Radial nerve
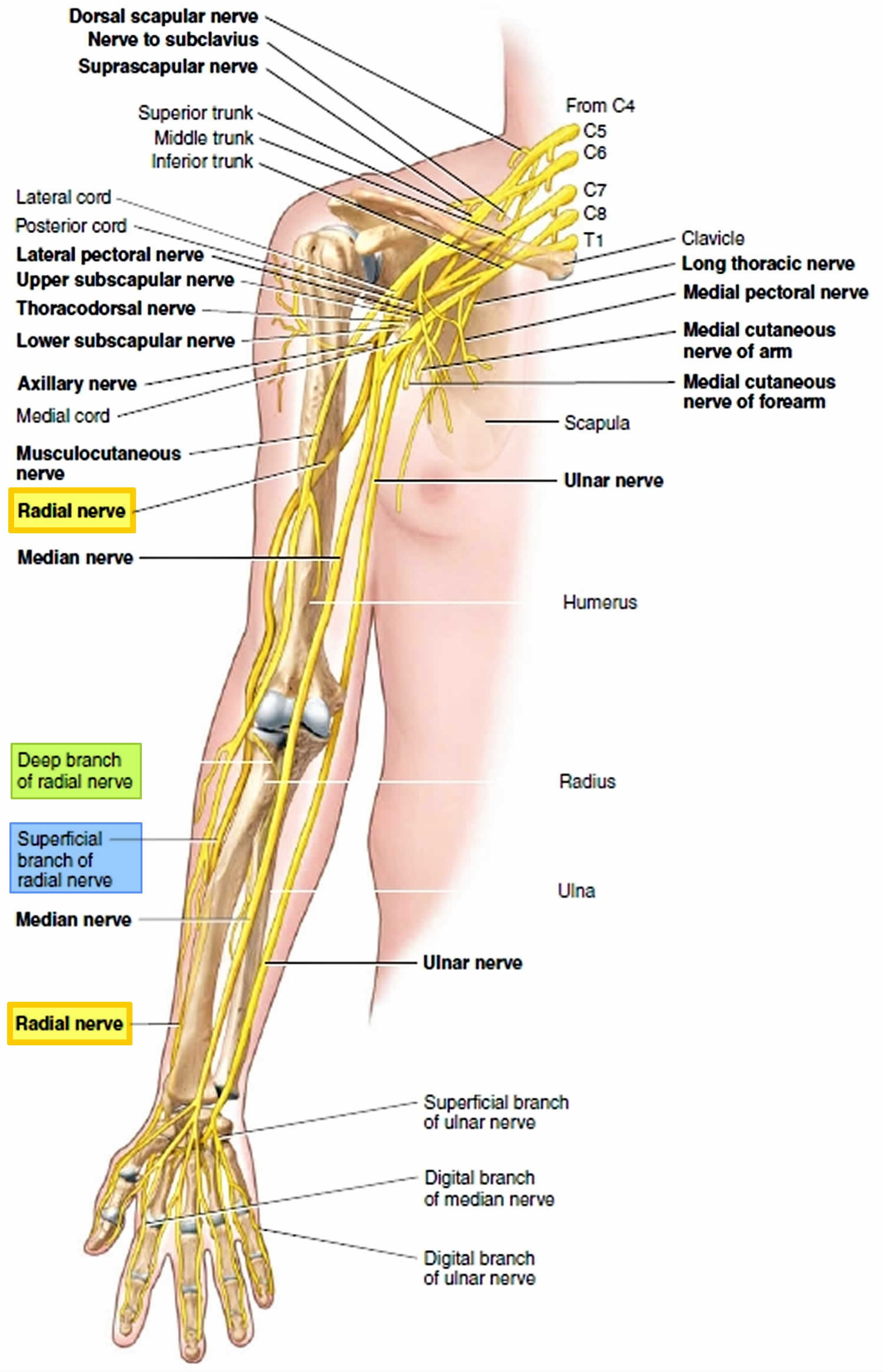
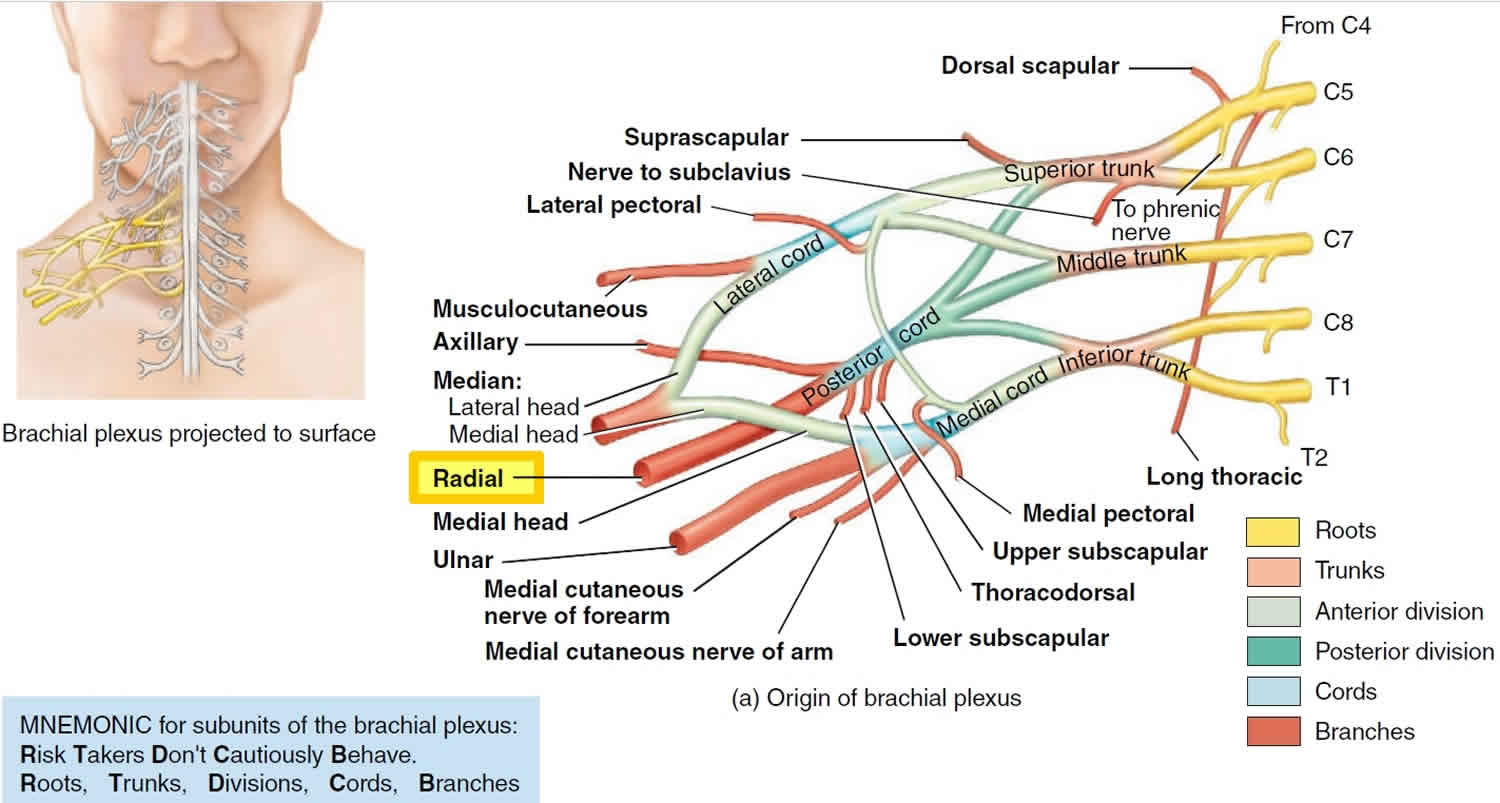
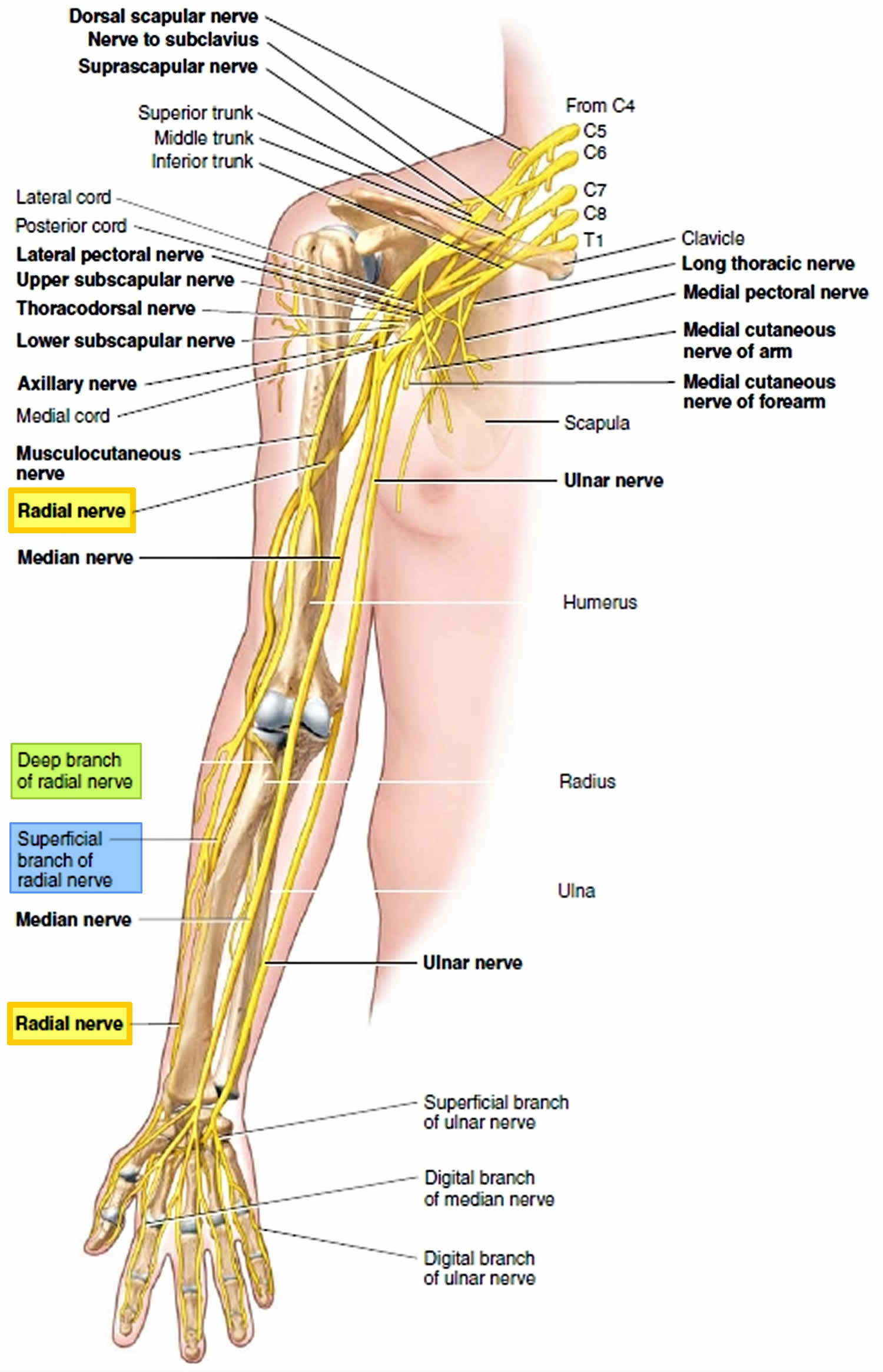
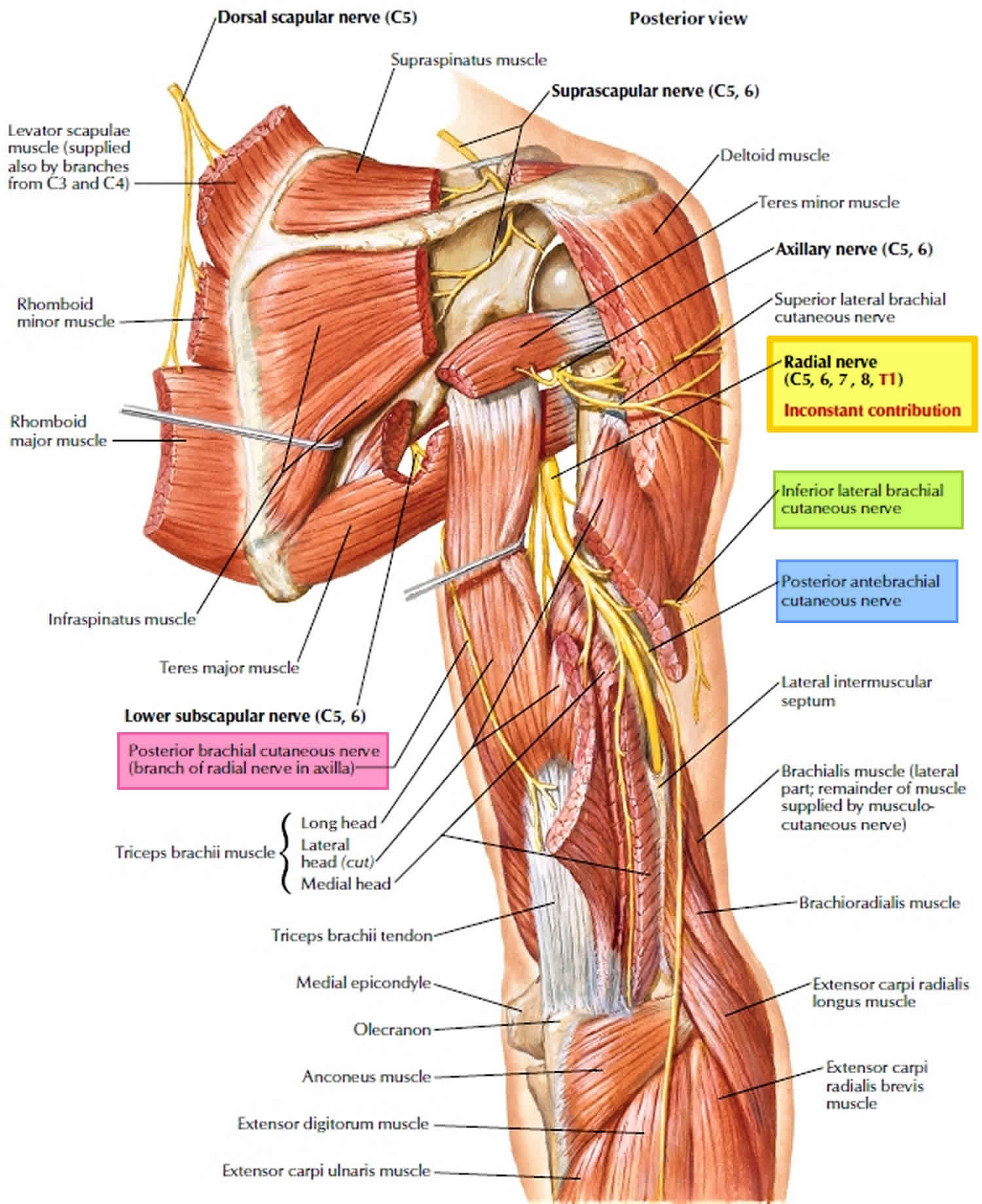
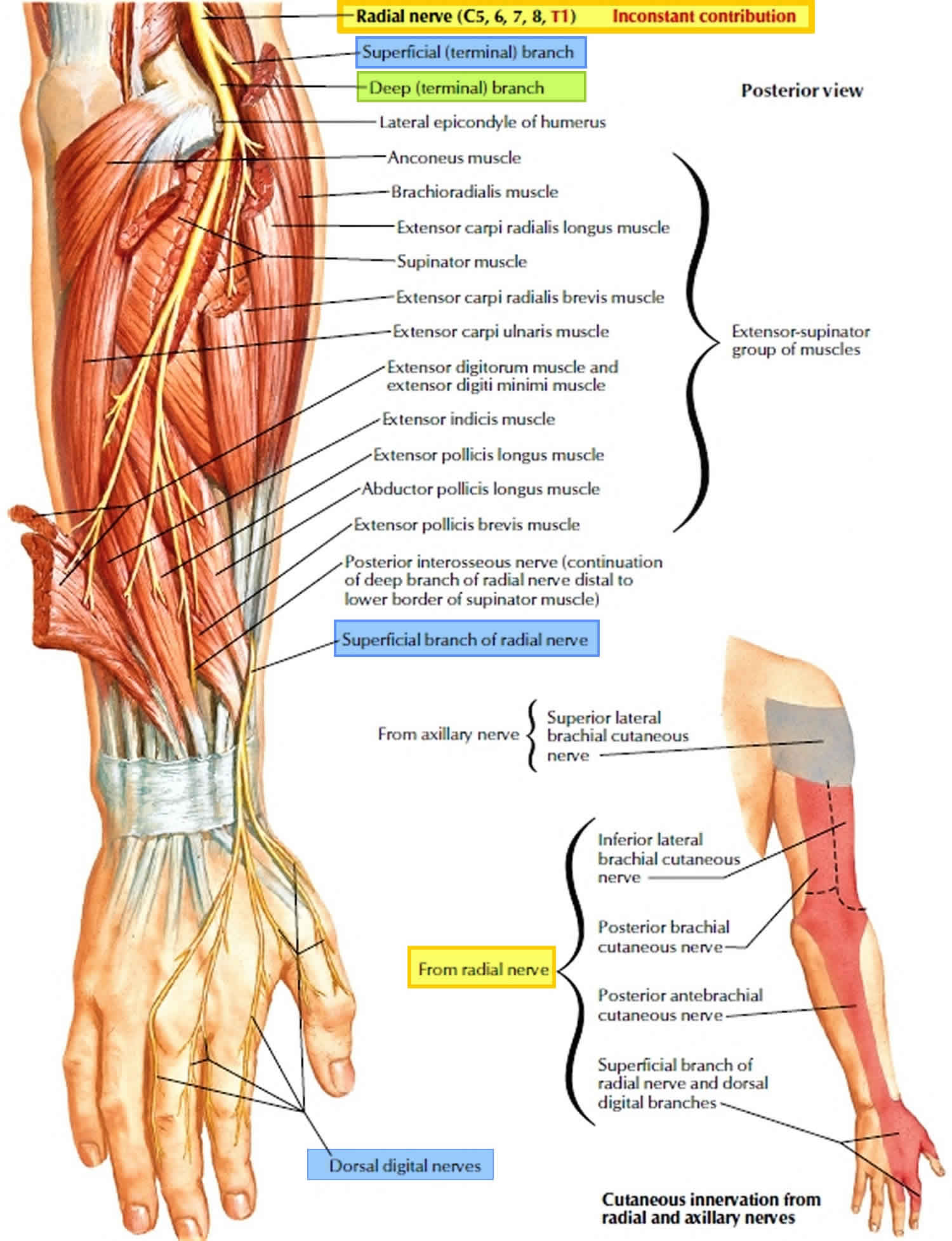
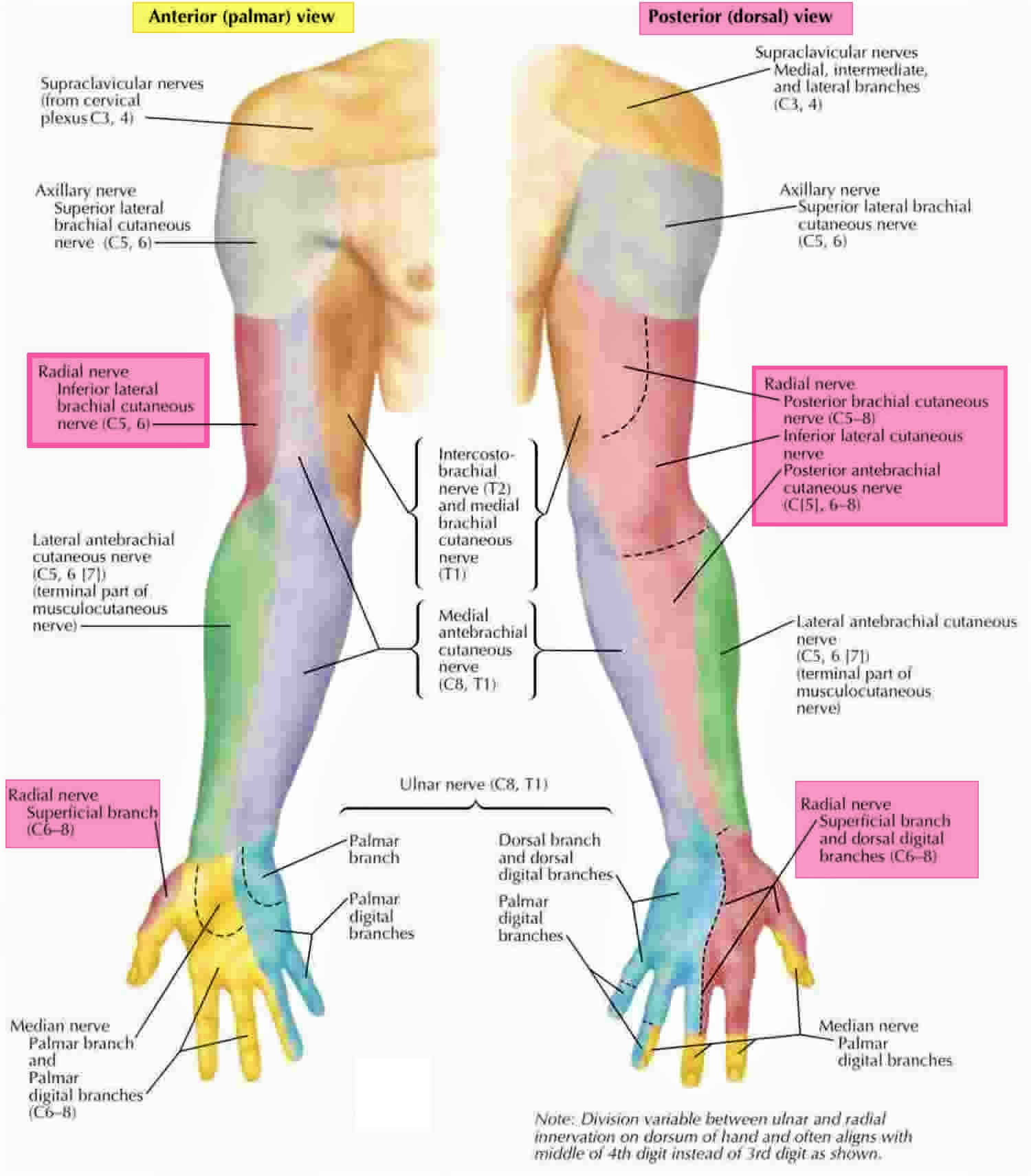
The radial nerve arises from ventral rami of C5 to C8 (+/- T1) and is a continuation of the posterior cord of the brachial plexus and is the largest branch of the brachial plexus, innervating almost the entire posterior side of the upper limb and provides a motor function to the extensor muscles of the forearm, wrist, fingers, and thumb.
Within the axilla, the radial nerve has three branches: sensory posterior cutaneous nerve of the arm and motor branch to