What is melanonychia
Melanonychia is brown or black discoloration of a finger or toe nail. Melanonychia commonly presents as pigmented band arranged lengthwise along the nail unit, and this presentation is known as longitudinal melanonychia or melanonychia striata and is due to melanin within the nail plate. The most concerning cause of melanonychia is subungual melanoma, although a variety of other causes includes physiologic longitudinal melanonychia, systemic disorders, trauma, inflammatory disorders, fungal infections, drugs, and benign melanocytic hyperplasias 1. Longitudinal melanonychia is most often benign and arises from a pigmented melanocytic nevus (a mole) or a lentigo (a freckle). However, a band of brown pigment in a single nail must be examined and investigated with caution, as melanonychia may be the presenting sign of melanoma of the nail unit.
Melanonychia occurs more commonly in dark-skinned individuals (Fitzpatrick skin type 5 and 6). Studies suggest that nearly all Afro-Caribbeans will develop black-brown pigmentation of the nails by the age of 50. It may also be present in up to 20% of Japanese patients. White-skinned people are less commonly affected.
Melanonychia can present in individuals of all ages, including children, and affects both sexes equally.
Is melanonychia cancer?
Melanonychia is a harmless brown or black discoloration of a finger or toe nail. Melanonychia most often occurs because of increased production of melanin by melanocytes in the nail matrix. A healthy adult has approximately 200 melanocytes per mm² in the nail matrix, of which the majority remain dormant. When these melanocytes are activated, melanosomes filled with melanin are transferred to differentiating matrix cells, which migrate distally as they become nail plate onychocytes 2. This results in a visible band of pigmentation in the nail plate. However, there are other more serious causes of of melanonychia and they are subungual melanoma, systemic disorders, inflammatory disorders, fungal infections and drugs 1.
Melanonychia causes
When determining the etiology of longitudinal melanonychia, it is important to distinguish between melanocytic activation and melanocytic hyperplasia. Melanocytic activation is caused by an increased synthesis of melanin with a normal number of melanocytes. Melanocytic hyperplasia (including melanocytic nevi and melanoma) refers to an increased synthesis of melanin with an increased number of melanocytes. Nevi constitute 12% of longitudinal melanonychia cases in adults and 50% of longitudinal melanonychia cases in children.
Approximately two thirds of cases have a brown-black color, and one third of cases have periungual pigmentation (benign pseudo-Hutchinson sign). The bands are wider than 3 mm in greater than 50% of cases.
Below are the causes of melanonychia 2, 3.
The nail (nail plate) is a hard and translucent structure that is not normally pigmented and is made of the skin protein, keratin.
Pigmentation results from the deposition of melanin by the pigment cells, or melanocytes. These typically lie dormant in the nail matrix where the nail originates. As the melanin is continuously deposited in the keratinocytic cells of the growing nail, a longitudinal streak arises. This is termed longitudinal melanonychia.
This deposition of melanin can result from 2 broad processes; melanocytic activation or melanocytic hyperplasia.
Melanocytic activation
Melanocytic activation is an increase in the production and deposition of melanin into the nail cells (onychocytes), without an increase in the number of melanocytes. There are a number of causes.
