Epiploic appendagitis
Epiploic appendagitis also called appendicitis epiploica, hemorrhagic epiploitis, epiplopericolitis or appendagitis, is a rare benign (harmless) self-limiting inflammatory process of the colonic epiploic appendices caused by an ischemic infarction of an epiploic appendage due to torsion (twisting) or spontaneous thrombosis of the epiploic appendage central draining vein 1. The risk of recurrence is low and complications are even rarer 2. Epiploic appendages are normal small fat-filled sacs on the anti-mesenteric surface of the colon. Epiploic appendagitis is a benign and self-limited condition 3. Unlike its mimics, epiploic appendagitis is, generally, a self-limiting local inflammation and can be treated with anti-inflammatory medication 4. For these reasons, it is very important for clinicians to consider epiploic appendagitis as a cause for abdominal pain since inaccurate diagnosis can lead to prolonged hospital stay, antibiotic therapy, and surgical interventions 5. Today, ultrasound (US) and CT scan play a crucial role in diagnosis of this epiploic appendagitis 6. The normal epiploic appendages are undetectable on computed tomography (CT) images due to the overlapping in density with the surrounding peritoneal and omental fat, while they can be noted when they are inflamed and/or outlined by ascites 7.
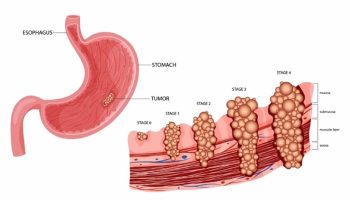
Epiploic appendagitis is usually diagnosed by CT scanning and has become more widely recognized given today’s higher resolution scanners. Imaging findings include the presence of an oval lesion with fat-attenuation surrounded by a thin hyperdense rim on CT (“hyperattenuating ring sign”) abutting anteriorly the large bowel, usually associated with inflammation of the adjacent mesentery 8. A central high-attenuation focus within the fatty lesion (“central dot sign”) can sometimes be observed and is indicative of a central thrombosed vein within the inflamed epiploic appendage 8. Rarely, epiploic appendagitis may be located within a hernia sac or attached to the vermiform appendix. Chronically infarcted epiploic appendage may detach, appearing as an intraperitoneal loose calcified body in the abdominal cavity 8.
The most common sites of development of epiploic appendagitis are the rectosigmoid (57%) and the ileocecum (26%); rarer sites are the ascending (9%), transverse (6%), and descending colon (2%) 5.
Epiploic appendagitis is a rare condition with an incidence of 8.8 per 1 million people and it is usually a diagnosis by exclusion 9. Epiploic appendagitis may occur at any age. Two retrospective studies reported that men (70%) were affected more than women with an age range of 26 to 75 years 6. The average patient is about 40 years old and develops acute abdominal pain which may be left-sided, right, or central. The pain is sharp and stabbing and may be associated with nausea or vomiting. Fever is usually absent. The symptoms from epiploic appendagitis often mimic acute appendicitis, diverticulitis, or cholecystitis. Initial lab studies are usually normal. Typically, a CT scan is ordered to help exclude more serious or surgical problems (above) and the inflammatory changes of epiploic appendagitis are seen coincidentally. epiploic appendagitis follows a benign, self-limiting course and may be treated with analgesics and expectant observation. The usual time course is about one week. A correct diagnosis is important to avoid unnecessary surgical or medical intervention.
At clinical examination, patients usually describe a localized, strong, nonmigratory, sharp pain which usually started after a specific physical movement of their body, like postprandial exercise. An abdominal tenderness is present in all patients. There is a lack of fever, vomiting or leukocytic response 6. Diagnosis of epiploic appendagitis is made challenging by the lack of pathognomonic clinical features and should therefore be considered as a potential diagnosis by exclusion. With diverticulitis and appendicitis being the most important causes of lower abdominal pain, they are the most frequent clinical diagnosis before diagnostic imaging or diagnostic laparoscopy. The pain usually is located on the left or right lower abdominal quadrant 6.
Epiploic appendagitis key points
- Epiploic appendagitis is a rare entity causing acute abdominal pain, due to a benign, self-limited inflammation of the epiploic appendages.
- Epiploic appendagitis is a clinical mimicker of other acute abdomen causes, including acute diverticulitis and appendicitis.
- Imaging features of epiploic appendagitis include fat-density ovoid lesion, “hyperattenuating ring sign,” mild bowel wall thickening, and “central dot sign.”
