Pronator teres syndrome
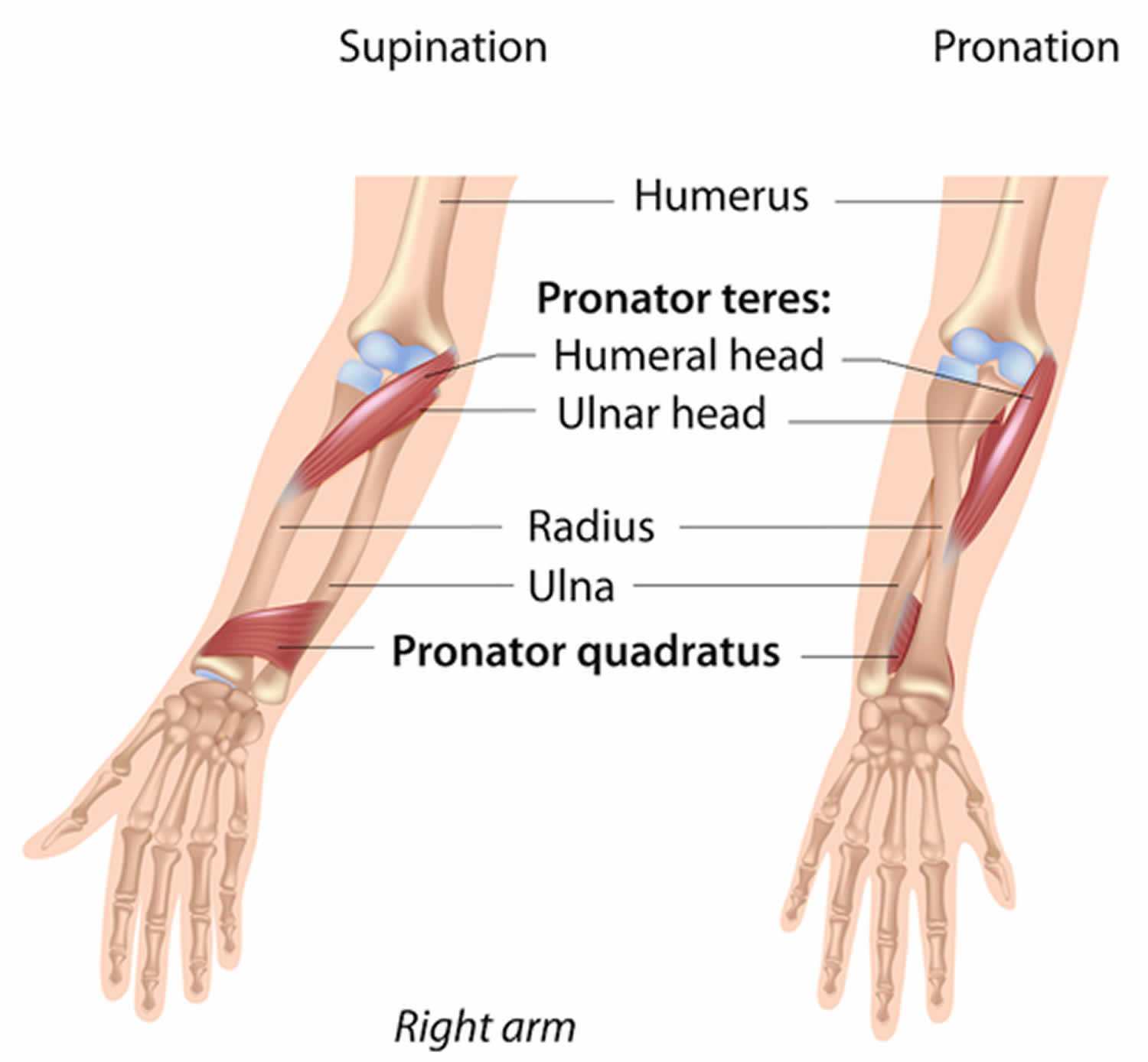
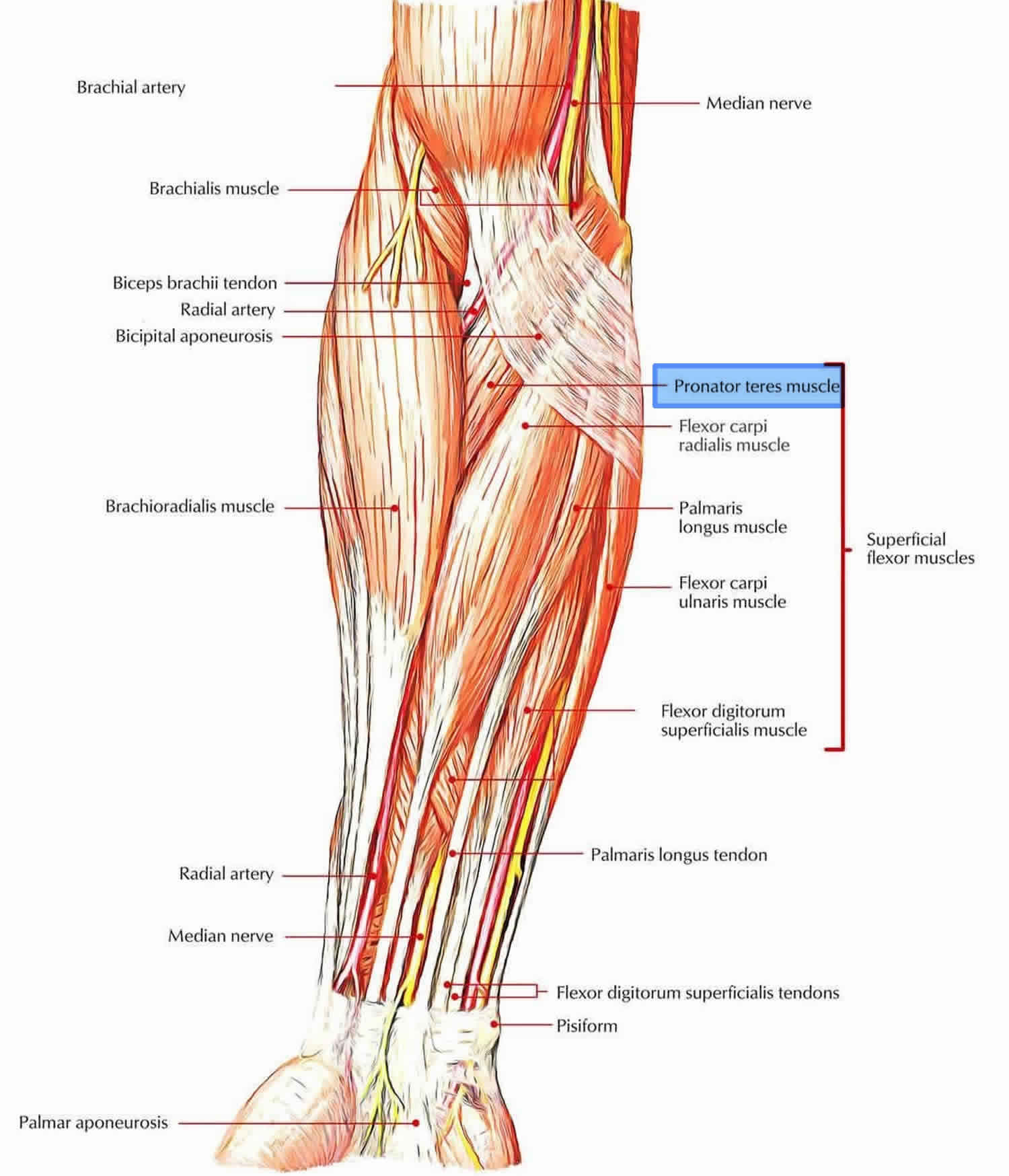
Pronator teres syndrome is caused by a compression of the median nerve by the pronator teres muscle in the forearm 1. The pronator teres muscle is named because of its action and shape; it is a rounded muscle that pronates. In the majority of cases (66%), pronator teres muscle arises from unequal two heads: the larger humeral head from the upper part of the medial epicondyle and the smaller ulnar head from the coronoid process of the ulna 2. They pass down to the forearm, form a common flexor tendon, and insert into the radial shaft. Before the two heads unite, the median nerve passes between them in 74% to 82% of the cases, innervating both heads from C6-7 roots 2. The absence of the ulnar head is rare (14%) and may reduce the risk of median nerve entrapment 2. Many individuals have additional fibrous brands within the two heads of the pronator teres muscle 2. The anterior interosseous nerve then branches from the median nerve about 5 to 8 cm distal to the medial epicondyle.
