Palinopsia
Palinopsia is derived from the Greek words palin (again) and opsis (vision or seeing) and is used to describe persistence or recurrence of visual images after the stimulus has been removed, is a nonspecific term that describes multiple types of visual symptoms with a wide variety of causes 1. In palinopsia, the illusory image often becomes incorporated appropriately into the visual scene being perceived; for example, in a famous case reported by Meadows 2, a Santa Claus beard became superimposed appropriately upon the faces of people at a party. Palinopsia is a dysfunction of the association areas at the junction of temporal, occipital and parietal lobes and can be triggered by any lesion or dysfunction in this region 3. This phenomenon arose with various proposed causes such as post-geniculate cortical lesions, peripheral lesions of visual pathways, epilepsy, migraine, drugs, trauma, and diffuse cortical pathologies 4. For example, palinopsia may be the presenting symptom of a potentially life-threatening posterior cortical lesion, yet it may also be a benign medication side effect. Palinopsia typically localizes to a lesion in the non-dominant occipitotemporal cortex 5, though functional MRI data have suggested its origin in parietal cortical projections to the occipital cortex 6. Its mechanism is uncertain, the most likely possibilities being a visual seizure, cerebral hyperperfusion adjacent to areas of cortical damage 7, following drug use or a release hallucination in cases where there is visual loss 8.
Palinopsia is a symptom distinct from the physiological after-image in which images of an object persist or reappear after the person has stopped looking at the object 9. Differences include the fact that palinoptic images have an interval between the original stimulus and the appearance of the after-image and are the same color as the original object 10. They are also constant in size regardless of the distance of the background and their intensity is independent of the intensity of the stimulus 10. The image itself is usually of an object seen in the patient’s immediate environment and does not relate to a more distant visual experience 11.
There is limited data on the epidemiology of palinopsia. Palinopsia may occur in up to 10% of migraineurs and seem to occur more frequently in migraine with aura than without aura 12. Although migraines occur more frequently in females than males and more frequently in younger to middle aged populations than elderly populations 13, there have not been significant studies done comparing palinopsia between the categories.
Gersztenkorn and Lee 14 divided palinopsia into “illusory palinopsia” and “hallucinatory palinopsia”. “Hallucinatory palinopsia” describes afterimages that are not usually affected by environmental conditions of light or motion and are long-lasting, isochromatic (single color), and high resolution. These are attributed to “a dysfunction of visual memory and is caused by posterior cortical lesions or seizures”. “Illusory palinopsia” describes afterimages that are unformed, indistinct or of low resolution and are affected by ambient light or motion. These are attibuted to migraine, drugs, or head trauma. Illusory palinopsia is due to an abnormality in the original perception of a stimulus, whereas hallucinatory palinopsia is due to an abnormality after a stimulus has been encoded in visual memory. External conditions such as stimulus intensity, background contrast, fixation time, and movement typically affect the generation and severity of illusory palinopsia but not hallucinatory palinopsia.
Illusory palinopsia occurs immediately after seeing the original stimulus in the same location in the visual field, while hallucinatory palinopsia may appear anywhere in the visual field and can be delayed in time. Illusory palinopsia occurs continuously or predictably such as in the morning or during light adaptation, however hallucinatory palinopsia is unpredictable. Visual field deficits are often present with hallucinatory palinopsia but not with illusory palinopsia.
Illusory palinopsia may be caused by diffuse neuronal pathology such as global alterations in neurotransmitter receptors, while hallucinatory palinopsia is typically caused by focal cortical pathology.
The clinical characteristics that separate illusory from hallucinatory palinopsia also help differentiate and assess risk in visual illusions and hallucinations. Complex visual hallucinations are usually more worrisome to patients than simple visual hallucinations or visual illusions 15.
Although palinopsia can be indicative of serious diseases that need treatment, many cases are benign and idiopathic. Hallucinatory palinopsia is less common and usually indicative of more severe diseases than illusory palinopsia. Images and scenes perceived by patients with hallucinatory palinopsia also usually deal greater stress to patients than illusory palinopsia.
Figure 1. Palinopsia
Footnote: Example of palinopsia. An example of a moving object (the hand is moving from left to right) with perseverance of multiple images is shown.
[Source 16 ]Hallucinatory palinopsia
Hallucinatory palinopsia resembles a complex visual hallucination of an image or scene previously seen by a person. Hallucinatory palinopsia describes afterimages that are not usually affected by environmental conditions of light or motion and are long-lasting (may last from minutes to hours), isochromatic (single color), and high resolution 14. Hallucinatory palinopsia images or scenes may be seen immediately after the original stimulus, or there may be a delay in time before they are perceived (see Table 1) 17. Hallucinatory palinopsia is associated with “a dysfunction of visual memory and is caused by posterior cortical lesions or seizures”. It can be caused by posterior cortical lesions or seizures 18. Examples of lesions that may cause hallucinatory palinopsia are neoplasms, infarctions, hemorrhages, arteriovenous malformations, aneurysm, abscesses, and tuberculomas. The seizures that cause palinopsia are associated with metabolic imbalances, such as hyperglycemia, carnitine deficiency, ion channel disturbances, and Creutzfeldt-Jakob disease 19.
