Giardia duodenalis
Giardia duodenalis also known as Giardia intestinalis or Giardia lamblia, is a microscopic parasite that causes the diarrheal illness known as giardiasis. Giardia duodenalis parasite is found on surfaces or in soil, food, or water that has been contaminated with feces (poop) from infected humans or animals 1. Once a person or animal (for example, cats, dogs, cattle, deer, and beavers) has been infected with Giardia duodenalis, the parasite lives in the intestines and is passed in feces (poop). Once outside the body, Giardia duodenalis can sometimes survive for weeks or months. Giardia duodenalis can be found within every region of the U.S. and around the world.
Giardia duodenalis is a protozoan flagellate (Diplomonadida). This protozoan was initially named Cercomonas intestinalis by Lambl in 1859. It was renamed Giardia lamblia by Stiles in 1915 in honor of Professor A. Giard of Paris and Dr. F. Lambl of Prague. However, many consider the name, Giardia duodenalis, (Davaine 1875) to be the correct taxonomic name for this protozoan.
Giardia duodenalis is protected by an outer shell that allows it to survive outside the body for long periods of time and makes it tolerant to chlorine disinfection. While the parasite can be spread in different ways, water (drinking water and recreational water) is the most common mode of transmission.
Many prescription drugs are available to treat Giardia duodenalis infection. Although the Giardia duodenalis parasite can infect all people, infants and pregnant women may be more likely to experience dehydration from the diarrhea caused by giardiasis. To prevent dehydration, infants and pregnant women should drink a lot of fluids while ill. Dehydration can be life threatening for infants, so it is especially important that parents talk to their healthcare providers about treatment options for their infants.
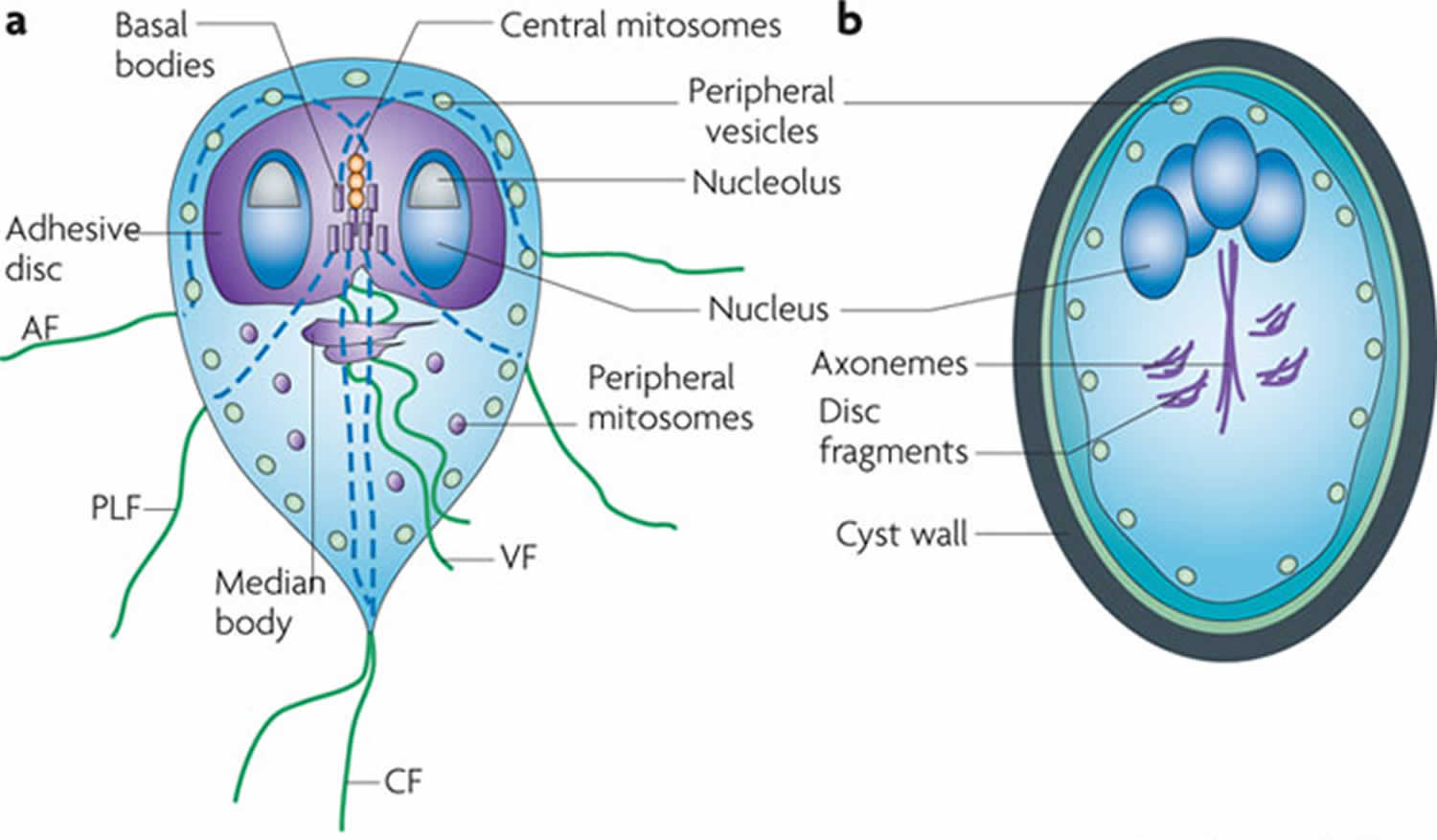
Figure 1. Giardia duodenalis parasite and cyst
My child was recently diagnosed as having a Giardia duodenalis infection, but does not have diarrhea. My healthcare provider says treatment is not necessary. Is this correct?
