Factor 7 deficiency
Factor 7 deficiency also known as factor VII deficiency, proconvertin deficiency or prothrombin conversion accelerator deficiency, is a rare bleeding disorder that varies in severity among affected individuals. The age of onset and severity varies from person to person. The signs and symptoms of factor 7 deficiency can begin at any age, although the most severe cases are apparent in infancy. While severe cases may become apparent in infancy, very mild cases may never cause any bleeding problems. Signs and symptoms may include nosebleeds (epistaxis); easy bruising; bleeding of the gums; excessive or prolonged bleeding after injury or surgery; and heavy or prolonged menstrual bleeding (menorrhagia) in women. Some people with factor 7 deficiency may have bleeding in the joints (hemarthrosis) or blood in the urine (hematuria). In very severe cases, factor 7 deficiency can be life-threatening, causing bleeding inside the skull (intracranial hemorrhage) or digestive tract. However, up to one-third of people with factor 7 deficiency never have any bleeding problems. Although factor 7 deficiency is primarily associated with increased bleeding, some people with the condition have excessive blood clotting (thrombosis).
Factor VII deficiency affects males and females in equal numbers. Factor 7 deficiency is the most frequently occurring of a group of disorders classified as rare bleeding disorders. Factor VII deficiency is estimated to affect 1 in 300,000 to 1 in 500,000 individuals in the general population. However, many cases of factor VII deficiency go undiagnosed or misdiagnosed, making it difficult to determine the true frequency in the general population. The incidence of factor VII deficiency tends to be higher in countries where marriage to close relatives (consanguineous marriage) is more common. According to the medical literature, more than 200 cases of true factor VII deficiency have been reported. Because of the variable severity of factor VII deficiency, the age of presentation can vary widely from birth until adulthood.
Factor 7 deficiency may be inherited or acquired. The inherited from is caused by mutations in the F7 gene and inheritance is autosomal recessive. The acquired form is not inherited and may be caused by liver disease, blood cell disorders, certain drugs, or vitamin K deficiency. Treatment for bleeding may include intravenous infusions of normal plasma, concentrated factor 7, or genetically-made (recombinant) factor 7. Those with acquired factor 7 deficiency due to vitamin K deficiency may take vitamin K by mouth, injection, or infusion.
Individuals with factor VII deficiency will benefit from a referral to a federally-funded hemophilia treatment center. These specialized centers can provide comprehensive care for individuals with hemophilia and rare bleeding disorders, such as factor VII deficiency. The treatment center’s medical team, headed by a hematologist with expert knowledge in bleeding disorders, will develop specific treatment plans and organize the monitoring and long term follow up of affected individuals, thus ensuring state-of-the-art medical care. Treatment at a hemophilia treatment center ensures that individuals and their family members will be cared for by a professional healthcare team (physicians, nurses, physical therapist, social worker and genetic counselor) experienced in treating individuals with rare bleeding disorders.
Factor 7 deficiency causes
When you bleed, a series of reactions take place in the body that helps blood clots form. This process is called the coagulation cascade. It involves special proteins called coagulation, or clotting factors. You may have a higher chance of excess bleeding if one or more of these factors are missing or are not functioning as they should. Factor VII is one such coagulation factor.
The inherited form of factor 7 deficiency, known as congenital factor 7 deficiency, is caused by mutations in the F7 gene, which provides instructions for making a protein called coagulation factor VII. This protein plays a critical role in the coagulation system, which is a series of chemical reactions that forms blood clots in response to injury. These mutations reduce the amount of coagulation factor VII in the bloodstream. Such a reduction prevents blood from clotting normally, causing episodes of excessive bleeding. It is not known why some people with this condition have problems with thrombosis. Researchers are also do not know what determines the severity of the condition; it does not appear to be related to the amount of coagulation factor 7 in the bloodstream.
The noninherited form of the disorder, called acquired factor 7 deficiency, is less common than the congenital form. It can be caused by liver disease or by blood cell disorders such as myeloma or aplastic anemia. Acquired factor 7 deficiency can also be caused by certain drugs such as medicines that prevent clotting, or by a deficiency of vitamin K.
