Eruptive lingual papillitis
Eruptive lingual papillitis also known as “transient lingual papillitis”, “lingual fungiform papillae hypertrophy”, “fungiform papillary glossitis”, “lie bumps or liar’s bumps” or “photocopier’s papillitis”, is a common painful inflammatory condition affecting one or several fungiform papillae on the tongue with excessive salivation 1. The term was introduced by Whitaker et al. 2 in 1996 to describe the inflammatory hyperplasia of one to several fungiform lingual papillae that has an acute onset, is painful and transient in nature. Eruptive lingual papillitis is an acute self-limiting condition, probably of viral origin, involving the fungiform papillae of tongue of children 3. Eruptive lingual papillitis or transient lingual papillitis can affect males and females as early as 3 years of age. Fever, difficulty in feeding, salivation and cervical lymphadenopathy (lymph gland enlargement) are usually associated. Spontaneous involution is seen in 2-15 days but may recur 3. Differential diagnoses are strawberry tongue of scarlet fever (widespread erythema and minute papules on skin), hand-foot-mouth disease (vesicles on palms and soles), and food allergy 3. There is no specific treatment for eruptive lingual papillitis apart from maintaining oral hygiene 3.
Eruptive lingual papillitis is considered as a common but under-diagnosed disease 4. It was self-reported by 92 (56%) of 163 workers at the Dental School of the Medical College of Georgia, in a study conducted through questionnaires 2. Three variants of eruptive lingual papillitis have been described, based on their clinical features 1. The localized variant presents with swelling of a single to several fungiform papillae of a solitary lingual area, especially of the tip, the lateral borders and the dorsal surface and may occur in patients of every age with a female predilection 4. In the generalized variant a large proportion of the fungiform papillae is involved. During its usual course, a child of a median age of 3.5 years is initially affected and progressively the disease presents in other family members. This form is more consistent with the descriptive terms eruptive familial lingual papillitis or eruptive lingual papillitis with household transmission 5. Both the localized and generalized forms have an acute onset 6 and the enlarged papillae may vary in color from normal, erythematous or whitish to yellow, while they rarely appear brown or black, due to staining from food or smoking 7. Moreover, these two clinical patterns may be accompanied by disproportionate symptoms, including pain, burning, tingling or itchy sensation, difficulty in feeding, sensitivity to hot foods 1 and, in cases with familial transmission, hypersalivation and occasionally fever and lymph gland enlargement (lymphadenopathy) 5. Symptoms typically resolve after a few hours or 1 to 4 days 6, while they may last for 1 to 3 weeks, when diffuse lingual inflammation coexist 4. Biopsy is not required for the final diagnosis 4, but in cases where it was performed microscopic examination showed an inflamed fungiform papillae with minimal spongiosis and neutrophils infiltration of the epithelium 8. Taste buds that are normally present in fungiform papillae were not detected 8. The papulokeratotic variant of eruptive lingual papillitis is characterized by chronic, generalized tongue involvement with painless, whitish or white-yellow in color enlarged fungiform papillae, histologically corresponding to parakeratosis 8.
Your dentist and dental hygienist are experts on the tongue. If you develop any tongue pain or changes in the appearance of your tongue, schedule a visit. They can give you an accurate diagnosis and the proper treatment for your needs.
Figure 1. Eruptive lingual papillitis
Footnote: Localized form of eruptive lingual papillitis affecting A) both sides of the tip of tongue (#1) and B) the anterior tongue dorsum (#2).
