Plastic bronchitis
Plastic bronchitis is a rare lymphatic flow disorder and potentially fatal disease that causes severe respiratory issues. In children with plastic bronchitis, lymph fluid builds in the airways and forms rubbery or caulk-like plugs known as bronchial casts. These casts block the airways and can cause obstruction of an entire lung, making it difficult to breathe 1. Bronchial casts can be seen in diseases associated with diffuse bronchial hypersecretion like asthma, bronchopulmonary aspergillosis, mucoviscoidosis 2. They can also occur in patients with congenital heart disease particularly after surgical correction using the Fontan procedure where it can occur in up to 4% of patients 3. Plastic bronchitis can occur at any age, but most publications interest children population 4.
The formation of bronchial casts in plastic bronchitis is extremely variable; it goes from small fragmented bronchial casts to enormous casts filling the airways of an entire lung.
Plastic bronchitis has been classified based on histology into cellular and acellular 5. Alternatively, plastic bronchitis has been classified according to the associated disease state 6. The cast morphology of plastic bronchitis in patients with congenital heart disease post corrective surgery is typically acellular and presents as a recurrent disease 7.
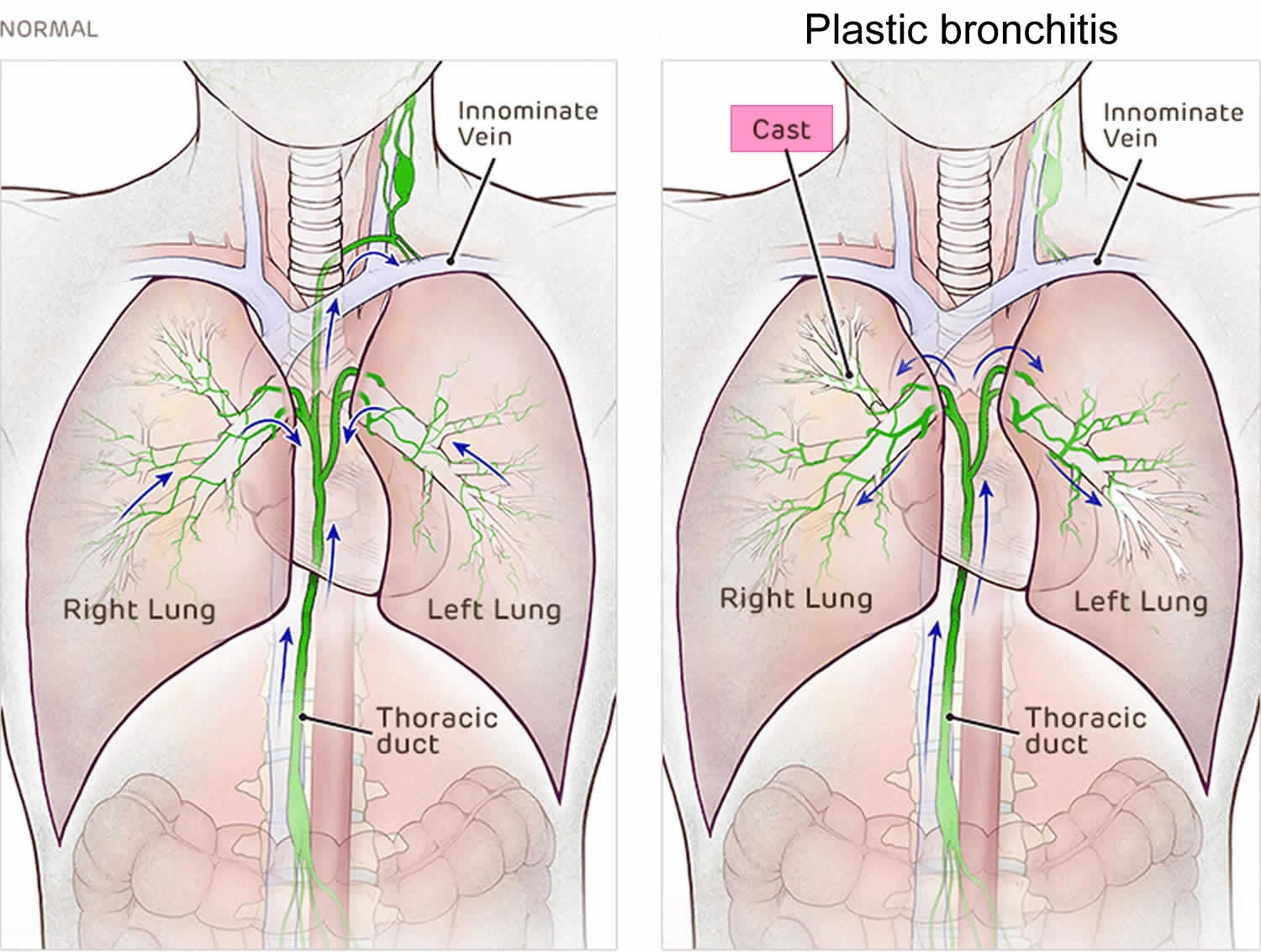
Lymphatic flow disorders refer to a group of diseases characterized by abnormal circulation of lymph fluid. Lymph vessels carry lymph fluid to veins, where it returns to the bloodstream, playing a crucial role in immune function and fat and protein transport.
