Pediatric anemia
Pediatric anemia is when there are fewer red blood cells than normal, or there is a low concentration of hemoglobin in the blood of children. Pediatric anemia is defined as a hemoglobin level two standard deviations below the mean for age 1 or hematocrit level lower than the age-adjusted reference range for healthy infants and children 2. After children reach 12 years of age, the hemoglobin norm can be further divided into gender-specific ranges 3. Table 1 lists age-based hemoglobin levels. This can lead to health problems because red blood cells contain hemoglobin, which carries oxygen to the body’s tissues. Anemia can cause a variety of complications, including fatigue (tiredness) and stress on the body’s organs. Worldwide, anemia affects up to one-half of children younger than five years 4.
- Hemoglobin (Hb) is the part of blood that distributes oxygen from the lungs to tissues in the body.
- Hematocrit (Hct) is the measurement of the percentage of red blood cells found in a specific volume of blood.
Table 1. Age-Based Hemoglobin Levels in Children and Adolescents
| Age | Mean hemoglobin level | −2 standard deviations | |
|---|---|---|---|
Birth (term infant) | 16.5 g per dL (165 g per L) | 13.5 g per dL (135 g per L) | |
1 month | 13.9 g per dL (139 g per L) | 10.7 g per dL (107 g per L) | |
2 months | 11.2 g per dL (112 g per L) | 9.4 g per dL (94 g per L) | |
3 to 6 months | 11.5 g per dL (115 g per L) | 9.5 g per dL (95 g per L) | |
6 months to 2 years | 12 g per dL (120 g per L) | 10.5 g per dL (105 g per L) | |
2 to 6 years | 12.5 g per dL (125 g per L) | 11.5 g per dL | |
6 to 12 years | 13.5 g per dL | 11.5 g per dL | |
12 to 18 years | |||
| Males | 14.5 g per dL (145 g per L) | 13 g per dL (130 g per L) | |
| Females | 14 g per dL (140 g per L) | 12 g per dL | |
Anemia is often a symptom of a disease rather than a disease itself. Anemia usually develops due to the presence of one of the following:
- Excessive blood loss or hemorrhaging
- Deficient production of red blood cells
- Excessive red blood cell destruction
- Both decreased production and excessive destruction of red blood cells
Anemia a fairly common blood disorder with many causes. They include inherited disorders, nutritional problems (such as an iron or vitamin deficiency), infections, some kinds of cancer, and exposure to a drug or toxin.
There are many different types of anemia, including:
- Iron deficiency anemia
- Megaloblastic (pernicious) anemia
- Hemolytic anemia
- Sickle cell anemia
- Cooley’s anemia (thalassemia)
- Aplastic anemia
- Chronic anemia
Anemia can be categorized as microcytic, normocytic, or macrocytic. Microcytic iron deficiency anemia is a common cause of childhood anemia, whereas macrocytic anemia is rare in children. Table 2 summarizes the causes of anemia 6.
In general, a child with significant anemia may tire more easily than other kids and need to take it easy. Make sure your child’s teachers and other caregivers are aware of the anemia. If iron deficiency is the cause, follow the doctor’s directions about dietary changes and taking any iron supplements.
If the spleen is enlarged, your child may not be able to play contact sports because there’s a risk that the spleen could rupture or hemorrhage.
Certain forms of anemia (such as sickle cell disease) need other, more specific kinds of care and treatment.
If you have any questions about anemia or you think your child might have it, speak with your doctor.
Table 2. Causes of anemia in children
| Age | Type of anemia | ||
|---|---|---|---|
| Microcytic | Normocytic | Macrocytic | |
|
|
|
|
|
|
|
|
|
|
|
|
Footnote: Causes are listed in approximate order of prevalence.
*—Iron deficiency anemia is most commonly microcytic.
[Source 5 ]Aplastic anemia in children
Aplastic anemia occurs when the bone marrow produces too few of all types of blood cells: red cells, white cells, and platelets. A reduced number of red blood cells causes the hemoglobin (a type of protein in the red blood cells that carries oxygen to the tissues of the body) to drop. A reduced number of white blood cells cause the patient to be susceptible to infection. A reduced number of platelets can cause the blood not to clot as easily.
Aplastic anemia causes
Aplastic anemia in children has multiple causes. Some of these causes are idiopathic, meaning they occur sporadically for no known reason. Other causes are secondary, resulting from a previous illness or disorder.
Nearly 50 to 75 percent of childhood cases of aplastic anemia occur sporadically for no known reason.
Acquired causes, however, may include:
- History of specific infectious diseases such as hepatitis, Epstein-Barr virus (EBV), cytomegalovirus (CMV), parvovirus B19, or human immunodeficiency virus (HIV)
- History of taking certain medications
- Exposure to certain toxins such as heavy metals
- Exposure to radiation
- History of an autoimmune disease such as lupus
Children may also inherit a disorder that predisposes them to developing aplastic anemia. Some disorders that are known to predispose a child to aplastic anemia include the following:
- Fanconi anemia
- Dyskeratosis congenita
- Shwachman Diamond syndrome
- Reticular dysgenesis
- Amegakaryocytic thrombocytopenia
- Familial aplastic anemias
Aplastic anemia signs and symptoms
Each child may experience symptoms of aplastic anemia differently. The following are some of the most common symptoms:
- Headache
- Dizziness
- Nausea
- Shortness of breath
- Bruising
- Lack of energy or tiring easily (fatigue)
- Abnormal paleness or lack of color of the skin
- Blood in stool
- Nosebleeds
- Bleeding gums
- Fevers
- Sinus tenderness
- Enlarged liver or spleen
- Oral thrush (white patches on a red, moist, swollen surface, occurring anywhere in the mouth)
The symptoms of aplastic anemia may resemble other blood disorders or medical problems. Always consult your child’s physician for a diagnosis.
Aplastic anemia diagnosis
Diagnostic evaluation begins with a thorough medical history and physical examination of your child. At The Children’s Hospital of Philadelphia, clinical experts use a variety of diagnostic tests to diagnose aplastic anemia and possible complications, including:
- Blood tests
- Bone marrow aspiration and/or biopsy — a procedure that involves taking a small amount of bone marrow fluid (aspiration) and/or solid bone marrow tissue (called a core biopsy), usually from the hip bones, to be examined for the number, size, and maturity of blood cells and/or abnormal cells.
Aplastic anemia treatments
Specific treatment for aplastic anemia will be determined by your child’s physician and will be based on:
- Your child’s age, overall health, and medical history
- The extent of the anemia
- Cause of the anemia
- Your child’s tolerance for specific medications, procedures, or therapies
- Expectations for the course of the anemia
- Your opinion or preference
Aplastic anemia is a serious illness and treatment usually depends on the underlying cause. For certain causes, recovery can be expected after treatment, however, relapses can occur. To treat the low blood counts, initial treatment is usually supportive, meaning that it is necessary to treat the symptoms but not possible to cure the disease.
