What is miliary tuberculosis
Miliary tuberculosis also known as disseminated tuberculosis is a contagious mycobacterial infection in which Mycobacterium tuberculosis bacteria have spread from the lungs to other parts of the body through the blood or lymph system. Miliary tuberculosis occurs when a tuberculous lesion erodes into a blood vessel, disseminating millions of Mycobacterium tuberculosis bacteria into the bloodstream and throughout the body. The lungs and bone marrow are most often affected, but any site may be involved. Miliary tuberculosis represents uncontrolled tuberculous infection and carries a relatively poor prognosis.
In 1700, John Jacob Manget 1 described a form of disseminated tuberculosis (TB) and likened the tiny tubercles evident on gross pathological examination to that of innumerable millet seeds in size and appearance. He coined the term miliary tuberculosis (derived from the Latin word miliarius, meaning related to millet seed) to denote this fatal form of disseminated tuberculosis 2.
Miliary tuberculosis is seen both in primary and post-primary tuberculosis or after reactivation of a latent focus and may be associated with tuberculous infection in numerous other tissues and organs.
Miliary tuberculosis is most common among:
- Children under 4 years of age
- Immunocompromised people
- The elderly
Of all patients with tuberculosis, 1.5% are estimated to have miliary tuberculosis. The World Health Organization (WHO) reports that 2-3 million patients die with or from all forms of tuberculosis each year 3.
The incidence of miliary tuberculosis may be higher in African Americans in the United States because of socioeconomic risk factors and may be more common in men than in women because of socioeconomic and medical risk factors. No genetic predisposition has been identified.
Miliary tuberculosis symptoms include fever, chills, weakness, malaise, and often progressive dyspnea. Intermittent dissemination of tubercle bacilli may lead to a prolonged fever of unknown origin (FUO). Bone marrow involvement may cause anemia, thrombocytopenia, or a leukemoid reaction.
Miliary tuberculosis is more difficult to detect in patients who are very young or very old. Children younger than 5 years who acquire miliary tuberculosis are more likely to develop life-threatening miliary and/or meningeal tuberculosis. The disease usually follows primary infection, with no or only a short latency period. Adults older than 65 years have a higher risk of miliary tuberculosis. Clinically, it may be subacute or may masquerade as a malignancy. If undiagnosed, miliary tuberculosis is detected at autopsy.
Miliary tuberculosis causes
Tuberculosis (TB) infection can develop after breathing in droplets sprayed into the air from a cough or sneeze by someone infected with the Mycobacterium tuberculosis bacterium. The resulting lung infection is called primary tuberculosis.
The usual site of tuberculosis is the lungs (pulmonary tuberculosis), but other organs can be involved. In the United States, most people with primary tuberculosis get better and have no further evidence of disease. Disseminated tuberculosis develops in the small number of infected people whose immune systems do not successfully contain the primary infection.
Miliary tuberculosis can occur within weeks of the primary infection. Sometimes, it does not occur until years after you become infected. You are more likely to get this type of tuberculosis if you have a weakened immune system due to disease (such as AIDS) or certain medicines. Infants and older adults are also at higher risk.
Your risk of catching tuberculosis increases if you:
- Are around people who have the disease (such as during overseas travel)
- Live in crowded or unclean conditions
- Have poor nutrition
The following factors can increase the rate of tuberculosis infection in a population:
- Increase in HIV infections
- Increase in number of homeless people with unstable housing (poor environment and nutrition)
- The appearance of drug-resistant strains of tuberculosis.
Risk factors for miliary tuberculosis
Risk factors for miliary tuberculosis involve immunosuppression and include, but are not limited to, the following:
- Cancer
- Transplantation
- HIV infection 4
- Malnutrition
- Diabetes
- Silicosis
- End-stage renal disease
- Major surgical procedures – Occasionally may trigger dissemination
Miliary tuberculosis prevention
Tuberculosis is a preventable disease, even in those who have been exposed to an infected person. Skin testing for tuberculosis is used in high-risk populations or in people who may have been exposed to tuberculosis, such as health care workers.
People who have been exposed to tuberculosis should be skin tested immediately and have a follow-up test at a later date, if the first test is negative.
