Helminthiasis
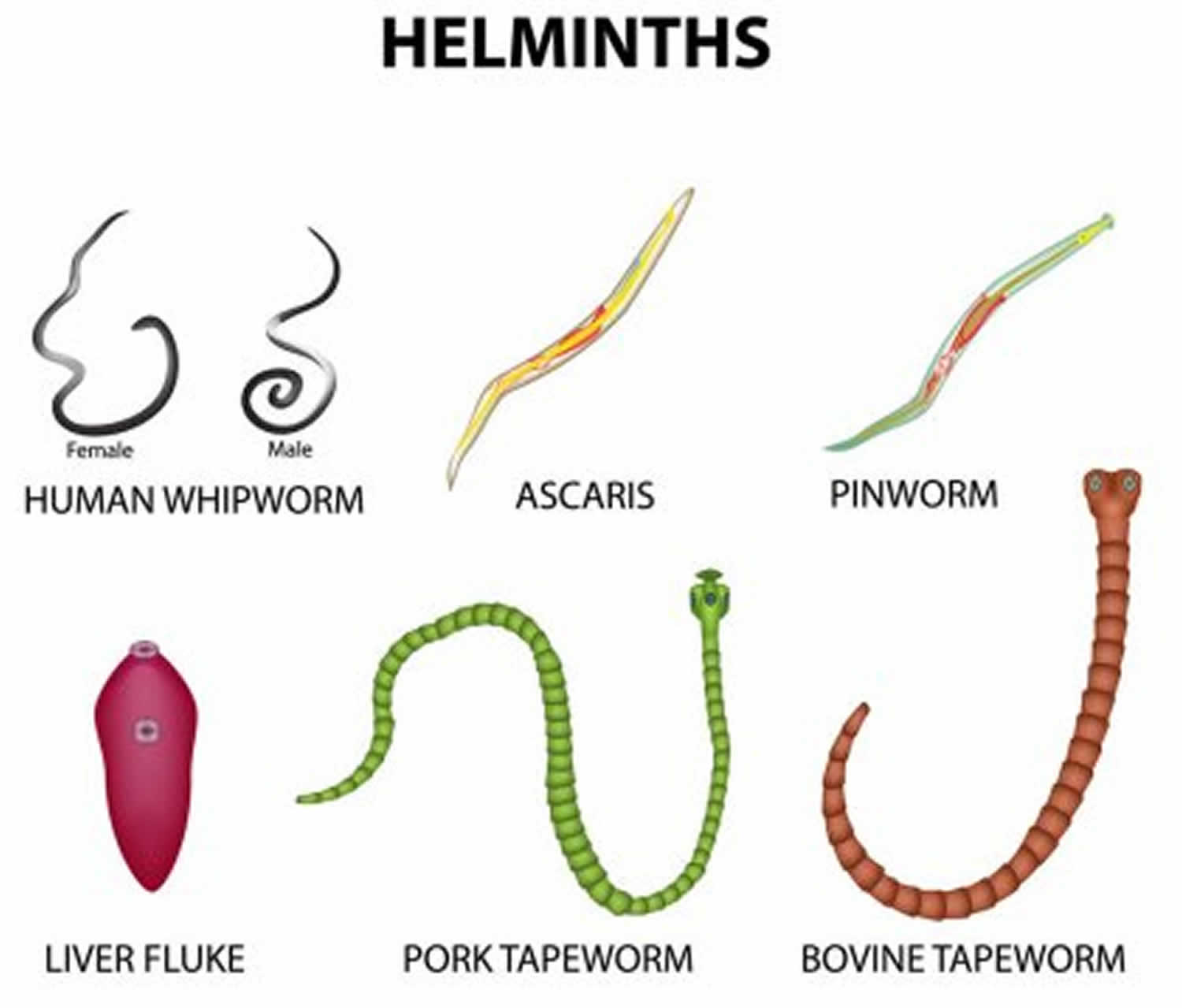
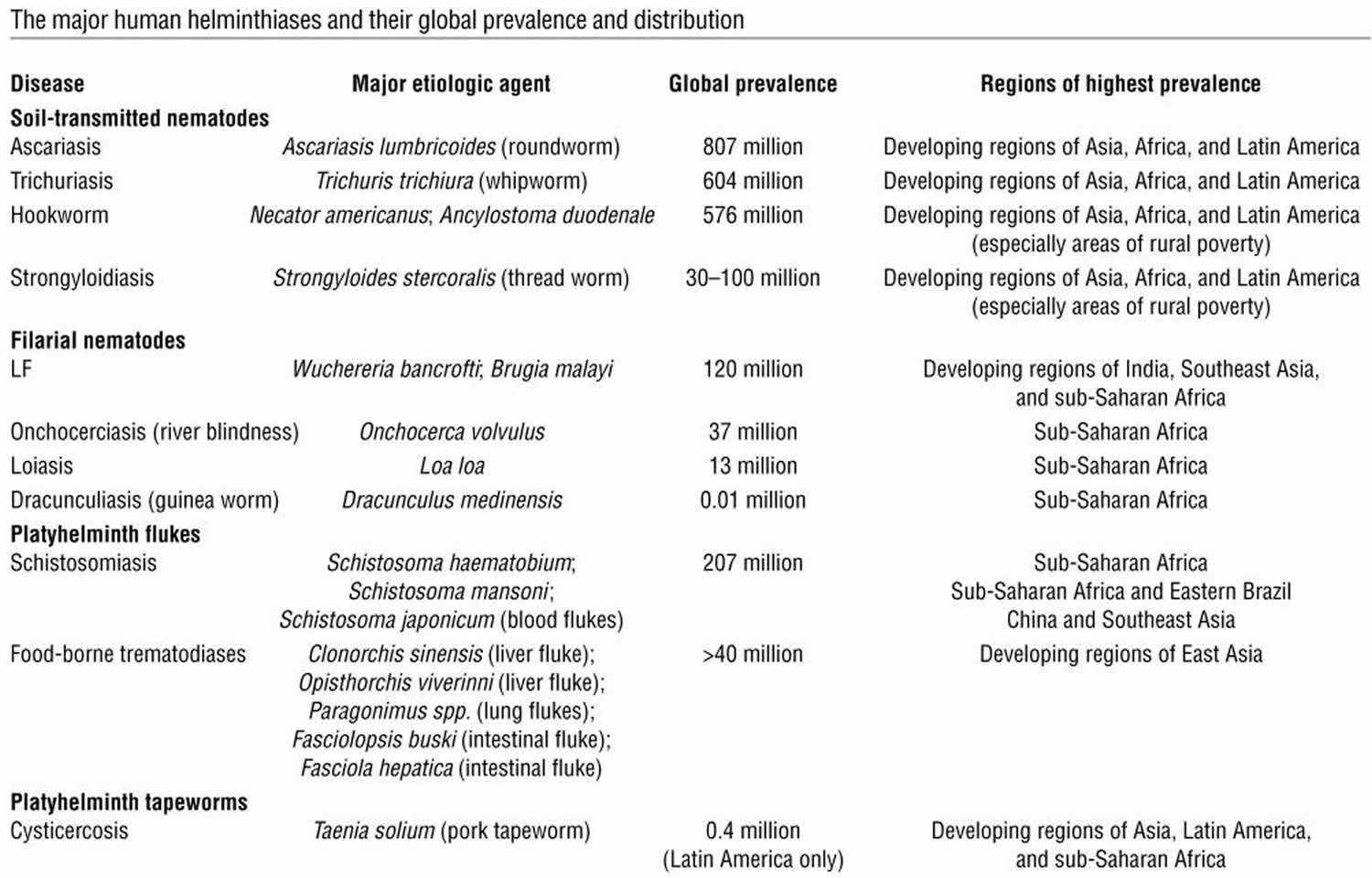
Helminthiasis also called intestinal helminthiasis is a medical term for intestinal parasitic worm (helminth) infection. Helminths are parasitic worms that infect the intestine and are transmitted via contaminated soil. There are two major phyla of helminths. The nematodes also known as roundworms include the major intestinal worms (also known as soil-transmitted helminths) and the filarial worms that cause lymphatic filariasis and onchocerciasis, whereas the platyhelminths (also known as flatworms) include the flukes (also known as trematodes), such as the schistosomes, and the tapeworms (also known as the cestodes), such as the pork tapeworm that causes cysticercosis (Table 1) 1. The most common helminthiases are those caused by infection with intestinal helminths, Ascaris lumbricoides (sometimes called just “Ascaris“ or ascariasis), trichuriasis or whipworm (Trichuris trichiura) and hookworm (Anclostoma duodenale and Necator americanus), followed by schistosomiasis (Schistosoma haematobium, Schistosoma japonicum and Schistosoma mansoni) and lymphatic filariasis (Wuchereria bancrofti, Brugia malayi and Brugia timori) (Table 1). A large part of the world’s population is infected with one or more of these helminths, and the prevalence is highest in tropical and subtropical countries where water supplies and sanitation are poor. These soil-transmitted helminths are considered Neglected Tropical Diseases because they inflict tremendous disability and suffering yet can be controlled or eliminated 2:
