What is Lambert-Eaton syndrome
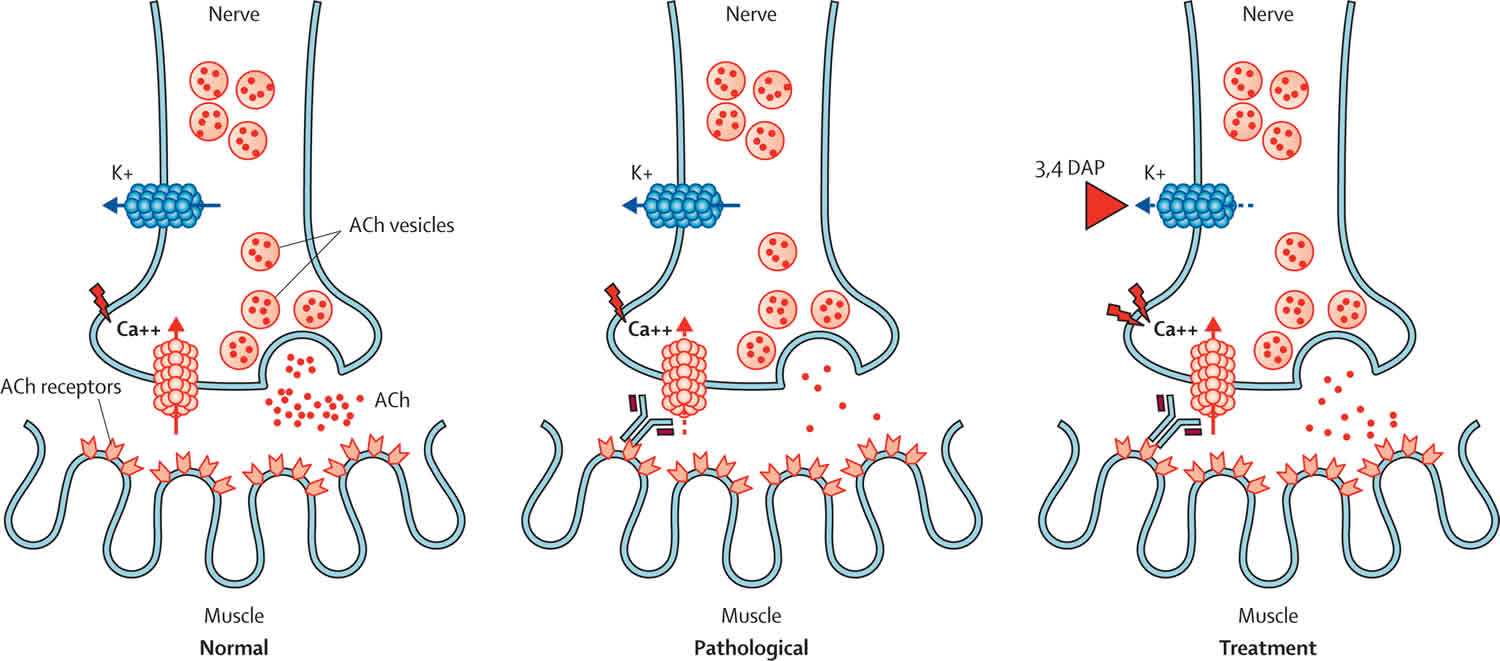
Lambert-Eaton syndrome also called Lambert-Eaton myasthenic syndrome, is a rare autoimmune disorder in which your immune system mistakenly targets healthy cells and tissues in the body. Autoimmune disorder occurs when the body’s defense system against foreign organisms (antibodies) attack healthy tissue. With Lambert-Eaton syndrome or Lambert-Eaton myasthenic syndrome, antibodies produced by your immune system attack your nerve cells (the voltage-gated calcium channels present on the presynaptic nerve terminal) at the neuromuscular junction 1, the site where nerve cells meet muscle cells and help activate the muscles. This makes nerves cells unable to release enough of a chemical called acetylcholine (ACh). This chemical transmits impulses between nerves and muscles. Symptoms include muscle weakness, a tingling sensation in the affected areas, fatigue, and dry mouth.