Injury to the thoracic duct (the main lymph vessel), congenital abnormalities or excessively high venous pressures can result in lymphatic flow problems and leakage of lymphatic fluid into the chest, abdomen or other body cavities. In plastic bronchitis, the abnormal circulation causes lymph to leak into the airways.
The management of plastic bronchitis consists largely of mechanical evacuation of the casts acutely with bronchoscopy and preventing recurrence 8. A large case series of plastic bronchitis patients found that extraction via bronchoscopy is the only effective treatment 9. Prior to extraction, the treatment includes bronchodilators, corticosteroids, mucolytics, and macrolide antibiotics 10. One case report found that steroid treatment dissolved the secretions 11. In cases where clots cannot be mobilized, chest physiotherapy might be an option. Dissolving the clots can be achieved by either inhaled mucolytic or fibrinolytic agents such as tissue plasminogen activator (tPA) 12. Another study utilized thoracic duct stents to prevent abnormal or retrograde flow back to the pulmonary circulation 13. One group found that utilization of complete parenteral low-fat nutrition decreased the amount of cast formation 14.
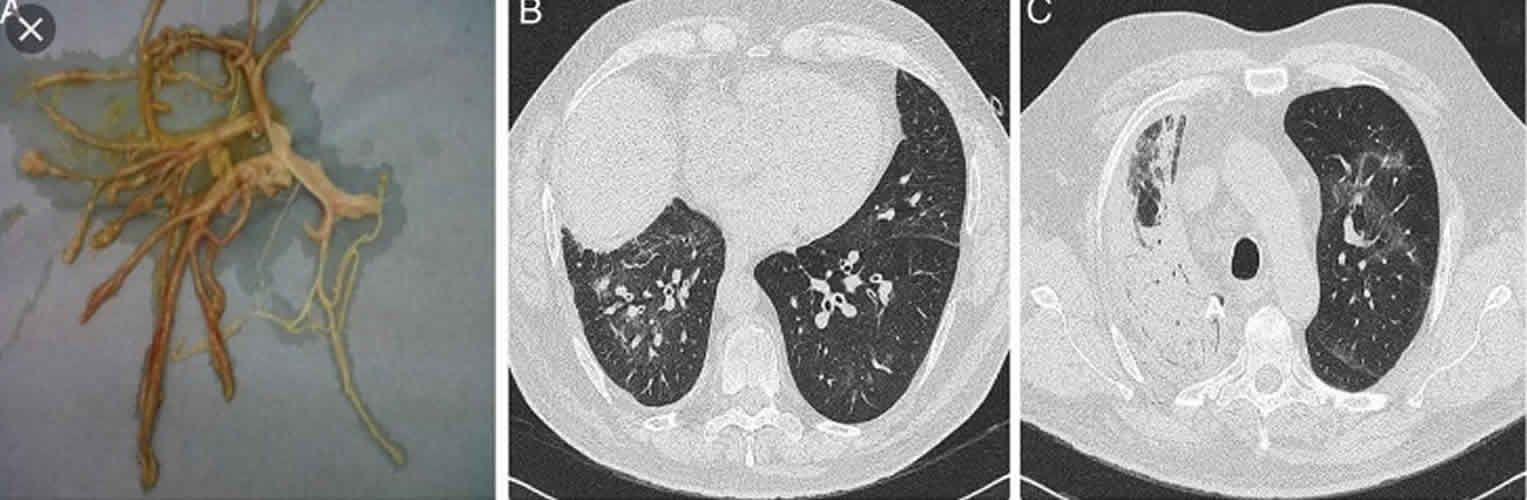
Figure 1. Plastic bronchitis
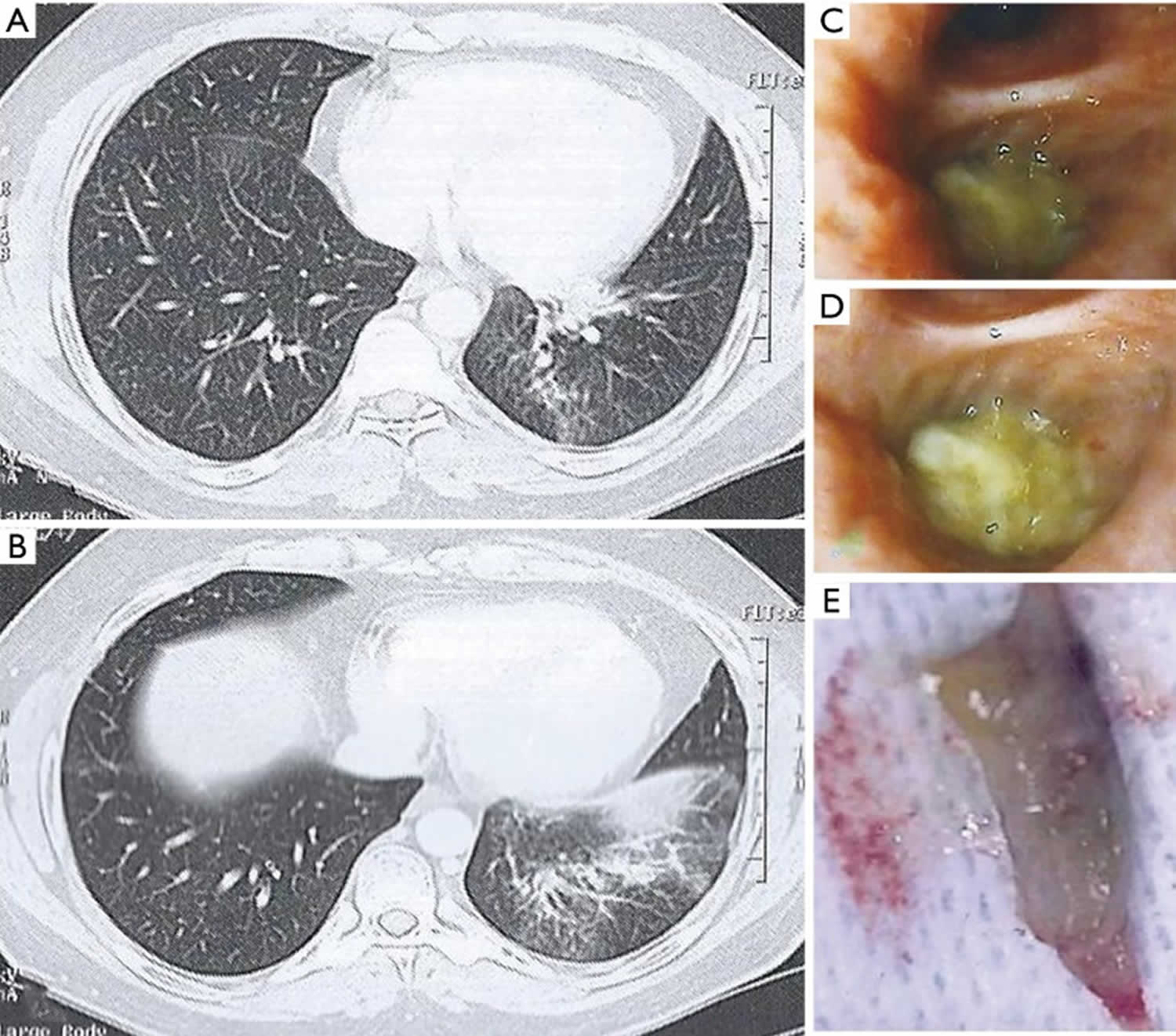
Figure 2. Plastic bronchitis casts
Footnote: Chest high-resolution computed tomography (HRCT) showing (A) left lower lobe bronchus obstruction and (B) partial atelectasis of the left lower lobe with ventilation defects; (C,D) left lower lobe bronchial obstruction by mucous plug; endoscopic view; (E) removed bronchial cast.