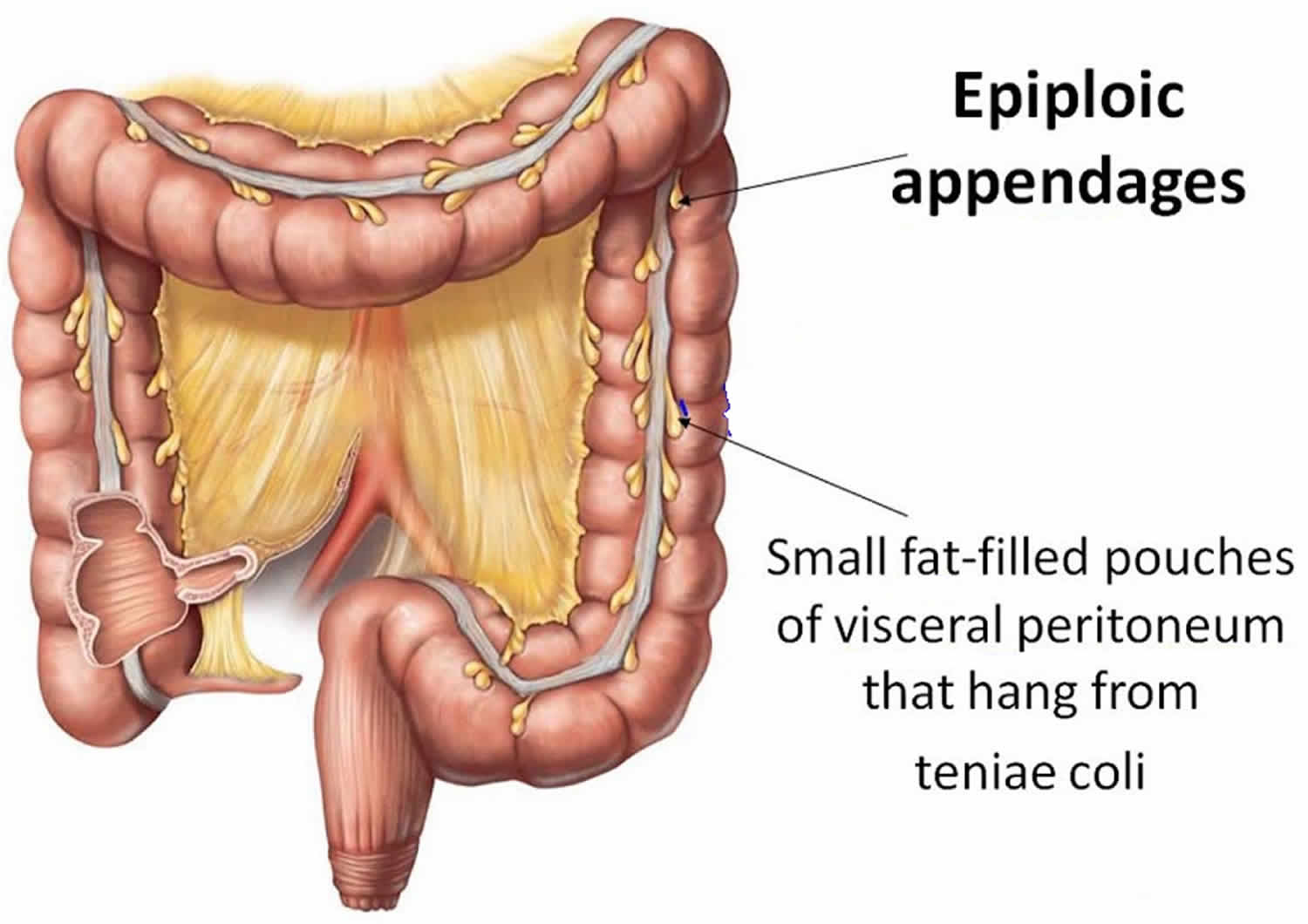
Figure 1. Epiploic appendages
Epiploic appendages anatomy
Epiploic appendages are small outpouchings of fat-filled, serosa-covered structures present on the external surface of the colon projecting into the peritoneal cavity. Each appendage encloses small branches of the circular artery (one or two arterioles) and a single vein that supply the corresponding segment of the colon 10. Subserosal lymphatic channels either terminate in a lymph node within an appendage or loop through its base en route to mesenteric nodes.