Lambert-Eaton syndrome may occur with cancers in particular small cell lung cancer 2 or autoimmune disorders such as vitiligo, which leads to a loss of skin pigment. More than half the individuals diagnosed with Lambert-Eaton myasthenic syndrome also develop small cell lung cancer. Small cell lung cancer is a smoking-related lung cancer with neuroendocrine characteristics, is almost always the tumour type that occurs in patients with Lambert-Eaton syndrome, although there have been a few reports of non-small-cell and mixed lung carcinomas 3. Lambert-Eaton myasthenic syndrome may appear up to 3 years before cancer is diagnosed.
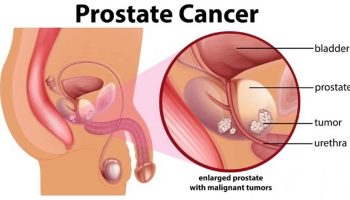
Several papers describe associations of Lambert-Eaton syndrome with non-lung-cancer tumours 4. Statistically, it is likely that many of these would have arisen by chance, but for certain disorders (eg, prostate carcinoma, thymoma, and lymphoproliferative disorders), the cause might be paraneoplastic. Six Lambert-Eaton syndrome patients with prostate carcinoma have been described 5. In these patients, the tumors had neuroendocrine and small-cell characteristics, and symptoms of Lambert-Eaton syndrome correlated with tumor activity. Prostate cancer is also the most common extrathoracic tumour in patients with anti-Hu syndrome, another paraneoplastic neurological syndrome that is mainly associated with small cell lung cancer 6. In four patients with thymoma, two had clear remission of Lambert-Eaton syndrome after surgery without chemotherapy 7. The association of lymphoproliferative disorders with Lambert-Eaton syndrome remains unclear; in 15 patients described, the timeframe of clinical symptoms of Lambert-Eaton syndrome and lymphoproliferative disorders were not well connected 2.
In instances where Lambert-Eaton syndrome is associated with cancer, the cause may be related to the body’s attempt to fight the cancer and accidental attack of nerve fiber endings, especially the voltage-gated calcium channels found there. The trigger for the cases not associated with cancer is unknown.
The prevalence of Lambert-Eaton syndrome is estimated to be between 1/250,000- 1/333,300 worldwide 8. Lambert-Eaton syndrome affects men more often than women. Common age of occurrence is around age 60 years. Lambert-Eaton syndrome is rare in children.
There is no cure for Lambert-Eaton syndrome or Lambert-Eaton myasthenic syndrome. In November 2018, the Food and Drug Administration approved amifampridine tablets (Firdapse) to treat Lambert-Eaton myasthenic syndrome in adults. Other treatment is directed at decreasing the autoimmune response (through the use of steroids, plasmapheresis, or high-dose intravenous immunoglobulin) or improving the transmission of the disrupted electrical impulses by giving drugs such as di-amino pyridine or pyridostigmine bromide (Mestinon). For patients with small cell lung cancer, treatment of the cancer is the first priority.
My husband has Lambert Eaton myasthenic syndrome. We read somewhere that this condition may be caused by an anesthetic. Is that true?
Lambert-Eaton syndrome is caused by an interruption in the nerve to muscle electrical impulses. There are medications that act upon the transmission of these impulses that can worsen symptoms of Lambert-Eaton syndrome. There have been cases reported in the literature, where symptoms worsened in untreated individuals or the first symptoms of Lambert-Eaton syndrome occurred in undiagnosed individuals following administration of such medications 9. In these instances, the medication triggered symptoms of the syndrome that were previously absent or unnoticeable.
Medications that act upon the transmission of impulses between nerve and muscle cells that may worsen symptoms of Lambert-Eaton syndrome, include muscle relaxants (such as succinylcholine) that may be used during anesthesia as well as the following drugs 10:
- Some antibiotics (e.g. aminoglycosides, fluoroquinolones, and erythromycin)
- Iodinated contrast agents (used in CT scans, plain XR and X-ray angiography)
- Beta-blockers
- Calcium channel blockers
- Lidocaine
- Medications used to treat cardiac arrhythmias (e.g. bretylium, quinidine, quinine, procainamide)
My husband had Lambert Eaton myasthenic syndrome. Are our two children at risk to develop this condition?