Your child does not usually need treatment if he or she has no symptoms. However, there are a few exceptions. If your child does not have diarrhea, but does have other symptoms such as nausea or upset stomach, tiredness, weight loss, or a lack of hunger, you and your healthcare provider may need to think about treatment. The same is true if many family members are ill, or if a family member is pregnant and unable to take the most effective medications to treat Giardia. Contact your healthcare provider for specific treatment recommendations.
Where and how does Giardia duodenalis get into drinking water?
Millions of Giardia duodenalis parasites can be released in a bowel movement of an infected human or animal. Human or animal waste (poop) can enter the water through different ways, including sewage overflows, sewage systems that are not working properly, polluted storm water runoff, and agricultural runoff. Wells may be more vulnerable to such contamination after flooding, particularly if the wells are shallow, have been dug or bored, or have been submerged by floodwater for long periods of time.
How can I find out whether there is Giardia duodenalis in my drinking water?
If you suspect a problem and your drinking water comes from a private well, you may contact your state certification officer (https://www.epa.gov/dwlabcert) for a list of laboratories in your area that will perform tests on drinking water for a fee.
How can I remove Giardia duodenalis from my drinking water?
To kill or inactivate Giardia duodenalis, bring your water to a rolling boil for one minute (at elevations above 6,500 feet, boil for three minutes). Water should then be allowed to cool, stored in a clean sanitized container with a tight cover, and refrigerated.
An alternative to boiling water is using a point-of-use filter. Not all home water filters remove Giardia duodenalis. Filters that are designed to remove Giardia duodenalis parasite should have one of the following labels:
- Reverse osmosis,
- Absolute pore size of 1 micron or smaller,
- Tested and certified by National Safety Foundation (NSF) Standard 53 or NSF/ANSI Standard 58 for cyst removal, or
- Tested and certified by National Safety Foundation (NSF) Standard 53 or NSF/ANSI Standard 58 for cyst reduction.
- As you consider ways to disinfect your well, it is important to note that Giardia duodenalis is moderately chlorine resistant. Contact your local health department for recommended procedures. Remember to have your well water tested regularly, at least once a year, after disinfection to make sure the problem does not recur.