Pronator teres syndrome is a rare condition that may be easily overlooked and mistaken for a more much frequent carpal tunnel syndrome 3. No age group preference has been described, but one study reports a higher prevalence of pronator teres syndrome in men 4.
Figure 1. Pronator teres muscle
Pronator teres syndrome cause
The cause of pronator teres syndrome may vary and it may affect various people ranging from a patient with multiple comorbidities (e.g., hemodialysis) to healthy individuals who are involved in sports or other physical activities requiring repetitive pronation movements of the forearm as well as people with specific anatomic variations of the elbow region. Quick and repetitive grasping or pronation movements (prolonged hammering, ladling food, cleaning dishes, tennis) may cause pronator teres muscle hypertrophy and entrapment of median nerve, especially in those individuals who have additional fibrous brands 5. Pronator teres syndrome has been described after local trauma, compression with Schwanomma, and in patients undergoing anticoagulation therapy and renal dialysis 6. Tight lacertus fibrosis may exacerbate the symptoms of pronator teres syndrome 7.
Pronator teres syndrome symptoms
Pronator teres syndrome may manifest with pain in the volar forearm region, aggravated by resisted pronation of the forearm and flexion of the elbow 5, and a positive Tinel sign over the proximal edge of pronator teres. The patient may report significant weakness. Wasting of the median innervated muscle is rare in pronator teres syndrome, but a mild weakness of flexor pollicis longus and abductor pollicis brevis is not uncommon, with some involvement of flexor digitorum profundus to digits 2 and 3 and opponens pollicis. The pronator teres itself is usually spared because it received innervation before the median nerve pierces it. Sensory loss is variable, involving the palm of the hand or mimic that of carpal tunnel syndrome including the thenar eminence, thumb, index, middle and ring fingers. Positive Phalen test over the pronator teres muscle can be present in 50% of cases 5
Pronator teres syndrome patients may present with 8:
- volar pain of the proximal lower arm
- paresthesia of the volar forearm and the radial three digits and radial aspect of the fourth digit
- weakness, on the other hand, is variable, often with unspecified grip clumsiness
- the proximal volar forearm is painful to palpation, and Tinel’s sign can be elicited on palpation of the pronator teres muscle
- simian hand deformity: unable to move the thumb away from the rest of the hand
- benediction sign: when trying to form a fist, due to weakness in flexion of radial sided digits
Symptoms provoked by examination maneuvers, such as during resisted forearm pronation (suggesting median nerve compression by pronator teres muscle), or resisted elbow flexion and forearm supination (indicating median nerve compression by biceps aponeurosis / lacertus fibrosus) can help pinpoint the site of compression 8.
Clinical presentation can harbor some pitfalls. Sensory and pain symptoms of pronator teres syndrome and carpal tunnel syndrome can overlap: distinguish the two by looking for numbness of the forearm, which does not occur in carpal tunnel syndrome, and asking about nocturnal exacerbation, which would atypical in pronator teres syndrome. Provocation tests as detailed above can help further.
Pronator teres syndrome diagnosis
It is important that nerve conduction studies are done in pronator teres syndrome to rule out other neuropathies, but they seldom show abnormalities 1. Sensory and motor amplitudes are reduced more than conduction velocities, mostly in patients with severe and axonal symptoms 4. Electromyography (EMG) abnormalities occur in flexor pollicis longus and flexor digitorum profundus to digits 2 and 3, less often in the flexor digitorum superficialis and abductor pollicis brevis, and only rarely in pronator teres because compression at the site most often occurs distal to its innervation. If any of the median muscles are abnormal, other muscles innervated by the same myotomes as the proximal median muscles but supplied by a different nerve should be tested to exclude more proximal lesion within the brachial plexus or cervical roots. Some authors report abnormal electrodiagnostic findings in 10% of pronator teres syndrome only 6.
Pronator teres syndrome among other entrapments within the upper limb also can be diagnosed by ultrasound and magnetic resonance imaging, but ultrasound is advantageous due to its dynamic character and lower cost 2. Several studies with an ultrasound evaluation of median nerve between the humeral and ulnar heads of pronator teres concluded that cross-sectional area of MN positively correlates with severity, duration of symptoms and nerve conduction failure 9.