Supportive therapy may include:
- Blood transfusion (both red blood cells and platelets)
- Preventative antibiotic therapy
- Meticulous handwashing
- Special care to food preparation (such as only eating cooked foods)
- Medications (to stimulate the bone marrow to produce cells)
- Immunosuppressive therapy
- Hormones
Follow-up care
Your child with aplastic anemia should continue to be monitored by a physician into adulthood. Your child’s physician may recommend your child see several different specialists because other body systems may be affected.
Activities that put your child with aplastic anemia at risk for infection or bleeding should be avoided. These activities include the following:
- Dental work (until your child’s white blood cell counts rise)
- Contact sports (i.e., football, hockey, skiing, or rollerblading)
- Traveling to high altitudes (children with a low red blood cell count will have increased fatigue and need for oxygen in high altitudes)
If your child has a relapse of aplastic anemia, additional treatment — including a possible bone marrow transplant — may be necessary.
Iron deficiency anemia in children
The most common cause of pediatric anemia is iron deficiency. Iron is needed to form hemoglobin. Iron is mostly stored in the body in the hemoglobin. About 30 percent of iron is also stored as ferritin and hemosiderin in the bone marrow, spleen and liver.
Iron deficiency anemia in children causes
Iron deficiency anemia can be caused by:
- Diets low in iron — Iron is obtained from foods in our diet, however, only 1 mg of iron is absorbed for every 10 to 20 mg of iron ingested. A child unable to have a balanced iron-rich diet may suffer some degree of iron deficiency anemia.
- Body changes — An increased iron requirement and increased red blood cell production is required when the body is going through changes such as growth spurts in children and adolescents.
- Gastrointestinal tract abnormalities — Malabsorption of iron is common after some forms of gastrointestinal surgeries. Most of the iron taken in by dietary route is absorbed in the upper small intestine. Any abnormalities in the gastrointestinal (GI) tract could alter iron absorption and result in iron deficiency anemia.
- Blood loss — Loss of blood can cause a decrease of iron and result in iron deficiency anemia. Sources of blood loss may include GI bleeding, menstrual bleeding, or injury.
Pediatric iron deficiency anemia prevention
During Pregnancy and Delivery
Up to 42% of pregnant women worldwide will have anemia, with a prevalence of 6% in North America. The iron requirement increases with each trimester and should be supported by higher maternal iron intake 7. Between 60% and 80% of the iron storage in a newborn occurs during the third trimester 1, but it is unclear whether treatment of maternal anemia prevents anemia in newborns and infants. The U.S. Preventive Services Task Force found insufficient evidence to recommend screening for or treating iron deficiency anemia in pregnant women to improve maternal or neonatal outcomes 8. Although two Cochrane reviews found that maternal hemoglobin levels improve with antepartum iron supplementation, studies have not demonstrated statistically significant benefits in clinical outcomes (e.g., low birth weight, preterm birth, infection, postpartum hemorrhage) for mothers or newborns 9.
Delayed umbilical cord clamping (approximately 120 to 180 seconds after delivery) is associated with improved iron status (ferritin levels) at two to six months of age 10. This benefit may be especially important in those vulnerable to iron deficiency, such as infants who were premature or small for gestational age. A Cochrane review 11 looking at the effects of the timing of cord clamping during preterm births showed a reduction of blood transfusions when clamping was delayed (24% vs. 36%). The effects of delayed cord clamping do not appear to persist beyond the first 12 months 12.
Iron Supplementation During Infancy
Iron is the most common single-nutrient deficiency. Preterm infants (born at less than 37 weeks’ gestation) who are exclusively breastfed should receive 2 mg per kg per day of elemental iron supplementation from one to 12 months of age, except for those who have had multiple blood transfusions 1. In healthy full-term infants, iron storage from in utero is adequate for the first four to six months of life 13. The American Academy of Pediatrics recommends that full-term, exclusively breastfed infants start 1 mg per kg per day of elemental iron supplementation at four months of age until appropriate iron-containing foods are introduced 1. Table 5 includes daily iron supplementation and requirements for children. Various oral iron formulations and dosing for supplementation and treatment of anemia are listed in Table 6. Formula-fed infants often receive adequate amounts of iron (average formula contains 10 to 12 mg per L of iron) and thus rarely require further supplementation 1.
Ideally, the estimated 7-mg daily iron requirement for children one to three years of age should be met through consumption of iron-rich foods 1. Consumption of large quantities of non–iron-fortified cow’s milk increases the risk of iron deficiency 14. Although iron supplementation may achieve more significant improvements in hemoglobin concentration, children are more likely to tolerate iron-fortified foods 15. Table 3 lists common childhood foods and their elemental iron content 1. If achieving daily iron supplementation is difficult, intermittent iron supplementation still improves hemoglobin concentration and reduces the risk of iron deficiency 16.
Iron deficiency anemia in children signs and symptoms
Each child may experience different symptoms or varying severity of symptoms from iron deficiency anemia. Symptoms may include:
- Abnormal paleness or lack of color of the skin
- Irritability
- Lack of energy or tiring easily (fatigue)
- Increased heart rate (tachycardia)
- Sore or swollen tongue
- Enlarged spleen
- A desire to eat peculiar substances such as dirt or ice (also called pica)
Iron deficiency anemia in children diagnosis
Diagnosing iron deficiency anemia begins with a complete medical history and physical examination of your child. A physician may order additional diagnostic tests or procedures for iron deficiency anemia, including:
- Blood tests to measure the amount of hemoglobin (number of red blood cells) that are present; and measure the amount of iron in your child’s blood
- Bone marrow aspiration and/or biopsy, a procedure where a small amount of bone marrow fluid (aspiration) and/or solid bone marrow tissue (called a core biopsy), usually from the hip bones, is examined for the number, size, and maturity of blood cells and/or abnormal cells.
