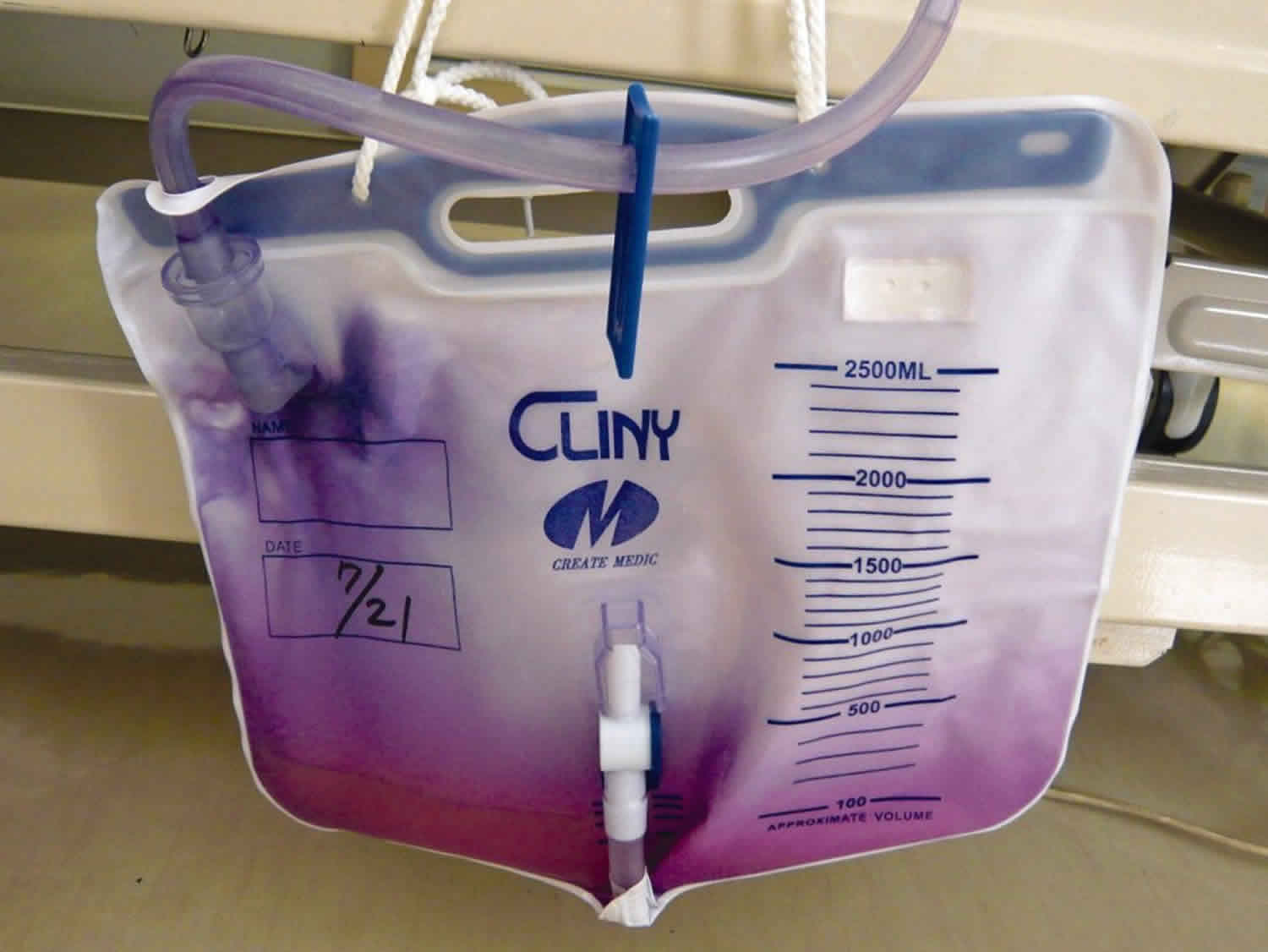
Purple urine bag syndrome
Purple urine bag syndrome is an uncommon but particularly striking phenomenon observed in people with urinary catheters and co-existent urinary tract infections (UTIs) 1. A chemical reaction between plastic and certain bacterial enzymes results in an intense purple urine color 1. Purple urine bag syndrome occurs predominantly in constipated women, chronically catheterized and associated with bacterial urinary infections that produce sulphatase/phosphatase 2. Discoloration of the urine bag is due to the presence of indigo (blue) and indirubin (red) pigments or to their mixture that becomes purple 2. The change in color is purely within the bag itself; interestingly, the urine itself remains unchanged in color 3. Purple urine bag syndrome is an uncommon occurrence, but prevalence of purple urine bag syndrome has been reported to be as high as 9.8% in institutionalized patients with long-term indwelling urinary catheter use 4.