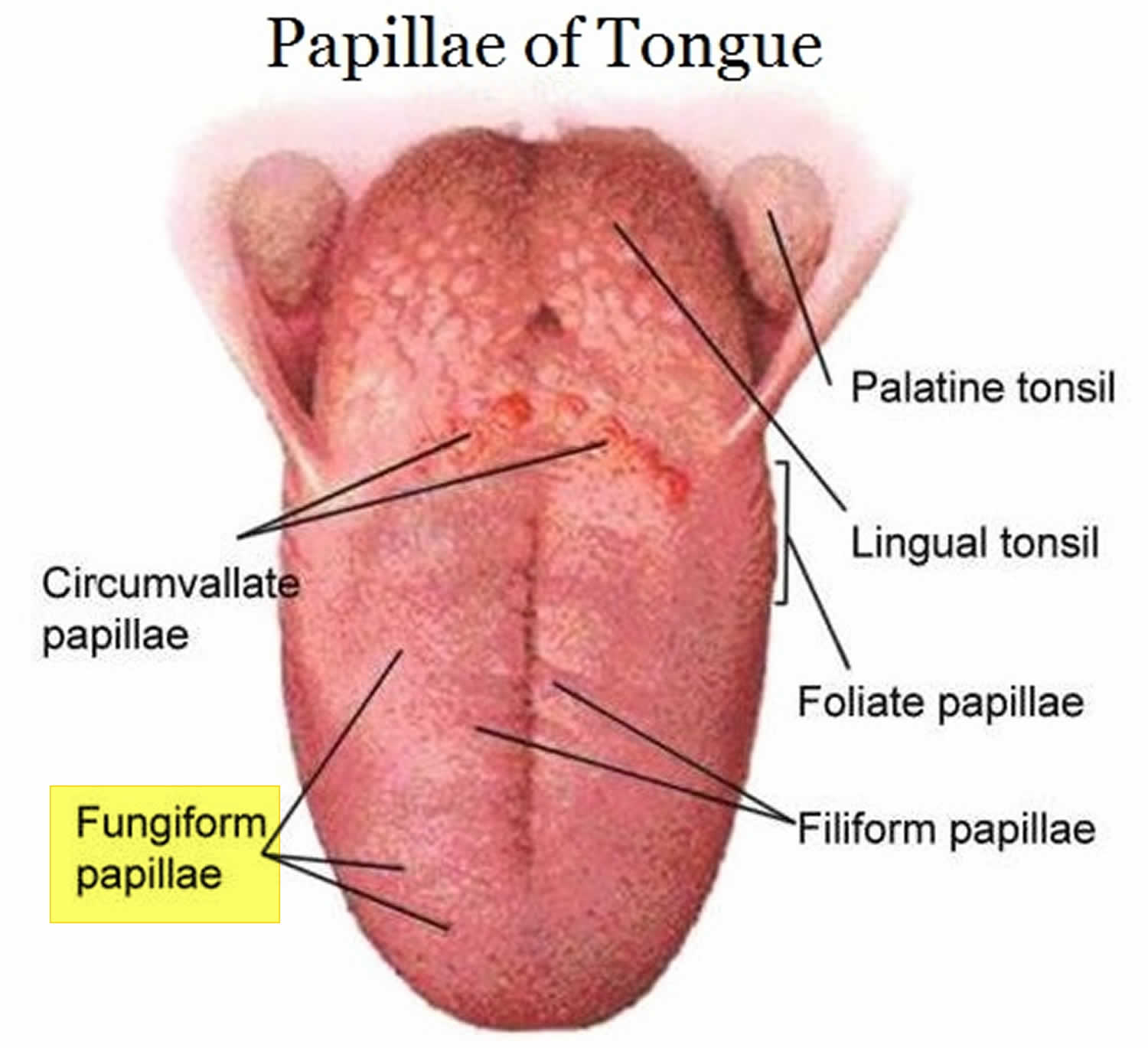
[Source 1 ]Figure 2. Fungiform papillae of tongue
What are fungiform papillae?
Fungiform papillae are one of the special types of bumps found on the surface of the tongue. Fungiform papillae contain taste buds (especially for bitter taste), temperature receptors and have a good blood supply.
They are scattered over the top and sides of the tongue, mainly towards the tip. Usually they are not obvious, being flat and pink.
The number and size of fungiform papillae varies:
- females have more fungiform papillae than males
- they become even more numerous after the menopause
- nerve injury may result in a reduced number of fungiform papillae and reduced taste sensation
Fungiform papillae can become obvious in a number of conditions, the most well recognized of which is the ‘strawberry tongue’ of scarlet fever.