[Source 15 ]Figure 3. Macroscopic appearance of the bronchial cast
[Source 7 ]Plastic bronchitis causes
Plastic bronchitis is most prevalent in patients with certain forms of congenital heart disease who have had the Fontan surgery and those with lymphatic abnormalities. It can also be associated with certain lung diseases, infections, and (very rarely) allergies.
The exact pathophysiology of plastic bronchitis in congenital heart disease is unknown. Lymphatic dysfunction, endobronchial lymph leakage, and mucus hypersecretion due to elevated venous pressure have all been proposed as possible mechanisms 16.
Plastic bronchitis symptoms
The accumulation of material in the airways leads to airway obstruction and respiratory symptoms such as cough and oxygen deprivation (hypoxia). In many cases, the early symptoms are nonspecific and can resemble asthma.
Patients with plastic bronchitis have difficulty breathing and are prone to uncomfortable coughing fits, dyspnea, pleuritic chest pain, fever, and wheezing. During these fits, they may cough up the casts. The casts often return within days, as more lymph fluid leaks into the airways. In severe cases, plastic bronchitis can lead to asphyxia (suffocation).
Plastic bronchitis diagnosis
Historically, plastic bronchitis was diagnosed when patients coughed up cast material or cast material was found during bronchoscopy, a procedure used to look inside the airways and lungs. Other tests, such as chest X-ray (CXR), can show that the affected lung is not expanding normally, but this is not a diagnostic finding by itself.
There is no specific cytological, pathologic, or laboratory test that is diagnostic for casts due to lymphatic plastic bronchitis.
Plastic bronchitis is diagnosed using a special type of MRI lymphatic imaging called dynamic contrast magnetic resonance lymphangiography, which can visualize lymphatic abnormalities.
During a dynamic contrast magnetic resonance lymphangiography study, very small needles are placed through your groin into your lymph nodes using ultrasound guidance. Contrast material is injected in to the lymph nodes, allowing the interventional radiologist to see where the “leakage” of the lymph is occurring in your lungs.
Plastic bronchitis treatment
Plastic bronchitis is treated by a team of experts that specialize in lymphatic imaging and interventions. Treatment depends on the exact cause and the patient’s anatomy.
Because plastic bronchitis is an uncommon condition, most reports of effective therapy are based on subjective criteria detailed in case reports or small case series.
Cardiopulmonary stabilization with intubation and mechanical ventilation is the main stay of treatment in acute life threatening emergencies. Airways clearance with immediate rigid or flexile bronchoscopy is often required in plastic bronchitis 7.
High-frequency chest wall oscillation can also be used to vibrate the chest wall at a high frequency to try to loosen and thin the casts 17.
It has been reported that inhalation of tissue plasminogen activator (tPA) and heparin can improve patients with plastic bronchitis, but there are many adverse effects limiting their use 18.
In all patients, the first step involves careful mapping of the anatomy and flow of the lymphatic system called intranodal lymphangiography. This is done using a specialized MRI technique called dynamic contrast magnetic resonance lymphangiography. During this procedure, an MRI contrast agent is injected directly into the lymphatic system. After the MRI procedure a small catheter is placed into the main lymphatic channel, called the thoracic duct, to further outline the abnormal ducts that are surrounding the airway. To further confirm the leakage, a technique called “blue bronchoscopy” is performed. During “blue bronchoscopy”, special blue dye is injected into the thoracic duct while performing a bronchoscopy, which is a standard procedure where a bronchoscope is inserted through your nose or mouth into your airway in order to view your lungs.
After the abnormal ducts are identified, they are sealed using a procedure called selective lymphatic duct embolization. Your or your child’s doctor will use oil, coils, particles, glue or other bonding agents, inserted through a tiny tube (catheter), to seal the ducts. With lymphatic embolization procedure, the interventional radiologists are careful not to block the main thoracic duct if possible, an approach that experts believe is important for the success of this procedure. Because lymphangiography allows clinicians to pinpoint the exact spot of the leak, they can target their intervention to the affected area, preserving the thoracic duct.
The treatment of plastic bronchitis in patients with heart disease may also include cardiac interventional procedures such as balloon dilation, stent dilation of a narrow vessel, or embolization of an abnormal blood vessel with coils.
You or your child may also be prescribed medications that can reduce inflammation, lower venous pressures or dissolve the bronchial casts.