A visual hallucination is the creation of an image or scene where none exists and can be simple/unformed (e.g., lights, colors, lines, geometric designs) or complex/formed (e.g., objects, animals, people, scenes). Hallucinatory palinopsia is similar to a complex hallucination but describes the persistence or recurrence of a previously-seen, formed, high-resolution image or scene 14. For example, after seeing a cat, an almost identical copy of the cat may remain fixed in the field of view. The hallucinatory afterimage usually is transitory and of short duration (e.g., lasting seconds to minutes) but may persist for hours.
A palinoptic scene consists of a short, stereotyped action sequence that continuously replays for several minutes (e.g., a patient views a person throwing a ball and then sees the same scene repeated many times). The palinoptic image or scene may occur immediately following the stimulus or may be delayed.
Hallucinatory palinopsia can also refer to seeing an object or physical feature which is superimposed onto other objects or people in the same context for a few minutes 14. For example, a patient sees a man with a beard and then observes the same beard on every subsequent person viewed. Another example might be seeing a person wearing distinctive shoes and then the same footwear is observed on every other person. Hallucinatory palinoptic afterimages are a dysfunction of visual memory and are caused by seizures or cortical lesions such as neoplasms, infarctions, and abscesses.
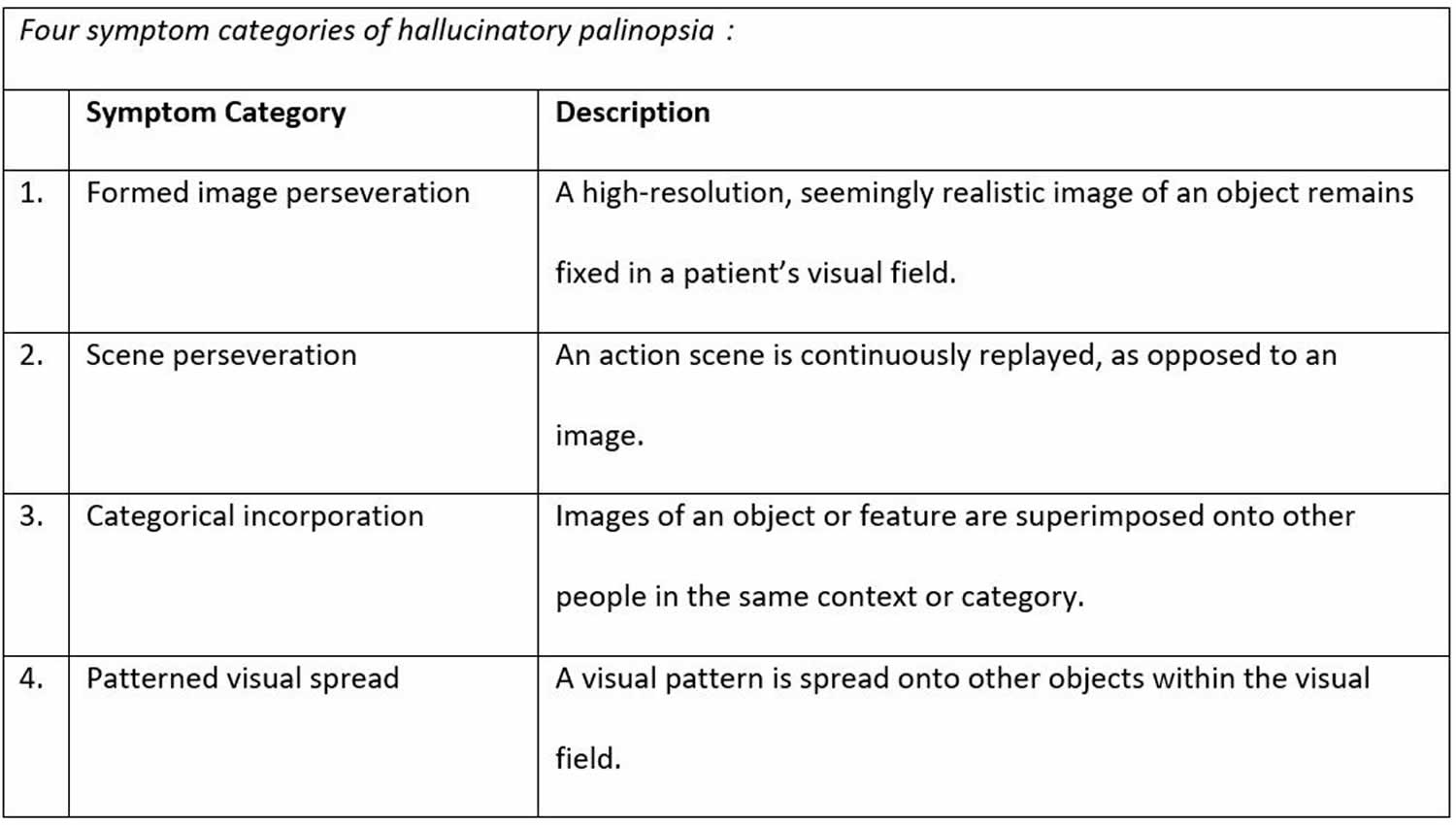
Table 1. Hallucinatory palinopsia
Illusory palinopsia
Illusory palinopsia refers to the distortion of a real external stimulus that has not yet been removed. There may be distortions in the shape, color, or size of the image. The perceived image will also remain in the same location in the visual field. llusory palinopsia is associated with alterations in visual perception of a real external stimulus affected by immediate environmental factors. Unlike hallucinatory palinopsia, illusory palinopsia images are influenced by immediate environmental factors, such as background contrast, stimulus intensity, and ambient lighting 20. Illusory palinopsia images are seen immediately after the original stimulus (see Table 2). Illusory palinopsia describes afterimages that are unformed, indistinct or of low resolution and are affected by ambient light or motion. These are attibuted to migraine, drugs, or head trauma 14.