Factor 7 deficiency inheritance pattern
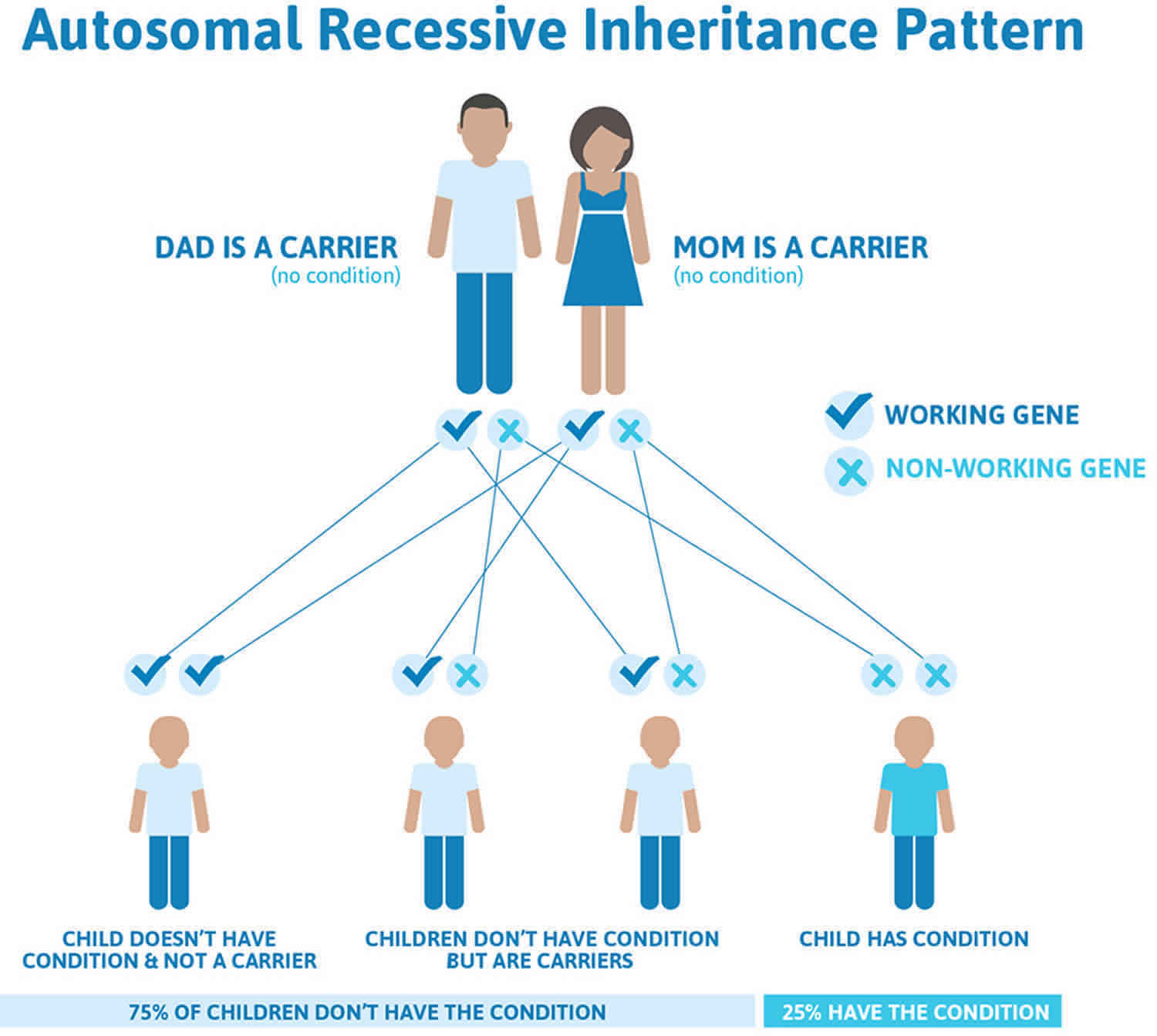
Congenital factor VII deficiency is inherited in an autosomal recessive pattern, which means both copies of the F7 gene in each cell have mutations. The parents of an individual with an autosomal recessive condition each carry one copy of the mutated gene, but they typically do not show signs and symptoms of the condition. Recessive genetic disorders occur when an individual inherits the same abnormal gene from each parent. If an individual receives one normal gene and one gene for the disease, the person will be a carrier for the disease, but usually will not show symptoms. The risk for two carrier parents to both pass on the defective gene and, therefore, have an affected child is 25 percent with each pregnancy. The risk to have a child who is a carrier like the parents is 50 percent with each pregnancy. The chance for a child to receive normal genes from both parents and be genetically normal for that particular trait is 25 percent. The risk is the same for males and females.
Acquired factor VII deficiency is not inherited. Acquired factor 7 deficiency. It can be caused by:
- Low vitamin K (some babies are born with vitamin K deficiency)
- Severe liver disease
- Use of medicines that prevent clotting (anticoagulants such as warfarin)
Figure 1. Congenital factor 7 deficiency autosomal recessive inheritance pattern
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
Factor 7 deficiency symptoms
Factor 7 deficiency symptoms may include any of the following:
- Bleeding from mucus membranes
- Bleeding into joints
- Bleeding into muscles
- Bruising easily
- Heavy menstrual bleeding
- Nosebleeds that do not stop easily
- Umbilical cord bleeding after birth
The symptoms and severity of factor 7 deficiency are highly variable; no consistent correlation between the amount of factor 7 in the blood and overall severity is seen. Some individuals may not develop any symptoms (asymptomatic), including individuals with relatively low levels of factor 7. Other individuals may have mild cases that are only apparent after trauma or surgery. Mild symptoms can include chronic nosebleeds, easy bruising, and bleeding from the gums. Affected women may develop heavy and prolonged periods (menorrhagia).