Physiological (functional)
- Racial variation – African American, Hispanic, Indian, Japanese, other dark-skinned races (multiple bands)
- Pregnancy (multiple bands)
Trauma
- Nail biting (single band)
- Friction: foot deformity, unsuitable footwear (single band)
- Carpal tunnel syndrome
- Onychotillomania (single band)
- Foreign body (subungual) (single band)
- Radiation therapy (multiple bands)
- Ultraviolet light (multiple bands) 4
- Postinflammatory hyperpigmentation (single band)
Inflammatory skin disease
- Psoriasis (multiple bands)
- Lichen planus (multiple bands)
- Amyloidosis
- Onychomycosis (nail infection)
- Chronic radiodermatitis (single bands)
- Scleroderma (multiple bands)
- Systemic lupus erythematosus (multiple bands)
Nonmelanocytic lesions
- Intraepidermal carcinoma or Bowen disease (single band)
- Basal cell carcinoma (single band)
- Subungual fibrous histiocytoma (single band)
- Mucous cyst (single band)
- Lichen striatus (multiple bands)
- Viral warts
Endocrine disorders
- Addison disease (multiple bands)
- Cushing syndrome (multiple bands)
- Nelson syndrome (multiple bands)
- Hyperthyroidism (multiple bands)
- Acromegaly (multiple bands)
Other systemic disease
- Hemosiderosis (iron overload) (multiple bands)
- Porphyria cutanea tarda
- Human immunodeficiency virus infection (HIV)
- Systemic lupus erythematosus (SLE)
- Systemic sclerosis (scleroderma)
- Hyperbilirubinemia (multiple bands)
- Alkaptonuria (multiple bands)
- Porphyria (multiple bands)
- Acquired immunodeficiency syndrome (multiple bands)
- Graft versus host disease (multiple bands)
- Malnutrition (multiple bands)
- Vitamin B-12 deficiency (multiple bands)
Syndrome-associations
- Laugier-Hunziker syndrome
- Peutz-Jeghers syndrome
- Touraine syndrome
Iatrogenic (caused by medical treatment)
- Phototherapy
- X-ray exposure; electron beam therapy
Medication-related
- Chemotherapy agents (especially hydroxyurea, busulfan, bleomycin, adriamycin, doxorubicin, cyclophosphamide, 5-fluorouracil)
- Anti-malarial therapy
- Other drug/agent-related causes of melanonychia are as follows (multiple bands):
- Corticotropin
- Amodiaquine
- Amorolfine
- Arsenic
- Chloroquine
- Clofazimine
- Clomipramine
- Cyclines
- Diquat
- Fluconazole
- Fluoride
- Gold salts
- Ibuprofen
- Ketoconazole
- Lamivudine
- Mepacrine
- Mercury
- Minocycline
- Melanocyte-stimulating hormone
- Polychlorinated biphenyl (PCB)
- Phenytoin
- Phenothiazine
- Psoralen 4
- Roxithromycin
- Steroids
- Sulfonamide
- Tetracycline
- Thallium
- Timolol
- Zidovudine
Melanocytic hyperplasia
Melanocytic hyperplasia refers to an increased number of the pigment cells (melanocytes) within the nail matrix. This can represent either a benign or a malignant process.
- Benign
- Lentigines are seen more commonly in adults
- Melanocytic naevi are seen more commonly in children. Histologically these are differentiated by the absence or presence of melanocyte nests
- Malignant
- Melanoma of the nail unit most commonly affects the thumbs, index fingers and big toes
Pigmentation due to external sources
Pathogens can also cause melanonychia.
- Some gram-negative bacteria (Proteus mirabilis, Klebsiella, Pseudomonas) and dermatophytes (Trichophyton rubrum) can produce melanin that stains the nail.
- Other pathogens involved in infections of the nail (onychomycosis, paronychia) can stimulate inflammation that activates the melanocytes.
- Fungal infection of the nail bed (Aspergillus, Scopulariopsis, Candida, Blastomyces, Trichophyton, Fonsecaea pedrosoi) (multiple bands)
The pigment may be exogenous and deposited on the top of the nail plate. Possible sources include:
- Tobacco
- Potassium permanganate
- Silver nitrate
- Dirt
- Henna
- Hair dye
What are the clinical features of melanonychia?
Melanonychia typically manifests as a single brown-black pigmented streak. It may affect a single nail, or be observed in multiple nails.
- Longitudinal melanonychia extends from the nail fold (cuticle) to the free edge of the nail.
- Complete melanonychia involves the entire nail plate and is due to pigment in the proximal nail matrix. Partial longitudinal melanonychia can be due to distal tumour under the nail plate.
- Transverse melanonychia runs across the nail. Transverse melanonychia is rare, and is often associated with iatrogenic causes such as irradiation and medications.
- Grey color often indicates melanocytic activation, whereas a brown band is due to melanocytic hyperplasia.
- Evaluate whether the pigment band has a regular parallel pattern (benign) or an irregular pattern with loss of parallelism and irregular dots (potential melanoma).
- Nail matrix melanoma affects both finger and toenails and most frequent in index, thumb, and the large toe.