Iron deficiency anemia in children treatments
Specific treatment for iron deficiency anemia will be determined by your child’s physician based on:
- Your child’s age, overall health and medical history
- Extent of the anemia
- Cause of the anemia
- Your child’s tolerance for specific medications, procedures or therapies
- Expectations for the course of the anemia
- Your opinion or preference
Treatment may include:
An iron-rich diet
Eating a diet with iron-rich foods can help treat iron deficiency anemia. Good sources of iron include the following:
- Meats — beef, pork, lamb, liver, and other organ meats
- Poultry — chicken, duck, turkey, liver (especially dark meat)
- Fish — shellfish, including clams, mussels, and oysters, sardines, anchovies
- Leafy greens of the cabbage family — broccoli, kale, turnip greens, and collards
- Legumes, such as lima beans and green peas; dry beans and peas, such as pinto beans, black-eyed peas, and canned baked beans
- Yeast-leavened whole-wheat bread and rolls
- Iron-enriched white bread, pasta, rice, and cereals
Iron supplements
Iron supplements can be taken over several months to increase iron levels in the blood. Iron supplements can cause irritation of the stomach and discoloration of bowel movements. They should be taken on an empty stomach or with orange juice to increase absorption. Always consult your child’s physician regarding the recommended daily iron requirements for your child. Iron-Rich Foods listed by quantity/approximate iron content in milligrams:
Table 3: Selected Food Sources of Iron
| Food | Milligrams per serving |
| Breakfast cereals, fortified with 100% of the DV for iron, 1 serving | 18 |
| Oysters, eastern, cooked with moist heat, 3 ounces | 8 |
| White beans, canned, 1 cup | 8 |
| Chocolate, dark, 45%–69% cacao solids, 3 ounces | 7 |
| Beef liver, pan fried, 3 ounces | 5 |
| Lentils, boiled and drained, ½ cup | 3 |
| Spinach, boiled and drained, ½ cup | 3 |
| Tofu, firm, ½ cup | 3 |
| Kidney beans, canned, ½ cup | 2 |
| Sardines, Atlantic, canned in oil, drained solids with bone, 3 ounces | 2 |
| Chickpeas, boiled and drained, ½ cup | 2 |
| Tomatoes, canned, stewed, ½ cup | 2 |
| Beef, braised bottom round, trimmed to 1/8” fat, 3 ounces | 2 |
| Potato, baked, flesh and skin, 1 medium potato | 2 |
| Cashew nuts, oil roasted, 1 ounce (18 nuts) | 2 |
| Green peas, boiled, ½ cup | 1 |
| Chicken, roasted, meat and skin, 3 ounces | 1 |
| Rice, white, long grain, enriched, parboiled, drained, ½ cup | 1 |
| Bread, whole wheat, 1 slice | 1 |
| Bread, white, 1 slice | 1 |
| Raisins, seedless, ¼ cup | 1 |
| Spaghetti, whole wheat, cooked, 1 cup | 1 |
| Tuna, light, canned in water, 3 ounces | 1 |
| Turkey, roasted, breast meat and skin, 3 ounces | 1 |
| Nuts, pistachio, dry roasted, 1 ounce (49 nuts) | 1 |
| Broccoli, boiled and drained, ½ cup | 1 |
| Egg, hard boiled, 1 large | 1 |
| Rice, brown, long or medium grain, cooked, 1 cup | 1 |
| Cheese, cheddar, 1.5 ounces | 0 |
| Cantaloupe, diced, ½ cup | 0 |
| Mushrooms, white, sliced and stir-fried, ½ cup | 0 |
| Cheese, cottage, 2% milk fat, ½ cup | 0 |
| Milk, 1 cup | 0 |
Table 4: Recommended Dietary Allowances (RDAs) for Iron
| Age | Male | Female | Pregnancy | Lactation |
|---|---|---|---|---|
| Birth to 6 months | 0.27 mg* | 0.27 mg* | ||
| 7–12 months | 11 mg | 11 mg | ||
| 1–3 years | 7 mg | 7 mg | ||
| 4–8 years | 10 mg | 10 mg | ||
| 9–13 years | 8 mg | 8 mg | ||
| 14–18 years | 11 mg | 15 mg | 27 mg | 10 mg |
| 19–50 years | 8 mg | 18 mg | 27 mg | 9 mg |
| 51+ years | 8 mg | 8 mg |
Footnote:
- Recommended Dietary Allowance (RDA): Average daily level of intake sufficient to meet the nutrient requirements of nearly all (97%–98%) healthy individuals; often used to plan nutritionally adequate diets for individuals.
- *Adequate Intake (AI): Intake at this level is assumed to ensure nutritional adequacy; established when evidence is insufficient to develop an RDA.
- Estimated Average Requirement (EAR): Average daily level of intake estimated to meet the requirements of 50% of healthy individuals; usually used to assess the nutrient intakes of groups of people and to plan nutritionally adequate diets for them; can also be used to assess the nutrient intakes of individuals.
- Tolerable Upper Intake Level (UL): Maximum daily intake unlikely to cause adverse health effects.
Table 5. Elemental Iron Supplementation or Requirement in Children
| Age | Iron supplementation or requirement |
|---|---|
Preterm (< 37 weeks’ gestation) infants: 1 to 12 months | 2 mg per kg per day supplementation if exclusively breastfed |
1 mg per kg per day supplementation if using iron-fortified formula | |
Term infants: 4 to 6 months to 12 months | 1 mg per kg per day supplementation if exclusively breastfed |
Supplementation not needed if using iron-fortified formula | |
Toddlers 1 to 3 years | Requires 7 mg per day; modify diet and/or supplement if anemic |
Children 4 to 8 years | Requires 10 mg per day; modify diet and/or supplement if anemic |
Table 6. Oral Iron Formulations and Dosing
| Formulation | Dosing (elemental iron) |
|---|---|
Ferrous fumarate | Tablet: 90 (29.5) mg, 324 (106) mg, 325 (106) mg, 456 (150) mg |
Ferrous gluconate | Tablet: 240 (27) mg, 256 (28) mg, 325 (36) mg |
Ferrous sulfate | Drops and oral solution: 75 (15) mg per mL |
Elixir and liquid: 220 (44) mg per 5 mL | |
Syrup: 300 (60) mg per 5 mL | |
Tablet: 300 (60) mg, 324 (65) mg, 325 (65) mg | |
Extended-release tablets: 140 (45) mg, 160 (50) mg, 325 (65) mg | |
Polysaccharide-iron complex and ferrous bisglycinate chelate | Capsule: elemental iron (50 mg, 150 mg with or without 50 mg vitamin C) |
Elixir: elemental iron (100 mg per 5 mL) |
Sickle cell disease in children
Sickle cell disease is the name of a group of inherited blood disorders that is characterized by chronic anemia, periodic episodes of pain and other complications.
The disease affects the red blood cells. Sickle cell disease results when red blood cells make mostly hemoglobin S instead of the normal hemoglobin A. Normal red blood cells are smooth, round and soft; their shape and softness enable them to move easily through the blood vessels to carry oxygen to all parts of the body.
In sickle cell disease, the abnormal hemoglobin S causes the red blood cells to become hard, pointed and sticky and shaped like crescents or sickles. When these hard and pointed red cells go through the small blood vessels, they often get stuck and block the vessels. They also stick to and damage the lining of larger blood vessels. The damaged vessels become scarred, narrowed and sometimes completely closed. The blockage of blood flow through blood vessels can lead to pain, stroke and damage to many organs.
Sickle cells also break up too easily and survive for only 10 to 20 days compared to 120 days for normal red blood cells. The rapid destruction of sickle cells leads to anemia — a shortage of red blood cells and hemoglobin. It becomes difficult for the body to make new red blood cells fast enough to keep up with the needed supply.
Sickle cell disease in children causes
Sickle cell conditions are inherited. People who make hemoglobin S in their red blood cells have inherited the sickle cell gene from one or both parents. Children who inherit the sickle cell gene from both parents will have sickle cell disease (SS). The sickle cell gene tells the body to make a variant (different from normal) hemoglobin. Children who inherit the sickle cell gene (S) from one parent and another abnormal hemoglobin gene from the other parent may have different types of sickle cell disease.