Though commonly benign, there have been case reports in the literature of purple urine bag syndrome progressing to Fournier’s gangrene and doubts on associations of increased urine alkalinity and PVC containing urinary bags 5. Further definitive studies are required to elucidate clear-cut pathogenesis, morbidity, and mortality implications and to delineate standard guidelines to treat this unique phenomenon.
Purple urine bag syndrome causes
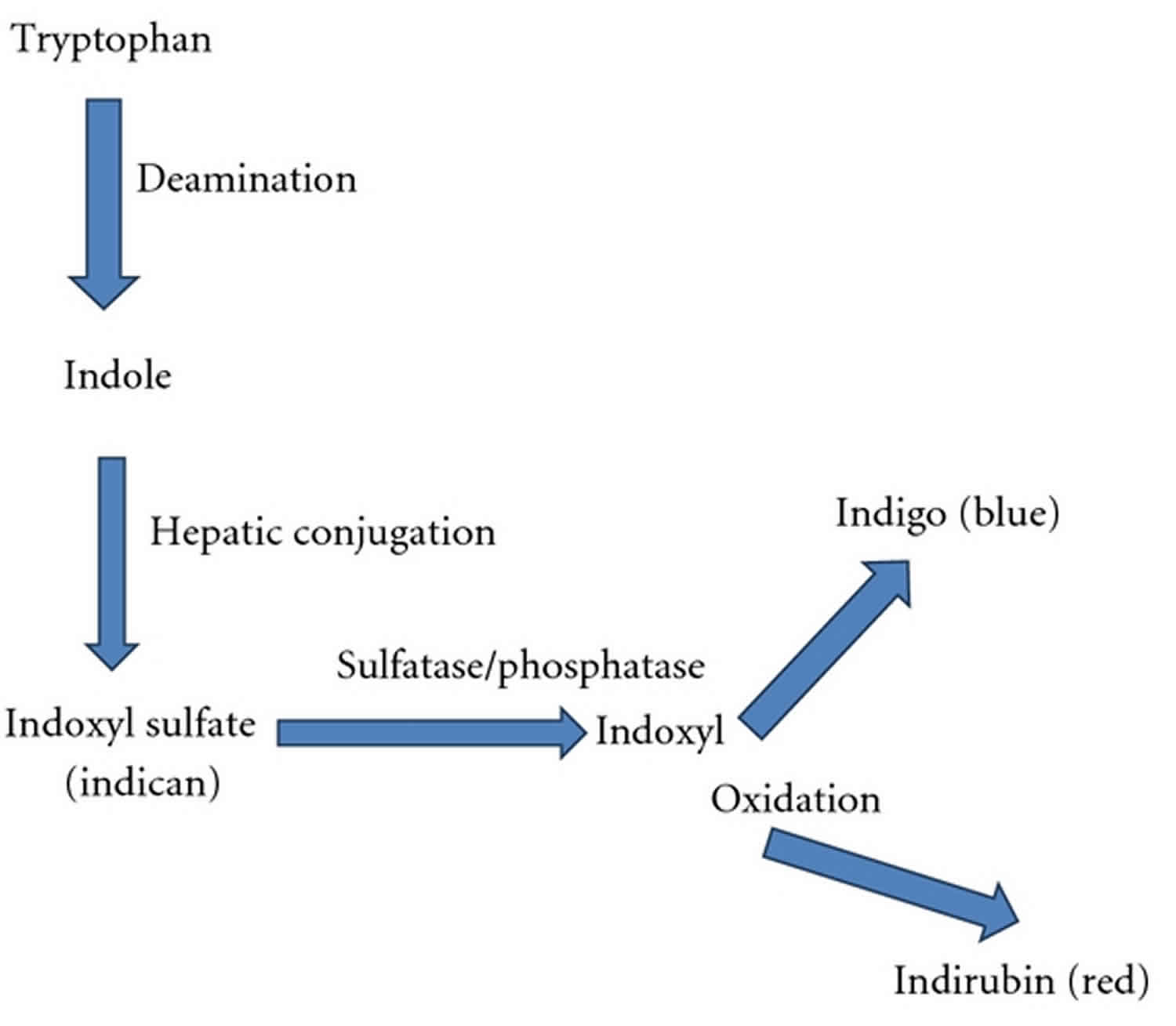
Purple urine bag syndrome is a rare manifestation of urinary tract infection 5. The major risk factors implicated in the cause of purple urine bag syndrome are outlined in Table 1 below. Purple urine bag syndrome have been shown to be associated with the female gender, alkaline urine, constipation, institutionalization and the use of plastic urinary catheter and bag 4. Higher bacterial load in urine, in combination with the above factors, facilitates the development of purple urine bag syndrome. Most authors believe that purple urine is a mixture of indigo (blue) and indirubin (red) which are derived from the metabolites of tryptophan 2. Tryptophan is metabolized in the gastrointestinal tract by gut bacteria and it produces indole that is absorbed into portal circulation. Indole is converted into indoxyl sulphate in the liver. Most indoxyl sulphate is excreted into the urine and digested into indoxyl by indoxyl sulphatase produced by some bacteria. Indoxyl turns into indigo (blue color) and indirubin (red color) in alkaline urine, and these colors then mix to form a purple color (see Figure 1 below) 6. However, there were some patients who presented with a purple urine bag without indicanuria and the violet pigment may be either a steroidal or bile acid conjugate 7. Chronic constipation is commonly associated with bacterial overgrowth in the colon which increases the conversion of tryptophan into indole 2. Catheter associated urinary tract infection increases the conversion of indoxyl sulphate into indoxyl. So, purple urine bag syndrome is most often observed in chronically catheterized and constipated people 8. Several bacterial species have been reported in association with purple urine bag syndrome including Providencia stuartii, Providencia rettgeri, Klebsiella pneumoniae, Proteus mirabilis, Escherichia coli, Enterococcus species, Morganella morganii, citrobacter species, Group B Streptococci and Pseudomonas aeruginosa 9.