Pronator teres syndrome test
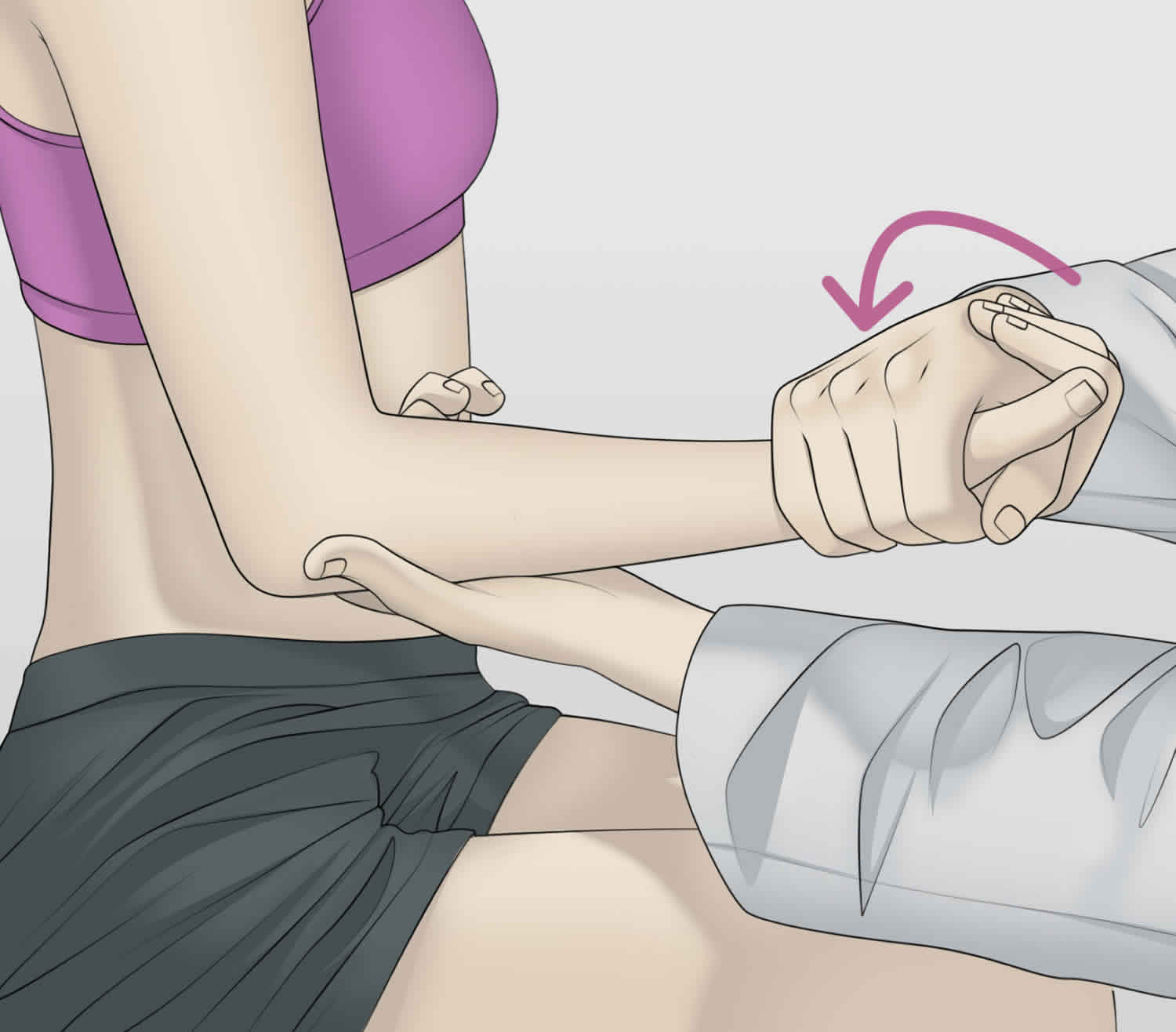
Pronator teres syndrome test is an elbow examination used to test for median nerve compression at the pronator teres muscle.