the long and medial head of the triceps 1. The radial nerve passes anterior to the subscapularis, latissimus dorsi and teres major. This is the first possible site of compression. An anomalous muscle, the accessory subscapularis-teres-latissimus is reported in literature to be another cause of compression of the radial nerve at this level 2. Another potential cause of compression, as described by Spinner 3 is penetration of the nerve directly by the subscapular artery more distally in the axilla, forming a neural loop.
The radial nerve enters the posterior compartment of the arm by traveling through the triangular interval bounded by the teres major superiorly, the long head of the triceps medially and the lateral head of the triceps laterally. The radial nerve then exits the axilla, courses through the lateral head of triceps brachii and winds around the posterior humerus in the radial groove accompanied by the profunda brachii artery, sending branches to the triceps brachii. Lorem et al. 4 described this as another possible site of entrapment. Familial radial nerve entrapment syndrome 5 also occurs secondary to compression at the lateral head of the triceps. Intermittent compression of the nerve may also occur secondary to genetic defect in Schwann cell myelin metabolism 6. The radial nerve gives off the following branches in the upper arm – the inferior lateral cutaneous nerve of the arm, posterior cutaneous nerve of the forearm and motor branches to the lateral head of triceps and anconeus. The radial nerve is in close proximity to the humerus in the spiral groove and is easily identified on ultrasound in its short axis overlying the humerus between the lateral and medial heads of the triceps. The radial nerve then courses from the posterior to anterior compartment of the arm by piercing the lateral intermuscular septum which is another possible site of entrapment.
The radial nerve then curves anteriorly around the lateral epicondyle at the elbow, where it divides into a superficial and a deep branches (posterior interosseous nerve) under the margin of the brachioradialis muscle in the lateral border of the cubital fossa.