- approximately 807-1,121 million with Ascaris lumbricoides
- approximately 604-795 million with whipworm (Trichuris trichiura)
- approximately 576-740 million with hookworm (Anclostoma duodenale and Necator americanus)
Soil-transmitted helminth infection is found mainly in areas with warm and moist climates where sanitation and hygiene are poor, including in temperate zones during warmer months. Travelers to these countries should be at low risk of infection if preventive measures are taken. Infections in the United States are typically seen in immigrant and refugee populations. Since these worms do not multiply in hosts, reinfection occurs only as a result of additional contacts with the infective stages.
Soil-transmitted helminths live in the intestine and their eggs are passed in the feces of infected persons. If an infected person defecates outside (near bushes, in a garden, or field) or if the feces of an infected person are used as fertilizer, eggs are deposited on soil. Ascaris and hookworm eggs become infective as they mature in soil. People are infected with Ascaris and whipworm when eggs are ingested. This can happen when hands or fingers that have contaminated dirt on them are put in the mouth or by consuming vegetables and fruits that have not been carefully cooked, washed or peeled. Hookworm eggs are not infective. They hatch in soil, releasing larvae (immature worms) that mature into a form that can penetrate the skin of humans. Hookworm infection is transmitted primarily by walking barefoot on contaminated soil. One kind of hookworm (Anclostoma duodenale) can also be transmitted through the ingestion of larvae.
People with light soil-transmitted helminth infections usually have no symptoms. Heavy infections can cause a range of health problems, including abdominal pain, diarrhea, blood and protein loss, rectal prolapse, and physical and cognitive growth retardation. Soil-transmitted helminth infections are treatable with medication prescribed by your health care provider.
Table 1. Major human helminthiases and their global prevalence and distribution
[Source 1 ]Helminthiasis disease
Hookworm
Hookworms (Anclostoma duodenale and Necator americanus) live in the small intestine of humans. Hookworm eggs are passed in the feces of an infected person. If the infected person defecates outside (near bushes, in a garden, or field) of if the feces of an infected person are used as fertilizer, eggs are deposited on soil. They can then mature and hatch, releasing larvae (immature worms). The larvae mature into a form that can penetrate the skin of humans. Hookworm infection is mainly acquired by walking barefoot on contaminated soil. One kind of hookworm can also be transmitted through the ingestion of larvae.
High-intensity hookworm infections occur among both school-age children and adults. An estimated 576-740 million people in the world are infected with hookworm. Hookworm was once widespread in the United States, particularly in the southeastern region, but improvements in living conditions have greatly reduced hookworm infections.