Illusory palinopsia can be caused by changes in neurotransmitter receptors associated with migraines 21, hallucinogen persisting perception disorder (HPPD) 22, trauma to the head, or drugs or other medications. Medications that have been reported to cause illusory palinopsia include trazodone 23, nefazodone, mirtazapine 24, topiramate, clomiphene, oral contraceptives, and risperidone.
A visual illusion is the altered perception of a real external stimulus such as seeing distortions in shape, size, or color. Illusory palinopsia is similar to a visual illusion in that there is a dysfunction in the original perception of a stimulus, and the afterimages are unformed and indistinct 14. For example, when viewing a light or other bright stimulus such as a computer screen and shifting visual focus, a prolonged, indiscrete afterimage remains for several minutes in the same location in the visual field. These illusory palinoptic afterimages are differentiated from physiological afterimages based on the afterimage intensity and duration.
Illusory palinopsia may also refer to an object or light in motion leaving a comet-like tail in its wake 14.
The visual trails may be discontinuous such as in a film reel or may be blurred together such as in a long-exposure photograph. These movement-induced afterimages persist for several seconds before fading and are usually identical in color and shape to the original object or light, but may be vague or less intense. Illusory palinopsia occurs in migraineurs, after concussions, after hallucinogen use, and as a prescription drug side effect (e.g. trazodone, clomiphene, oral contraceptives, topiramate).
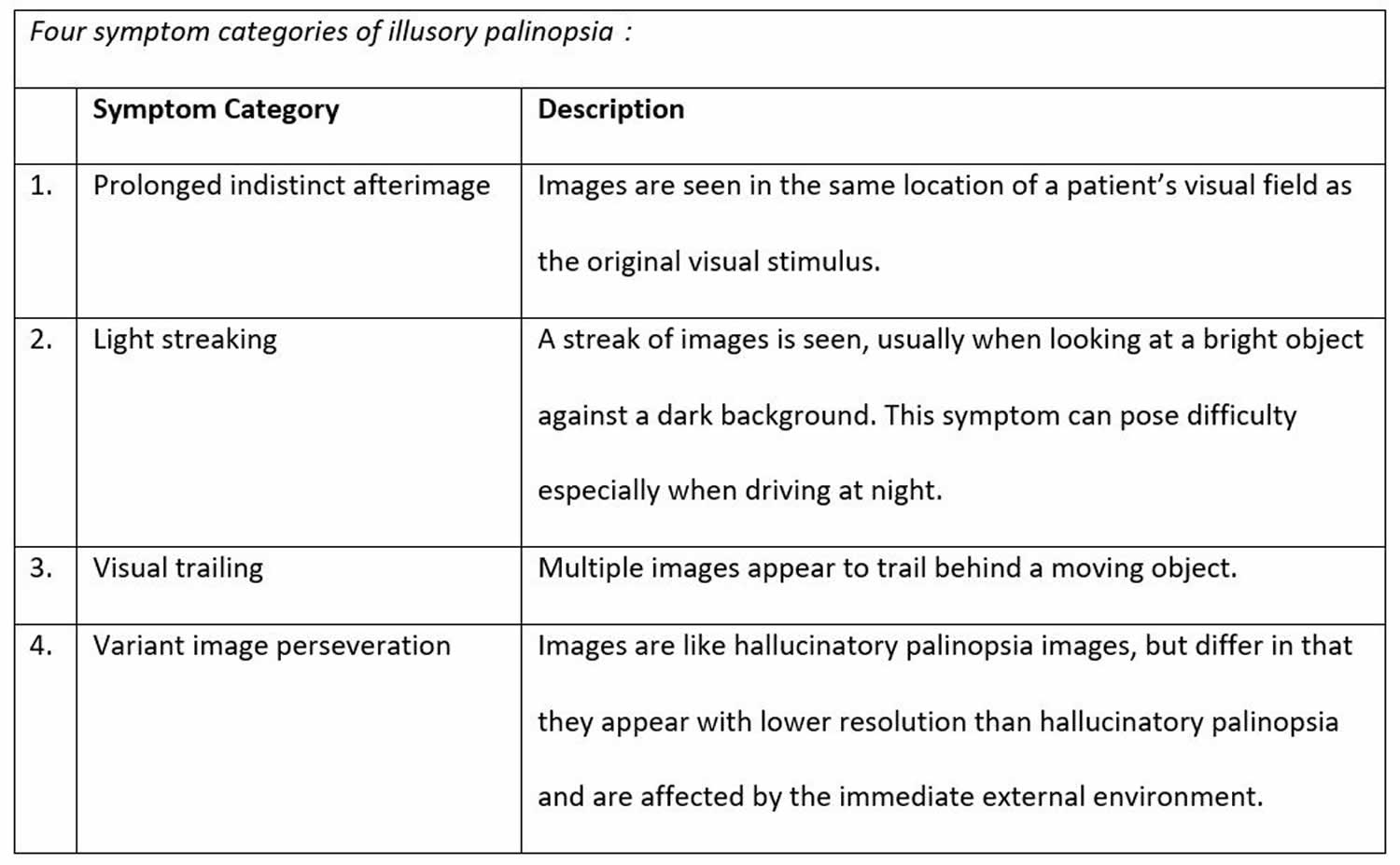
Table 2. Illusory palinopsia
Palinopsia causes
Various causes have been proposed for palinopsia such as post-geniculate cortical lesions, peripheral lesions of visual pathways, epilepsy, migraine, drugs, trauma, and diffuse cortical pathologies 4. Palinopsia may also be idiopathic. Palinopsia typically localizes to a lesion in the non-dominant occipitotemporal cortex 5, though functional MRI data have suggested its origin in parietal cortical projections to the occipital cortex 6.
There may be a number of mechanisms for palinopsia in general, and more than one factor may be involved in any single patient 3. Its mechanism is uncertain, the most likely possibilities being a visual seizure, cerebral hyperperfusion adjacent to areas of cortical damage 7, following drug use or a release hallucination in cases where there is visual loss 8.
Bender et al 1 proposed four possible mechanisms of palinopsia: visual after-sensations, sensory seizures, hallucinations and psychogenic elaborations or fantasies. Although different entities, these authors noted similarities between normal after-images and palinoptic images and considered many occurrences of palinopsia to be visual after-sensations generated at the cerebral level 7.