It is interesting to note that despite the common occurrence of urinary tract infections in patients with risk factors for purple urine bag syndrome, this interesting syndrome is rarely encountered. There are a few possible reasons. purple urine bag syndrome probably require the simultaneous presence of various factors: The presence of urinary tract infection caused by sulphatase-and phosphatase-producing bacteria, the presence of high tryptophan in the diet for the formations of the essential pigments, and being catheterized. It has been shown that not all bacteria organisms of the same species produce the phosphatase and sulphatase enzymes required for the formation of the responsible pigments 10. Furthermore, a certain concentration of the pigments may be required for the precipitations to become visible. The presence of alkaline urine, and also the type of materials used to manufacture the urinary catheter and bag may be important factors 10. Interestingly, purple urine bag syndrome in the presence of acidic urine has also been reported 9.
Table 1. Risk factors and associated mechanisms in purple urine bag syndrome
| Risk factors for purple urine bag syndrome | Associated mechanisms |
|---|---|
| Female gender | Predisposing anatomy to urinary tract infection (UTI) occurrence |
| Increased tryptophan dietary content | Increased available substrate for conversion |
| Increased urine alkalinity 11 | Facilitates indoxyl oxidation |
| Severe constipation 12 | Increased time for bacterial deamination |
| Chronic indwelling urinary catheterization | Increased risk of urinary tract infections (UTIs) |
| High urinary bacterial load 12 | Bacterial sulfatase/phosphatase availability |
| Renal failure | Impaired clearance of indoxyl sulfate |
Figure 1. Biochemical pathway of conversion of tryptophan to indigo and indirubin.
[Source 5 ]Purple urine bag syndrome symptoms
Purple urine bag syndrome is generally a benign process. Despite this fact, it is distressing for family, friends, and healthcare workers who are unaware of this phenomenon and tend to become unusually alarmed because of the sudden inexplicable discoloration of the urine and sometimes the urine bag. Nevertheless, physicians should be aware of the fact that this syndrome signals underlying recurrent urinary tract infections (UTIs), due to improper care of the urinary catheters and improper sanitation. Although relatively benign and easily treatable, it can be associated with significant morbidity and mortality 5.