There are four common types of sickle cell disease: SS, SC, S/beta-plus thalassemia, and S/beta-zero thalassemia. A person who is SS has inherited a double dose of the sickle cell gene (S), one from each parent. People with any other type of sickle cell disease have inherited the S gene from one parent and another abnormal hemoglobin gene from the other parent.
Children who inherit the sickle cell (S) gene from only one parent and the normal genes for hemoglobin A from the other parent will not have the disease, but will have the sickle cell trait (AS). People with sickle cell trait (AS) generally have no symptoms of the disease and lead normal lives, but can pass the gene on to their children.
When two people with the sickle cell trait have a baby, they can have a child with normal hemoglobins (AA), sickle cell trait (AS), or the SS type of sickle cell disease. These possibilities exist with each pregnancy.
Risk factors for sickle cell disease
Sickle cell disease affects millions of people throughout the world. It is common in people whose origins are:
- African
- Mediterranean
- Arabian
- Indian (Asian)
People with sickle cell conditions predominantly live in countries in Africa, the Americas (North, Central and South), the Caribbean region, Mediterranean region, the Middle East, India and Western Europe.
In the United States, sickle cell disease affects 19:
- 1 in approximately 360 African-American newborns
- 1 in approximately 16,300 Hispanic-American newborns
It has been estimated that more than 2 million Americans carry the sickle cell “trait” (which means they don’t have the disease themselves but could potentially pass it on to their children). About 1 in 12 African-Americans has the sickle cell trait.
Sickle cell disease in children signs and symptoms
Anemia is the most common feature of sickle cell disease. Anemia may cause fatigue, paleness, yellowing of the skin and eyes (jaundice), or shortness of breath.
Pain is the most common symptom of sickle cell disease. Some people have few or no severe pain episodes a year while others have 15 or more. Pain may last a few hours to a few days, and, in some cases, it can last for weeks. Some people have chronic, almost daily pain.
The pain occurs in organs or joints and results from tissue damage caused when sickle cells block blood flow. Mild pain episodes may be treated with over-the-counter pain medications such as acetaminophen and ibuprofen. Pain that is severe may require treatment in the hospital with strong pain medicines given intravenously (into a vein).
Complications of sickle cell disease may be acute or or chronic.
Acute complications
- Anemia. It is the most common feature of sickle cell disease. Anemia may cause fatigue, paleness, yellowing of the skin and eyes (jaundice), or shortness of breath.
- Pain. It is the most common symptom of sickle cell disease. Some people have few or no severe pain episodes a year while others have several. The duration of pain can vary, and some people have chronic, almost daily pain. This is the result from tissue damage caused when sickle cells block blood flow. Mild pain episodes may be treated with heat (warm baths or compresses) and over-the-counter pain medications such as acetaminophen and ibuprofen. Pain that is severe may require treatment in the hospital with strong pain medicines given intranasal (into the nose) and intravenously (into a vein).
- Infection. Repeated red cell sickling within the spleen causes it to lose the ability to remove bacteria from the blood. Infants and young children are susceptible to blood infections, pneumonia, meningitis, and bone and other serious infections. Individuals are given twice-daily penicillin and vaccines to prevent serious infection and death. Fever should be immediately evaluated by a healthcare provider.
- Splenic sequestration. Sickled red blood cells can become trapped in the spleen. The spleen becomes larger and is frequently painful. The blood in the spleen is no longer in the circulation, and the patient can become pale and tired from the anemia. This is a life-threatening emergency and requires immediate evaluation by a healthcare provider.
- Aplastic crises. Infection with parvo virus B19 can cause an aplastic crisis. The bone marrow temporarily stops making red blood cells and the patient becomes more anemic. Sometimes patients may need a red blood cell transfusion.
- Dactylitis (hand-foot syndrome). Swollen and/or painful hands or feet may be the first symptom of sickle cell disease in infants and should be evaluated by a doctor immediately.
- Acute chest syndrome. This life-threatening complication of sickle cell disease is caused by trapped sickle cells or infection in the lung. People who have chest pain and fever must be seen by a doctor immediately.
- Stroke. Sickled cells damage and block blood vessels that supply blood to the brain; this may result in a stroke. About 10 percent of children with sickle cell disease develop stroke. Another 20 percent develop scars in the brain without stroke. The damage to brain tissue can cause learning problems and disabilities. Doctors can sometimes identify children who are at increased risk of stroke by using a special type of ultrasound test.
- Priapism. This refers to painful and unwanted erections, which occur because sickled red blood cells cause blood to be trapped in the vessels of the penis. Immediate medical attention is needed when the erection lasts for more than an hour. Recurrent priapism can lead to erectile dysfunction.
Chronic complications
- Gallstones. These stones form in the gallbladder when there is too much of a substance called bilirubin in the body; bilirubin is made when red blood cells are destroyed. People with gallstones may have pain episodes in the upper right side of the belly, under the right shoulder or between the shoulder blades. They may also experience yellowing of the eyes or skin. Eating a large or fatty meal may trigger gallstone attacks.
- Pulmonary hypertension. This is high blood pressure of the main artery to the lungs (pulmonary artery); this artery carries blood from the heart to the lungs where it becomes oxygenated. Pulmonary hypertension is a common complication of adults with sickle cell disease and has become more widely recognized in children. Early diagnosis and treatment may reverse or prevent progress of this condition.
- Joint disease. Aseptic necrosis (death of tissue not related to infection) of bone is the most common problem of bones and joints related to sickle cell disease. It is caused by sickled cells blocking blood flow. This condition can begin in childhood but is more common later in life.
- Eye problems. When the retina does not get enough blood, it can weaken and result in problems, including blindness. Children with sickle cell disease need regular eye exams, as tiny blood vessels in the eye may become blocked with the sickled cells. Early detection of these problems can allow treatment to prevent poor vision or complete blindness.
- Kidney problems. The inability to maximally concentrate urine is the most common renal abnormality in sickle cell disease. One result is enuresis (bedwetting). Another is an increased susceptibility to dehydration, which can initiate vaso-occlusive events (painful episodes). To compensate, people with sickle cell disease should drink large amounts of fluids; this is particularly important for children at play in warm weather.
- Neuropsychological effects. Silent strokes and cerebral vessel narrowing are common in young children with sickle cell disease, and it puts them at increased risk for cognitive deficits. These can lead to learning difficulties. Neuropsychological testing of children with poor academic performance should be conducted, so appropriate interventions can be started. Also, early brain imaging studies can provide information so that interventions can be started as soon as possible.
Sickle cell disease in children diagnosis
Sickle cell conditions can be accurately diagnosed at any age. However, the newborn period is the best time. Newborn diagnosis enables healthcare providers to start preventive treatment (penicillin prophylaxis) and family health education before the start of symptoms.
Forty-nine U.S. states, the District of Columbia, Puerto Rico and the Virgin Islands currently screen all newborns for sickle cell disease through blood tests. These tests use blood from the same samples taken for other routine newborn screening tests and can determine if the child has the disease itself or only the trait. It is also possible to identify sickle cell disease before birth by getting a sample of amniotic fluid or tissue taken from the placenta; this test can be done as early as the first few months of pregnancy.