A positive skin test means you have come into contact with the tuberculosis bacteria. It does not mean that you have active disease or are contagious. Talk to your doctor about how to prevent getting tuberculosis.
Prompt treatment is extremely important in controlling the spread of tuberculosis from those who have active tuberculosis disease to those who have never been infected with tuberculosis.
Some countries with a high incidence of tuberculosis give people a vaccination (called BCG) to prevent tuberculosis. The effectiveness of this vaccine is limited and it is not routinely used in the United States.
People who have had BCG may still be skin tested for tuberculosis. Discuss the test results (if positive) with your doctor.
Miliary tuberculosis symptoms
Miliary tuberculosis can affect many different body areas. Symptoms depend on the affected areas of the body and can include:
- Abdominal pain or swelling
- Chills
- Cough and shortness of breath
- Fatigue
- Fever
- General discomfort, uneasiness, or ill feeling (malaise)
- Joint pain
- Pale skin due to anemia (pallor)
- Sweating
- Swollen glands
- Weight loss
Patients with miliary tuberculosis may experience progressive symptoms over days to weeks or occasionally over several months 5.
Symptoms include the following:
- Weakness, fatigue (90%)
- Weight loss (80%)
- Headache (10%)
Signs of miliary tuberculosis include the following:
- Subtle signs, such as low-grade fever (20%)
- Fever (80%)
- Cough (60%)
- Generalized lymphadenopathy (40%)
- Hepatomegaly (40%)
- Splenomegaly (15%)
- Pancreatitis (< 5%)
- Multiorgan dysfunction, adrenal insufficiency
Miliary tuberculosis possible complications
Complications of miliary tuberculosis can include:
- Adult respiratory distress syndrome (ARDS)
- Liver inflammation
- Lung failure
- Return of the disease
Medicines used to treat tuberculosis can cause side effects, including:
- Changes in vision
- Orange- or brown-colored tears and urine
- Rash
- Liver inflammation
A vision test may be done before treatment so your doctor can monitor any changes in the health of your eyes.
Miliary tuberculosis diagnosis
Your doctor will perform a physical exam. This may show:
- Swollen liver
- Swollen lymph nodes
- Swollen spleen
Tests that may be ordered include:
- Biopsies and cultures of affected organs or tissues
- Bronchoscopy for biopsy or culture
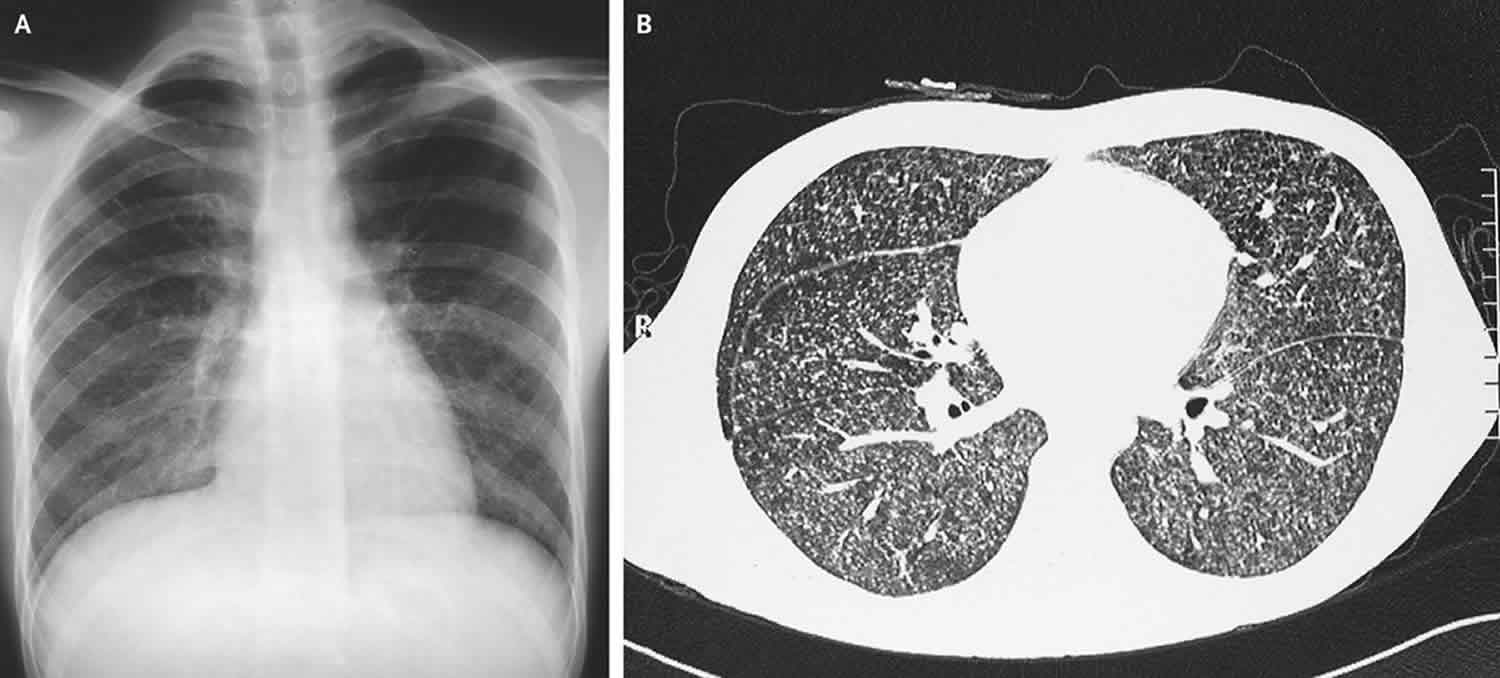
- Chest x-ray
- CT scan of the affected area