The answer to this question is complex. While Lambert-Eaton syndrome is not known to follow a specific pattern of inheritance, there appears to be a genetic predisposition to autoimmune diseases in general 11. Families with a history of Lambert Eaton myasthenic syndrome may benefit from consulting with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
Lambert-Eaton syndrome causes
Lambert-Eaton syndrome is a disorder of the immune system, also known as an autoimmune disorder. Autoimmune disorders occur when the body’s defense system against foreign organisms (antibodies) attack healthy tissue. Lambert-Eaton syndrome occurs when part of the neuromuscular junction is damaged. The neuromuscular junction is the area between a nerve cell and a muscle cell, where communication occurs through the release of a chemical signal, called acetylcholine (ACh). This results in muscle contraction or movement. When individuals have Lambert-Eaton syndrome, this process is blocked and acetylcholine (ACh) is not effectively released from nerve cells 8.
In instances where Lambert-Eaton syndrome is associated with cancer, the cause may be related to the body’s attempt to fight the cancer and accidental attack of nerve fiber endings, especially the voltage-gated calcium channels found there. The trigger for the cases not associated with cancer is unknown 12.
Lambert-Eaton syndrome symptoms
Lambert-Eaton syndrome signs and symptoms usually appear around 40 years of age and are characterized by muscle weakness, dysautonomia (autonomic nervous system disorders), and decreased tendon reflexes 13.
Muscle weakness may vary in severity and can lead to 13:
- Difficulty climbing stairs, walking, or lifting things
- Muscle pain
- Drooping of the head
- The need to use the hands to get up from a sitting or lying position
- Problems talking
- Problems chewing or swallowing, which may include gagging or choking
- Vision changes, such as blurry vision, double vision, and problem keeping a steady gaze
Weakness is generally mild in Lambert-Eaton syndrome. Leg muscles are mostly affected. Weakness may improve after exercise, but continuous exertion causes fatigue in some cases.
Symptoms related to the other parts of the nervous system often occur, and include:
- Blood pressure changes
- Dizziness upon standing
- Dry mouth
- Erectile dysfunction
- Dry eyes
- Constipation
- Decreased sweating
Lambert-Eaton syndrome possible complications
Complications of Lambert-Eaton syndrome may include:
- Difficulty breathing, including respiratory failure (less common)
- Difficulty swallowing
- Infections, such as pneumonia
- Injuries from falls and problems with coordination
Lambert-Eaton syndrome diagnosis
Your health care provider will perform a physical exam and ask about the symptoms. The exam may show:
- Decreased reflexes
- Possible loss of muscle tissue
- Weakness or paralysis that gets slightly better with activity
Tests to help diagnose and confirm Lambert-Eaton syndrome may include:
- Blood tests to look for the antibodies that attack the nerves
- Electromyography (EMG) to test the health of the muscle fibers
- Nerve conduction velocity to test the speed of electrical activity along nerves
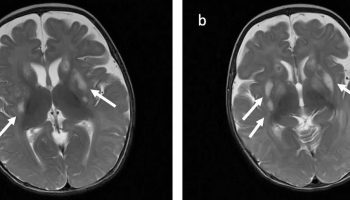
CT scan and MRI of the chest and the abdomen, followed by bronchoscopy for smokers may be done to exclude cancer. PET scan may also be done if a lung tumor is suspected.
Lambert-Eaton syndrome treatment
There is no cure for Lambert-Eaton syndrome.
The main goals of treatment are to:
- Identify and treat any underlying disorders, such as lung cancer
- Give treatment to help with the weakness
Treatment may vary depending on the individual’s age, general health, and whether there is an associated cancer or autoimmune disorder. If cancer or an underlying autoimmune disorder is present, treatment should focus on these conditions first. They may result in symptom relief.