There are several tests suitable for determining what type of hemoglobin is made by a person’s red blood cells. These include:
- Hemoglobin electrophoresis
- Isoelectric focusing
- Chromatography
These tests can determine whether a person has a type of sickle cell disease or sickle cell trait.
DNA analysis is used to determine changes in the genes for making hemoglobin. This test indirectly predicts the type of hemoglobin made in the red cells.
Tests that are not suitable for determining sickle cell disease or sickle cell trait include:
- Solubility tests (e.g., Sickledex®)
- Sickling test
A “positive” result from these tests simply indicates the presence of hemoglobin S in a person’s blood; this occurs in both sickle cell trait and all types of sickle cell disease.
Other tests that are not useful by themselves for diagnosing sickle cell conditions include:
- Blood count. This test may detect anemia, but there are many other causes of anemia in infants and others with mild types of sickle cell disease, and there may be little or no anemia.
- Blood smear. Sickled cells can be easily seen on a blood smear examined under a microscope. However, even in some people with severe sickle cell disease and particularly in young children and in others with milder types of sickle cell disease, there may be no sickled cells on the regular blood smears.
Sickle cell disease in children treatment
The goals of treatment are to prevent infections, relieve pain, and prevent or control complications. Infections are the leading cause of death in sickle cell disease. Pain attacks are the leading cause of emergency room visits and hospitalizations.
Because infections may lead to death, special measures are taken to prevent or reduce the severity of infections. This includes twice-daily penicillin for children for at least the first five years of life, special vaccines, and aggressive evaluation and treatment when patients develop fever or other signs of infection.
Vaccinations against certain dangerous bacteria (pneumococcus, haemophilus influenza type B, and meningococcus) and viruses (hepatitis B and influenza) are especially important for people with sickle cell disease. For more information about what vaccinations your child needs, visit the Children’s Hospital of Philadelphia Vaccine Education Center.
Blood transfusions are used to treat some acute complications and to prevent the occurrence or recurrence of other complications. Children who have had a stroke or are at high risk for initial stroke are given blood transfusions on a regular and long-term basis to prevent stroke.
Pain is most often treated with acetaminophen, nonsteroidal anti-inflammatory drugs (also known as NSAIDs) and opioids, which are the strongest pain medications and include substances such as morphine, oxycodone and hydrocodone.
Sickle cell disease in children follow-up care
Important health maintenance measures in sickle cell disease include:
- Doctor visits every two or three months for children up to 2 years of age, then at least every three to four months after age 2
- Regular well visits to a sickle cell clinic or primary healthcare provider
- All recommended well child immunizations with the addition of Prevnar® and Pneumovax® vaccines, which protect against pneumococcus
- Blood tests to monitor blood counts when well
- Antibiotic (penicillin) prophylaxis in young children
- Folic acid supplementation
- Transcranial Doppler (TCD) (an ultrasound of the brain) at least once a year in children with sickle cell disease-SS and sickle cell disease-SB0 thalassemia starting at 2 years and until 16 years of age
- Hydroxyurea therapy beginning at 9 months of age in children with sickle cell disease-SS and sickle cell disease-SB0 thalassemia
- Eye (retina) examination for early detection of retina disease
Researchers are investigating new medications, bone marrow transplants and gene therapy to treat and possibly provide a universal for cure sickle cell disease. Fortunately, a child may live a full, productive life with the disease as doctors know a great deal about the disease and how to manage it.
Pediatric anemia causes
Generally, anemia may be caused by several problems, including the following:
- Infection
- Certain diseases
- Certain medications
- Poor nutrition
The underlying pathologic processes that cause anemia can be broadly categorized as (1) decreased or ineffective red cell production, (2) increased red cell destruction (hemolysis), and (3) blood loss, although more than 1 mechanism may be involved in some anemias.
Anemia caused by decreased red cell production
This generally develops gradually and causes chronic anemia. Marrow failure may result from the following:
- Diamond-Blackfan anemia (congenital pure red cell aplasia)
- Transient erythroblastopenia of childhood
- Physiologic anemia of infancy. High levels of hemoglobin and red blood cells help fetal blood carry enough oxygen to developing babies in utero. After the birth, more oxygen is available and a baby’s hemoglobin level normally drops to a low point at about 2 months of age. This temporary and expected drop in the blood count is normal and no treatment is needed because the baby’s body soon starts making red blood cells on its own.
- Aplastic crisis caused by parvovirus B19 infection (in patients with an underlying chronic hemolytic anemia)
- Marrow replacement (eg, leukemia, neuroblastoma, medulloblastoma, retinoblastoma, Ewing sarcoma, soft tissue sarcoma, myelofibrosis, osteopetrosis)
- Aplastic anemia
- Aplastic anemia happens when the bone marrow can’t make enough blood cells. This can be due to a viral infection, or exposure to certain toxic chemicals, radiation, or medicines (like antibiotics, anti-seizure drugs, or cancer treatments). Some childhood cancers like leukemia can cause it, while some genetic and other chronic diseases can affect how the bone marrow works.
- Paroxysmal nocturnal hemoglobinuria
- Iron deficiency anemia. This is the most common cause of anemia in kids. It can affect kids at any age, but is most common in those younger than 2 years old. Because iron is essential to hemoglobin production, anemia can happen when someone has an iron deficiency. Poor dietary iron intake (or excessive loss of iron from the body) can lead to iron deficiency anemia. Young children who drink excessive amounts of milk are at increased risk for iron deficiency. Girls going through puberty also have a high risk for iron deficiency anemia because of the onset of menstruation. They should be sure to include plenty of iron in their diets because of this monthly blood loss.
Impaired erythropoietin production may result from the following:
- Anemia of chronic disease in renal failure
- Chronic inflammatory diseases
- Hypothyroidism
- Severe protein malnutrition
Defect in red cell maturation and ineffective erythropoiesis may result from the following:
- Nutritional anemia secondary to iron, folate, or vitamin B-12 deficiency
- Congenital dyserythropoietic anemia
- Sideroblastic anemias
- Thalassemias
- Thalassemia affects the way the body makes hemoglobin. The body contains more red blood cells than any other type of cell, and each has a life span of about 4 months. Each day, the body produces new red blood cells to replace those that die or are lost from the body. With thalassemia, the cells are destroyed at a faster rate, leading to anemia. Thalassemia major, also called Cooley’s anemia is a severe form of anemia where red blood cells are rapidly destroyed and iron is deposited in the vital organs. Thalassemia minor causes less severe anemia.
- Erythropoietic protoporphyria
- Myelodysplastic syndromes 20
Anemia caused by increased red cell destruction
When the body destroys red blood cells (a process called hemolysis) more quickly than normal, the bone marrow makes up for it by increasing production of new red cells. But if red blood cells are destroyed faster than they can be replaced, a person will develop anemia. This is called hemolytic anemia.
Autoimmune hemolytic anemia happens when the body’s immune system mistakenly attacks and destroys RBCs. This can happen because of disease, but sometimes no cause is found.