Cummings et al 8 considered palinopsia to be a type of release hallucination resulting from loss or suppression of normal visual input, and emphasized the need to distinguish it from ictal palinopsia caused by seizures. Palinopsia caused by seizures has several characteristic features, including accompanying signs of seizure activity, absence of hemianopia and spread of palinoptic images to involve the whole visual field 25. Various articles have reported cases of patients with seizures presenting with palinopsia 25.
Palinopsia has often been associated with organic brain disease, for example, trauma 26, parasite 27, abscess 28, stroke 29, brain tumor 30, Creutzfeldt–Jakob disease 31, multiple sclerosis 32, carbon monoxide poisoning 33, non-ketotic hyperglycemia 34, migraine 35, schizophrenia 36, psychotic depression 37 and Charles Bonnet syndrome 38, subcortical hemorrhage 7 and arteriovenous malformations 39.
Several drugs that have been associated with palinopsia share a 5-HT2-receptor activity, including lysergic acid diethylamide 40, trazodone 41, nefazodone 42, risperidone 43 and more recently, mirtazapine 44. Topiramate has also been suggested to have serotonergic activity and a case report has been published documenting it as a cause of palinopsia 45. Marijuana 9, mescaline 46, 3,4-methylenedioxymethamphetamine (ecstasy) 47, interleukin-2 48 and clomiphene citrate 49 have also been reported to be causes of palinopsia.
Stafuzza et al 50 hypothesized that palinopsia could be linked to alterations of peripheric vestibular function combined to a non-adaptation of the temporal binding process of visual and vestibular information. It has long been known that the otolithic and canalar functions converge and interact in the medial vestibular nucleus 51 generally in the form of an inhibitory modulation of the canalar inputs by the otolithic ones 52. More recently it has been shown that the velocity of the vestibular signal was slower than normal in case of deficient canalar function combined to a preserved otolithic function 53. It is also known that the vestibular system is faster than the visual system. Thus during a head rotation the vestibular inputs reach the cortex precociously while the visual inputs reach it later. This delay must be corrected by the brain by curbing the vestibular information so that the movement is perceived as unique by individual. If the temporal binding process of visual and vestibular information does not adapt to the slower than normal vestibular signals and continue to act normally, the vestibular inputs will remain be curbed and finally reach the cortex after the visual inputs. Thus, the patient will keep in mind the visual image that he had before head’s movement and only will become aware of the new visual image once the information of movement given by the vestibular system arrives at the cortex. Finally, it has been shown that the deficiency of the vestibulo-ocular reflex resulting from an alteration of canalar function combined to a preserved otolithic function worsens over time 53. This explains why the episodes of palinopsia only started with a vague sensation of projection of the image during the head impulse test to become evident only several months after the partial loss of the vestibular function.
