Newborn heel stick procedure
Heel stick is a minimally invasive and easily accessible way of obtaining capillary blood and is the most common way to draw newborn’s blood for various laboratory tests, especially newborn screens and glucose levels. Heel-stick technique is used to collect blood for newborn screening tests, usually before the baby leaves the hospital. Heel sticks are the most commonly performed invasive procedure in neonatal intensive care units (NICU). Thanks to improved laboratory techniques that require smaller sample volumes and improved automated heel lancing devices that minimize trauma and pain 1, heel stick is a viable method of obtaining blood for many routine blood tests 2. Heel stick sampling can also help preserve venous access for future intravenous (IV) lines.
Adequate quantities of serum may be obtained via heel stick in almost any neonate. If done properly, hemolysis should not be a significant problem. The skin’s blood supply is located at the junction of the dermis and subcutaneous tissue, 0.35 to 1.6 mm from the skin surface.
Due to the special technical requirements of this procedure, it is ideal to have experienced staff who perform heel sticks frequently. It is also important to have a program in place to maintain this special skill set. Some evidence exists that in term neonates, skilled venipuncture may result in fewer total punctures and less pain than heel stick. A Cochrane review first published in 1999 and updated in 2011 suggests that it may in fact be the procedure of choice in this population 3. However, these results may not be extrapolatable to preterm infants or infants who require multiple or frequent blood sampling 4. In addition, the development of newer, more effective, and less painful lancing devices may increase the relative utility of heel stick.
Prewarming with the commercially-available heel warmers or with a diaper which has been warmed under a warm faucet and taped around the heel often increases the blood supply and arterializes the sample. The area should be cleaned thoroughly with alcohol swab. The person performing the procedure should wear appropriately fitting gloves.
The heel puncture should be done on the most medial or lateral portions of the plantar surface of the heel, not on the posterior curvature, to avoid the calcaneous. The lancets are designed to enter no deeper than 2-3 mm. If using a scalpel blade, the blade should enter the skin no more than 2-3 mm. After the puncture, wipe the first small drop off to rid the skin of the tissue juices that may increase clotting at the site.
Hold the ankle area with the 3 fingers on your ulnar side while placing your thumb behind the heel and your second finger just below the ventral surface of the toes. By alternately pressing the lateral three fingers , followed