Inherited hemolytic anemia is due to an inherited (passed down from parents to their children) defect in the red blood cells. These defects can cause anemia. Common forms of inherited hemolytic anemia include sickle cell disease, thalassemia, glucose-6-phosphate dehydrogenase (G6PD) deficiency, and hereditary spherocytosis.
Extracellular causes may include the following:
- Mechanical injury (hemolytic-uremic syndrome, cardiac valvular defects, Kasabach-Merritt syndrome or hemangioma with thrombocytopenia)
- Antibodies (autoimmune hemolytic anemia)
- Infections, drugs, toxins
- Thermal injury to red blood cells (with severe burns)
Intracellular causes may include the following:
- Red cell membrane defects (eg, hereditary spherocytosis, elliptocytosis)
- Hereditary spherocytosis is an inherited condition where red blood cells aren’t shaped correctly (like tiny spheres, instead of disks) and are very fragile because of a genetic problem with a protein in the structure of the red blood cell. This causes the cells to be easily destroyed and can cause anemia, jaundice (yellow-tinged skin), and enlargement of the spleen. A family history increases the risk for this disorder, which is most common in people of northern European heritage but can affect all races.
- Enzyme defects (eg, glucose-6-phosphate dehydrogenase (G6PD) deficiency, pyruvate kinase deficiency)
- G6PD deficiency. G6PD is one of many enzymes that help the body process carbohydrates and turn them into energy. G6PD also protects RBCs from harmful byproducts that can gather when a person takes certain medicines or when the body is fighting an infection. In people with G6PD deficiency, either the red blood cells don’t make enough G6PD or what’s produced doesn’t work correctly. Without enough G6PD to protect them, the cells can be damaged or destroyed. G6PD deficiency most commonly affects males of African heritage, although it has been found in many other people.
- Hemoglobinopathies (sickle cell disease, unstable hemoglobinopathies)
- Sickle cell disease is a severe form of anemia that’s most common in people of African heritage (about 1 out of every 500 African-American children is born with it). It affects hemoglobin, a protein in red blood cells that helps carry oxygen throughout the body. RBCs with normal hemoglobin move easily through the bloodstream because of their rounded shape and flexibility. Sickle cell disease makes RBCs sticky, stiff, and more fragile, and they form into a curved, sickle shape. Instead of moving through the bloodstream easily, sickle cells can clog blood vessels. When blood can’t get where it’s needed, the body’s tissues and organs don’t have the oxygen they need to stay healthy.
- Paroxysmal nocturnal hemoglobinuria
Anemia caused by blood loss
Blood loss can cause anemia — whether from excessive bleeding due to injury, surgery, or a problem with the blood’s clotting ability. Slower, long-term blood loss, such as intestinal bleeding from inflammatory bowel disease, also can cause anemia, as can heavy menstrual periods in teen girls and women. All of these factors increase the body’s need for iron because iron is needed to make new red blood cells.
Obvious or occult sites of blood loss may include the gastrointestinal tract or intra-abdominal, pulmonary, or intracranial (in neonates) sites. Patients with bleeding disorders are at particular risk for massive hemorrhage (internal or external).
Acute anemia caused by multiple mechanisms
Anemia associated with acute infection is common. This may be mediated by increased destruction by erythrophagocytosis 21 and suppression of erythropoiesis by the infection.
Pediatric anemia prevention
Many kinds of anemia cannot be prevented. But you can help protect your kids from iron deficiency, the most common form of anemia. Before following any of these suggestions, though, be sure to talk them over with your doctor:
Limiting cow’s milk
During their first 6 months, babies are usually protected against developing an iron deficiency by the stores of iron built up in their bodies before birth. But after month 6, they often don’t get enough iron through breast milk alone or regular cow’s milk (which contains less iron than fortified infant formula). Regular cow’s milk can cause some infants to lose iron, and drinking lots of cow’s milk can make a baby less interested in eating other foods that are better sources of iron.
For these reasons, regular cow’s milk is not recommended for children until they’re 1 year old and eating an iron-rich diet. And they should not drink more than 24–32 ounces (709–946 ml) of milk each day. If you can’t get your child to eat more iron-rich foods, speak with your doctor about giving your child an iron supplement.
Iron-fortified cereal and formula
These can help make sure your baby gets enough iron, especially during the transition from breast milk or formula to solid foods.
Well-balanced diet
Make sure your kids regularly eat foods that contain iron. Good choices include iron-fortified grains and cereals, red meat, egg yolks, leafy green vegetables, yellow vegetables and fruits, tomatoes, molasses, and raisins.
If your child is a vegetarian, make an extra effort to ensure sufficient iron sources because iron found in meat, poultry, and fish is more easily absorbed than iron found in plant-based and iron-fortified foods.
Also, certain food combinations can lower the amount of iron the body can absorb (for example, drinking coffee or tea or iced tea with a meal). On the other hand, vitamin C helps the body absorb iron.
Pediatric anemia symptoms
Most symptoms of anemia are a result of the decrease of oxygen in the cells or “hypoxia.” Because red blood cells (as hemoglobin) carry oxygen, a decreased production or number of these cells result in “hypoxia.” Many of the symptoms will not be present with mild anemia, as the body can often compensate for gradual changes in hemoglobin.
Each child may experience symptoms of anemia differently. Symptoms may include:
- Abnormal paleness or lack of color of the skin
- Increased heart rate (tachycardia)
- Breathlessness, or difficulty catching a breath (dyspnea)
- Lack of energy, or tiring easily (fatigue)
- Dizziness, or vertigo especially when standing
- Headache
- Irritability
- Irregular menstruation cycles
- Absent or delayed menstruation (amenorrhea)
- Sore or swollen tongue (glossitis)
- Jaundice, or yellowing of skin, eyes, and mouth
- Enlarged spleen or liver (splenomegaly, hepatomegaly)
- Slow or delayed growth and development
- Impaired wound and tissue healing
The symptoms of anemia may resemble other blood disorders or medical problems. Because anemia is often a symptom associated with another disease, it is important for your child’s physician to be aware of symptoms your child may be experiencing. Always consult your child’s physician for a diagnosis.
The acute development of anemia in the pediatric age group commonly occurs in 2 situations, (1) acute blood loss and (2) acute hemolysis.
Acute blood loss
In neonates, blood loss can occur through the placenta, abruption, placenta previa, and fetomaternal transfusion. The former 2 can be known by history, while fetomaternal transfusion cannot be discerned from history findings. Iatrogenic blood loss through multiple blood samplings in extremely low birth weight infants can cause anemia rapidly.
In older children, the gastrointestinal tract is the most common site of blood loss; common causes include esophageal and gastric varices (inquire about a history of umbilical vein catheterization during neonatal ICU stay), ulcerative colitis, and Crohn disease. Menstruating girls’ blood loss due to dysmenorrhea is an extremely common cause of acute blood loss (may or may not be associated with von Willebrand disease; ask about easy bruisability, frequent epistaxis, and family history of similar bleeding history).