- Fundoscopy may reveal retinal lesions
- Interferon-gamma release blood test, such as the QFT-Gold test to test for prior exposure to TB
- Lung biopsy
- Mycobacterial culture of bone marrow or blood
- Pleural biopsy
- Tuberculin skin test (PPD test)
- Sputum examination and cultures
- Thoracentesis
Testing is similar to that for pulmonary tuberculosis, including chest x-ray, tuberculin skin test (PPD test) or interferon gamma release assay (IGRA) blood test, and microscopic analysis (with appropriate staining) and mycobacterial cultures of affected body fluids (cerebrospinal fluid [CSF], urine, or pleural, pericardial, or joint fluid) and tissue for mycobacteria. Nucleic acid–based testing can be done on fresh fluid or biopsy samples and on fixed tissue (eg, if tuberculosis was not suspected during a surgical procedure and cultures were not done). Blood culture results are positive in about 50% of patients with disseminated tuberculosis; such patients are often immunocompromised, often by HIV infection. However, cultures and smears of body fluids and tissues are often negative because few organisms are present; in such cases, nucleic acid amplification tests (NAAT) may be helpful.
Typically, lymphocytosis is present in body fluids. A very suggestive finding in the cerebrospinal fluid (CSF) is a glucose level < 50% of that in serum and an elevated protein level.
If all tests are negative and miliary tuberculosis is still a concern, biopsies of the bone marrow and the liver are done. If tuberculosis is highly suspected based on other features (eg, granuloma seen on biopsy, positive TST or IGRA plus unexplained lymphocytosis in pleural fluid or CSF), treatment should usually proceed despite inability to demonstrate tuberculosis organisms.
Chest x-ray and other imaging, TST, and IGRA can also provide helpful diagnostic information. Chest x-ray may show signs of primary or active tuberculosis; in miliary tuberculosis, it shows thousands of 2- to 3-mm interstitial nodules evenly distributed through both lungs.
Other imaging tests are done based on clinical findings. Abdominal or GU involvement usually requires CT or ultrasonography; renal lesions are often visible. Bone and joint involvement requires CT or MRI; MRI is preferable for spinal disease.
TST and IGRA may initially be negative, but a repeat test in a few weeks is likely to be positive. If it is not, the diagnosis of tuberculosis should be questioned or causes of anergy sought.