Medications and therapies that may be used to treat Lambert-Eaton myasthenic syndrome include: 3,4-diaminopyridine (enhances acetylcholine release), anticholinesterase agents (e.g., Pyridostigmine), plasma exchange (where blood plasma is removed and replaced with fluid, protein, or donated plasma), intravenous immunoglobulins (IVIg), and medications that suppress the immune system (e.g., prednisone, azathioprine).
Plasma exchange or plasmapheresis, is a treatment that helps remove from the body any harmful proteins (antibodies) that are interfering with nerve function. This involves removing blood plasma that contains the antibodies. Other proteins (such as albumin) or donated plasma are then infused into the body.
Another procedure involves using intravenous immunoglobulin (IVIg) to infuse a large amount of helpful antibodies directly into the bloodstream.
Medicines that may also be tried include:
- Drugs that suppress the immune system’s response
- Anticholinesterase drugs to improve muscle tone (although these are not very effective when given alone)
- Drugs that increase the release of acetylcholine from nerve cells
The US Food and Drug Administration (FDA) Approved Treatments
The medication Amifampridine phosphate (Firdapse) has been approved by the Food and Drug Administration (FDA) as orphan products for treatment of Lambert-Eaton syndrome in adults.
Lambert-Eaton syndrome prognosis
Symptoms of Lambert-Eaton syndrome may improve by treating the underlying disease, suppressing the immune system, or removing the antibodies. However, Lambert-Eaton syndrome associated with cancer also called paraneoplastic Lambert-Eaton syndrome, may not respond as well to treatment. Paraneoplastic Lambert-Eaton syndrome symptoms are due to an altered immune system response to a tumor. Death is due to underlying malignancy.
- Lambert–Eaton myasthenic syndrome: from clinical characteristics to therapeutic strategies. Lancet Neurol 2011; 10: 1098–107 https://www.thelancet.com/action/showPdf?pii=S1474-4422%2811%2970245-9[↩]
- Clinical Dutch-English Lambert-Eaton myasthenic syndrome (LEMS) tumor association prediction score accurately predicts small-cell lung cancer in the LEMS. J Clin Oncol. 2011; 29: 902-908[↩][↩]
- The Lambert-Eaton myasthenic syndrome—a review of 50 cases. Brain. 1988; 111: 577-596[↩]
- Differences in clinical features between the Lambert-Eaton myasthenic syndrome with and without cancer: an analysis of 227 published cases. Clin Neurol Neurosurg. 2002; 104: 359-363[↩]
- Lambert-Eaton myasthenic syndrome: tumor versus nontumor forms. Ann NY Acad Sci. 2008; 1132: 129-134[↩]
- Anti-Hu-associated paraneoplastic encephalomyelitis: analysis of 200 patients. Brain. 2001; 124: 1138-1148[↩]
- Isolated dysphagia due to paraneoplastic myasthenic syndrome with anti-P/Q-type voltage-gated calcium-channel and anti-acetylcholine receptor antibodies. Neuromuscul Disord. 2011; 21: 126-128[↩]
- Lambert-Eaton myasthenic syndrome. https://www.orpha.net/consor/cgi-bin/OC_Exp.php?lng=en&Expert=43393[↩][↩]
- Weingarten, TN. et al. Lambert-Eaton myasthenic syndrome during anesthesia: a report of 37 patients. Journal of Clinical Anesthesia. December 2014; 26(8):648-653. https://www.ncbi.nlm.nih.gov/pubmed/25468580[↩]
- Stevens RD. Neuromuscular disorders and anesthesia. Curr Opin Anaesthesiol. December 2001; 14(6):693-698. https://www.ncbi.nlm.nih.gov/pubmed/17019167[↩]
- Verbeek, S. et al. Lambert–Eaton myasthenic syndrome in a 13-year-old girl with Xp11.22-p11.23 duplication. European Journal of Paediatric Neurology. May 2014; 18(3):439-443. https://www.ncbi.nlm.nih.gov/pubmed/24461257[↩]
- Lambert-Eaton Myasthenic Syndrome (LEMS). https://emedicine.medscape.com/article/1170810-overview[↩]
- Lambert-Eaton syndrome. https://medlineplus.gov/ency/article/000710.htm[↩][↩]