A history of trauma is important (eg, rupture of spleen)
Rapid hemolysis
- Isoimmune or alloimmune hemolytic anemia (ABO incompatibility or Rh incompatibility in neonates) – (1) Mother’s blood group (ABO) and type (Rh); (2) minor Rh antigen incompatibility such as c, E, may cause severe hemolytic anemia (even if there is no ABO or D incompatibility), therefore do direct antiglobulin test (DAT) whenever there is a suspicion
- Autoimmune hemolytic anemia – (1) History of a viral infection such as mycoplasma or Ebstein-Barr virus (EBV) may precede paroxysmal cold hemoglobinuria; (2) an infection with Streptococcuspneumoniae may cause autoimmune hemolytic anemia due to exposure of cryptic T antigen on the red blood cells by the bacterial neuraminidase
- Transfusion reaction due to major blood group incompatibility – Usually due to clerical error or misidentification of patient delayed transfusion reaction due to previously unrecognized antibodies to red blood cell antigens (may occur a few days to 1 wk after previous transfusion)
- Ingestion of strong oxidants in a child with G6PD deficiency – Ingestion or sniffing of a mothball is most common
- Splenic sequestration in a child with sickle cell anemia or hereditary spherocytosis – Sudden onset of severe abdominal pain; shocklike state with a drop in hemoglobin and platelet count
Pediatric anemia diagnosis
Diagnosing anemia begins with a complete medical history and physical examination of your child. Your child’s physician may order additional diagnostic procedures including:
- Blood tests to measure the concentration of hemoglobin and the number of red blood cells in your child’s blood
- A complete blood count (CBC) may show that there are fewer red blood cells than normal.
- Blood smear examination: Blood is smeared on a glass slide for microscopic examination of red blood cells, which can sometimes indicate the cause of the anemia.
- Iron tests: These include total serum iron and ferritin tests, which can help determine if anemia is due to iron deficiency.
- Hemoglobin electrophoresis: This identifies any abnormal types of hemoglobin and helps diagnose sickle cell disease, thalassemia, and other inherited forms of anemia.
- Reticulocyte count: A measure of young red blood cells, this helps doctors see if red blood cell production is at normal levels.
- Bone marrow aspiration and/or biopsy, a procedure that involves taking a small amount of bone marrow fluid (aspiration) and/or solid bone marrow tissue (called a core biopsy), usually from the hip bones, to be examined for the number, size, and maturity of blood cells and/or abnormal cells.
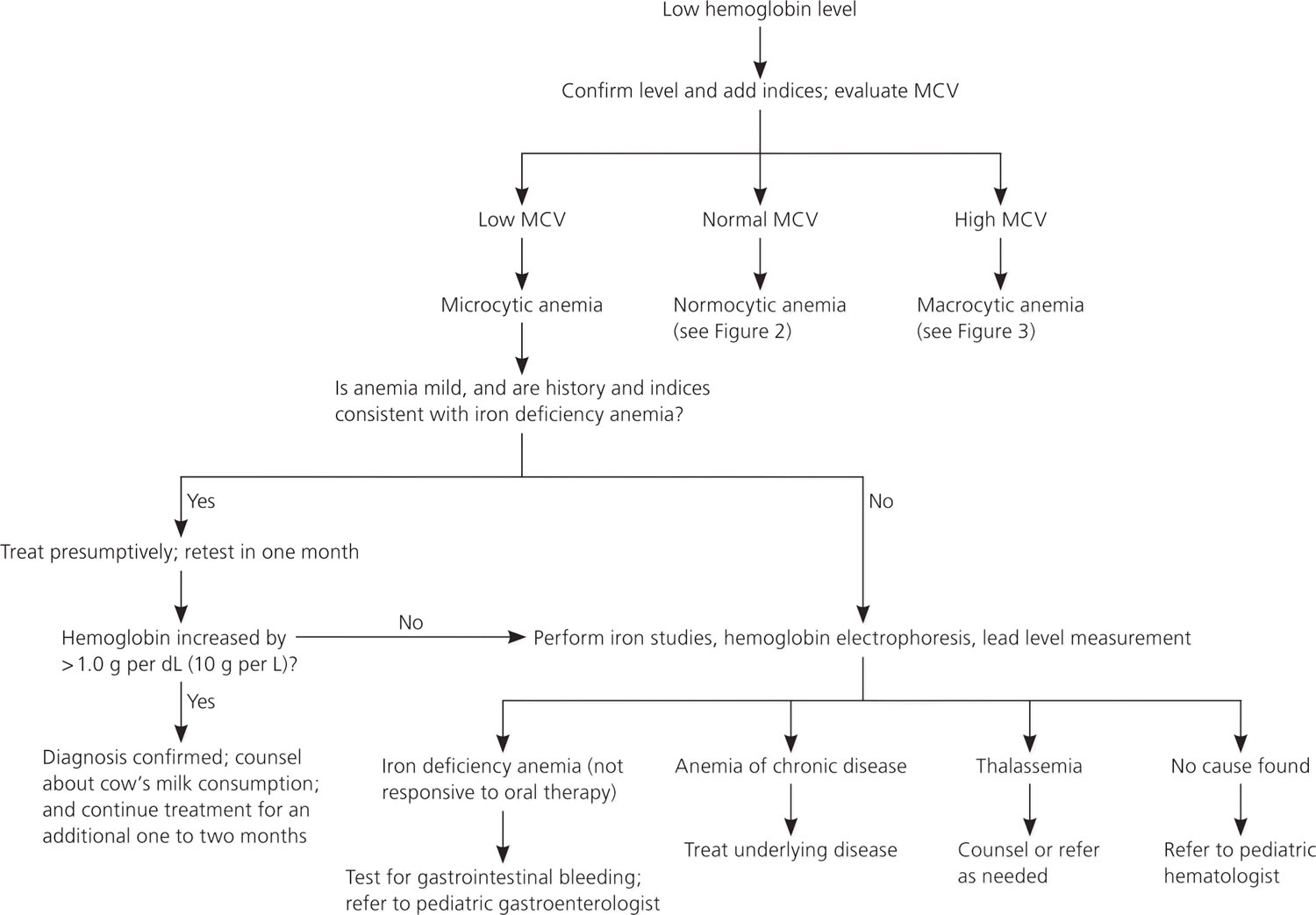
Figure 1 is an algorithm for the evaluation of children with low hemoglobin levels 6.
Figure 1. Evaluation of low hemoglobin levels in children
Pediatric anemia treatment
Treatment for anemia depends on its cause. The type, cause, and severity of your child’s anemia will determine what kind of care is needed. Kids often tolerate anemia much better than adults. Specific treatment for pediatric anemia will be determined by your child’s physician based on the following:
- Your child’s age, overall health, and medical history
- The extent of the anemia
- The type of anemia
- Cause of the anemia
- Your child’s tolerance for specific medications, procedures or therapies
- Expectations for the course of the anemia
- Your opinion or preference
Pediatric anemia can be challenging to treat because the condition — and what causes the disorder — differs from child to child. Treatments may include:
- Vitamin and mineral supplements
- Change in your child’s diet
- Medication and/or discontinuing causative medications
- Treatment of the causative disorder
- Surgery to remove spleen (if related to hemolytic anemia)
- Blood transfusions, if necessary (to replace significant loss)
- Antibiotics (if infection is causative agent)
- Bone marrow transplant (for aplastic anemia).