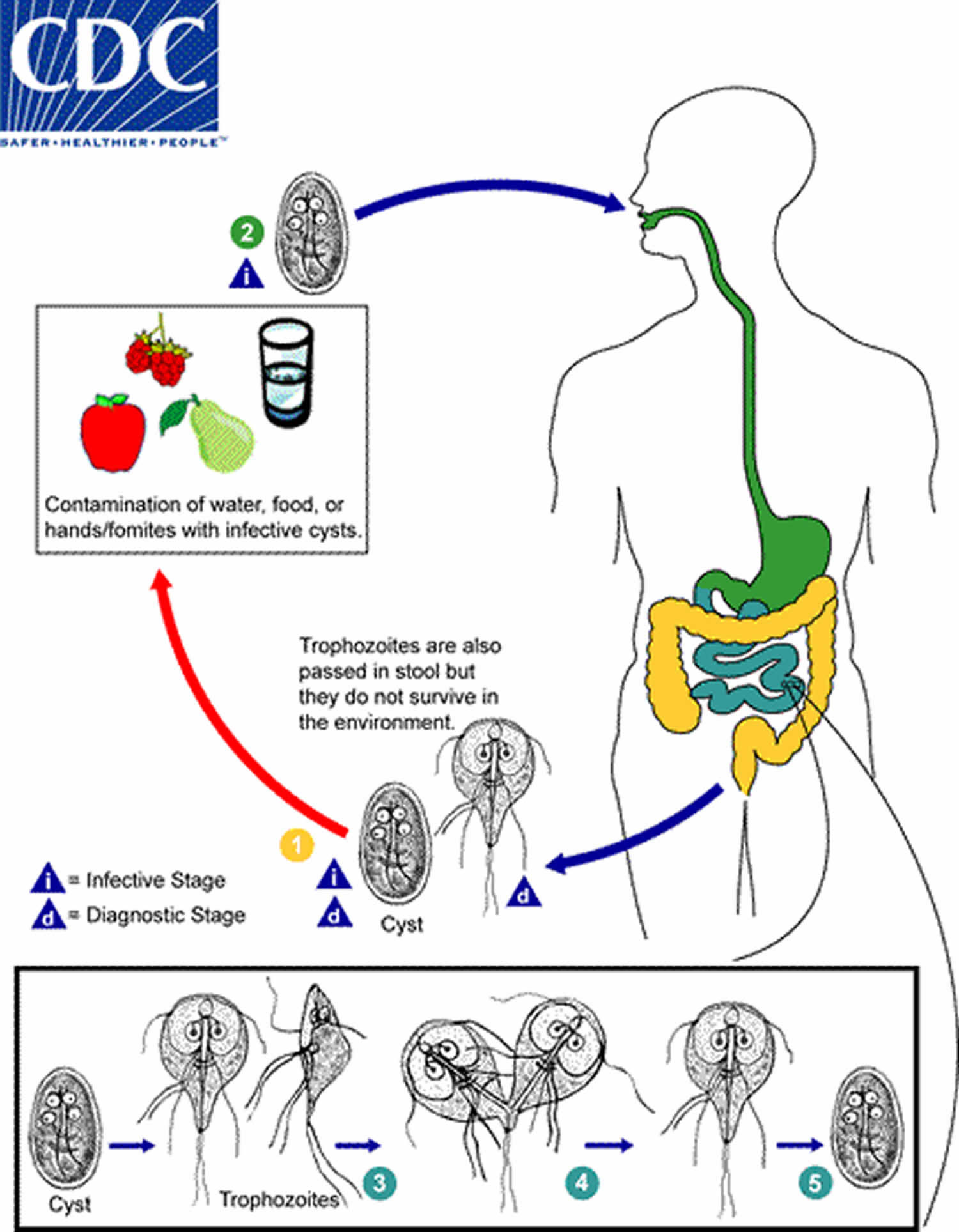
Giardia duodenalis life cycle
Giardia duodenalis cysts are resistant forms and are responsible for transmission of giardiasis. Both cysts and trophozoites can be found in the feces (diagnostic stages) (number 1). The cysts are hardy and can survive several months in cold water. Infection occurs by the ingestion of cysts in contaminated water, food, or by the fecal-oral route (hands or fomites) (number 2). In the small intestine, excystation releases trophozoites (each cyst produces two trophozoites) (number 3). Trophozoites multiply by longitudinal binary fission, remaining in the lumen of the proximal small bowel where they can be free or attached to the mucosa by a ventral sucking disk (number 4). Encystation occurs as the parasites transit toward the colon. The cyst is the stage found most commonly in nondiarrheal feces (number 5). Because the cysts are infectious when passed in the stool or shortly afterward, person-to-person transmission is possible. While animals are infected with Giardia, their importance as a reservoir is unclear.