Palinopsia pathophysiology
The pathophysiology of palinopsia is not clear, but many hypothesis are proposed. One of them is that drugs could alter serotoninergic activity 54 or inhibit the synthesis of gamma-aminobutyric acid (GABA) involved in the generation of action potentials of the visual system 55. Another involves a local irritation of the occipito-parietal cortex by surrounding edema 56.
Hallucinatory palinopsia results from a dysfunction in visual memory. It is thought to occur from localized cortical hyperexcitability or heightened activity in the posterior visual pathway through the mechanisms of cortical deafferentation, focal cortical irritation, and epileptic discharges.
Illusory palinopsia results from a dysfunction in visual perception. It is thought to occur from changes in the excitability of neurons in the visual pathways. Drugs that cause palinopsia (trazodone, nefazodone, risperidone, and mirtazapine) are similar in sharing antagonism at the 5-HT2 receptor which binds the neurotransmitter serotonin, and the hallucinogen LSD is an agonist for 5-HT2A and 5-HT2C. It is therefore proposed that 5-HT2 receptor excitotoxicity may be involved in the mechanism of illusory palinopsia 57. Illusory palinopsia after-images are affected by environmental light and motion, which indicates changes in neuronal excitability for both pathways.
Finally, according to the Bayesian theory that says that surrounding images can be predicted using stored memories of previous images, palinopsia could result from a mistake of the brain in the prediction phase of images 58.
Palinopsia symptoms
Palinopsia is a visual symptom in which images of an object persist or reappear after the person has stopped looking at the object. In many cases patients see a series of repeated images (visual echos) of the object. Eye movements to follow an object may appear to leave a trail. Palinopsia sounds somewhat similar to another rare neurological condition where there are echoing of sounds (palinacusis), but the two disorders are not related. In palinopsia, the illusory image often becomes incorporated appropriately into the visual scene being perceived; for example, in a famous case reported by Meadows 2, a Santa Claus beard became superimposed appropriately upon the faces of people at a party. Patients with palinopsia usually have visual field disturbances, and these are more commonly left sided, reflecting the importance of posteriorly placed, right-sided cerebral lesions 1. According to Bender et al 1, palinopsia occurs in visual fields that are defective but not blind. Apart from visual field defects, a number of other clinical features may be associated 46. Illusions of movement may occur, as may visual perseveration in space (illusory visual spread) such that, for example, the pattern of a wallpaper appears to spread to adjacent structures.
In addition to just plain palinopsia, there are 8 subcategories of symptoms:
- Formed image perservation — such as seeing a picture of an insect superimposed on vision for seconds to days.
- Scene perseveration — this is similar to a video clip that replays.
- Categorical incorporation — seeing an object and then superimposing it on similar objects. For example, seeing a beard, and seeing other bearded people.
- Illusory visual spread — for example a checkerboard that spreads onto other perseverated objects.
- Light streaking — relative motion between a person and light source causes streaking to appear behind the light. For example, while driving at night.
- Visual trailing — copies left in the wake of a moving object.
- Prolonged indistinct afterimage
- Variant image perservation — faded image.
Associated symptoms to palinaopsia include:
- Cerebral polyopia is defined by Gersztenkorn and Lee 14 as when a patient sees two or more duplicated images arranged in ordered rows or columns after fixation on an object. Not all authors seem to define polyopia as images in columns however. It is also difficult to imagine a mechanism for this to occur.
- Akinetopsia is defined as failure to percieve motion, also called “stroboscopic vision”.
- Visual allesthesia occurs when fixation on an object causes its duplication in the opposite hemifield.
- Entopic phenomena are observation of real physiologic processes, such as seeing white blood cells moving through retinal capillaries or tree-like outlines representing the retinal circulation. These may be related to visual hypersensitivity, which is discussed under the category of photophobia.
Palinopsia diagnosis
The diagnosis of palinopsia is made clinically. There are no diagnostic tests or examination findings.
Initially there is an attempt to determine the cause. The examiner should obtain the details of the palinopsia to determine if it is hallucinatory or illusory. A full neuro-ophthalmologic exam including automated visual fields should then be performed 14. Hallucinatory palinopsia, usually caused by a cortical lesion or seizure, can be the presenting symptom of a serious neurological disease and typically resolves after treating the underlying disturbance.