On average, the adult colon has approximately 50 to 100 appendages 11. Epiploic appendages occur all along the entire colon but are more abundant and larger in the transverse and sigmoid colon. They are usually rudimentary at the base of the appendix 12. The epiploic appendages vary considerably in size, shape, and contour. Most epiploic appendages are 1 to 2 cm thick and 2 to 5 cm long, although they are occasionally up to 15 cm 13. For unclear reasons, they are largest and most prominent in obese persons and in those who have recently lost weight 14. Although the exact role of epiploic appendages is not known, they are presumed to serve a protective and defensive mechanism similar to that offered by the greater omentum and may have a role in colonic absorption 14. Epiploic appendages may also act as a cushion, protecting colonic blood supply during peristalsis 15.
Epiploic appendagitis causes
Epiploic appendagitis is caused by a spontaneous torsion or twisiting causing obstruction of blood flow within the tissue and then ischemia up to a gangrenous necrosis of the epiploic appendage or by primary thrombosis of the draining vein and inflammation 11. Epiploic appendagitis may also be secondary to other local inflammatory processes affecting adjacent organs, particularly in case of diverticulitis, appendicitis, pancreatitis, or cholecystitis 16. Obesity and rapid weight loss are described as potential risk factors for the development of epiploic appendagitis 17.
Epiploic appendagitis symptoms
Epiploic appendagitis clinical presentation may vary among patients. Epiploic appendagitis clinical presentation is typically characterized by acute or subacute abdominal pain, in most cases (60–80%) in the left lower quadrant, but it can also be localized in the right lower quadrant 18 miming a varied number of diseases such as appendicitis, diverticulitis, acute cholecystitis, and omental infarction 19. Patients may also report postprandial fullness, swelling, vomiting, early satiety, diarrhea, and rarely mild fever 20.
Epiploic appendagitis is often an underestimated and overlooked mimicker, easily misdiagnosed with other causes of abdominal pain requiring urgent care or surgical evaluation in emergency department, particularly acute diverticulitis (left iliac pain) or acute appendicitis (right iliac pain) 21.
On physical examination, patients complain of focal non-migratory abdominal pain in the lower abdominal quadrants (left more commonly than right), not exacerbated by physical movement, without significant guarding or rigidity, and in the absence of a palpable mass 20. The pain is typically circumscribed and the patient may often point his finger on the place where the lesion is situated.
Epiploic appendagitis complications
Complications of primary epiploic appendagitis have been occasionally reported. The inflammatory process may rarely cause adhesions and lead to small bowel obstruction and thus required surgical treatment 22. Epiploic appendages are not in continuity with the fecal content, indeed pyogenic abscesses are not a typical complication 23. In case of CT evidence of intra-abdominal abscess, the diagnosis of epiploic appendagitis secondary to complicated diverticulitis should be considered 24.
Epiploic appendagitis diagnosis
Imaging studies
The clinical diagnosis of epiploic appendagitis is challenging due to the lack of pathognomonic clinical signs or laboratory markers 8. Currently, thanks to the increased use of ultrasound (US) and CT scan in the evaluation of acute abdominal pain, most cases of epiploic appendagitis are diagnosed using CT (preferred) and ultrasound scan 25. Instead, Magnetic Resonance Imaging (MRI) is rarely used for diagnosis. Abdominopelvic ultrasound scan and CT examinations do not allow seeing the normal epiploic appendices, unless there is surrounding intraperitoneal fluid 26. In cases of acute epiploic appendagitis, ultrasound evaluation shows, in the patient’s area of maximal tenderness, the presence of a small (2-4 cm in maximal diameter) rounded or ovoid, noncompressible, and hyperechoic mass adherent to the colonic wall, without internal blood flow on color or power Doppler studies, frequently surrounded by a subtle hypoechoic line 27. The typical CT findings in cases of acute epiploic appendagitis include the presence of rounded or ovoid fat-density mass adjacent to the colonic wall, usually less than 5 cm in diameter (typical diameter range: 1.5–3.5 cm) 28, the “hyperattenuating/hyperdense ring sign” 29, a hyperdense enhancing rim (thickness of 1-3 mm) surrounding the lesion, and the perilesional inflammatory fat stranding 27. A pathognomonic CT finding of epiploic appendagitis is the “central dot sign”, characterized by a central, ill-defined round area of high attenuation within the fat-density mass 30. This sign is also known as the “dense central vessel sign” due to engorged or thrombosed vessel within the inflamed epiploic appendage 31. Although the presence of this area of high attenuation is pathognomonic, its absence does not preclude a diagnosis of acute epiploic appendagitis 32.