Melanonychia diagnosis
Physical examination must involve inspection of all 20 nails, nail folds and mucosal membranes to detect associated signs that may suggest the underlying cause. In particular, pigmentation of mucosal membranes is associated with Laugier-Hunziker syndrome and Addison disease.
Pathogen-induced pigmentation should be suspected when pigmentation appears at the nail edge or can be removed by scraping. Exogenous pigmentation grows-out with the nail plate, or may similarly be scraped off. Ascorbic acid at 10% concentration may be used to remove potassium permanganate staining.
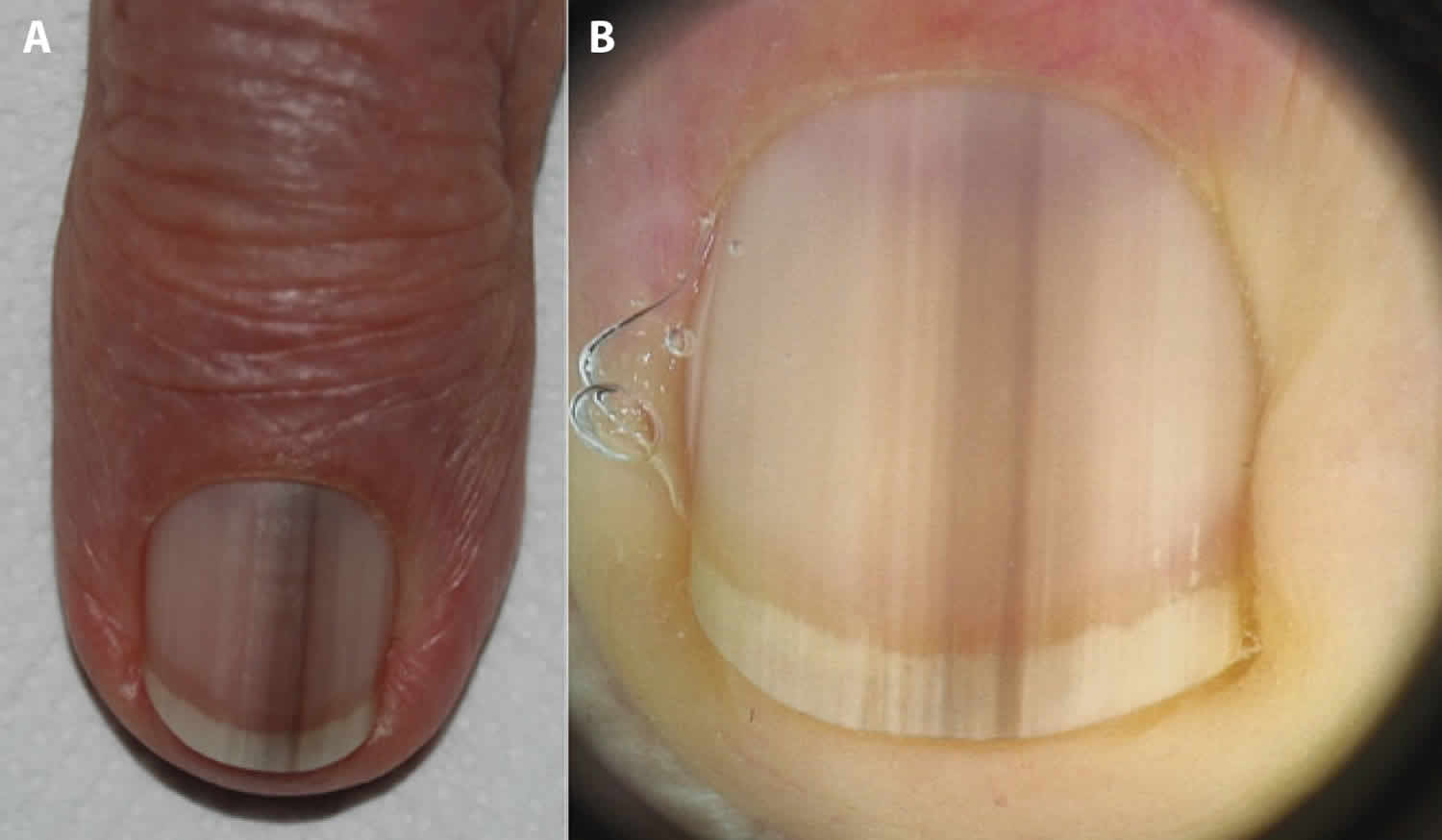
Dermoscopy
Dermatoscopic examination of benign longitudinal melanonychia should reveal light to dark brown lines or bands that are parallel, regular in colour, thickness and spacing as the band extends from the nail fold to the free edge. The borders should be clearly defined and usually of a width of less than 3 mm.