Most people infected with hookworms have no symptoms. Some have gastrointestinal symptoms, especially persons who are infected for the first time. The most serious effects of hookworm infection are blood loss at the site of the intestinal attachment of the adult worms leading to anemia, in addition to protein deficiency. When children are continuously infected by many worms, the loss of iron and protein can retard growth and mental development.
Hookworm infections are treatable with medication prescribed by your health care provider.
How is hookworm spread?
Hookworm eggs are passed in the feces of an infected person. If an infected person defecates outside (near bushes, in a garden, or field) or if the feces from an infected person are used as fertilizer, eggs are deposited on soil. They can then mature and hatch, releasing larvae (immature worms). The larvae mature into a form that can penetrate the skin of humans. Hookworm infection is transmitted primarily by walking barefoot on contaminated soil. One kind of hookworm (Ancylostoma duodenale)can also be transmitted through the ingestion of larvae.
How can I prevent hookworm infection?
Do not walk barefoot in areas where hookworm is common and where there may be fecal contamination of the soil. Avoid other skin-to-soil contact and avoid ingesting such soil. Fecal contamination occurs when people defecate outdoors or use human feces as fertilizer.
The infection of others can be prevented by not defecating outdoors or using human feces as fertilizer, and by effective sewage disposal systems.
Who is at risk for hookworm infection?
People living in areas with warm and moist climates and where sanitation and hygiene are poor are at risk for hookworm infection if they walk barefoot or in other ways allow their skin to have direct contact with contaminated soil. Soil is contaminated by an infected person defecating outside or when human feces (“night soil”) are used as fertilizer. Children who play in contaminated soil may also be at risk.
Hookworm signs and symptoms
Itching and a localized rash are often the first signs of hookworm infection. These symptoms occur when the larvae penetrate the skin. A person with a light infection may have no symptoms. A person with a heavy infection may experience abdominal pain, diarrhea, loss of appetite, weight loss, fatigue and anemia. The physical and cognitive growth of children can be affected.
How is hookworm diagnosed?
Health care providers can diagnose hookworm by taking a stool sample and using a microscope to look for the presence of hookworm eggs. Because eggs may be difficult to find in light infections, a concentration procedure is recommended. Concentration procedure separate parasites from fecal debris and increase the chances of detecting parasitic organisms when these are in small numbers. They are divided into flotation techniques and sedimentation techniques 3.
- Flotation techniques (most frequently used: zinc sulfate or Sheather’s sugar) use solutions which have higher specific gravity than the organisms to be floated so that the organisms rise to the top and the debris sinks to the bottom. The main advantage of this technique is to produce a cleaner material than the sedimentation technique. The disadvantages of most flotation techniques are that the walls of eggs and cysts will often collapse, thus hindering identification. Also, some parasite eggs do not float.
- Sedimentation techniques use solutions of lower specific gravity than the parasitic organisms, thus concentrating the latter in the sediment. Sedimentation techniques are recommended for general diagnostic laboratories because they are easier to perform and less prone to technical errors. The sedimentation technique used at Centers for Disease Control and Prevention (CDC) is the formalin-ethyl acetate technique, a diphasic sedimentation technique that avoids the problems of flammability of ether, and which can be used with specimens preserved in formalin, MIF or SAF.
Formalin-Ethyl Acetate Sedimentation Concentration
- Mix the specimen well.
- Strain 5ml of the fecal suspension (more or less depending on its consistency) through wetted cheesecloth-type gauze placed over a disposable paper funnel into a 15 ml conical centrifuge tube. (Conical paper cups with the tips cut off are sufficient).
- Add 0.85% saline or 10% formalin through the debris on the gauze to bring the volume in the centrifuge tube to 15 ml. Distilled water may be used; however, Blastocystis hominis may be deformed or destroyed.
- Centrifuge at 500 × g for 10 minutes.
- Decant supernatant. Add 10 ml of 10% formalin to the sediment and mix thoroughly with wooden applicator sticks.
- Add 4 ml of ethyl acetate, stopper the tube, and shake vigorously in an inverted position for 30 seconds. Carefully remove the stopper.