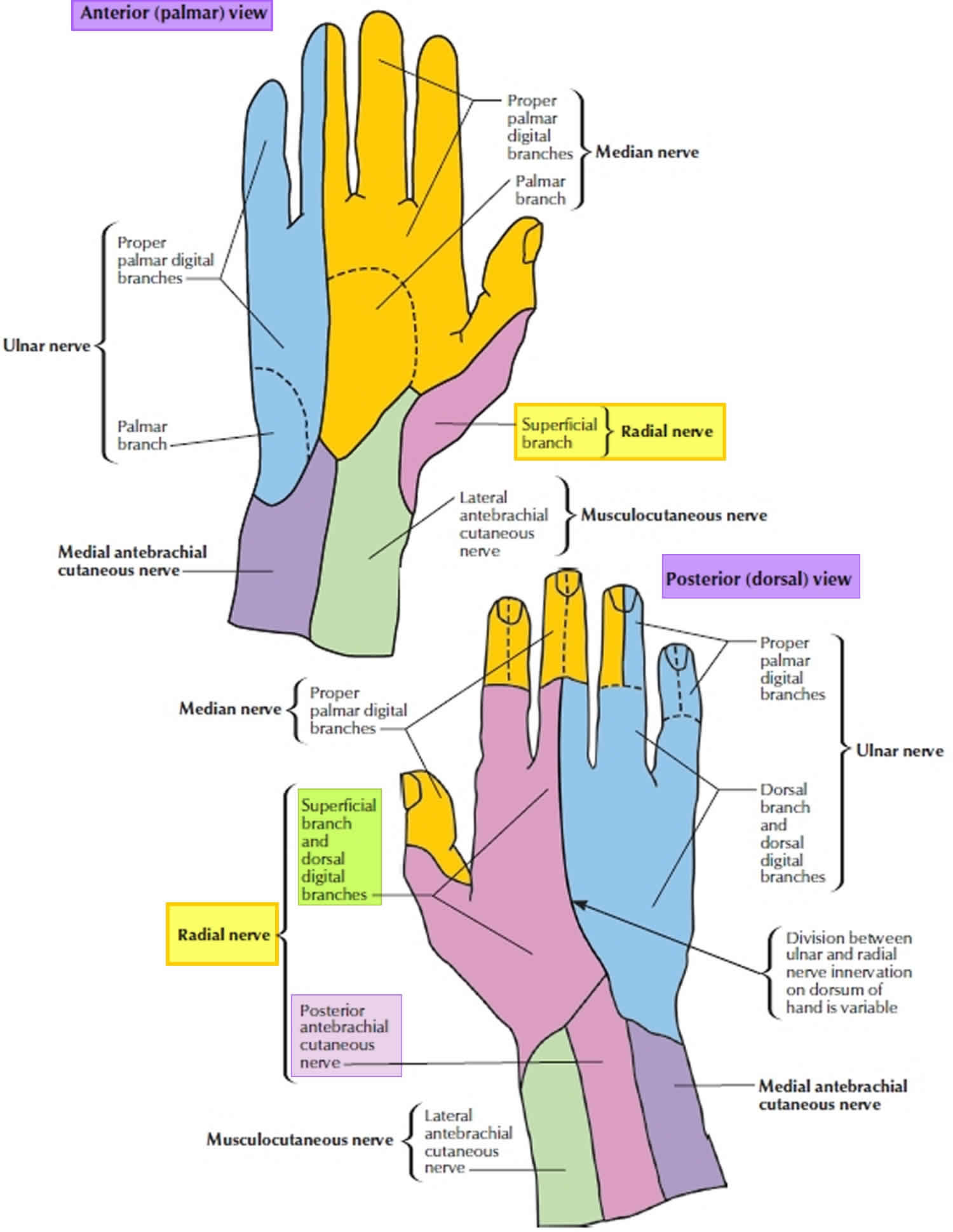
The deep branch (posterior interosseous nerve) is predominantly motor and passes between the two heads of the supinator muscle to access and supply muscles in the extensor muscles on the forearm. The deep branch (posterior interosseous nerve) winds around the radial head, lying between two heads of the supinator muscle and then travels on the dorsal surface of the interosseous membrane. The superficial layer of the supinator muscle forms the arcade of Frohse which is the most common site of entrapment neuropathy causing the radial tunnel syndrome 7. Two anomalous courses of the posterior interosseous nerve have been reported in the literature by Woltman and Learmonth. First is passage of the nerve within the substance of the supinator, and the other involves a branch travelling superficial to the supinator brevis 8. The origin of the radial tunnel is where the deep branch (lateral) courses over the radio-humeral joint. The tunnel ends at the distal edge of the superficial supinator where the posterior interosseous nerve is formed. Radial tunnel syndrome can be caused by the arcade of Frohse, fibrous fascial bands coursing superficial to the nerve or the vascular leash of Henry 9 which is formed by the recurrent radial vessels. The posterior interosseous nerve supplies the abductor pollicis longus, the extensor pollicis brevis, the extensor indicis proprius and the extensor pollicis longus.
The superficial branch of the radial nerve is sensory. The superficial radial nerve descends medially along the lateral edge of the radius under cover of the brachioradialis muscle and in association with the radial artery. Approximately two-thirds of the way down the forearm, the superficial branch of the radial nerve passes laterally and posteriorly around the radial side of the forearm deep to the tendon of the brachioradialis . The superficial radial nerve continues into the hand where it pierces the lateral fascia to enter the anatomical snuffbox and gives sensory innervation to the dorsal surface of three and a half digits on the radial aspect. It also innervates the extensor digitorum, the extensor digiti minimi and the extensor carpi ulnaris muscles.