Purple urine bag syndrome treatment
Treatment is directed at the underlying urinary tract infection as well as control of constipation and good urologic sanitation. Good care of the urinary catheters will prevent urinary tract infections (UTIs) and hence this phenomenon as well. Though described as relatively benign, review of the literature reveals couple of cases of purple urine bag syndrome which progressed to Fournier’s gangrene requiring aggressive debridement 13. The typical organisms which lead to purple urine bag syndrome were isolated from the scrotal wound cultures. However, treatment of patients with purple urine bag syndrome aggressively with antibiotics is a point of debate and needs to be further investigated.
Purple urine bag syndrome prognosis
Purple urine bag syndrome is generally a benign process. Despite this fact, it is distressing for family, friends, and healthcare workers who are unaware of this phenomenon and tend to become unusually alarmed because of the sudden inexplicable discoloration of the urine and sometimes the urine bag. Nevertheless, physicians should be aware of the fact that this syndrome signals underlying recurrent urinary tract infections (UTIs), due to improper care of the urinary catheters and improper sanitation. purple urine bag syndrome is also associated generally with higher incidence of morbidity and mortality than urinary tract infections alone without this occurrence 14.
- Chassin-Trubert C AM. Síndrome de la bolsa de orina púrpura: un fenómeno inusual y muy llamativo [Purple urine bag syndrome: report of one case]. Rev Med Chil. 2014;142(11):1482–1484. doi:10.4067/S0034-98872014001100018[↩][↩]
- Al Montasir A, Al Mustaque A. Purple urine bag syndrome. J Family Med Prim Care. 2013;2(1):104–105. doi:10.4103/2249-4863.109970 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3894016[↩][↩][↩][↩]
- Peters P, Merlo J, Beech N, et al. The purple urine bag syndrome: a visually striking side effect of a highly alkaline urinary tract infection. Can Urol Assoc J. 2011;5(4):233–234. doi:10.5489/cuaj.10177 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3147034[↩]
- Lin CH, Huang HT, Chien CC, Tzeng DS, Lung FW. Purple urine bag syndrome in nursing homes: Ten elderly case reports and a literature review. Clin Interv Aging. 2008;3:729–34.[↩][↩]
- Khan F, Chaudhry MA, Qureshi N, Cowley B. Purple urine bag syndrome: an alarming hue? A brief review of the literature. Int J Nephrol. 2011;2011:419213. doi:10.4061/2011/419213 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3184437[↩][↩][↩][↩]
- Su FH, Chung SY, Chen MH, Sheng ML, Chen CH, Chen YJ, et al. Case analysis of purple urine-bag syndrome at a long-term care service in a community hospital. Chang Gung Med J. 2005;28:636–42.[↩]
- Lin HH, Li SJ, Su KB, Wu LS. Purple urine bag syndrome: A Case Report and Review of the Literature. J Intern Med Taiwan. 2002;13:209–12.[↩]
- Dealler SF, Hawkey PM, Millar MR. Enzymatic degradation of urinary indoxyl sulfate by Providencia stuartii and Klebsiella pneumoniae causes the purple urine bag syndrome. J Clin Microbiol. 1988;26:2152–6.[↩]
- Ollapallil J, Irukulla S, Gunawardena I. Purple urine bag syndrome. ANZ J Surg. 2002;72:309–10.[↩][↩]
- Jones RA, Deacon HJ, Allen SC. Two cases and a short discussion of purple urine bag syndrome. CME Geriatr Med. 2003;5:84–7.[↩][↩]
- Umeki S. Purple urine bag syndrome (PUBS) associated with strong alkaline urine. Kansenshogaku Zasshi. 1993;67(12):1172–1177.[↩]
- Shiao CC, Weng CY, Chuang JC, Huang MS, Chen ZY. Purple urine bag syndrome: a community-based study and literature review. Nephrology. 2008;13(7):554–559.[↩][↩]
- Tasi YM, Huang MS, Yang CJ, Yeh SM, Liu CC. Purple urine bag syndrome, not always a benign process. The American Journal of Emergency Medicine. 2009;27(7):895–897.[↩]
- Pillai BP, Chong VH, Yong AML. Purple urine bag syndrome. Singapore Medical Journal. 2009;50(5):e193–e194.[↩]