Figure 2. Giardia duodenalis life cycle
Giardia duodenalis transmission
Giardia duodenalis parasite can be spread by:
- Swallowing Giardia duodenalis picked up from surfaces (such as bathroom handles, changing tables, diaper pails, or toys) that contain feces (poop) from an infected person or animal
- Drinking water or using ice made from water sources where Giardia duodenalis parasite may live (for example, untreated or improperly treated water from lakes, streams, or wells)
- Swallowing water while swimming or playing in water where Giardia duodenalis parasite may live, especially in lakes, rivers, springs, ponds, and streams
- Eating uncooked food that contains Giardia duodenalis parasites
- Having contact with someone who is ill with giardiasis
- Traveling to countries where giardiasis is common
Anything that comes into contact with feces (poop) from infected humans or animals can become contaminated with the Giardia parasite. People become infected when they swallow the parasite. It is not possible to become infected through contact with blood.
Though Giardia duodenalis infection is commonly thought of as a camping or backpacking-related disease and is sometimes called “Beaver Fever,” anyone can get giardiasis. People more likely to become infected include:
- Children in childcare settings, especially diaper-aged children
- Close contacts of people with giardiasis (for example, people living in the same household) or people who care for those sick with giardiasis
- People who drink water or use ice made from places where Giardia duodenalis may live (for example, untreated or improperly treated water from lakes, streams, or wells)
- Backpackers, hikers, and campers who drink unsafe water or who do not practice good hygiene (for example, proper handwashing)
- People who swallow water while swimming and playing in recreational water where Giardia duodenalis may live, especially in lakes, rivers, springs, ponds, and streams
- International travelers
- People exposed to human feces (poop) through sexual contact
Giardia duodenalis prevention
To prevent and control infection with the Giardia duodenalis parasite, it is important to:
- Practice good hygiene
- Everywhere
- Wash hands with soap and clean, running water for at least 20 seconds; rub your hands together to make a lather and be sure to scrub the backs of your hands, between your fingers, and under your nails.
- Before, during, and after preparing food
- Before eating food
- Before and after caring for someone who is sick
- Before and after treating a cut or wound
- After using the toilet
- After changing diapers or cleaning up a child who has used the toilet
- After blowing your nose, coughing, or sneezing
- After touching an animal or animal waste
- After handling pet food or pet treats
- After touching garbage
- Help young children and other people you are caring for with handwashing as needed.
- Wash hands with soap and clean, running water for at least 20 seconds; rub your hands together to make a lather and be sure to scrub the backs of your hands, between your fingers, and under your nails.
- At childcare facilities
- To reduce the risk of spreading the disease, children with diarrhea should be removed from child care settings until the diarrhea has stopped.
- At recreational water venues (for example, pools, beaches, fountains)
- Protect others by not swimming if you have diarrhea (this is most important for children in diapers).
- Shower before entering the water.
- Wash children thoroughly (especially their bottoms) with soap and water after they use the bathroom or after their diapers are changed and before they enter the water.
- Take children on frequent bathroom breaks and check their diapers often.
- Change diapers in the bathroom, not by the water.
- Around animals
- Minimize contact with the feces (poop) of all animals, especially young animals.
- When cleaning up animal feces (poop), wear disposable gloves and always wash hands when finished.
- Wash hands after any contact with animals or their living areas.
- Minimize contact with the feces (poop) of all animals, especially young animals.