Figure 1. Radial nerve
Figure 2. Radial nerve in the arm and posterior shoulder
Figure 3. Radial nerve in the forearm
Figure 4. Radial nerve distribution
Figure 5. Radial nerve innervation
Radial nerve injury
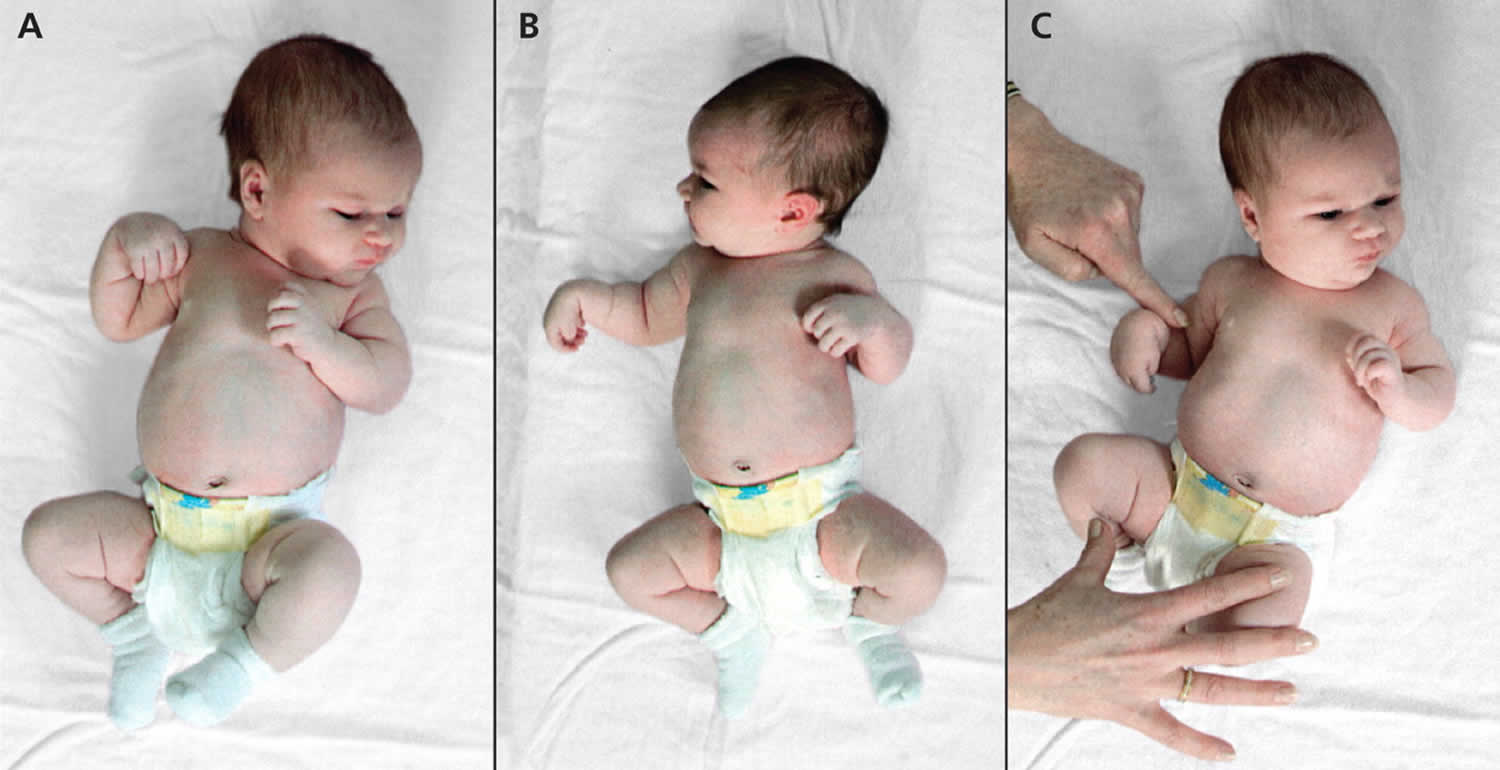
Trauma to the radial nerve results in wrist-drop, an inability to extend the hand at the wrist (Figure 6). If the lesion occurs far enough superiorly, the triceps muscle is paralyzed, so that the forearm cannot be actively extended at the elbow. Many fractures of the humerus follow the radial groove and the radial nerve may become stretched or transected in this region, leading to permanent damage and loss of function. The radial nerve can also be crushed in the axilla by improper use of a crutch or if a person falls asleep with an arm draped over the back of a chair.
Fracture of humerus shaft is the most common cause of radial nerve injury in the upper arm 10. Humeral fractures are due to a fall (87%), motor accidents (8%) or direct trauma (5%) 11. The overall prevalence of radial nerve palsy after fracture of the humerus shaft is 11.8% and commonly occurs following fractures of the middle and middle-distal parts of the shaft 12. Use of high-resolution ultrasound in cases of post-traumatic radial nerve palsy helps in rapid assessment of the nerve throughout its course and helps in identifying the exact site and cause of palsy 1. Ultrasound is widely available, less expensive, has no contraindications and can be done at the bed side in cases of trauma. The nerve is easily identified in its short axis in the distal upper arm where it lies between the brachialis and brachioradialis and then traced proximally and distally. The pathological segment of the nerve is identified by decreased echogenicity, change in calibre, loss of continuity or impingement by or entrapment in the fracture segment.
Figure 6. Radial nerve palsy
Footnote: Typical posture of the upper limb in right radial nerve palsy of the newborn. The patient shows a wrist drop and an inability to extend the thumb and metacarpophalangeal joints of the fingers (A), active external rotation of the right shoulder, which is universally seen in radial nerve palsy of the newborn (B), and intact flexion of the right elbow (C).
[Source 13 ]Radial nerve injury causes
Damage to one nerve group, such as the radial nerve, is called mononeuropathy. Mononeuropathy means there is damage to a single nerve. Diseases affecting the entire body (systemic disorders) can also cause isolated nerve damage.
Causes of radial nerve palsy are manifold with fracture of the humerus shaft being the commonest association. It can occur due to entrapment of the nerve at anatomical sites, entrapment within scar tissue, pressure by tourniquet, under-arm crutches, healing callus, etc. Iatrogenic radial nerve palsy is another common cause of injury which can occur after fracture reduction or after operative management of fracture of the humerus or radius. Elbow surgeries like arthroplasty, radial head fracture repair, synovectomy can cause posterior interosseous nerve palsy. Penetrating injuries like gun shot injuries, animal bites, sharp objects, and intramuscular injections can cause direct insult to the nerve. Thermal and burn injuries are another cause of radial nerve palsy which may also include other nerves in the region of the burn. Systemic demyelinating diseases, lead poisoning or neurotoxic drugs may affect the radial nerve along with other peripheral nerves.
Tumor and tumor-like lesions involving the radial nerve include eripheral nerve sheath tumours, fibrolipomatous hypertrophy, intraneural lipomas, intraneural ganglion, true neuromas and pseudo neuromas 14.
Causes of radial nerve mononeuropathy include:
- An illness in the whole body that damages a single nerve
- Post-traumatic radial nerve palsy
- Direct injury to the radial nerve
- Penetrating trauma to the arm
- Long-term pressure on the radial nerve
- Pressure on the radial nerve caused by swelling or injury of nearby body structures
- Iatrogenic causes of radial nerve palsy may be manifold. Immediate post-operative wrist drop may be due to direct injury to the nerve, local hematoma causing compression, implant abutting the nerve or due to ‘tourniquet palsy’ or residual block.
- Peripheral nerve sheath tumours include neurofibroma and schwannoma and may be benign or malignant.
Radial neuropathy occurs when there is damage to the radial nerve, which travels down the arm and controls:
- Movement of the triceps muscle at the back of the upper arm
- Ability to bend the wrist and fingers backward
- Movement and sensation of the wrist and hand
When damage destroys the radial nerve covering (myelin sheath) or part of the radial nerve itself, nerve signaling is slowed or prevented.