by a milking motion of the second finger, blood can be expressed. The fingers should be relaxed for a few seconds periodically to allow refilling. To prevent bruising, caution should be used to limit squeezing with the finger tips. To prevent hemolysis, allow large droplets to form, collecting the drops as they form into the microtube, not scraping the blood into the tube.
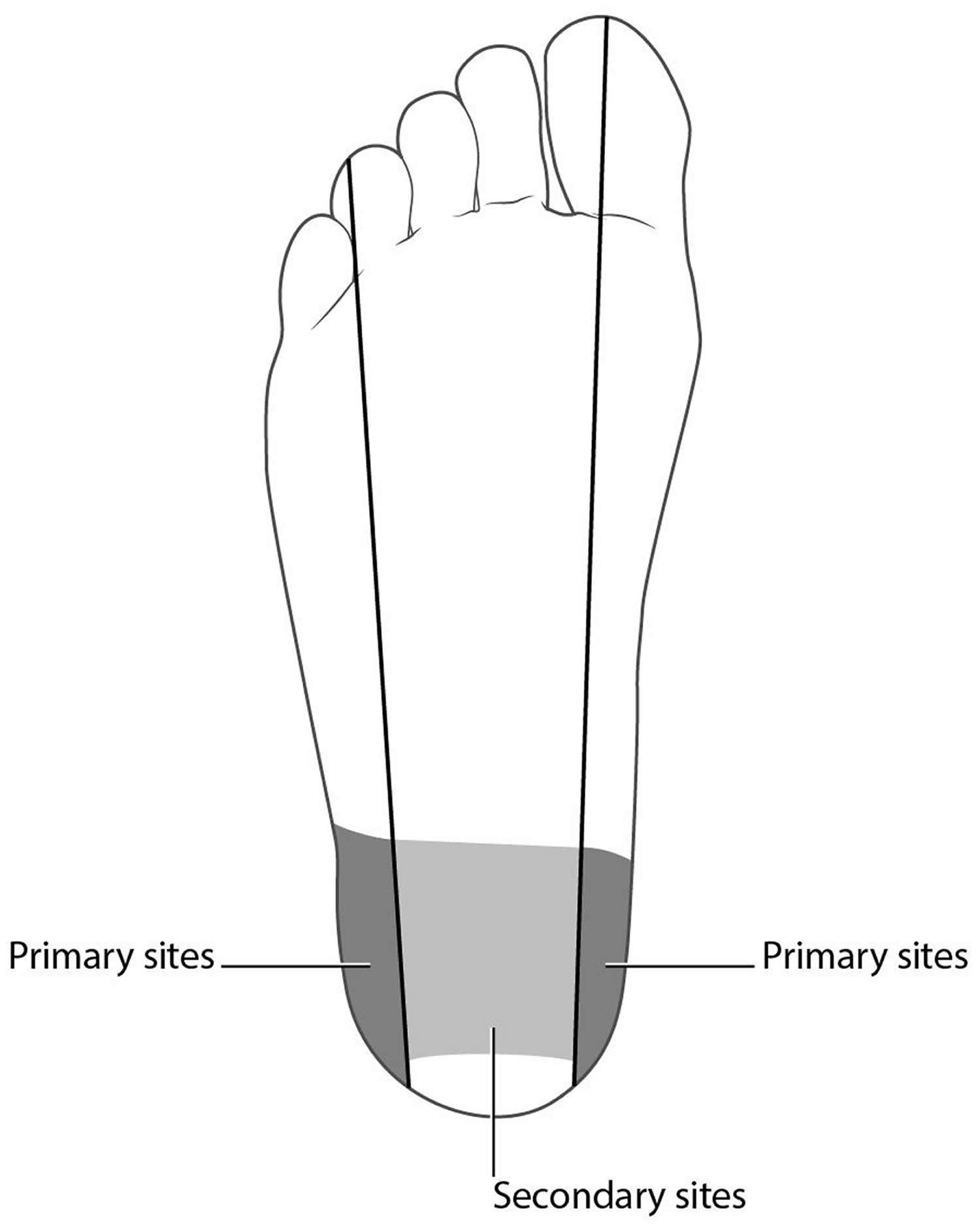
Figure 1. Heel stick location
Footnote: Safest sites for heel stick are outer edges of heel (dark areas). Lighter gray area between outer edges may be used as secondary site if outer areas have been accessed frequently. To avoid damage to calcaneus, posterior pole of heel should not be used.
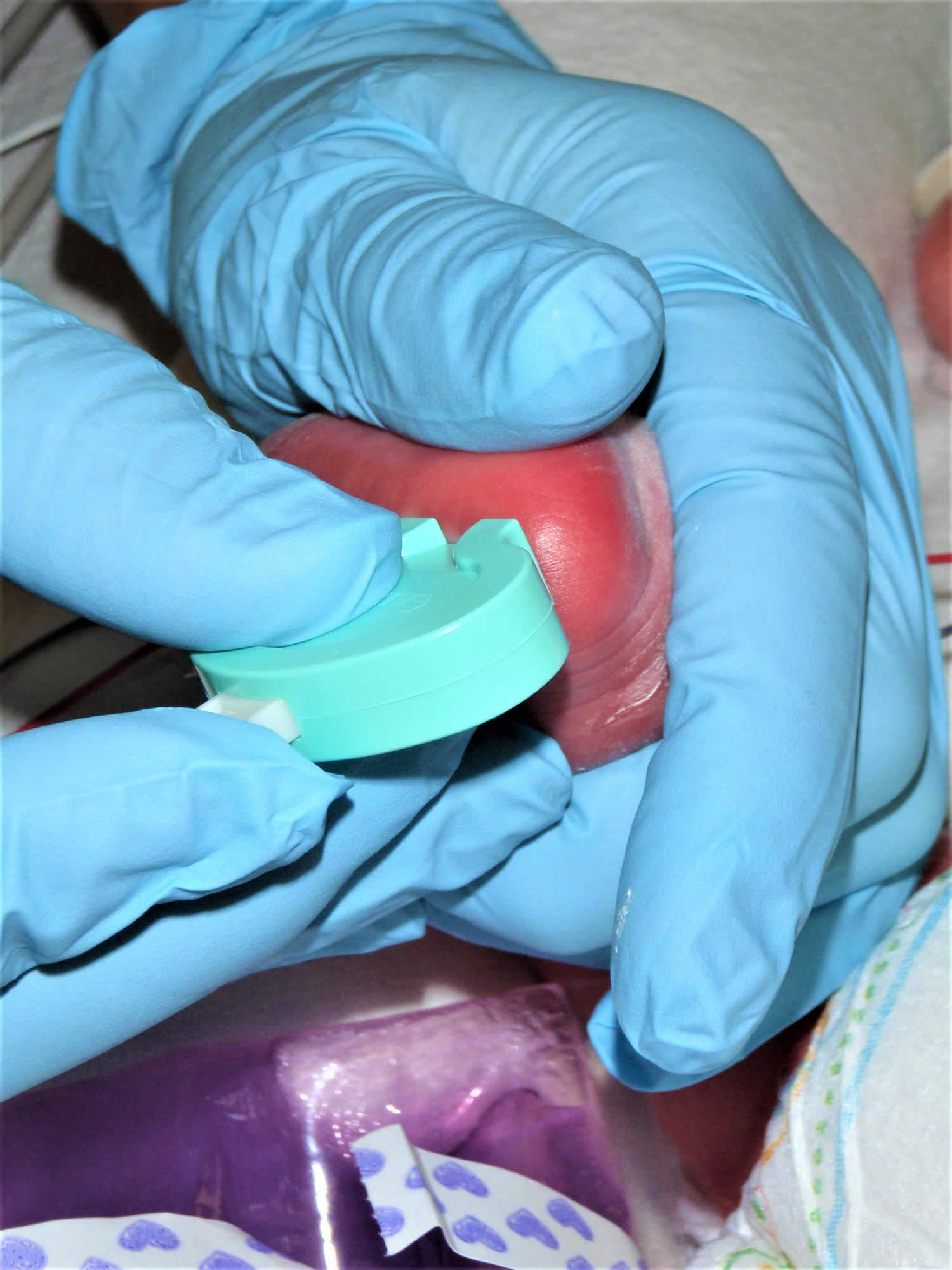
Figure 2. Infant heel stick positioning
Footnote: Infant positioning for heel stick procedure. Note heel warming device in place.
Figure 3. Apply mild pressure between thumb and fingers to hold ankle in dorsiflexion. Do not excessively squeeze heel.
Figure 4. Placement of heel lancing device on outer portion of plantar surface of heel.
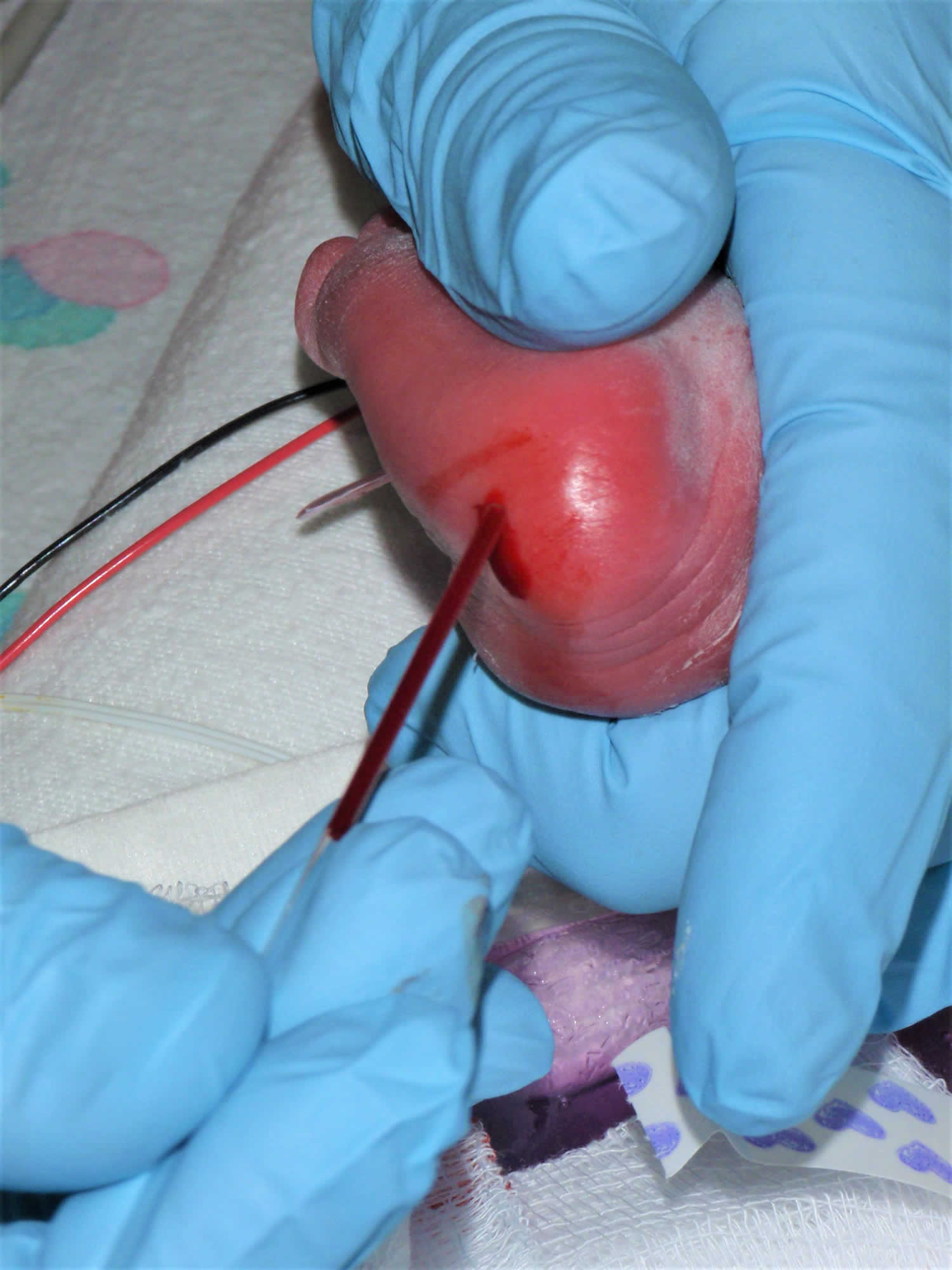
Figure 5. Collection of blood sample from heel stick site. Capillary tube collection is pictured. First drop of blood after incision should be wiped away and not used in sample.
Figure 6. Newborn screening
Newborn heel stick technique and location
Anesthesia
Standard local or systemic pharmacologic anesthesia is not required for heel stick sampling. Local anesthetics may interfere with the quality of the blood sample.
Anesthesia for heel stick in infants can involve oral sucrose, ambient light and noise reduction, and swaddling. Sucrose has been shown to have a substantial anesthetic effect in multiple trials, though an optimal dose has not been definitively established 5. It may be administered with a dropper, a needleless syringe, or a pacifier dipped in a dose of approximately 0.1-1 mL.
Swaddling, bringing the infant’s hands to the midline, and minimizing environmental stimulation has also been shown to have an effect on how infants tolerate this painful procedure 6.
Positioning
Developmentally appropriate positioning, should be implemented when possible. The heel stick sample is obtained most easily with the infant supine (see Figure 2 above).
Proper site selection (see Figure 1 above) is important for minimizing pain and avoiding contact with the calcaneus. The posterior pole of the heel should not be used for a heel stick, because this site is where the calcaneus is in its most superficial position 7.
Heel stick sampling
If heel warming is desired, apply a heel warmer according to the manufacturer’s directions for approximately 5 minutes before performing the heel stick. Some studies have found heel warming to offer no improvement in blood volume collected 8.