- Outside
- Wash hands after gardening, even if wearing gloves.
- Everywhere
- Avoid water (drinking or recreational) that may be contaminated
- Do not swallow water while swimming in pools, hot tubs, interactive fountains, lakes, rivers, springs, ponds, streams or the ocean.
- Do not drink untreated water from lakes, rivers, springs, ponds, streams, or shallow wells.
- Do not drink poorly treated water or ice made from water during community outbreaks caused by contaminated drinking water.
- Do not use or drink poorly treated water or use ice when traveling in countries where the water supply might be unsafe.
- If the safety of drinking water is in doubt (for example, during or after an outbreak, in a place with poor sanitation or lack of water treatment systems), do one of the following:
- Drink bottled water.
- Disinfect tap water by heating it to a rolling boil for 1 minute.
- Use a filter that has been tested and certified for cyst and oocyst reduction; filtered tap water will need additional treatment to kill or weaken bacteria and viruses.
- Avoid eating food that may be contaminated
- Use safe, uncontaminated water to wash all food that is to be eaten raw.
- After washing vegetables and fruit in safe, uncontaminated water, peel them if you plan to eat them raw.
- Avoid eating raw or uncooked foods when traveling in countries with poor food and water treatment.
- Prevent contact and contamination with feces (poop) during sex
- Use a barrier during oral-anal sex.
- Wash hands right after handling a condom used during anal sex and after touching the anus or rectal area.
Giardia duodenalis cysts are resistant to chlorination. Iodine can be used for disinfection but may take up to 8 hours before the water is safe for drinking. Filters are also available. Travelers should ensure filters meet the National Safety Foundation (NSF) Standard 53 or NSF Standard 58 ratings for oocyst or cyst reduction. Boiling water for 10 minutes also kills Giardia duodenalis cysts 2.
Giardia duodenalis is hard to completely eliminate from the environment, but you can decrease the risk of human infection or of your dog’s or cat’s reinfection if it has been ill. The risk of acquiring Giardia duodenalis infection from your dog or cat is small, but there are some steps you can take to minimize your exposure.
Clean and disinfect your home in this way:
- Hard surfaces (for example: cement and tile floors, pet crates, tables, trash cans, etc.)
- Cleaning
- Wear gloves.
- Remove feces and discard in a plastic bag.
- Clean and scrub surfaces using soap. Rinse surface thoroughly until no obvious visible contamination is present.
- Disinfection
- Wear gloves.
- Disinfect according to manufacturer guidelines using one of the following:
- Follow product instructions, ensuring the product stays in contact with the surface for the recommended amount of time.
- Rinse with clean water.
- Cleaning
- Carpet / Upholstered Furniture
- Cleaning
- Wear gloves.
- If feces are on a carpet or upholstered furniture, remove them with absorbent material (for example, double layered paper towels).
- Place and discard the feces in a plastic bag.
- Clean the contaminated area with regular detergent or carpet cleaning agent.
- Allow carpet or upholstered furniture to fully dry.
- Cleaning
- Disinfection
- Wear gloves.
- Steam clean the area at 158ºF (70ºC) for 5 minutes or 212ºF for 1 minute.
- Quaternary ammonium compound products are found in some carpet cleaning products and can also be used after cleaning to disinfect. Read the product labels for specifications, and follow all instructions.
- Other items (toys, clothing, pet bed, etc.)
- Household items should be cleanedand disinfected daily while a dog or cat is being treated for Giardia infection.
- Dishwasher
- Dishwasher-safe toys and water and food bowls can be disinfected in a dishwasher that has a dry cycle or a final rinse that exceeds one of the following:
- 113ºF (45ºC) for 20 minutes
- 122ºF (50ºC) for 5 minutes
- 162ºF (72.2ºC) for 1 minute
- If a dishwasher is not available, submerge dishwasher-safe items in boiling water for at least 1 minute (at elevations above 6,500 feet, boil for 3 minutes).