Damage to the radial nerve can be caused by:
- Broken arm bone and other injury
- Diabetes
- Improper use of crutches
- Lead poisoning
- Long-term or repeated constriction of the wrist (for example, from wearing a tight watch strap)
- Long-term pressure on the nerve, usually caused by swelling or injury of nearby body structures
- Pressure to the upper arm from arm positions during sleep or coma
In some cases, no cause can be found.
Radial nerve injury symptoms
Radial nerve injury symptoms may include any of the following:
- Abnormal sensations in the back and thumb side of the hand, or in the thumb, 2nd, and 3rd fingers
- Weakness, loss of coordination of the fingers
- Problem straightening the arm at the elbow
- Problem bending the hand back at the wrist, or holding the hand
- Pain, numbness, decreased sensation, tingling, or burning sensation in the areas controlled by the nerve
Patients with radial neuropathy can present either with motor dysfunction or sensory symptoms only. Pain over the lateral aspect of the arm extending up to the wrist is the most common complaint in cases of radial tunnel syndrome 15. Injury to the radial nerve high up in the arm can result in complete loss of extensor function while injuries distal to the supply of triceps brachii spares its function. Fracture of the humerus shaft can result in wrist drop as injury to the nerve usually occurs in the spiral groove or in the mid-arm 10. The patients will also have loss of sensation over the lateral aspect of arm, forearm, thenar eminence and radial three and a half digits.
Compression of the superficial branch causes paralysis of the extensor carpi ulnaris, extensor digiti quinti and extensor digitorum communis, while compression of the posterior interosseous nerve causes paralysis of the abductor pollicis longus, extensor pollicis brevis, extensor pollicis longus and extensor indicis proprius. Function of the extensor carpi radialis longus is spared as the fibres arise more proximally from the main branch of the radial nerve. This results in finger drop with deviation of the wrist to the radial aspect which is the classical presentation in cases of posterior interosseous nerve palsy. Wartenburg syndrome is entrapment of the superficial branch at the distal radius and presents with pain and numbness in the posterior part of the thumb 16.
Patients with peripheral nerve sheath tumours may present with visible swelling with no motor or sensory deficit.
Clinical examination and electrodiagnostic studies (nerve conduction velocity and electromyography [EMG]) have been the mainstays of diagnosis in neuropathies as they provide essential information about the type of dysfunction and help in clinical monitoring. EMG may not be positive for 3–6 weeks following injury. Tinel’s sign helps in assessing the possible site of injury and helps in assessment of improvement over time. Nerve injuries were classified by Seddon in 1943 and expanded by Sunderland in 1951. Mackinnon and Dellon in 1992 added grade 6 injury to Sunderland’s grading scheme and defined it as a mixed type of injury which denotes various types of injuries across the cross section of the nerve 17. Table 1 below illustrates this classification along with imaging findings in different types of nerve injuries.
Radial nerve injury possible complications
Radial nerve injury complications may include:
- Mild to severe deformity of the hand
- Partial or complete loss of feeling in the hand
- Partial or complete loss of wrist or hand movement
- Recurrent or unnoticed injury to the hand
Radial nerve injury diagnosis
Your doctor will examine you and ask about your symptoms and medical history. You may be asked what you were doing before the symptoms started.
Tests that may be needed include:
- Blood tests
- Imaging tests to view the nerve and nearby structures
- Electromyography (EMG) to check the health of the radial nerve and the muscles it controls
- Nerve biopsy to examine a piece of nerve tissue (rarely needed)
- Nerve conduction tests to check how fast nerve signals travel
Radial nerve injury treatment
The goal of treatment is to allow you to use the hand and arm as much as possible. Your doctor will find and treat the cause, if possible. Sometimes, no treatment is needed and you will get better on your own.
If there is a mechanical cause such as a bone spur or compression, then surgery may be helpful. The timing of surgery when radial nerve palsy is due to a humeral fracture is not yet known 18. Some surgeons wait a few months to see if spontaneous recovery occurs before undertaking explorative surgery. In the acute setting of humeral shaft fracture, proper immobilization of the wrist is necessary. This immobilization can be made possible with a modified coaptation splint 19. Surgical exploration of the radial nerve is appropriate if the radial nerve palsy occurs during splint application and does not resolve with removal of the splint. Approximately 70% of radial nerve palsy cases have been reported to be resolved with conservative treatment. In the case of immunologically mediated wrist drop, as in mixed cryoglobulinemia, drugs such as rituximab may facilitate a rather rapid recovery 20.
If medicines are needed, they may include:
- Over-the-counter or prescription pain medicines
- Corticosteroid injections around the nerve to reduce swelling and pressure
Your doctor will likely suggest self-care measures. These may include:
- A supportive splint at either the wrist or elbow to help prevent further injury and relieve the symptoms. You may need to wear it all day and night, or only at night.
- An elbow pad of the radial nerve is injured at the elbow. Also, avoid bumping or leaning on the elbow.
- Physical therapy exercises to help maintain muscle strength in the arm.
Occupational therapy or counseling to suggest changes in the workplace may be needed.
Surgery to relieve pressure on the radial nerve may help if the symptoms get worse, or if there is proof that part of the nerve is wasting away.
Figure 7. Radial nerve palsy splint (modified coaptation splint)
Footnote: Coaptation splinting is the standard of treatment for acute humeral 28 shaft fractures in the emergency department. A and B, Coaptation portion of the splint is applied first starting fromunder the axilla to the top of the shoulder. C and D, The intrinsic plus component is placedwith careful attention
paid to wrist extension.
Figure 8. Radial nerve palsy splint (modified coaptation splint continued)
Footnote: The proper molds are applied. A, Valgus mold to prevent healing of humeral shaft fracture in varus. B, Intrinsic plus splint with wrist in extension to prevent wrist drop.
[Source 21 ]Figure 9. Radial nerve palsy splint (modified coaptation splint – final position)
[Source 21 ]Radial nerve injury prognosis
If the cause of the radial nerve injury can be found and successfully treated, there is a good chance that you will fully recover. In some cases, there may be partial or complete loss of movement or sensation. Factors that may affect results after radial nerve repair include age, the type of wound and nerve, and location of the injury. Although radial nerve injuries may create lasting problems, proper treatment helps patients return to more normal function.
Radial nerve entrapment
Radial nerve entrapment is an uncommon condition caused by the compression or entrapment of the radial nerve that can occur at any location within the course of the radial nerve distribution, but the most frequent location of radial nerve entrapment occurs in the proximal forearm. This most common location is typically in proximity to the supinator and often will involve the posterior interosseous nerve branch. Depending on the location of radial nerve entrapment a patient may experience pain, numbness, weakness, and overall dysfunction or any combination of these 22. Radial nerve entrapment is uncommon and often under-recognized. The annual incidence rate of the posterior interosseous nerve compression is estimated to be 0.03% while the rate for superficial radial nerve compression is 0.003% 23.