Eruptive lingual papillitis causes
In many eruptive lingual papillitis cases, the cause is unknown and probably multifactorial, as it can be hypothesized by the variable and non-specific histological findings 8. It is related to acute or chronic mechanical trauma, compulsive lingual movements because of local irritating factors, such as sharp-edged teeth or restorations, orthodontic appliances or increased calculus on the anterior teeth 6. Some dental professionals believe the inflammation is due to chronic irritation from teeth, calculus, fillings or dental appliances. Stress, poor nutrition, smoking and alcohol use may also be initiating factors. Other possible factors include stress, lack of sleep, poor nutrition, geographic tongue 4, thermal injury 6, excessive smoking and alcohol uptake 8, consumption of spicy or acidic foods 2, allergy to foods, oral hygiene products or photocopier’s toner 4, as well as gastrointestinal disorders and hormonal changes during menstruation or menopause 4. As eruptive lingual papillitis is more common in patients with history of atopy (dermatitis or eczema), it may also represent a local atopic reaction to heat or irritating foods 9. Often, though, eruptive lingual papillitis is considered idiopathic 2, while it is also regarded as a relapse in adults of eruptive familial lingual papillitis or eruptive lingual papillitis with household transmission that occurred during childhood 5. Possible triggering factors included the chronic lingual irritation on the orthodontic appliance, the habitual lingual trauma, stress or the coexistence with geographic tongue.
Infectious agents, particularly viruses, is implicated in the pathogenesis of both eruptive lingual papillitis and eruptive familial lingual papillitis or eruptive lingual papillitis with household transmission, but is not documented 10. Immunohistochemical investigation for human papillomavirus types 6 and 11 and herpes simplex virus (HSV) type 1 and 2 2, as well as the histochemical investigation for fungi and parasites in biopsy specimens were all negative in eruptive lingual papillitis 8. In a recent publication, though, Krakowski et al. 11 described a case of eruptive lingual papillitis, where the presence of herpes simplex virus (HSV) type 1, was confirmed by direct lesional viral culture, in a patient with Kawasaki disease.
The classic form of transient lingual papillitis affects over 50% of the population. It appears to be most common in young women, but all age groups can be affected. The most likely cause of transient lingual papillitis is local irritation or trauma to a fungiform papilla. However many other possible triggers have been suggested including stress, hormone fluctuations, gastrointestinal upset and specific foods.
Eruptive (familial) lingual papillitis affects young children, and their families. It appears to be most common in Spring, although it can occur all year round. Children in contact with many other children, such as school, kindergarten or day care, appear to be most likely to develop this condition. A viral cause has been suggested because of the common development of the condition in family members. One theory is that, similar to herpes simplex virus / cold sores, the virus is caught in childhood and may then cause recurrent episodes throughout life, in this case presenting in adulthood as the classic form of transient lingual papillitis.
Fungiform papillary glossitis has been described in patients with a history of eczema, asthma or hayfever. It may be another name for transient lingual papillitis. These authors suggested the condition is due to increased environmental sensitivity of the tongue, similar to the increased sensitivity of the skin, lungs or nose resulting in eczema, asthma or hayfever respectively.
Eruptive lingual papillitis symptoms
Eruptive lingual papillitis is a systemic illness often associated with fever and lymph gland enlargement. The onset is sudden, causing acute pain, burning, tingling or itching. It can also cause dry mouth, difficulty eating and discomfort while eating hot foods. The inflammation and symptoms can last anywhere from a few hours to a couple days to several weeks, depending on the case.
Eruptive lingual papillitis generally affects the tip of the tongue, either in an isolated area or on both sides. The enlarged bumps may appear as the tongue’s normal color, or they may be red, white or yellow. Researchers have found that the affected papillae don’t contain taste buds as they usually do.
An affected child may be reluctant to eat and produces excessive saliva. The tongue shows enlarged inflamed fungiform papillae on the tip and the sides of the tip but not the top. These may look like pustules. Angular cheilitis may be seen.
The illness lasts on average 1 week (range 2-15 days). Recurrences have been reported 1-2 months later with the same clinical features. Family members, parents and siblings, may develop symptoms on average one week later (range 1-15 days). In adults, the illness presents as a sudden intense burning of the tongue made worse by food. The clinical appearance is the same as in the child.