More serious bleeding complications occur in some individuals and may mimic bleeding patterns seen in hemophilia. Bleeding into the joints (hemarthrosis) can result in progressive joint damage and degeneration, eventually limiting the range of motion of an affected joint. Soft tissue bleeding can result in bruising that seems spontaneous or out of proportion to an injury. Affected individuals can develop masses of congealed blood called hematomas that can cause symptoms due to compression of nearby structures or organs. Bleeding in the stomach, intestines and urogenital tract can also occur resulting in blood in the urine (hematuria) or black, tarry, bloody stools (melena or hematochezia).
Bleeding in severe factor 7 deficiency can result in life-threatening complications. These include major gastrointestinal bleeds as well as head bleeds (intracranial hemorrhage), often during the first few weeks or months of life. Although quite rare, head bleeds have been reported in adults as well.
Individuals with factor 7 deficiency may experience bleeding after surgery or minor procedures or following trauma or injury. Affected women may bleed excessively following childbirth (postpartum bleeding). Some newborns have experienced abnormal bleeding from the umbilical cord stump at birth.
A seemingly paradoxical increased incidence of clotting (thrombosis) has been noted in factor 7 deficiency in recent years. These thromboses can be arterial or venous and they can occur spontaneously or in conjunction with treatment.
Factor 7 deficiency complications
Factor 7 deficiency complications may include:
- Excessive bleeding (hemorrhage)
- Stroke or other nervous system problems from central nervous system bleeding
- Joint problems in severe cases when bleeding happens often
Factor 7 deficiency diagnosis
Tests that may be done include:
- Activated partial thromboplastin time (aPTT)
- Plasma factor VII activity
- Prothrombin time (PT)
- Mixing study, a special PTT test to confirm factor VII deficiency
Individuals with factor VII deficiency have a normal activated partial thromboplastin time (aPTT) and a prolonged prothrombin time (PT). Diagnosis can be confirmed with a factor 7 assay. In affected individuals a factor VII assay will demonstrate reduced activity of factor VII.
Acquired factor VII deficiency can occur in patients with liver disease and vitamin K deficiency, and in those taking oral anticoagulants.
Factor 7 deficiency treatment
Bleeding can be controlled by getting intravenous (IV) infusions of normal plasma, concentrates of factor VII, or genetically produced (recombinant) factor VII. Fresh frozen plasma (FFP) is another option. In some patients, the use of fresh frozen plasma (FFP) has led to blood clots. Antifibrinolytics such as aminocaproic acid can help alleviate the bleeding symptoms.
You will need frequent treatment during bleeding episodes because factor VII does not last for long inside the body.
NovoSeven® RT is a genetically engineered (recombinant) version of factor VII. Because it does not contain human blood or plasma, there is no risk of transmitting blood-borne viruses or other pathogens. NovoSeven has been well-tolerated and associated with few side effects. NovoSeven has been approved by the Food and Drug Administration (FDA) to treat bleeding episodes of individuals with congenital factor VII deficiency.
Individuals with factor VII deficiency have also been treated with prothrombin complex concentrates, which are blood products that contain a concentrated form of four different clotting factors: II, VII, IX and X. However, the amount of each specific factor contained in these products can vary from one preparation to another, making it difficult to determine the most appropriate dosage. Prothrombin complex concentrates undergo a purification process to eliminate viruses and other pathogens. Prothrombin complex concentrates are associated with an increased risk of developing blood clots, especially following repeated administration.
Theoretically, factor VII deficiency can be treated with fresh frozen plasma. However, in clinical practice the very large volume required to stop bleeding renders this impractical, primarily due to the short half-life of factor VII. Half-life refers to the time it takes for half of the infused factor to breakdown and to disappear from the bloodstream.
Some individuals with factor VII deficiency may undergo preventative (prophylactic) therapy in an attempt to prevent or minimize future bleeding complications. Prophylactic therapy has been used for individuals with a history of bleeding into the joints or the brain. The decision to undergo prophylactic therapy in factor VII deficiency is made after careful consultation with a patient’s medical team. The specific prophylactic regimen in factor VII deficiency is case dependent.
Additional treatment options for individuals with factor VII deficiency are symptomatic and supportive. For example, excessive menstrual bleeding in women may be treated by birth control pills or drugs known as antifibrinolytics.
Genetic counseling is recommended for affected individuals and their families.
If you have factor VII deficiency due to a lack of vitamin K, you can take this vitamin by mouth, through injections under the skin, or through a vein (intravenously).
If you have this bleeding disorder, be sure to:
- Tell your health care providers before you have any kind of procedure, including surgery and dental work.
- Tell your family members because they may have the same disorder but do not know it yet.
Factor 7 deficiency prognosis
You can expect a good outcome with proper treatment.
Inherited factor VII deficiency is a lifelong condition.
The outlook for acquired factor VII deficiency depends on the cause. If it is caused by liver disease, the outcome depends on how well your liver disease can be treated. Taking vitamin K supplements will treat vitamin K deficiency.