MR may show a small oval mass with a signal intensity similar to the fat. Contrast-enhanced T1-weighted MRI images show also an enhancing rim around the oval fatty mass 19.
The wall of the colon may show associated reactive thickening 27.
Chronically, a calcification can develop within the infarcted appendage epiploica and may detach to form an intraperitoneal loose body (peritoneal “mice”) 33. Rarely, appendagitis may be located in the hernia sac 27 or involve the vermiform appendix, mimicking appendicitis 34.
Colonoscopy is sometimes performed before CT or ultrasound for the evaluation of abdominal colic pain; however, such a procedure will not provide an explanation for the presented symptoms in patients who have epiploic appendagitis 35.
Differential diagnosis for the imaging features of acute epiploic appendagitis include other acute inflammatory diseases, such as acute appendicitis, acute diverticulitis and sclerosing mesenteritis, fat-containing primary tumors or metastasis, and acute omental infarction, each one with characteristics imaging findings 27. In particular, omental infarction is described as having many pathophysiologic similarities to epiploic appendagitis but, at CT, an omental infarction lesion is usually larger than that of epiploic appendagitis and is cake-like, centred in the omentum, and located medial to the cecum or ascending colon 35.
Laboratory studies
White blood cell count, erythrocyte sedimentation rate, and C-reactive protein levels are within normal range in the majority of patients, while mild leukocytosis may occasionally be observed due to inflammatory response 21.
Epiploic appendagitis treatment
In the current literature, epiploic appendagitis is predominantly described as a self-limiting condition which spontaneously resolves within 2 weeks from the onset of symptoms 36 and most patients are treated conservatively and nonsurgically either with or without nonsteroidal anti-inflammatory drugs 35.
Epiploic appendagitis surgery
Surgery is not indicated, since the treatment is conservative with nonsteroidal anti-inflammatory drugs, according to the patient’s symptoms 24. Some authors believed that surgical intervention with ligation and excision of the inflamed epiploic appendages was the only way to prevent recurrences and complications, such as adhesions and intussusception induced by inflammation 37. However, invasive intervention is usually avoided due to the potential complications present in all surgical procedures. In some cases, epiploic appendagitis has been reported as an unexpected finding in patients who underwent laparotomy for acute abdominal pain with clinical suspicion of acute appendicitis or acute diverticulitis 38. Epiploic appendagitis can also be a diagnosis of exclusion when other causes of acute abdominal pain are disproved.
In very rare circumstances, an epiploic appendix can protrude into a hernia sac and become an irreducible hernia 39. The diagnosis of incarcerated or strangulated hernia, clinically suspected in patients with non-reducible and painful inguinal mass, should be excluded by CT imaging in the absence of radiological signs of intestinal obstruction. However, in these cases, an emergency exploration of the inguinal canal cannot be postponed in order to rule out a possible incarceration of intestinal loops. Treatment involves the excision of epiploic appendix followed by hernia repair (herniorrhaphy or hernioplasty) 40.