A patient reporting even one such episode should probably be offered an MRI and a possible referral to neurology or neuro-ophthalmology.
In contrast, illusory palinopsia is more common and usually less worrisome. Patients often have multiple types of illusory palinopsia, along with visual illusions and simple hallucinations like visual snow, Alice in Wonderland Syndrome, and entoptic phenomena. These illusory symptoms are generally benign and long standing, but are often refractory to treatment.
Diagnosing the etiology of illusory palinopsia is based on clinical history, with the physical exam and work-up usually being non-contributory. Illusory palinopsia can be attributed to prescription drugs, head trauma, migrainous neuronal dysfunction, hallucinogen ingestion, or symptoms may be idiopathic. There is occasional treatment success with pharmaceuticals that reduce cortical excitability such as gabapentin. Sunglasses or tinted lenses or filters may improve symptoms.
Many patients with illusory palinopsia have played referral pinball between neurologists and ophthalmologists and have already received extensive work-ups. Due to the subjective nature of the symptoms and the absence of physical findings, clinicians are sometimes dismissive or mention non-organic disease.
There is considerable evidence in the literature confirming the symptom legitimacy, so validating and explaining the patient’s symptoms can help ease anxiety and should be of primary concern. Illusory palinopsia is presumably due to a modified neural excitability state causing dysfunction in light and motion processing mechanisms, thus there is an exaggeration of normal phenomena such as physiological afterimages from bright lights and trails behind quickly-moving objects.
Diagnostic procedures
To determine patient whether a patient has hallucinatory or illusory palinopsia, a full ophthalmologic and neurologic history and physical exam should be done. Automated visual field testing and neuroimaging should be performed. These procedures are warranted for hallucinatory palinopsia for its common cause by seizures and posterior cortical lesions. They may also be useful for illusory palinopsia for its common cause by migraines. More often however, epileptiform discharges are usually not seen in EEGs for patients with illusory palinopsia, or palinopsia without structural correlate 20. Neuroimaging is therefore more useful for patients with hallucinatory palinopsia.
Hallucinatory palinopsia can indicate serious neurological disease, and therefore a patient who reports experience of even one episode of hallucinatory palinopsia should be referred to a neuro-ophthalmologist or neurologist. An MRI should be offered to patients with hallucinatory palinopsia.
Laboratory test
If the neuroimaging is unremarkable for a patient with hallucinatory palinopsia, then directed additional evaluation may be considered.
Palinopsia treatment
Palinopsia treatment is directed at the underlying cause, if one can be identified.
For hallucinatory palinopsia, treatment of the underlying cause usually resolves the palinopsia 59. For hallucinatory palinopsia caused by from seizures, treatment of the seizures usually resolves the palinopsia. Hallucinatory palinopsia caused by lesions is directed by treatment of the type of lesion.
For illusory palinopsia, treatment can involve medications that decrease the excitability of neurons, such as clonidine, gabapentin, acetazolamide, magnesium, or calcium channel blockers 20. However, more studies need to be done on the efficacy of these drugs as they vary from reported cases. Sunglasses or other tinted lenses may also alleviate symptoms of illusory palinopsia. For illusory palinopsia caused by migraines, treatment of the migraine would also be appropriate.
If no cause is identified, treatment for migraine may be offered.
- Bender MB, Feldman M, Sobin AJ. Palinopsia. Brain, Volume 91, Issue 2, June 1968, Pages 321–338, https://doi.org/10.1093/brain/91.2.321[↩][↩][↩][↩]
- Meadows JC, Munro SS. Palinopsia. J Neurol Neurosurg Psychiatry. 1977 Jan;40(1):5-8. doi: 10.1136/jnnp.40.1.5 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC492596/pdf/jnnpsyc00151-0012.pdf[↩][↩]