Plastic bronchitis prognosis
The prognosis of plastic bronchitis is generally favorable if the disease is properly treated at the beginning and if the search of associated diseases is negative. By contrast, plastic bronchitis secondary to cyanotic congenital heart disease is often associated with a rather grim prognosis with respiratory failure secondary to central airway obstruction as a common mechanism of death 19.
- Eberlein, Michael H., Drummond Michael B., Haponik Edward F. Plastic bronchitis: a management challenge. Am. J. Med. Sci. 2008;335(2):163–169.[↩]
- Sulavik S.B. Bronchocentric granulomatosis and allergic bronchopulmonary aspergillosis. Clin. Chest Med. 1988;9:609–621.[↩]
- Grutter G., Di Carlo D., Gandolfo F., Adorisio R., Alfieri S., Michielon G. Plastic bronchitis after extracardiac Fontan operation. Ann. Thorac. Surg. 2012;94:860–864.[↩]
- Kim E. J., Park J. E., Kim D. H., Lee J. Plastic Bronchitis in an Adult with Asthma. Tuberculosis and Respiratory Diseases. 2012;73(2):122–126. doi: 10.4046/trd.2012.73.2.122[↩]
- Seear M., Hui H., Magee F. Bronchial casts in children: a proposed classification based on nine cases and a review of the literature. Am. J. Respir. Crit. Care Med. 1997;1:364–370.[↩]
- Brogan T.V., Finn L.S., Pyskaty D.J. Plastic bronchitis in children: a case series and review of the medical literature. Pediatr. Pulmonol. 2002;34:482–487.[↩]
- Patil MH, Siddiqi A, Jeffrey Mador M. Successful bronchoscopy in a pregnant patient with plastic bronchitis. Respir Med Case Rep. 2016;18:8-9. Published 2016 Mar 11. doi:10.1016/j.rmcr.2016.03.003 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4802819[↩][↩][↩]
- Uchel T, Labana S, Tancer S, et al. Unusual Case of Plastic Bronchitis Presenting with Pneumopericardium. Am J Case Rep. 2018;19:1434-1436. Published 2018 Dec 3. doi:10.12659/AJCR.911311 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6287447[↩]
- Singhi AK, Vinoth B, Kuruvilla S, Sivakumar K. Plastic bronchitis. Ann Pediatr Cardiol. 2015;8(3):246–48.[↩]
- Kim EJ, Park JE, Kim DH, Lee J. Plastic bronchitis in an adult with asthma. Tuberc Respir Dis. 2012;73(2):122–26.[↩]
- Turgut T, In E, Ozercan IH, Kaplan M. A case of plastic bronchitis. Arch Iran Med. 2014;17(8):589–90.[↩]
- Manna SS, Tibby SM, Durward A. Treatment of plastic bronchitis in acute chest syndrome of sickle cell disease with intratracheal rhDNase. Arch Dis Child. 2003;88(7):626–27[↩]
- Dori Y, Keller MS, Rome JJ, et al. Percutaneous lymphatic embolization of abnormal pulmonary lymphatic flow as treatment of plastic bronchitis in patients with congenital heart disease. Circulation. 2016;133(12):1160–70.[↩]
- Demont P, Fehr T, Geiser T, Ott SR. Bronchial cast formation in plastic bronchitis. Respiration. 2016;91:325–26.[↩]
- Coen M, Daniel L, Serratrice J. An adult case of plastic bronchitis: a rare and multifactorial disease. J Thorac Dis. 2018;10(1):E16-E19. doi:10.21037/jtd.2017.12.02 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5863104[↩]
- Languepin J., Scheinmann P., Mahut B. Bronchial casts in children with cardiopathies: the role of pulmonary lymphatic abnormalities. Pediatr. Pulmonol. 1999;28:329–336.[↩]
- Koga T., Kawazu T., Iwashita K., Yahata R. Pulmonary hyperinflation and respiratory distress following solvent aspiration in a patient with asthma: expectoration of bronchial casts and clinical improvement with high-frequency chest wall oscillation. Respiratory care. 2004;49(11):1335–1338.[↩]
- Eason D. E., Cox K., Moskowitz W. B. Aerosolised heparin in the treatment of Fontan-related plastic bronchitis. Cardiology in the Young. 2014;24(1):140–142. doi: 10.1017/S1047951112002089[↩]
- Raoufi M, Achachi L, Mrabet FZ, et al. A Rare Case of Idiopathic Plastic Bronchitis. Case Rep Pulmonol. 2017;2017:4789751. doi:10.1155/2017/4789751 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5643106[↩]