their hands with soap and warm water after using the toilet, changing diapers, and before handling food. They should also cut fingernails regularly, and avoid biting the nails and scratching around the anus. Frequent changing of underclothes and bed linens first thing in the morning is a great way to prevent possible transmission of eggs in the environment and risk of reinfection. These items should not be shaken and carefully placed into a washer and laundered in hot water followed by a hot dryer to kill any eggs that may be there.
Control can be difficult in child care centers and schools because the rate of reinfection is high. In institutions, mass and simultaneous treatment, repeated in 2 weeks, can be effective. Hand hygiene is the most effective method of prevention. Trimming and scrubbing the fingernails and bathing after treatment is important to help prevent reinfection and spread of pinworms.
Enterobiasis symptoms
Enterobiasis (pinworm infection) causes itching around the anus which can lead to difficulty sleeping and restlessness. Symptoms are caused by the female pinworm laying her eggs. Symptoms of pinworm infection usually are mild and some infected people have no symptoms.
Symptoms of pinworm infection may include:
- Itching of the anal or vaginal area
- Insomnia, irritability and restlessness
- Intermittent abdominal pain and nausea
Enterobiasis complications
Typical pinworm infections don’t cause serious problems. In rare circumstances, heavy infestations can cause infection of female genitals.
The parasite can travel from the anal area up the vagina to the uterus, fallopian tubes and around the pelvic organs. This can cause problems such as inflammation of the vagina (vaginitis) and inflammation of the inner lining of the uterus (endometritis).
Although rare, other complications of a pinworm infection may include:
- Urinary tract infections
- Weight loss
Enterobiasis diagnosis
Itching during the night in a child’s perianal area strongly suggests pinworm infection. Diagnosis is made by identifying the worm or its eggs. Worms can sometimes be seen on the skin near the anus or on underclothing, pajamas, or sheets about 2 to 3 hours after falling asleep.
Pinworm eggs can be collected and examined using the “tape test” as soon as the person wakes up. The “tape test” is done by firmly pressing the adhesive side of clear, transparent cellophane tape to the skin around the anus. The eggs stick to the tape and the tape can be placed on a slide and looked at under a microscope. Because washing/bathing or having a bowel movement can remove eggs from the skin, this test should be done as soon as the person wakes up in the morning before they wash, bathe, go to the toilet, or get dressed. For best results, perform the tape test three days in a row, and then take the pieces of tape to your doctor. Your doctor can look at the tape under a microscope to see if there are any pinworm eggs.
Because itching and scratching of the anal area is common in pinworm infection, samples taken from under the fingernails may also contain eggs. Pinworm eggs rarely are found in routine stool or urine samples.
Enterobiasis treatment
Pinworm can be treated with either prescription or over-the-counter medications. A health care provider should be consulted before treating a suspected case of enterobiasis. The medications used for the treatment of pinworm are either mebendazole, pyrantel pamoate, or albendazole. Any of these drugs are given in one dose initially, and then another single dose of the same drug two weeks later. Pyrantel pamoate is available without prescription. The medication does not reliably kill pinworm eggs. Therefore, the second dose is to prevent re-infection by adult worms that hatch from any eggs not killed by the first treatment. Your doctor may recommend over-the-counter pyrantel pamoate (Reese’s Pinworm Medicine, others) or prescribe medication to all members of your household to prevent infection and reinfection.
The most common prescription anti-parasite medications for pinworms are:
- Mebendazole
- Albendazole (Albenza)
You may have mild gastrointestinal side effects during the course of treatment, and you often need to take at least two doses to get rid of the pinworms completely.
All household contacts and caretakers of the infected person should be treated at the same time. Reinfection can occur easily so strict observance of good hand hygiene is essential (e.g. proper handwashing, maintaining clean short fingernails, avoiding nail biting, avoiding scratching the perianal area).
Daily morning bathing and daily changing of underwear helps removes a large proportion of eggs. Showering may be preferred to avoid possible contamination of bath water. Careful handling and frequent changing of underclothing, night clothes, towels, and bedding can help reduce infection, reinfection, and environmental contamination with pinworm eggs. These items should be laundered in hot water, especially after each treatment of the infected person and after each usage of washcloths until infection is cleared.
Mebendazole
Note on treatment in pregnancy
Pregnancy Category C: Either studies in animals have revealed adverse effects on the fetus (teratogenic or embryocidal, or other) and there are no controlled studies in women or studies in women and animals are not available. Drugs should be given only if the potential benefit justifies the potential risk to the fetus.