- Centrifuge at 500 × g for 10 minutes.
- Free the plug of debris from the top of the tube by ringing the sides with an applicator stick. Decant the top layers of supernatant.
- Use a cotton-tipped applicator to remove debris from sides of the centrifuge tube.
- Add several drops of 10% formalin to resuspend the concentrated specimen. Proceed with applicable testing.
*Commercial fecal concentration tubes are available that decrease processing time and supplies needed for concentrating specimens (e.g., Fecal Parasite Concentrator, Evergreen Scientific).
Specimens preserved in PVA are mostly used for permanent staining with trichrome. Prior to staining, they are processed as follows:
- Insure that the specimen is well mixed.
- Prepare a smear using 2 to 3 drops of the specimen depending on density.
- Heat fix on slide warmer set at 60°C for 5 minutes or air dry completely at room temperature.
Slides may be trichrome stained or kept for several months in a protective slide tray or box for future staining.
What is the treatment for hookworm?
Hookworm infection is treated with anthelminthic medications (drugs that rid the body of parasitic worms), such as albendazole, mebendazole, or pyrantel pamoate for 1-3 days as prescribed by your health care provider. Dosage is the same for children as for adults. Albendazole should be taken with food. Albendazole is not FDA-approved for treating hookworm infection. The recommended medications are effective and appear to have few side effects. Iron supplements may be prescribed if you have anemia.
| Drug | Dosage for adults and children |
|---|---|
| Albendazole | 400 mg orally once |
| Mebendazole | 100 mg orally twice a day for 3 days or 500 mg orally once |
| Pyrantel pamoate | 11 mg/kg (up to a maximum of 1 g) orally daily for 3 days |
Ascariasis
An estimated 807 million–1.2 billion people in the world are infected with Ascaris lumbricoides (sometimes called just Ascaris or ascariasis). Ascariasis is now uncommon in the United States.
Humans can also be infected by pig roundworm (Ascaris suum). Ascaris lumbricoides (human roundworm) and Ascaris suum (pig roundworm) are indistinguishable. It is unknown how many people worldwide are infected with Ascaris suum (pig roundworm).
Ascaris parasites live in the small intestine and Ascaris eggs are passed in the feces (poop) of infected people. If an infected person defecates outside (for example, near bushes, in a garden, or in a field), or if the feces of an infected person are used as fertilizer, eggs are deposited on soil. The eggs can then mature into a form of the parasite that is infective. Ascariasis is caused by ingesting eggs. This can happen when hands or fingers that have contaminated dirt on them are put in the mouth, or by consuming vegetables or fruits that have not been carefully cooked, washed, or peeled.
People infected with Ascaris often show no symptoms. If symptoms do occur they can be light and include abdominal discomfort. Heavy infections can cause intestinal blockage and impair growth in children. Other symptoms such as cough are due to migration of the worms through the body. Ascariasis is treatable with medication prescribed by your health care provider.
How is ascariasis spread?
Ascaris lives in the intestine and Ascaris eggs are passed in the feces of infected persons. If the infected person defecates outside (near bushes, in a garden, or field), or if the feces of an infected person are used as fertilizer, then eggs are deposited on the soil. They can then mature into a form that is infective. Ascariasis is caused by ingesting infective eggs. This can happen when hands or fingers that have contaminated dirt on them are put in the mouth or by consuming vegetables or fruits that have not been carefully cooked, washed or peeled.
How can I prevent Ascaris infection?
The best way to prevent people from getting ascariasis from humans or pigs is to always do the following:
- Avoid ingesting soil that may be contaminated with human or pig feces, including where human fecal matter (“night soil”), wastewater, or pig manure is used to fertilize crops.
- Wash your hands with soap and water before handling food.
- Wash your hands with soap and water after touching or handling pigs, cleaning pig pens, or handling pig manure.
- Teach children the importance of washing hands to prevent infection.
- Supervise children around pigs, ensuring that they do not put unwashed hands in their mouths.