Procedure:
- Patient seated with elbow fixed in 90 degrees of flexion. The clinician then places one hand on the client’s elbow for stabilization and the other hand grasps the patient’s hand in a handshake position. The client holds this position as the practitioner attempts to supinate the patient’s forearm (forcing the client to contract the pronator muscles). While holding the resistance against pronation, the clinician extends the patient’s elbow. If the patient’s pain or discomfort is reproduced, there is a good chance of median nerve compression by the pronator teres. The patient should keep the elbow relaxed during the test, because holding the elbow firmly in flexion will not allow elbow extension.
Figure 2. Pronator teres syndrome test
Pronator teres syndrome differential diagnosis
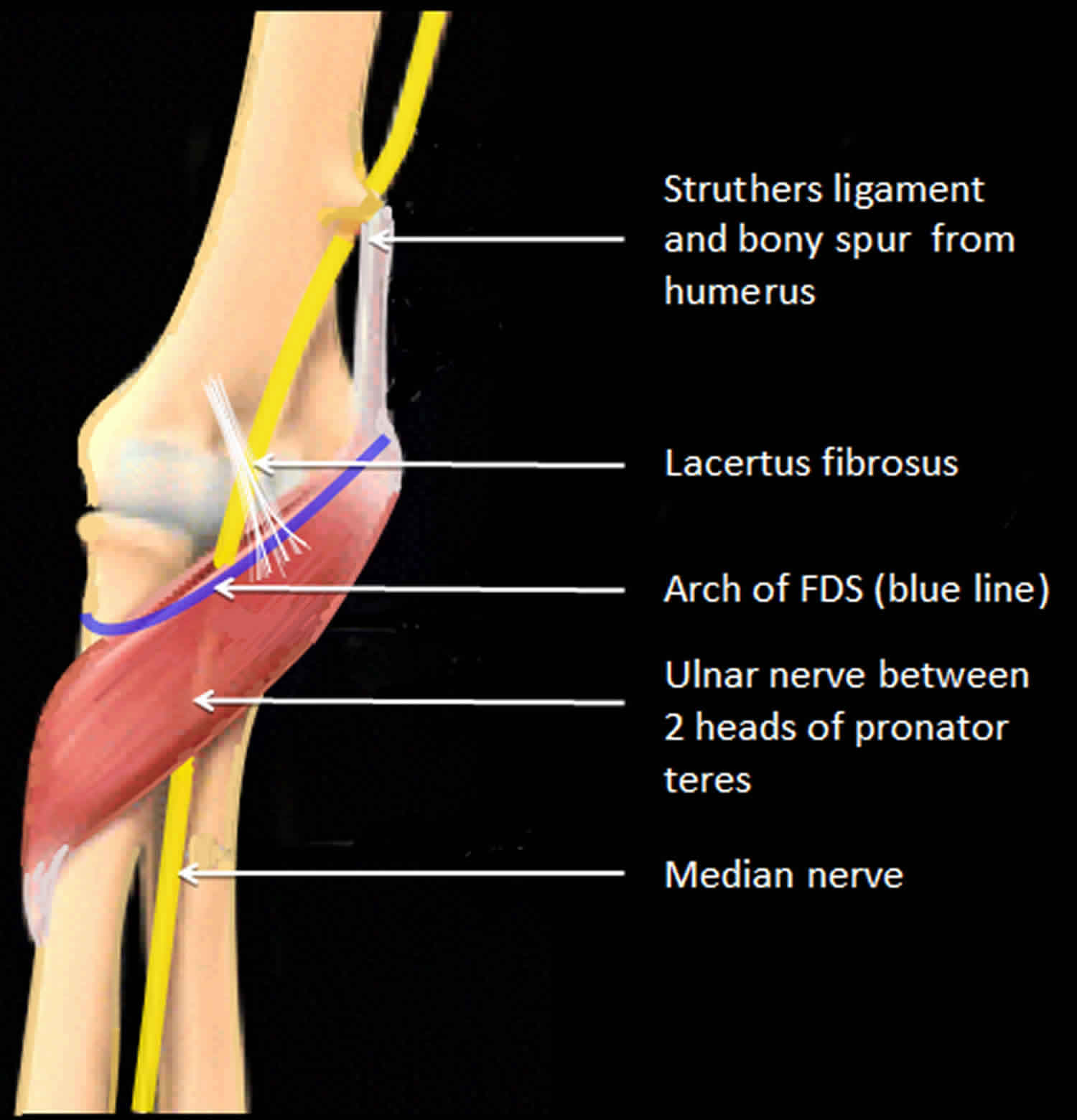
Due to similar clinical presentation, some authors combine pronator teres syndrome with the following proximal median nerve entrapment syndromes 6:
- Ligament of Struthers entrapment – median nerve compression by a ligament running from medial epicondyle to a bony spur on a distal medial humerus, which is present only in 1-2 % of the population. The pain in a forearm and paresthesias in the median-innervated digits is exacerbated by supination of the forearm and extension of the elbow (versus pronation in pronator teres syndrome). The radial pulse may also be decreased as the brachial artery runs next to the median nerve.