Mebendazole is in pregnancy category C. Data on the use of mebendazole in pregnant women are limited. The available evidence suggests no difference in congenital anomalies in the children of women who were treated with mebendazole during mass treatment programs compared with those who were not. In mass treatment programs for which the World Health Organization (WHO) has determined that the benefit of treatment outweighs the risk, WHO allows use of mebendazole in the 2nd and 3rd trimesters of pregnancy. The risk of treatment in pregnant women who are known to have an infection needs to be balanced with the risk of disease progression in the absence of treatment.
Note on treatment during breastfeeding
It is not known whether mebendazole is excreted in breast milk. The WHO classifies mebendazole as compatible with breastfeeding and allows the use of mebendazole in lactating women.
Note on treatment in children
The safety of mebendazole in children has not been established. There is limited data in children age 2 years and younger. Mebendazole is listed as an intestinal antihelminthic medicine on the WHO Model List of Essential Medicines for Children, intended for the use of children up to 12 years of age.
Pyrantel Pamoate
Note on treatment in pregnancy
Pregnancy Category C: Either studies in animals have revealed adverse effects on the fetus (teratogenic or embryocidal, or other) and there are no controlled studies in women or studies in women and animals are not available. Drugs should be given only if the potential benefit justifies the potential risk to the fetus.
Pyrantel pamoate is in pregnancy category C. Data on the use of pyrantel pamoate in pregnant women are limited. In mass treatment programs for which the World Health Organization (WHO) has determined that the benefit of treatment outweighs the risk, WHO allows use of pyrantel pamoate in the 2nd and 3rd trimesters of pregnancy, acknowledging that the effects of pyrantel on birth outcome are not certain. The risk of treatment in pregnant women who are known to have an infection needs to be balanced with the risk of disease progression in the absence of treatment.
Note on treatment during breastfeeding
It is not known whether pyrantel pamoate is excreted in breast milk. The WHO classifies pyrantel pamoate as compatible with breastfeeding, although data on the use of pyrantel pamoate during lactation are limited.
Note on treatment in children
The safety of pyrantel pamoate in children has not been established. According to WHO guidance on preventive chemotherapy, pyrantel may be used in children age 1 year and older during mass treatment programs without diagnosis. Pyrantel pamoate is listed as an intestinal antihelminthic medicine on the WHO Model List of Essential Medicines for Children, intended for the use of children up to 12 years of age.
Albendazole
Note on treatment in pregnancy
Pregnancy Category C: Either studies in animals have revealed adverse effects on the fetus (teratogenic or embryocidal, or other) and there are no controlled studies in women or studies in women and animals are not available. Drugs should be given only if the potential benefit justifies the potential risk to the fetus.
Albendazole is pregnancy category C. Data on the use of albendazole in pregnant women are limited, though the available evidence suggests no difference in congenital abnormalities in the children of women who were accidentally treated with albendazole during mass prevention campaigns compared with those who were not. In mass prevention campaigns for which the World Health Organization (WHO) has determined that the benefit of treatment outweighs the risk, WHO allows use of albendazole in the 2nd and 3rd trimesters of pregnancy. However, the risk of treatment in pregnant women who are known to have an infection needs to be balanced with the risk of disease progression in the absence of treatment.
Note on treatment during breastfeeding
It is not known whether albendazole is excreted in human milk. Albendazole should be used with caution in breastfeeding women.
Note on treatment in children
The safety of albendazole in children less than 6 years old is not certain. Studies of the use of albendazole in children as young as one year old suggest that its use is safe. According to WHO guidelines for mass prevention campaigns, albendazole can be used in children as young as 1 year old. Many children less than 6 years old have been treated in these campaigns with albendazole, albeit at a reduced dose.
Should family and other close contacts of someone with pinworm also be treated for pinworm?
Yes. The infected person and all household contacts and caretakers of the infected person should be treated at the same time.
What should be done if the pinworm infection occurs again?
Reinfection occurs easily. Prevention always should be discussed at the time of treatment. Good hand hygiene is the most effective means of prevention. If pinworm infection occurs again, the infected person should be retreated with the same two-dose treatment. The infected person’s household contacts and caretakers also should be treated. If pinworm infection continues to occur, the source of the infection should be sought and treated. Playmates, schoolmates, close contacts outside the home, and household members should be considered possible sources of infection. Each infected person should receive the recommended two-dose treatment.