Dermatoscopic examination from the free edge of the nail may help reveal the origin of the implicated melanocytes. The proximal nail matrix produces the superficial (dorsal) nail plate, whereas the distal nail matrix and nail bed produces the deep (ventral) nail plate.
An International Dermoscopy Society study concluded that acquired longitudinal melanonychias in adults should give rise to suspicion of nail unit melanoma if any of the following are present.
- Involvement of more than two-thirds of the nail plate
- Grey or black in addition to brown color
- Irregular brown pigmentation
- Granular pigmentation
- And/or nail dystrophy.
Additional factors of concern include:
- New pigment, especially if there is no preceding trauma or other explanation
- Recurrent spontaneous haemorrhage in the same site
- Variation in colour and thickness of the pigment band.
Nail biopsy
- Definitive exclusion of melanoma of the nail unit is obtained with a nail matrix biopsy. There should be a low threshold for biopsy especially in elderly patients where melanonychia has appeared in a single digit.
Biopsy can result in nail plate deformity.
Melanoma can cause subungual hemorrhage, unsightly nail dystrophy with fissuring and splitting of the nail plate.
Melanonychia treatment
Where melanonychia is attributed to a benign cause, no further treatment is necessary. If melanonychia is secondary to systemic and/or dermatologic disease, treatment of the underlying condition is helpful.
If melanonychia is secondary to a drug, discontinuation of the offending agent may result in clearance.
The management of melanoma of the nail unit requires complete excision of the tumor, which may require amputation of part of the digit 5. In a large case series, the 5-year survival rates for cutaneous melanoma of the hand versus subungual melanoma treated with a wide local excision was reported as 100% and 80%, respectively 6. This was due to a delay in diagnosing subungual lesions, which averaged 3.68 mm in depth versus 1.36 mm for hand melanomas of the cutaneous surface.
Because diagnosis is often delayed in these patients, sentinel lymph node biopsy after surgery may be warranted 7. In cases of subungual melanoma with a poor prognosis, consultation with a hematologist/oncologist regarding potential chemotherapeutic options may be warranted.
Melanonychia prognosis
Melanonychia tends to persist, except when it is related to medication – in which case it fades following withdrawal of the medication.
Nail matrix melanoma tends to have a poor prognosis.
- Tseng YT, Liang CW, Liau JY, Chang K, Tseng YH, Chen JS, et al. Longitudinal Melanonychia: Differences in Etiology Are Associated with Patient Age at Diagnosis. Dermatology. 2017. 233 (6):446-455.[↩][↩]
- Andre J, Lateur N. Pigmented nail disorders. Dermatol Clin. 2006 Jul. 24(3):329-39.[↩][↩]
- Sarti HM, Vega-Memije ME, Dominguez-Cherit J, Arenas R. Longitudinal melanonychia secondary to chromoblastomycosis due to Fonsecaea pedrosoi. Int J Dermatol. 2008 Jul. 47(7):764-5.[↩]
- Parkins GJ, Burden AD, Makrygeorgou A. Psoralen ultraviolet A-induced melanonychia. Clin Exp Dermatol. 2014 Sep 30.[↩][↩]
- Cohen T, Busam KJ, Patel A, Brady MS. Subungual melanoma: management considerations. Am J Surg. 2008 Feb. 195(2):244-8.[↩]
- Glat PM, Spector JA, Roses DF, Shapiro RA, Harris MN, Beasley RW. The management of pigmented lesions of the nail bed. Ann Plast Surg. 1996 Aug. 37(2):125-34[↩]
- Tan KB, Moncrieff M, Thompson JF, et al. Subungual melanoma: a study of 124 cases highlighting features of early lesions, potential pitfalls in diagnosis, and guidelines for histologic reporting. Am J Surg Pathol. 2007 Dec. 31(12):1902-12.[↩]