For iron deficiency anemia, the doctor may prescribe medicine as drops (for infants) or as a liquid or tablet (for older kids). Medicine usually must be taken for as long as 3 months to rebuild the body’s store of iron. The doctor also may recommend adding certain iron-rich foods to a child’s diet or reducing milk intake.
If your teenage daughter is anemic and has heavy or irregular menstrual periods, the doctor may prescribe hormonal treatment to help regulate the bleeding.
Folic acid and vitamin B12 supplements may be recommended for anemia due to a deficiency of these nutrients. However, this is rare in children.
Anemia caused by an infection will usually improve when the infection passes or is treated. If a certain medicine appears to be the cause, the doctor may discontinue it or replace it with something else (unless the benefit of the drug outweighs this side effect).
Depending on the cause, treatment for more severe or chronic forms of anemia may include:
- transfusions of normal red blood cells taken from a donor
- removal of the spleen or treatment with medicines to prevent blood cells from being removed from circulation or destroyed too rapidly
- medicines to fight infection or stimulate the bone marrow to make more blood cells
In some cases of sickle cell anemia, thalassemia, and aplastic anemia, bone marrow transplantation may be used. In this procedure, bone marrow cells taken from a donor are injected into the child’s vein. The bone marrow cells then travel through the bloodstream to the bone marrow and make new blood cells.
Pediatric anemia prognosis
Pediatric anemia prognosis depends on the severity and acuteness with which the anemia develops and the underlying cause of the anemia.
Mortality and morbidity rates vary according to the underlying pathologic process causing the anemia, the degree of severity, and the acuteness of the process. When a precipitous drop in the hemoglobin or hematocrit level occurs (eg, due to massive bleeding or acute hemolysis), the clinical presentation is typically dramatic and can be fatal if the person is not immediately treated. In addition to the signs and symptoms of anemia, patients can present with congestive heart failure or hypovolemia. Cerebral injury has been reported in perioperative patients with anemia 22.
- Baker RD, Greer FR; Committee on Nutrition American Academy of Pediatrics. Diagnosis and prevention of iron deficiency and iron-deficiency anemia in infants and young children (0–3 years of age). Pediatrics. 2010;126(5):1040–1050.[↩][↩][↩][↩][↩][↩][↩]
- Pediatric Acute Anemia. https://emedicine.medscape.com/article/954506-overview[↩]
- Flerlage J, Engorn B, eds. The Harriet Lane Handbook: A Manual for Pediatric House Officers. 20th ed. Philadelphia, Pa.: Saunder/Elsevier; 2015:305.[↩]
- World Health Organization. Worldwide prevalence of anaemia 1993–2005. 2008.[↩]
- Iron Deficiency and Other Types of Anemia in Infants and Children. Am Fam Physician. 2016 Feb 15;93(4):270-278. https://www.aafp.org/afp/2016/0215/p270.html[↩][↩][↩][↩]
- Janus J, Moerschel SK. Evaluation of anemia in children. Am Fam Physician. 2010;81(12):1462–1471.[↩][↩]
- Scholl TO. Maternal iron status: relation to fetal growth, length of gestation, and iron endowment of the neonate. Nutr Rev. 2011;69(suppl 1):S23–S29.[↩]
- U.S. Preventive Services Task Force. Iron deficiency anemia in pregnant women: screening and supplementation. September 2015. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/iron-deficiency-anemia-in-pregnant-women-screening-and-supplementation?ds=1&s=Iron%20deficiency%20anemia%20screening%29[↩]
- Pena-Rosas JP, De-Regil LM, Garcia-Casal MN, Dowswell T. Daily oral iron supplementation during pregnancy. Cochrane Database Syst Rev. 2015;(7):CD004736[↩]
- Andersson O, Hellström-Westas L, Andersson D, Domellöf M. Effect of delayed versus early umbilical cord clamping on neonatal outcomes and iron status at 4 months: a randomised controlled trial. BMJ. 2011;343:d7157.[↩]
- Rabe H, Diaz-Rossello JL, Duley L, Dowswell T. Effect of timing of umbilical cord clamping and other strategies to influence placental transfusion at preterm birth on maternal and infant outcomes. Cochrane Database Syst Rev. 2012;(8):CD003248[↩]
- Andersson O, Domellöf M, Andersson D, Hellström-Westas L. Effect of delayed vs early umbilical cord clamping on iron status and neurodevelopment at age 12 months: a randomized clinical trial. JAMA Pediatr. 2014;168(6):547–554.[↩]
- Uijterschout L, Vloemans J, Rövekamp-Abels L, Feitsma H, van Goudoever JB, Brus F. The influences of factors associated with decreased iron supply to the fetus during pregnancy on iron status in healthy children aged 0.5 to 3 years. J Perinatol. 2014;34(3):229–233.[↩]
- Brotanek JM, Halterman JS, Auinger P, Flores G, Weitzman M. Iron deficiency, prolonged bottle-feeding, and racial/ethnic disparities in young children. Arch Pediatr Adolesc Med. 2005;159(11):1038–1042.[↩]
- Rosado JL, González KE, Caamaño Mdel C, García OP, Preciado R, Odio M. Efficacy of different strategies to treat anemia in children: a randomized clinical trial. Nutr J. 2010;9:40–50.[↩]
- De-Regil LM, Jefferds ME, Sylvetsky AC, Dowswell T. Intermittent iron supplementation for improving nutrition and development in children under 12 years of age. Cochrane Database Syst Rev. 2011;(12):CD009085[↩]
- U.S. Department of Agriculture (USDA). https://fdc.nal.usda.gov[↩]
- Institute of Medicine. Food and Nutrition Board. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc : a Report of the Panel on Micronutrients. Washington, DC: National Academy Press; 2001. https://www.nap.edu/read/10026/chapter/1[↩]
- Newborn screening for sickle cell diseases in the United States: A review of data spanning 2 decades. Therrell BL Jr, Lloyd-Puryear MA, Eckman JR, Mann MY. Semin Perinatol. 2015 Apr;39(3):238-51.[↩]
- Niemeyer CM, Baumann I. Myelodysplastic syndrome in children and adolescents. Semin Hematol. 2008 Jan. 45(1):60-70.[↩]
- Ballin A, Hussein A, Vaknine H, Senecky Y, Avni Y, Schreiber L. Anemia associated with acute infection in children: an animal model. J Pediatr Hematol Oncol. 2013 Jan. 35(1):14-7.[↩]
- Hare GM, Tsui AK, McLaren AT, Ragoonanan TE, Yu J, Mazer CD. Anemia and cerebral outcomes: many questions, fewer answers. Anesth Analg. 2008 Oct. 107(4):1356-70.[↩]