Eruptive lingual papillitis diagnosis
Eruptive lingual papillitis or transient lingual papillitis is usually diagnosed clinically based on typical presentation. Your dentist can make a diagnosis based on a visual exam and your health history alone. The severity of your symptoms helps your dentist determine the appropriate treatment for relief.
The diagnosis of eruptive lingual papillitis or transient lingual papillitis does not require a biopsy. Mucosal biopsy shows inflammation and swelling of a fungiform papilla. Special stains fail to detect viral, fungal or bacterial infection. In the papulokeratotic variant, biopsy shows severe hyperparakeratosis and mild chronic inflammation.
Eruptive lingual papillitis treatment
Usually no treatment is required for the classic form of eruptive lingual papillitis as the condition resolves within hours or days. Cases that are not very painful can be managed with warm salt water rinses and over-the-counter pain medications.
In painful cases local anesthetics, topical corticosteroids, coating agents, saline mouthwashes and combination of antihistamines with aluminum hydroxide or magnesium hydroxide suspension for topical use have been administrated, and eating of cold foods has been recommended. The use of analgesics such as acetaminophen (paracetamol) or ibuprofen have not been found to alter the duration or severity of the symptoms in children 5, while there is no consensus on the usefulness of topical antiseptics 5. Patients are also recommended to avoid irritating chewing gums, candies or oral hygiene agents 7. Most often, though, the condition resolves on its own in just a few days and doesn’t return. In some cases eruptive lingual papillitis may relapse 4, most commonly its papulokeratotic variant 8. In recurrences the investigation of the possible trigger factors, especially trauma or allergens, is mandatory 4.
Treatments reported by some patients to give relief have included:
- salt water mouth rinses
- cold fluids
- soothing foods such as yogurt
- antiseptic or local anaesthetic mouthwashes
- topical steroids
However, the majority of sufferers have found nothing to relieve the symptoms or prevent recurrence.
- Kalogirou EM, Tosios KI, Nikitakis NG, Kamperos G, Sklavounou A. Transient lingual papillitis: A retrospective study of 11 cases and review of the literature. J Clin Exp Dent. 2017;9(1):e157-e162. Published 2017 Jan 1. doi:10.4317/jced.53283 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5268094[↩][↩][↩][↩]
- Whitaker SB, Krupa JJ 3rd, Singh BB. Transient lingual papillitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82:441–5.[↩][↩][↩][↩][↩]
- Mondal A, Kumar P. Eruptive lingual papillitis. Indian Pediatr. 2014 Mar;51(3):243. http://www.indianpediatrics.net/mar2014/243.pdf[↩][↩][↩][↩]
- Flaitz ΚΜ, Chavarria C. Painful tongue lesions associated with a food allergy. Pediatr Dent. 2001;23:506–7.[↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Roux O, Lacour JP. Eruptive lingual papillitis with household transmission: a prospective clinical study. Br J Dermatol. 2004;150:299–303. https://doi.org/10.1111/j.1365-2133.2004.05703.x[↩][↩][↩][↩][↩]
- Bouquot JE, Adibi SS, Sanchez M. Chronic lingual papulosis: new, independent entity or “mature” form of transient lingual papillitis? Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:111–7.[↩][↩][↩][↩]
- Noonan V, Kemp S, Gallagher G, Kabani S. Transient lingual papillitis. J Mass Dent Soc. 2008;57:39.[↩][↩]
- Brannon RB, Flaitz CM. Transient lingual papillitis: a papulokeratotic variant. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:187–91.[↩][↩][↩][↩][↩][↩][↩]
- Marks R, Scarff CE, Yap LM, Verlinden V, Jolley D, Campbell J. Fungiform papillary glossitis: atopic disease in the mouth? Br J Dermatol. 2005;153:740–5.[↩]
- Lacour JP, Perrin C. Eruptive familial lingual papillitis: a new entity? Pediatr Dermatol. 1997;14:13–6.[↩]
- Krakowski AC, Kim SS, Burns JC. Transient lingual papillitis associated with confirmed herpes simplex virus 1 in a patient with kawasaki disease. Pediatr Dermatol. 2014;31:e124–5.[↩]