- Wash, peel, or cook all raw vegetables and fruits before eating, particularly those that have been grown in soil that has been fertilized with manure.
Transmission of Ascaris lumbricoides infection to others in a community setting can be prevented by:
- Not defecating outdoors.
- Effective sewage disposal systems.
Ascaris suum (pig roundworm) eggs left in the soil from pigs can survive for up to 10 years. The eggs are very hardy and can survive extreme environmental conditions like freezing and extreme heat. It is virtually impossible to completely remove Ascaris suum eggs from the environment where an infected pig has been present. Consult a veterinarian for recommendations on preventing and controlling Ascaris suum in your pigs.
Who is at risk for Ascaris infection?
Infection occurs worldwide in warm and humid climates, where sanitation and hygiene are poor, including in temperate zones during warmer months. Persons in these areas are at risk if soil contaminated with human feces enters their mouths or if they eat vegetables or fruit that have not been carefully washed, peeled or cooked. Ascariasis is now uncommon in the United States.
What are the symptoms of ascariasis?
People infected with Ascaris often show no symptoms, regardless of the species of worm. If symptoms do occur they can be light and include abdominal discomfort. Heavy infections can cause intestinal blockage and impair growth in children. Other symptoms such as cough are due to migration of the worms through the body.
How is ascariasis diagnosed?
Health care providers can diagnose ascariasis by taking a stool sample and using a microscope to look for the presence of eggs. Because eggs may be difficult to find in light infections, a concentration procedure is recommended.
Some people notice infection when a worm is passed in their stool or is coughed up. If this happens, bring in the worm specimen to your health care provider for diagnosis.
What is the treatment for ascariasis?
Ascariasis is treated with albendazole, mebendazole, or ivermectin for 1-3 days. Dosage is the same for children as for adults. Albendazole should be taken with food. Ivermectin should be taken on an empty stomach with water. Albendazole is not FDA-approved for treating ascariasis, and the safety of ivermectin for treating children who weigh less than 15 kg has not been established. The recommended medications are effective.
| Drug | Dosage |
|---|---|
| Albendazole | 400 mg orally once |
| Mebendazole | 100 mg orally twice daily for 3 days or 500 mg orally once |
| Ivermectin | 150-200 mcg/kg orally once |
Whipworm infection or Trichuriasis
Whipworms (Trichuris trichiura) live in the large intestine and whipworm eggs are passed in the feces of infected persons. If the infected person defecates outside (near bushes, in a garden, or field) or if human feces as used as fertilizer, eggs are deposited on soil. They can then mature into a form that is infective. Whipworm infection is caused by ingesting eggs. This can happen when hands or fingers that have contaminated dirt on them are put in the mouth or by consuming vegetables or fruits that have not been carefully cooked, washed or peeled.
An estimated 604-795 million people in the world are infected with whipworm.
People infected with whipworm can suffer light or heavy infections. People with light infections usually have no symptoms. People with heavy symptoms can experience frequent, painful passage of stool that contains a mixture of mucus, water, and blood. Rectal prolapse can also occur. Children with heavy infections can become severely anemic and growth-retarded. Whipworm infections are treatable with medication prescribed by your health care provider.
How is whipworm spread?
Whipworms live in the large intestine and whipworm eggs are passed in the feces of infected persons. If the infected person defecates outside (near bushes, in a garden, or field), or if the feces of an infected person are used as fertilizer, then eggs are deposited on the soil. They can then mature into a form that is infective. Roundworm infection is caused by ingesting eggs. This can happen when hands or fingers that have contaminated dirt on them are put in the mouth, or by consuming vegetables or fruits that have not been carefully cooked, washed or peeled.
How can I prevent whipworm infection?
- Avoid contact with soil that may be contaminated with human feces, including with human fecal matter (“night soil”) used to fertilize crops.
- Wash your hands with soap and warm water before handling food.
- Teach children the importance of washing hands to prevent infection.