- Epiploic appendagitis. https://www.uptodate.com/contents/epiploic-appendagitis[
]
- Hwang JA, Kim SM, Song HJ, et al. Differential diagnosis of left-sided abdominal pain: primary epiploic appendagitis vs colonic diverticulitis. World J Gastroenterol. 2013;19:6842–6848. doi: 10.3748/wjg.v19.i40.6842[
]
- DOCKERTY MB, LYNN TE, WAUGH JM. A clinicopathologic study of the epiploic appendages. Surg Gynecol Obstet 1956; 103:423.[
]
- Di Serafino M, Iacobellis F, Trovato P, et al. Acute Epiploic Appendagitis: A Nonsurgical Abdominal Pain. Case Rep Emerg Med. 2019;2019:7160247. Published 2019 Jul 14. doi:10.1155/2019/7160247 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6662477[
]
- Chu E. A., Kaminer E. Epiploic appendagitis: a rare cause of acute abdomen. Radiology Case Reports. 2018;13(3):599–601. doi: 10.1016/j.radcr.2018.02.022[
][
]
- Sand M., Gelos M., Bechara F. G., et al. Epiploicappendagitis – clinical characteristics of an uncommon surgical diagnosis. BMC Surgery. 2007;7, article 11[
][
][
][
]
- Singh AK, Gervais DA, Hahn PF, Sagar P, Mueller PR, Novelline RA. Acute epiploic Appendagitis and its mimics. Radiographics. 2005;25:1521–1534. doi: 10.1148/rg.256055030[
]
- Giambelluca D, Cannella R, Caruana G, et al. CT imaging findings of epiploic appendagitis: an unusual cause of abdominal pain. Insights Imaging. 2019;10(1):26. Published 2019 Feb 22. doi:10.1186/s13244-019-0715-9 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6386757[
][
][
][
]
- de Brito P., Gomez M. A., Bessson M. Frequency and epidemiology of primary epiploicappendagitis on CT in adults with abdominal pain. Journal de Radiologie. Feb 2008;89(2):235–243. doi: 10.1016/S0221-0363(08)70399-8[
]
- Gourgiotis S., Oikonomou C., Veloudis G., Lardou I., Pittaras G., Villias C. The diagnostic dilemma of primary epiploic appendagitis and how to establish a diagnosis. Oman Medical Journal. 2016;31(3):235–237. doi: 10.5001/omj.2016.45[
]
- Tabbara T. A., Alassaf O. Y., Kaouas M. C. Acute epiploic appendigitis: Diagnostic and laparoscopic approach. International Journal of Surgery Case Reports. 2018;44:157–160. doi: 10.1016/j.ijscr.2018.02.003[
][
]
- Patterson DC. Appendices epiploicae and their surgical significance with report of three cases. N Engl J Med 1933; 209:1255.[
]
- Linkenfeld F. Deutsche Ztschr f Chir 1908; 92:383.[
]
- Ghahremani GG, White EM, Hoff FL, Gore RM, Miller JW, Christ ML. Appendices epiploicae of the colon: radiologic and pathologic features. Radiographics. 1992;12:59–77. doi: 10.1148/radiographics.12.1.1734482[
][
]
- Pines BR, Beller J. Primary torsion and infarction of the appendices epiploicae. Arch Surg 1941; 42:775.[
]
- Jalaguier A, Zins M, Rodallec M, Nakache JP, Boulay-Coletta I, Jullès MC. Accuracy of multidetector computed tomography in differentiating primary epiploic appendagitis from left acute colonic diverticulitis associated with secondary epiploic appendagitis. Emerg Radiol. 2010;17:51–56. doi: 10.1007/s10140-009-0822-x[
]
- Nugent JP, Ouellette HA, O’Leary DP, Khosa F, Nicolaou S, McLaughlin PD. Epiploic appendagitis: 7-year experience and relationship with visceral obesity. Abdom Radiol (NY) 2018;43:1552–1557. doi: 10.1007/s00261-017-1355-5[
]
- Legome E. L., Belton A. L., Murray R. E., Rao P. M., Novelline R. A. Epiploic appendagitis: the emergency department presentation. The Journal of Emergency Medicine. 2002;22(1):9–13. doi: 10.1016/S0736-4679(01)00430-9[
]
- Chan E., El-Banna A. A case report of epiploic appendagitis as a mimic of acute cholecystitis. International Journal of Surgery Case Reports. 2018;53:327–329. doi: 10.1016/j.ijscr.2018.11.003[
][
]
- Ortega-Cruz HD, Martinez-Souss J, Acosta-Pumarejo E, Toro DH. Epiploic appendagitis, an uncommon cause of abdominal pain: a case series and review of the literature. P R Health Sci J. 2015;34:219–221.[
][
]