- Dishwasher-safe toys and water and food bowls can be disinfected in a dishwasher that has a dry cycle or a final rinse that exceeds one of the following:
- Washer and Dryer
- Clothing, some pet items (for example, bedding and cloth toys) and linens (sheets and towels) can be washed in the washing machine and then heat-dried on the highest heat setting for 30 minutes.
- If a clothes dryer is not available, allow clothes to thoroughly air dry under direct sunlight.
Giardia duodenalis symptoms
Giardia duodenalis infection can cause a variety of intestinal symptoms, which include:
- Diarrhea
- Gas or flatulence
- Greasy stool that can float
- Stomach or abdominal cramps
- Upset stomach or nausea
- Dehydration
These symptoms may also lead to weight loss. Some people with Giardia duodenalis infection have no symptoms at all.
Symptoms of giardiasis normally begin 1 to 3 weeks after becoming infected.
Other, less common symptoms include itchy skin, hives, and swelling of the eye and joints 5. Sometimes, the symptoms of giardiasis might seem to resolve, only to come back again after several days or weeks. Giardiasis can cause weight loss and failure to absorb fat, lactose, vitamin A and vitamin B12 6.
In children, severe giardiasis might delay physical and mental growth, slow development, and cause malnutrition 7.
In otherwise healthy people, symptoms of Giardia duodenalis infection may last 2 to 6 weeks. Occasionally, symptoms last longer. Medications can help decrease the amount of time symptoms last.
Giardia duodenalis complications
Giardiasis can lead to complications, including irritable bowel syndrome (IBS), chronic fatigue syndrome, food allergies, and even reactive arthritis 8. Patients presenting with these conditions should be screened for possible giardia exposure.
Giardia duodenalis diagnosis
Your doctor will ask you to submit stool (poop) samples to see if you are infected. Because Giardia duodenalis cysts can be excreted intermittently, multiple stool collections (i.e., three stool specimens collected on separate days) increase test sensitivity 9. The use of concentration methods and trichrome staining might not be sufficient to identify Giardia duodenalis because variability in the concentration of organisms in the stool can make this infection difficult to diagnose. For this reason, fecal immunoassays that are more sensitive and specific should be used 10.
Rapid immune-chromatographic cartridge assays also are available but should not take the place of routine ova and parasite examination 10. Only molecular testing (e.g., polymerase chain reaction) can be used to identify the subtypes of Giardia.
Giardia duodenalis treatment
The majority of Giardia duodenalis infections will be non-toxic and may only require oral rehydration for initial fluid resuscitation. In more severe Giardia duodenalis infection cases, intravenous (IV) fluids may be needed 11.
Several drugs can be used to treat Giardia infection. Effective treatments include metronidazole, tinidazole, and nitazoxanide 12. Alternatives to these medications include paromomycin, quinacrine, and furazolidone 13. Some of these drugs may not be routinely available in the United States.
Different factors may shape how effective a drug regimen will be, including medical history, nutritional status, and condition of the immune system 14. Therefore, it is important to discuss treatment options with a healthcare provider.
Metronidazole is the first-line treatment for giardiasis 15. Typical dosing is 250 to 500 mg 3 times a day for 5 to 10 days, though studies indicate once-daily dosing may be as effective. Metronidazole should be used with caution in pregnant women, especially in the first trimester, due to concerns for cleft lip. Also, patients should be counseled on avoiding alcohol due to the disulfiram effect (flushing, headaches, and nausea). Metronidazole can also be safely used in children in a typical dose of 30 mg/kg to 50 mg/kg per day divided into three doses.
Other possible regimens include tinidazole, nitazoxanide, mebendazole, albendazole, and paromomycin. Paromomycin is poorly systemically absorbed and may be considered if giardiasis needs to be treated in a pregnant patient in her first trimester 16.
Data appears to be conflicting about the most effective treatment. A systematic review found that albendazole may be as effective as metronidazole with fewer side effects 17. If patients continue to have symptoms despite therapy, a medication from another class should be used.