- Wash, peel, or cook all raw vegetables and fruits before eating, particularly those that have been grown in soil that has been fertilized with manure.
Transmission of whipworm infection to others can be prevented by
- not defecating outdoors, and by
- effective sewage disposal systems.
Who is at risk for whipworm infection?
Whipworm infection occurs worldwide in warm and humid climates where sanitation and hygiene are poor, including in temperate climates during warmer months. Persons in these areas are at risk if soil contaminated with human feces enters their mouths or if they eat vegetables or fruits that have not been carefully washed, peeled or cooked.
What are the signs and symptoms of whipworm?
People with light whipworm infections usually have no signs or symptoms. People with heavy infections can experience frequent, painful passage of stool that contains a mixture of mucus, water, and blood. The diarrhea typically has an acrid smell. In severe cases growth retardation can occur. Rectal prolapse can also occur. In children, heavy infection may be associated with growth retardation and impaired cognitive development.
How is whipworm diagnosed?
Health care providers can diagnose whipworm by taking a stool sample. By using a microscope, providers can look for the presence of whipworm eggs.
What is the treatment for whipworm?
Whipworm is effectively treated with albendazole, mebendazole or ivermectin. Each drug needs to be taken for 3 days. Dosage guidelines are the same for children as for adults. Albendazole should be taken with food. Ivermectin should be taken with water on an empty stomach and the safety of ivermectin for children weighing less than 15 kg has not been established. Neither albendazole nor ivermectin is FDA-approved for treating whipworm. The drugs are effective and appear to have few side effects.
| Drug | Dosage for adults and children |
|---|---|
| Albendazole | 400 mg orally for 3 days |
| Mebendazole | 100 mg orally twice a day for 3 days |
| Ivermectin | 200 mcg/kg/day orally for 3 days |
Helminthiasis causes
Common soil-transmitted helminths are Ascaris lumbricoides (sometimes called just “Ascaris“), whipworm (Trichuris trichiura), and hookworm (Anclostoma duodenale and Necator americanus). A large part of the world’s population is infected with one or more of these soil-transmitted helminths 2:
- approximately 807-1,121 million with Ascaris lumbricoides
- approximately 604-795 million with whipworm (Trichuris trichiura)
- approximately 576-740 million with hookworm (Anclostoma duodenale and Necator americanus)
Helminthiasis prevention
To avoid hookworm infection, travelers should not walk barefoot in areas where hookworm is common and where there may be human fecal contamination of the soil. In general, avoid ingesting soil that may be contaminated with human feces, including where human fecal matter or wastewater is used to fertilize crops.
Helminthiasis symptoms
Most intestinal helminth infections are asymptomatic, especially when few worms are present. Pulmonary symptoms (Löffler syndrome) occur in a small percentage of patients when roundworm larvae pass through the lungs. Löffler syndrome is associated with fever and marked eosinophilia. Roundworms can also cause intestinal discomfort, obstruction, and impaired nutritional status. Hookworm infection can lead to anemia due to blood loss and chronic protein deficiency. Whipworm infection can cause chronic abdominal pain, diarrhea, blood loss, dysentery, and rectal prolapse. However, travelers are rarely at risk, because these more severe manifestations are generally associated with high worm burdens seen in indigenous populations.
Helminthiasis diagnosis
The standard method for diagnosing soil-transmitted helminths is by identifying eggs in a stool specimen using a microscope.
Helminthiasis treatment
The drugs most commonly used are albendazole and mebendazole.
- Hotez PJ, Brindley PJ, Bethony JM, King CH, Pearce EJ, Jacobson J. Helminth infections: the great neglected tropical diseases. J Clin Invest. 2008;118(4):1311-1321. doi:10.1172/JCI34261 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2276811[↩][↩]
- Parasites – Soil-transmitted helminths. https://www.cdc.gov/parasites/sth[↩][↩]
- Stool Specimens – Specimen Processing. https://www.cdc.gov/dpdx/diagnosticprocedures/stool/specimenproc.html[↩]