Put on gloves. Prepare the automated heel-lancing device according to the manufacturer’s directions. A heel-lancing device (eg, Tenderfoot [ITC Medical, Edison, NJ] or Quikheel Lancet [BD, Franklin Lakes, NJ]), sized appropriately for the infant’s weight – A 0.65 mm incision depth is appropriate for infants weighing 1 kg or less; a 0.85 mm incision depth is appropriate for small-for-gestational-age (SGA) infants and premature infants who weigh more than 1 kg; and a 1 mm incision depth is appropriate for term infants aged 6 months or younger.
Prepare an adequate area around the heel stick site with antiseptic solution.
Position the heel between thumb and forefinger, with the fingers underneath the calf and posterior ankle and the thumb over the ball of foot or arch (see Figure 3 above). Apply a small amount of pressure to place the foot in a comfortable dorsiflexed position.
Place the automated lancing device on the appropriate area on the side of the heel (see Figure 4 above), then activate it.
Apply mild pressure with thumb and fingers. Avoid excessive squeezing or milking of the heel; this may lead to greater hemolysis and more pain.
Wipe away the first drop of blood, and collect the sample. Fill the capillary tube by touching the open tip of the tube to a blood drop, which is drawn into the tube by capillary action. Collect blood drops into hematology or chemistry tubes (see Figure 5 above), taking care to avoid excessive scooping of blood from the adjacent skin with the lip of the collection tube, which can interfere with test results.
Blot blood drops onto appropriate areas on the filter paper according to the laboratory’s instructions (see Figure 6 above); methods of collecting filter paper samples for newborn screens have strict guidelines and vary between laboratories. If blood stops flowing, try to wipe away any clot that may have formed at the incision site with gauze or an alcohol wipe. Release pressure to allow capillary refill, then reapply pressure to allow a blood drop to form again.
When sampling is complete, apply pressure to the incision site until bleeding stops. Apply gauze or a bandage.
Heel stick indications
Heel stick blood sampling is indicated whenever capillary blood is an acceptable source. Such situations include the following:
- The sample required is relatively small
- Another acceptable source of blood (eg, central venous catheter, umbilical catheter, arterial line) is not already available
Heel stick samples can be used for general chemistries and liver function tests, complete blood counts (CBCs), toxicology, newborn screening, bedside glucose monitoring, and blood gas analysis 9.
Heel stick contraindications
Heel stick should not be performed if any significant injury, infection, anomaly, or edema is present on the sampling area of the heel 10.
At present, coagulation studies may not be performed with capillary samples. Blood tests that require relatively larger sample volumes may not be feasible with heel stick samples. Blood cultures require perfectly sterile technique and, therefore, may not be done with samples obtained via heel stick. Certain other sophisticated tests may also not be performed on heel stick samples (eg, chromosomal analyses and certain immunoglobulins and titers).
When ordering a laboratory test that is sent to another facility or is out of the ordinary, check with the laboratory to determine which type of blood sample is required.
When is the heel-stick method used to draw blood from infants?
The answer to this question depends on the baby’s developmental milestones. While fingers are the site of choice after infancy, heel sticks are appropriate for most babies, including premature infants, neonates, and even babies 4 to 7 months old. The only caveat is that babies discover other parts of their bodies, such as their feet and toes, as they grow older.
A bandage placed on a baby’s heel can pose a safety risk when the child is able to place its feet in its mouth. By 8 to 12 months, babies are pulling themselves up, standing, and preparing to walk or walking; so heel sticks are not recommended at this developmental stage because the heels are bearing weight to varying degrees. Premies may not reach such milestones on the same schedule as full-term babies, so parents should be questioned about their child’s development before performing a heel stick.
Heel sticks complications
Complications of heel stick include the following:
- Pain 11
- Infection (cellulitis, abscess, osteomyelitis)
- Scarring
- A too-deep incision (potentially making contact with calcaneus)
- Inaccurate results (eg, hemolysis causing hyperkalemia, air bubbles causing erroneous blood gas results, platelet clumping)
Improper heel-stick technique can damage the structures of the foot, including the calcaneus bone and soft tissues. In fact, some reports have documented difficulties walking later in life. It is safe to perform a heel stick if the puncture site is limited to the medial and lateral planter aspects of each heel pad, specifically medial to a visual line drawn from the middle of the big toe extending posterior to the heel or lateral to a line drawn from between the fourth and fifth toes and extending posterior to the heel. Repeated punctures, bruising, or redness (erythema) limit the available area for punctures, especially in premature infants who may have blood drawn multiple times or very tiny heels.