- Khan AN, Sharma R, Khalid S, McKean D, Armstrong R, Kennard C. Palinopsia from a posteriorly placed glioma–an insight into its possible causes. BMJ Case Rep. 2011;2011:bcr0820103273. Published 2011 Feb 2. doi:10.1136/bcr.08.2010.3273 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3062347[↩][↩]
- Gersztenkorn D, Lee AG.. Palinopsia revamped: A systematic review of the literature. Surv Ophthalmol. 2015;60(1):1–35. doi:10.1016/j.survophthal.2014.06.003[↩][↩]
- Norton JW, Corbett JJ. Visual perceptual abnormalities: hallucinations and illusions. Semin Neurol 2000;20:111–21[↩][↩]
- Santhouse AM, Ffytche DH, Howard RJ, et al. The functional significance of perinatal corpus callosum damage: an fMRI study in young adults. Brain 2002;125(Pt 8):1782–92[↩][↩]
- Hayashi R, Shimizu S, Watanabe R, et al. Palinopsia and perilesional hyperperfusion following subcortical hemorrhage. Acta Neurol Scand 2002;105:228–31[↩][↩][↩][↩]
- Cummings JL, Syndulko K, Goldberg Z, et al. Palinopsia reconsidered. Neurology 1982;32:444–7[↩][↩][↩]
- Kawasaki A, Purvin V. Persistent palinopsia following ingestion of lysergic acid diethylamide (LSD). Arch Ophthalmol 1996;114:47–50[↩][↩]
- Pomeranz HD, Lessell S. Palinopsia and polyopia in the absence of drugs or cerebral disease. Neurology 2000;54:855–9[↩][↩]
- Swash M. Visual perseveration in temporal lobe epilepsy. J Neurol Neurosurg Psychiatr 1979;42:569–71[↩]
- Belcastro V, Cupini LM, Corbelli I, Pieroni A, D’Amore C, Coproni S, Gorgone G, Ferlazzo E, Palma FD, Sarchielli P, Calabresi P. Palinopsia in patients with migraine: A case-control study. Cephalalgia. 2011;31:999.[↩]
- Younger DS. Epidemiology of Migraine. Neurol Clin. 2016;34:849–861.[↩]
- Gersztenkorn D, Lee AG. Palinopsia revamped: a systematic review of the literature. Surv Ophthalmol. 2015 Jan-Feb;60(1):1-35. https://doi.org/10.1016/j.survophthal.2014.06.003[↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Teeple RC, Caplan JP, Stern TA. Visual hallucinations: differential diagnosis and treatment. Prim Care Companion J Clin Psychiatry. 2009;11:26-32.[↩]
- van Dongen RM, Haan J. Symptoms related to the visual system in migraine. F1000Res. 2019;8:F1000 Faculty Rev-1219. Published 2019 Jul 30. doi:10.12688/f1000research.18768.1 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6668047[↩]
- Kinsbourne M, Warrington E. A study of visual perseveration. J Neurol Neurosurg Psychiatry. 1963;26:468-475.[↩]
- Auzou P, Ozsancak C, Miret N, Hitzel A, Hannequin D. Palinopsia associated with partial seizures secondary to right parietal hemorrhage. Ann Med Interne (Paris). 1998;149(3),161-163.[↩]
- Purvin V, Bonnin J, Goodman J. Palinopsia as a presenting manifestation of Creutzfeldt–Jakob disease. Journal of clinical neuro-ophthalmology. 1989;9(4):242–6.[↩]
- Gersztenkorn D, Lee AG. Palinopsia revamped: A systematic review of the literature. Survey of ophthalmology. 2014;60:1–35.[↩][↩][↩]
- Belcastro V, Cupini LM, Corbelli I, Pieroni A, D’Amore C, Caproni S, Calabresi P. Palinopsia in patients with migraine: a case-control study. Cephalalgia. 2011;231(9), 999-1004.[↩]
- Kawasaki A, Purvin V. Persistent palinopsia following ingestion of lysergic acid diethylamide (LSD). Arch Ophthalmol. 1996;114(1):47-50.[↩]
- Hughes MS, Lessell S. Trazodone-induced palinopsia. Arch Ophtalmol. 1990;108:399-400.[↩]
- Ihde-Scholl T, Jefferson JW. Mitrazapine-associated palinopsia. The Journal of Clinical Psychiatry. 2001;62(5):373.[↩]
- Lefébre C, Kölmel HW. Palinopsia as an epileptic phenomenon. Eur Neurol. 1989;29(6):323-7. doi: 10.1159/00011643[↩][↩]
- Lessell S. Higher disorders of visual function: positive phenomena. In: Glaser JS, Smith JL, eds. Neuro-ophthalmology. St. Louis: CV Mosby; 1975:27–44[↩]
- Ardila A, Botero M, Gomez J. Palinopsia and visual allesthesia. Int J Neurosci 1987;32:775–82[↩]
- Lunardi P, Tacconi L, Missori P, et al. Palinopsia: unusual presenting symptom of a cerebral abscess in a man with Kartagener’s syndrome. Clin Neurol Neurosurg 1991;93:337–9[↩]
- Vaphiades MS, Celesia GG, Brigell MG. Positive spontaneous visual phenomena limited to the hemianopic field in lesions of central visual pathways. Neurology 1996;47:408–17[↩]
- Michel EM, Troost BT. Palinopsia: cerebral localization with computed tomography. Neurology 1980;30:887–9[↩]