- Overview of Giardiasis. https://www.merckvetmanual.com/digestive-system/giardiasis-giardia/overview-of-giardiasis[↩]
- Adeyemo FE, Singh G, Reddy P, Bux F, Stenström TA. Efficiency of chlorine and UV in the inactivation of Cryptosporidium and Giardia in wastewater. PLoS ONE. 2019;14(5):e0216040[↩]
- Tangtrongsup S, Scorza V. Update on the diagnosis and management of Giardia spp infections in dogs and cats. Top Companion Anim Med. 2010;25(3):155-62. https://actualidadveterinaria.files.wordpress.com/2011/08/update-on-the-diagnosis-and-management-of-giardia-spp-infections-in-dogs-and-cats.pdf[↩]
- Erickson MC, Ortega YR. Inactivation of protozoan parasites in food, water, and environmental systems. J Food Prot. 2006;69(11):2786-2808. doi:10.4315/0362-028x-69.11.2786[↩]
- Robertson LJ, Hanevik K, Escobedo AA, Mørch K, Langeland N. Giardiasis–why do the symptoms sometimes never stop?. Trends Parasitol. 2010;26(2):75-82. doi:10.1016/j.pt.2009.11.010[↩]
- Gardner TB, Hill DR. Treatment of giardiasis. Clin Microbiol Rev. 2001;14(1):114-28. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC88965/pdf/cm000114.pdf[↩]
- Botero-Garces JH, Garcia-Montoya GM, Grisales-Patino D, Aguirre-Acevedo DC, Alvarez-Uribe MC. Giardia intestinalis and nutritional status in children participating in the complementary nutrition program, Antioquia, Colombia, May to October 2006. Rev Inst Med Trop Sao Paulo. 2009;51(3):155-62. https://doi.org/10.1590/S0036-46652009000300006[↩]
- Litleskare S, Rortveit G, Eide GE, Emberland KE, Hanevik K, Langeland N, Wensaas KA. Quality of life and its association with irritable bowel syndrome and fatigue ten years after giardiasis. Neurogastroenterol. Motil. 2019 May;31(5):e13559[↩]
- Clinical and Laboratory Standards Institute. Procedures for the recovery and identification of parasites from the intestinal tract; approved guideline. CLSI document M28-A2. 2nd ed. Wayne, PA: Clinical Laboratory Standards Institute; 2005.[↩]
- Johnston SP, Ballard MM, Beach MJ, Causer L, Wilkins PP. Evaluation of three commercial assays for detection of Giardia and Cryptosporidium organisms in fecal specimens. J Clin Microbiol. 2003;41(2):623-626. doi:10.1128/jcm.41.2.623-626.2003[↩][↩]
- Stallmach A, Hagel S, Lohse AW. [Diagnostic workup and therapy of infectious diarrhea. Current standards]. Internist (Berl). 2015 Dec;56(12):1353-60.[↩]
- Drugs for Parasitic Infections: The Medical Letter; 2010.[↩]
- Escobedo AA, Cimerman S. Giardiasis: a pharmacotherapy review. Expert Opin Pharmacother. 2007;8(12):1885-1902. doi:10.1517/14656566.8.12.1885[↩]
- Solaymani-Mohammadi S, Genkinger JM, Loffredo CA, Singer SM. A meta-analysis of the effectiveness of albendazole compared with metronidazole as treatments for infections with Giardia duodenalis. PLoS Negl Trop Dis. 2010;4(5):e682. Published 2010 May 11. doi:10.1371/journal.pntd.0000682[↩]
- Iza JA, Iza SN, Olivera MJ. Giardiasis: report of a case refractory to treatment. Infez Med. 2019 Sep 01;27(3):336-339.[↩]
- Krueger A, Schulkin J, L Jones J. Survey of obstetrician-gynecologists about giardiasis. Infect Dis Obstet Gynecol. 2007;2007:21261.[↩]
- Escobedo AA, Almirall P, Chirino E, Pacheco F, Duque A, Avila I. Treatment of refractory paediatric giardiasis using secnidazole plus albendazole: a case series. Infez Med. 2018 Dec 01;26(4):379-384.[↩]