- Median nerve entrapment by hypertrophied bicipital aponeurosis (lacertus fibrosis) – This is fascia attaching the biceps to the ulna and overlies the median nerve in the proximal forearm. The pain in a forearm and paresthesias in the median-innervated digits is exacerbated by resisted flexion of the elbow with the forearm in supination.
- Median nerve compression by the sublimus bridge of the flexor digitorum superficialis muscle – The pain in a forearm and paresthesias in the median-innervated digits is exacerbated by resisted flexion of the proximal interphalangeal joint of the middle finger while other fingers are held in extension.
Pronator teres syndrome should also be distinguished from carpal tunnel syndrome, median nerve entrapment at the wrist, which is the most common median nerve entrapment syndrome, as well as from anterior interosseous nerve syndrome, brachial plexus injury, or cervical radiculopathy.
Pronator teres syndrome has sensory loss in the entire median nerve distribution versus carpal tunnel syndrome where sensation is spared over the thenar eminence because palmar cutaneous branch leaves the median nerve proximal to carpal tunnel but distal to pronator teres muscle. In addition, pronation is spared in carpal tunnel syndrome, and nocturnal paresthesia symptoms are usually absent in pronator teres syndrome 10. Nerve conduction study and amplitude of the median nerve may decrease in the forearm, but the distal motor and sensory latencies are normal in pronator teres syndrome except when there is associated carpal tunnel syndrome 4.
Because of overlapping symptoms, carpal tunnel syndrome is sometimes diagnosed, and more proximal pronator teres syndrome is missed when both are present in the same limb 11. Thus in patients with carpal tunnel syndrome pronator teres syndrome should be ruled out especially when the patient is a candidate for surgery 4.
To distinguish anterior interosseous nerve from pronator teres syndrome, the pronation should be demonstrated with elbow flexed (pronator quadratus function) to avoid contribution of the pronator teres, which is the primary muscle to pronate with the arm extension 12. Also, there is no sensory loss in anterior interosseous nerve syndrome (as it carries only deep sensory fibers to the wrist), and in some cases, pronator teres syndrome may have only mild paresthesias in median nerve distribution. In both cases, flexor pollicis longus and flexor digitorum profundus to digits 2 and 3 may be affected; but in anterior interosseous nerve, the pronator quadratus does not weaken the pronator teres as anterior interosseous nerve leaves median nerve distal to pronator teres muscle. Clinically, in both cases, the patient presents with inability to flex the distal phalanx of the thumb, index, and middle fingers and the weakness of pronation.
In the case of brachial plexus injury or cervical radiculopathy, the examination may reveal weakness in other muscles outside the median nerve territory. Neck pain that radiates to the arm is a common complaint, suggesting cervical radiculopathy.
One group of authors describe a neuralgic amyotrophy as a potential competing condition with pronator teres syndrome due to similar symptoms; but it usually involves multiple nerves, and pain is more commonly localized in the shoulder rather than in the forearm. Neuralgic amyotrophy is an idiopathic condition that usually improves spontaneously in 6 to 12 months 13.
Pronator teres syndrome treatment
Conservative treatment may be effective in 50–70% of cases, includes rest, modification of activities that exacerbate the symptoms, physical and occupational therapy, nonsteroidal anti-inflammatory medications, and local injections with corticosteroids or local anesthetic 2. Patients usually may continue to work unless they present with prominent motor or sensory deficits that limit work activities. Conservative treatment should be conducted for at least 6 weeks. If conservative treatment fails, surgery is considered.