- Purvin V, Bonnin J, Goodman J. Palinopsia as a presenting manifestation of Creutzfeldt-Jakob disease. J Clin Neuroophthalmol 1989;9:242–6[↩]
- Jacome DE. Palinopsia and bitemporal visual extinction on fixation. Ann Ophthalmol 1985;17:251–2, 257[↩]
- Adler A. Disintegration and restoration of optic recognition in visual agnosia. Arch Neurol Psychiatry 1944;51:243–59[↩]
- Johnson SF, Loge RV. Palinopsia due to nonketotic hyperglycemia. West J Med 1988;148:331–2[↩]
- Klee A, Willanger R. Disturbances of visual perception in migraine. Review of the literature and a report of eight cases. Acta Neurol Scand 1966;42:400–14[↩]
- Marneros A, Körner J. Chronic palinopsia in schizophrenia. Psychopathology 1993;26:236–9[↩]
- Gates TJ, Stagno SJ, Gulledge AD. Palinopsia posing as a psychotic depression. Br J Psychiatry 1988;153:391–3[↩]
- Ozsancak C, Auzou P. [Palinopsia in Charles Bonnet syndrome]. Presse Med 1998;27:359.[↩]
- Kupersmith MJ, Berenstein A, Nelson PK, et al. Visual symptoms with dural arteriovenous malformations draining into occipital veins. Neurology 1999;52:156–62[↩]
- Sunness JS. Persistent afterimages (palinopsia) and photophobia in a patient with a history of LSD use. Retina (Philadelphia, Pa) 2004;24:805[↩]
- Hughes MS, Lessell S. Trazodone-induced palinopsia. Arch Ophthalmol 1990;108:399–400[↩]
- Faber RA, Benzick JM. Nafazodone-induced palinopsia. J Clin Psychopharmacol 2000;20:275–6[↩]
- Lauterbach EC, Abdelhamid A, Annandale JB. Posthallucinogen-like visual illusions (palinopsia) with risperidone in a patient without previous hallucinogen exposure: possible relation to serotonin 5HT2a receptor blockade. Pharmacopsychiatry 2000;33:38–41[↩]
- Ihde-Scholl T, Jefferson JW. Mitrazapine-associated palinopsia. J Clin Psychiatry 2001;62:373.[↩]
- Fontenelle LF. Topiramate-induced palinopsia. J Neuropsychiatry Clin Neurosci 2008. 20:249–50[↩]
- Critchley M. Types of visual perseveration: “paliopsia” and “illusory visual spread”. Brain 1951;74:267–99[↩][↩]
- McGuire PK, Cope H, Fahy TA. Diversity of psychopathology associated with use of 3,4-methylenedioxymethamphetamine (‘Ecstasy’). Br J Psychiatry 1994;165:391–5[↩]
- Friedman DI, Hu EH, Sadun AA. Neuro-ophthalmic complications of interleukin 2 therapy. Arch Ophthalmol 1991;109:1679–80[↩]
- Purvin VA. Visual disturbance secondary to clomiphene citrate. Arch Ophthalmol 1995;113:482–4[↩]
- Palinopsia Following Acute Unilateral Partial Vestibular Deafferentation: A Case Report. Front. Neurol., 21 September 2018. https://doi.org/10.3389/fneur.2018.00773[↩]
- Curthoys I, Markham CH. Convergence of labyrinthine influences on units in the vestibular nuclei of the cat. I. Natural stimulation. Brain Res. (1971) 35:469–90. doi: 10.1016/0006-8993(71)90489-6[↩]
- Fluur E. Positional and positioning nystagmus as a result of utriculocupular integration. Acta Otolaryngol. (1974) 78:19–27. doi: 10.3109/00016487409126321[↩]
- Angelaki DE, Merfeld DM, Hess BJ. Low-frequency otolith and semicircular canal interactions after canal inactivation. Exp Brain Res. (2000) 132:539–49.[↩][↩]
- Yun SH, Lavin PJ, Schatz MP, Lesser RL. Topiramate-induced palinopsia: a case series and review of the literature. J Neuroophthalmol. (2015) 35:148–51. doi: 10.1097/WNO.0000000000000216[↩]
- Venkatesh R, Gujral GS, Gurav P, Tibrewal S, Mathur U. Clomiphene citrate-induced visual hallucinations: a case report. J Med Case Rep. (2017) 11:60. doi: 10.1186/s13256-017-1228-0[↩]
- Ziaei M, Elgohary MA, Bremner FD. Palinopsia as the initial manifestation of non-hodgkin’s lymphoma. Int Ophthalmol. (2013) 33:553–6. doi: 10.1007/s10792-012-9682-6[↩]
- Lauterbach EC, Abdelhamid A, Annandale JB. Posthallucinogen-like visual illusions (palinopsia) with risperidone in a patient without previous hallucinogen exposure: possible relation to serotonin 5-HT2A blockade. Pharmacopsychiatry 2000;33:38-41.[↩]
- Khan AN, Sharma R, Khalid S, McKean D, Armstrong R, Kennard C. Palinopsia from a posteriorly placed glioma – an insight into its possible causes. Case Rep. (2011) pii: bcr0820103273. doi: 10.1136/bcr.08.2010.3273[↩]
- Khan AN, Sharma R, Khalid S, McKean D, Armstrong R, Kennard C. Palinopsia from a posteriorly placed glioma – an insight into its possible causes. BMJ Case Reports. 2011.[↩]