Miliary tuberculosis treatment
The goal of treatment is to cure the tuberculosis infection with medicines that fight the tuberculosis bacteria. Treatment of miliary tuberculosis involves a combination of several medicines (usually 4). All medicines are continued until lab tests show which work best. Adjunct corticosteroid treatment is helpful when there is adrenal insufficiency, with tuberculosis meningitis, large pericardial or pleural effusion, dyspnea and/or disabling chest pain, immune reconstitution inflammatory syndrome 6, acute respiratory distress syndrome (ARDS), immune complex nephritis, and histiocyticphagocytosis syndrome 7. In patients co-infected with HIV, careful consideration must be given for drug-drug interactions between anti-tuberculosis and anti-retroviral drugs. Patients receiving anti-tuberculosis drugs must be carefully monitored for adverse drug reactions, especially drug-induced hepatotoxicity and other complications of miliary tuberculosis. In new patients with miliary tuberculosis without tuberculosis meningitis, nine months of anti-tuberculosis treatment should be adequate. When tuberculosis meningitis is present, 12 months of antituberculosis treatment may be required. However, the duration of treatment may have to be prolonged based on individual requirements.
Miliary tuberculosis can be treated by taking several drugs for 6 to 9 months. There are 10 drugs currently approved by the U.S. Food and Drug Administration (FDA) for treating tuberculosis. Of the approved drugs, the first-line anti-tuberculosis agents that form the core of treatment regimens are:
- Isoniazid (INH)
- Rifampin (RIF)
- Ethambutol (EMB)
- Pyrazinamide (PZA)
You may need to take many different pills for 6 months or longer. It is very important that you take the pills the way your provider instructed.
Regimens for treating tuberculosis disease have an intensive phase of 2 months, followed by a continuation phase of either 4 or 7 months (total of 6 to 9 months for treatment).
Table 1. Drug susceptible tuberculosis disease treatment regimens
Abbreviations: DOT = directly observed therapy; EMB = ethambutol; HIV = human immunodeficiency virus; INH = isoniazid; PZA = pyrazinamide; RIF = rifampin.
Footnotes:
- (a) Other combinations may be appropriate in certain circumstances; additional details are provided in the Official American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America Clinical Practice Guidelines: Treatment of Drug-Susceptible TuberculosisExternal.
- (b) When DOT is used, drugs may be given 5 days per week and the necessary number of doses adjusted accordingly. Although there are no studies that compare 5 with 7 daily doses, extensive experience indicates this would be an effective practice. DOT should be used when drugs are administered less than 7 days per week.
- (c) Based on expert opinion, patients with cavitation on initial chest radiograph and positive cultures at completion of 2 months of therapy should receive a 7-month (31-week) continuation phase.
- (d) Pyridoxine (vitamin B6), 25–50 mg/day, is given with INH to all persons at risk of neuropathy (e.g., pregnant women; breastfeeding infants; persons with HIV; patients with diabetes, alcoholism, malnutrition, or chronic renal failure; or patients with advanced age). For patients with peripheral neuropathy, experts recommend increasing pyridoxine dose to 100 mg/day.
- (e) Alternatively, some U.S. TB control programs have administered intensive-phase regimens 5 days per week for 15 doses (3 weeks), then twice weekly for 12 doses.
Use of once-weekly therapy with INH 900 mg and rifapentine 600 mg in the continuation phase is not generally recommended. In uncommon situations where more than once-weekly DOT is difficult to achieve, once-weekly continuation phase therapy with INH 900 mg plus rifapentine 600 mg may be considered for use only in HIV uninfected persons without cavitation on chest radiography.
Continuation Phase of Treatment
The continuation phase of treatment is given for either 4 or 7 months. The 4-month continuation phase should be used in most patients. The 7-month continuation phase is recommended only for the following groups:
- Patients with cavitary pulmonary TB caused by drug-susceptible organisms and whose sputum culture obtained at the time of completion of 2 months of treatment is positive;
- Patients whose intensive phase of treatment did not include PZA;
- Patients with HIV who are not receiving antiretroviral treatment (ART) during TB treatment; and
- Patients being treated with once weekly INH and rifapentine and whose sputum culture obtained at the time of completion of the intensive phase is positive.