Surgical treatment is indicated if a patient is symptomatic, has one or more objective findings in a physical examination of weakness or motor atrophy, and has abnormal electrodiagnostic studies 13. Surgery usually includes exploration of median nerve in the forearm and release of pronator teres muscle as well as all other compressive structures – ligament of Struthers, lacertus fibrosis, and/or fascia of flexor digitorum superficialis. Although median nerve is sometimes decompressed at multiple sites, this is considered a single procedure 13.
An endoscopic release has advantages over open surgery because it does not compromise the nerve’s blood supply, reduces scar formation, and has been reported to have excellent results 14. In the case of recurrent symptoms, open surgery has been indicated 14.
Pronator teres syndrome prognosis
Pronator teres syndrome only requiring pronator teres muscle release has a good recovery in most of the cases, and patients return to light duty in approximately 3 weeks and regular duty in 6 weeks 13. Occupational therapy fastens recovery and is particularly important for patients who underwent tendon transfers or have a residual weakness. In these cases, patients may return to light duty work in approximately 6 to 8 weeks and regular duty in 10 to 12 weeks 13.
- Lacey SH, Soldatis JJ. Bilateral pronator syndrome associated with anomalous heads of the pronator teres muscle: a case report. J Hand Surg Am. 1993 Mar;18(2):349-51.[↩][↩]
- Olewnik Ł, Podgórski M, Polguj M, Wysiadecki G, Topol M. Anatomical variations of the pronator teres muscle in a Central European population and its clinical significance. Anat Sci Int. 2018 Mar;93(2):299-306.[↩][↩][↩][↩][↩][↩]
- Bair MR, Gross MT, Cooke JR, Hill CH. Differential Diagnosis and Intervention of Proximal Median Nerve Entrapment: A Resident’s Case Problem. J Orthop Sports Phys Ther. 2016 Sep;46(9):800-8.[↩]
- Asheghan M, Hollisaz MT, Aghdam AS, Khatibiaghda A. The Prevalence of Pronator Teres among Patients with Carpal Tunnel Syndrome: Cross-sectional Study. Int J Biomed Sci. 2016 Sep;12(3):89-94.[↩][↩][↩][↩]
- Hartz CR, Linscheid RL, Gramse RR, Daube JR. The pronator teres syndrome: compressive neuropathy of the median nerve. J Bone Joint Surg Am. 1981 Jul;63(6):885-90.[↩][↩][↩]
- Afshar A. Pronator Syndrome Due to Schwannoma. J Hand Microsurg. 2015 Jun;7(1):119-22.[↩][↩][↩]
- Dididze M, Sherman Al. Pronator Teres Syndrome. [Updated 2019 Jan 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526090[↩]
- Miller TT, Reinus WR. Nerve entrapment syndromes of the elbow, forearm, and wrist. AJR Am J Roentgenol. 2010 Sep;195(3):585-94. doi: 10.2214/AJR.10.4817 https://www.ajronline.org/doi/full/10.2214/AJR.10.4817[↩][↩]
- Kowalska B, Sudoł-Szopińska I. Ultrasound assessment on selected peripheral nerve pathologies. Part I: Entrapment neuropathies of the upper limb – excluding carpal tunnel syndrome. J Ultrason. 2012 Sep;12(50):307-18.[↩]
- Nebot-Cegarra J, Perez-Berruezo J, Reina de la Torre F. Variations of the pronator teres muscle: predispositional role to median nerve entrapment. 1991-1992Arch Anat Histol Embryol. 74:35-45.[↩]
- Bilecenoglu B, Uz A, Karalezli N. Possible anatomic structures causing entrapment neuropathies of the median nerve: an anatomic study. Acta Orthop Belg. 2005 Apr;71(2):169-76.[↩]
- Ulrich D, Piatkowski A, Pallua N. Anterior interosseous nerve syndrome: retrospective analysis of 14 patients. Arch Orthop Trauma Surg. 2011 Nov;131(11):1561-5.[↩]
- Carter GT, Weiss MD. Diagnosis and Treatment of Work-Related Proximal Median and Radial Nerve Entrapment. Phys Med Rehabil Clin N Am. 2015 Aug;26(3):539-49.[↩][↩][↩][↩][↩]
- Hsiao CW, Shih JT, Hung ST. Concurrent carpal tunnel syndrome and pronator syndrome: A retrospective study of 21 cases. Orthop Traumatol Surg Res. 2017 Feb;103(1):101-103.[↩][↩]