Are there other safety risks associated with heel sticks?
Yes, there is also a risk of burning the baby’s skin while warming its heel before the blood is drawn. Heel warming is used to increase blood flow in the capillaries. If the heel is to be warmed, using warm water submersion is risky unless you tightly control the temperature.
Chemical heat packs are single-use, and offer a temperature-controlled, safer, but more expensive alternative. Though heel warming is commonly performed to increase blood flow, this protocol is actually based more on theoretical grounds than on any solid evidence that it works. Two studies have claimed that heel warming does not increase blood flow; however, the studies were not blinded 12. It is costly in terms of time and consumables, so a well-designed study to resolve this question would be welcome.
Are finger sticks on infants safe?
Yes, they can be performed with special safety measures. Special lancets less than 1.5-mm thick can be used once heel sticks are no longer an option and after 6 months of age. At that age, distance from the skin surface to bone and cartilage in the middle finger is only 2.5 mm 13.
Finger stick sampling is used for capillary blood gas analysis in neonatal intensive care unit (NICU) and may be used for additional laboratories as well. The technique is similar to heel stick in that only the medial and lateral aspects of the finger are stuck. The milking motion includes the whole finger and even portions of the hand.
- Vertanen H, Fellman V, Brommels M, et al. An automatic incision device for obtaining blood samples from the heels of preterm infants causes less damage than a conventional manual lancet. Arch Dis Child Fetal Neonatal Ed. 2001 Jan. 84(1):F53-5.[↩]
- American Association for Respiratory Care. Capillary Blood Gas Sampling for Neonatal & Pediatric Patients. Respiratory Care. 2001. 46(5):506-513.[↩]
- Shah VS, Ohlsson A. Venepuncture versus heel lance for blood sampling in term neonates. Cochrane Database Syst Rev. 2011 Oct 5. CD001452.[↩]
- D’Apolito KC. State of the science: procedural pain management in the neonate. J Perinat Neonatal Nurs. 2006 Jan-Mar. 20(1):56-61.[↩]
- Stevens B, Yamada J, Ohlsson A. Sucrose for analgesia in newborn infants undergoing painful procedures. Cochrane Database Syst Rev. 2010 Jan 20. CD001069[↩]
- Folk LA. Guide to capillary heelstick blood sampling in infants. Adv Neonatal Care. 2007 Aug. 7(4):171-8.[↩]
- Arena J, Emparanza JI, Nogues A, et al. Skin to calcaneus distance in the neonate. Arch Dis Child Fetal Neonatal Ed. 2005 Jul. 90(4):F328-f331.[↩]
- Janes M, Pinelli J, Landry S, et al. Comparison of capillary blood sampling using an automated incision device with and without warming the heel. J Perinatol. 2002 Mar. 22(2):154-8.[↩]
- Algeciras-Schimnich A, Cook WJ, Milz TC, Saenger AK, Karon BS. Evaluation of hemoglobin interference in capillary heel-stick samples collected for determination of neonatal bilirubin. Clin Biochem. 2007 Nov. 40(16-17):1311-6.[↩]
- Folk L. Capillary heelstick blood sampling. MacDonald MG, Ramasethu J, eds. Atlas of Procedures in Neonatology. 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2007. 93-6.[↩]
- Herrington CJ, Chiodo LM. Human touch effectively and safely reduces pain in the newborn intensive care unit. Pain Manag Nurs. 2014 Mar. 15 (1):107-15.[↩]
- Janus M, Pinelli J. Comparison of blood sampling using an automated incision device with and without warming the heel. J Perinatol 2002;22:154–8.[↩]
- Reiner CB, Meites S, Hayes JR. Optimal sites and depths for skin puncture of infants and children as assessed from anatomical measurements. Clin Chem 1990;36:547–9.[↩]