- (Note: Use of once-weekly therapy with INH 900 mg and rifapentine 600 mg in the continuation phase is not generally recommended. In uncommon situations where more than once-weekly DOT is difficult to achieve, once-weekly continuation phase therapy with INH 900 mg plus rifapentine 600 mg may be considered for use only in HIV uninfected persons without cavitation on chest radiography.)
When people do not take their tuberculosis medicines as instructed, the infection can become much more difficult to treat. The tuberculosis bacteria can become resistant to treatment. This means the medicines no longer work.
When there is concern that a person may not take all the medicines as directed, a healthcare provider may need to watch the person take the prescribed medicines. This approach is called directly observed therapy. In this case, medicines may be given 2 or 3 times a week, as prescribed by a doctor.
You may need to stay at home or be admitted to a hospital for 2 to 4 weeks to avoid spreading the tuberculosis to others until you are no longer contagious.
Your doctor may be required by law to report your tuberculosis illness to the local health department. Your health care team will ensure that you receive the best care.
Surgery is required for the following:
- To drain empyema, cardiac tamponade, or CNS abscess
- To close bronchopleural fistulas
- To resect infected bowel
- To decompress spinal cord encroachment
Surgical debridement is sometimes needed in Pott disease to correct spinal deformities or to relieve cord compression if there are neurologic deficits or pain persists; fixation of the vertebral column by bone graft is required in only the most advanced cases. Surgery is usually not necessary for TB lymphadenitis except for diagnostic purposes.
Miliary tuberculosis prognosis
Most forms of miliary tuberculosis respond well to treatment. The tissue that is affected, such as the bones or joints, may have permanent damage due to the infection.
If left untreated, the mortality associated with miliary tuberculosis is assumed to be close to 100%. With early and appropriate treatment, however, mortality is reduced to less than 10%. The earlier the diagnosis, the better the likelihood of a positive outcome. Early treatment for suspected tuberculosis has been shown to improve outcome.
Most deaths occur within the first 2 weeks of admission to the hospital. This may be related to delayed onset of treatment. Up to 50% of all cases of disseminated tuberculosis detected at autopsy were missed antemortem in reported case series.
The relapse rate is 0-4% with adequate therapy and directly observed therapy, although results from studies vary. Most relapses occur during the first 24 months after completion of therapy.
- Manget JJ. Sepulchretum sive anatomica practica. Vol. 1. London: Cramer and Perachon; 1700. Observatio XLVII, 3 vols [↩]
- Sharma SK, Mohan A. Miliary tuberculosis. In: Schlossberg D, editor. Tuberculosis and nontuberculous mycobacterial infections. 6th ed. Washington: American Society for Microbiology Press; 2011. pp. 415–35[↩]
- [Guideline] American Thoracic Society, US Centers for Disease Control and Prevention. Diagnostic Standards and Classification of Tuberculosis in Adults and Children. This official statement of the American Thoracic Society and the Centers for Disease Control and Prevention was adopted by the ATS Board of Directors, July 1999. This stat. Am J Respir Crit Care Med. 2000 Apr. 161(4 Pt 1):1376-95[↩]
- Regnier S, Ouagari Z, Perez ZL, Veziris N, Bricaire F, Caumes E. Cutaneous miliary resistant tuberculosis in a patient infected with human immunodeficiency virus: case report and literature review. Clin Exp Dermatol. 2009 Jul 29[↩]
- Hussain SF, Irfan M, Abbasi M, Anwer SS, Davidson S, Haqqee R, et al. Clinical characteristics of 110 miliary tuberculosis patients from a low HIV prevalence country. Int J Tuberc Lung Dis. 2004 Apr. 8(4):493-9.[↩]
- Predictors of development and outcome in patients with acute respiratory distress syndrome due to tuberculosis. Sharma SK, Mohan A, Banga A, Saha PK, Guntupalli KK. Int J Tuberc Lung Dis. 2006 Apr; 10(4):429-35.[↩]
- Sharma SK, Mohan A, Sharma A. Challenges in the diagnosis & treatment of miliary tuberculosis. Indian J Med Res. 2012;135(5):703–730. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3401706[↩]