- Ergelen R, Asadov R, Özdemir B, Tureli D, Demirbaş BT, Tuney D. Computed tomography findings of primary epiploic appendagitis as an easily misdiagnosed entity: case series and review of literature. Ulus Travma Acil Cerrahi Derg. 2017;23:489–494.[
][
]
- Willingham T, Royer AM, Giles WH. Epiploic Appendagitis: a rare cause of small bowel obstruction. Am Surg. 2018;84:e73–e74.[
]
- Thoeni RF, Cello JP. CT imaging of colitis. Radiology. 2006;240:623–638. doi: 10.1148/radiol.2403050818[
]
- Giambelluca D, Cannella R, Caruana G, et al. CT imaging findings of epiploic appendagitis: an unusual cause of abdominal pain. Insights Imaging. 2019;10(1):26. Published 2019 Feb 22. doi:10.1186/s13244-019-0715-9 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6386757/[
][
]
- Patel H., Abdelbaki A., Steenbergen P., Chanana C., Li S. Know the name: acute epiploic appendagitis—CT findings and review of literature. AME Case Reports. 2018;2, article 8 doi: 10.21037/acr.2018.02.02[
]
- Abu-Zidan F. M., Cevik A. A. Diagnostic point-of-care ultrasound (POCUS) for gastrointestinal pathology: state of the art from basics to advanced. World Journal of Emergency Surgery. 2018;13, article 47 doi: 10.1186/s13017-018-0209-y[
]
- Singh A. K., Gervais D. A., Hahn P. F., Sagar P., Mueller P. R., Novelline R. A. Acute epiploic appendagitis and its mimics. RadioGraphics. 2005;25(6):1521–1534. doi: 10.1148/rg.256055030[
][
][
][
][
]
- Boulanger B. R., Barnes S., Bernard A. C. Epiploic appendagitis: an emerging diagnosis for general surgeons. The American surgeon. Nov 2002;68(11):1022–1025.[
]
- Han Q., Nair R. T., DiSantis D. J. The hyperattenuating ring sign of acute epiploic appendagitis. Abdominal Radiology. 2016;41(7):1431–1432. doi: 10.1007/s00261-016-0641-y[
]
- Nejadhamzeeigilani H. The central dot sign of epiploic appendagitis. Abdominal Radiology. 2019;44(2):802–803. doi: 10.1007/s00261-018-1769-8[
]
- Giambelluca D., Dimarco M., Vaccaro Notte M. R., Lo Re G., Midiri M. The ‘central dot sign’ in acute epiploic appendagitis. Abdominal Radiology. 2019;44(4):1606–1607. doi: 10.1007/s00261-018-1785-8[
]
- Almeida A. T., Melão L., Viamonte B., Cunha R., Pereira J. M. Epiploic appendagitis: an entity frequently unknown to clinicians—diagnostic imaging, pitfalls, and look-alikes. American Journal of Roentgenology. 2009;193(5):1243–1251. doi: 10.2214/AJR.08.2071[
]
- Sharma P., Chkhikvadze T., Sharma P. Epiploic appendagitis: a self-limiting cause of abdominal pain. Journal of Natural Science, Biology and Medicine. 2018;9(2):282–284. doi: 10.4103/jnsbm.JNSBM_173_17[
]
- Purysko A. S., Remer E. M., Filho H. M., Bittencourt L. K., Lima R. V., Racy D. J. Beyond appendicitis: common and uncommon gastrointestinal causes of right lower quadrant abdominal pain at multidetector CT. RadioGraphics. 2011;31(4):927–947. doi: 10.1148/rg.314105065[
]
- Schnedl W. J., Krause R., Tafeit E., Tillich M., Lipp R. W., Wallner-Liebmann S. J. Insights into epiploic appendagitis. Nature Reviews Gastroenterology & Hepatology. 2011;8(1):45–49. doi: 10.1038/nrgastro.2010.189[
][
][
]
- Choi YU, Choi PW, Park YH, et al. Clinical characteristics of primary epiploic appendagitis. J Korean Soc Coloproctol. 2011;27:114–121. doi: 10.3393/jksc.2011.27.3.114.[
]
- Saad J, Mustafa HA, Elsani AM, Alharbi F, Alghamdi S. Primary epiploic appendagitis: reconciling CT and clinical challenges. Indian J Gastroenterol. 2014;33:420–426. doi: 10.1007/s12664-014-0466-y[
]
- Aurello P, Petrucciani N, D’Angelo F, Romano C, Balesh A, Ramacciato G. Management of primary epiploic appendagitis in the laparoscopic era. Am Surg. 2012;78:112–114.[
]
- Capaccio E, Di Vito L, Derchi LE. Epiploic appendage torsed within a spigelian hernia: US and CT findings. J Clin Ultrasound. 2012;40:310–313. doi: 10.1002/jcu.20872[
]
- Ballas K, Kontoulis T, Skouras C, et al. Unusual findings in inguinal hernia surgery: report of 6 rare cases. Hippokratia. 2009;13:169–171.[
]