Radial nerve entrapment is typically a result of radial nerve injury secondary to compression, traction, or direct trauma causing a process of local swelling, edema, or even partial or complete laceration. The compression and/or traction often occur secondary to repetitive motions causing inflammation or architectural changes to the surrounding tissue. There are varying degrees of radial nerve damage severity. In mild cases, the compression of the radial nerve causes no permanent damage to the nerve and nerve sheath fully recover. More severe cases can cause permanent damage to the radial nerve and/or nerve sheath causing persistent deficits.
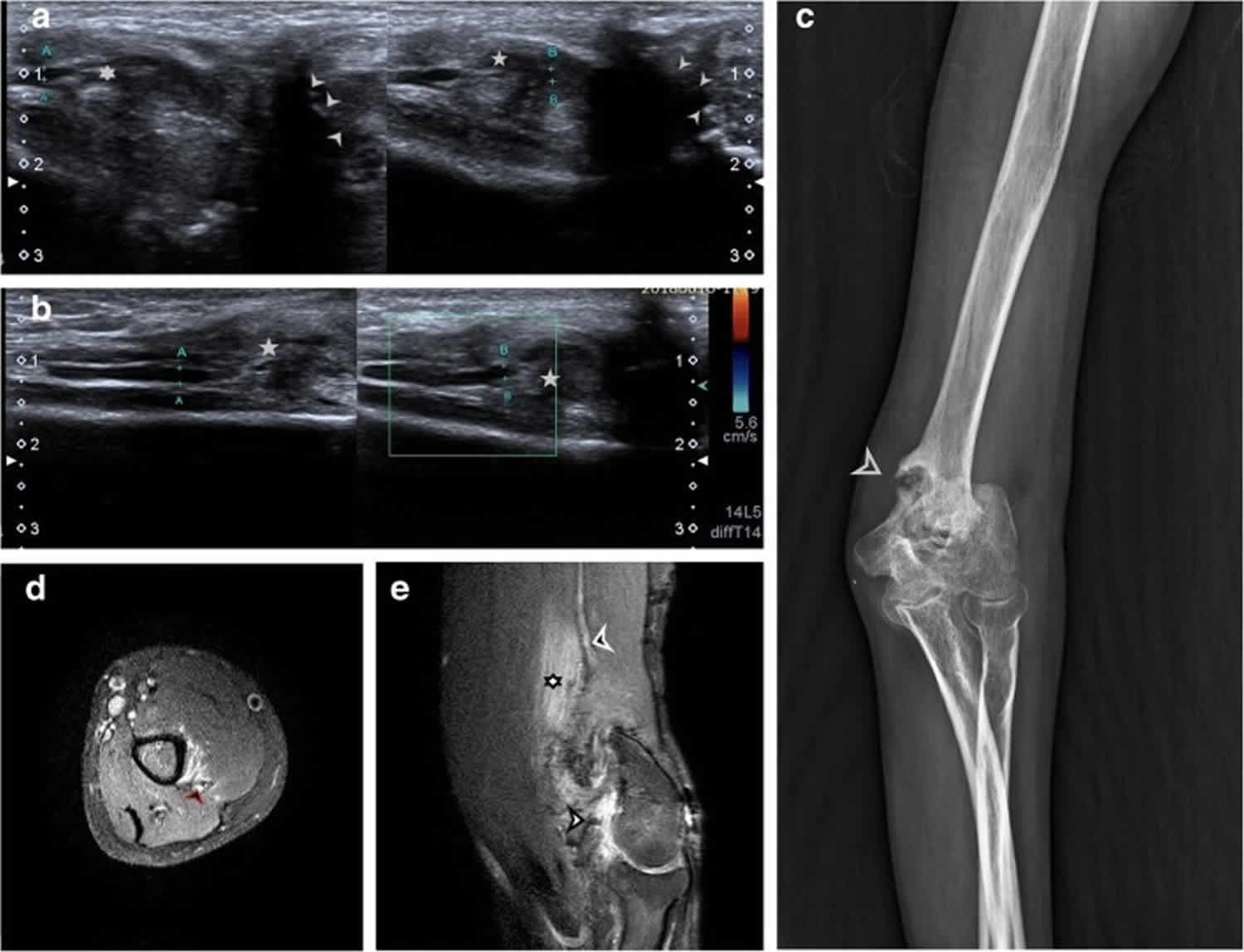
Figure 10. Radial nerve entrapment
Footnote: Radial nerve entrapment in local scar tissue at the site of chronic inflammation in a case of malunited supracondylar fracture of the humerus. (a) Hypoechoic radial nerve (point A and B) is seen entrapped within mixed echogenic chronic inflammatory soft tissue (5 point and 6 point star). Malunited fracture of humerus can be seen adjacent to it (arrowheads). (b) Long axis view of hypoechoic radial nerve (point A and B) seen entering into the chronic inflammatory tissue. There was no evidence of increased vascularity of the nerve. (c) Plain radiograph showing malunited, displaced fragment of supracondylar fracture of humerus. (d) Axial proton density sequence showing hyperintense radial nerve (black arrowhead) with surrounding hyperintense muscle oedema. (e) Sagittal proton density sequence showing heterogeneously hyperintense area of chronic inflammation in region of malunited supracondylar fracture of humerus (white arrowhead). The radial nerve is enlarged and hyperintense (black arrowhead) and is not visualised within the area of chronic inflammation and surrounding muscle oedema (6 point star) due to similar signal intensities.
[Source 1 ]Radial nerve entrapment causes
Radial nerve entrapment is often thought to be a result of overuse but can certainly occur secondary to other causes such as direct trauma, fractures, lacerations, compressive devices, or post-surgical changes 24. The radial nerve divides into the superficial radial and posterior interosseous nerves at the level of the radiocapitellar joint. The posterior interosseous nerve runs along the radial neck before piercing the supinator muscle, a common site of entrapment. The radial nerve further divides into four terminal branches that can typically be compressed at one of four other sites as well. These four sites are the fibrous bands around the radial head, the recurrent radial vessels, the arcade of Frohse, and/or the tendinous margin of the extensor carpi radialis brevis. Overuse actions and exercises that can lead to radial nerve entrapment are often repetitive pronation and supination of the wrist and forearm and commonly occur in the locations discussed previously 25.
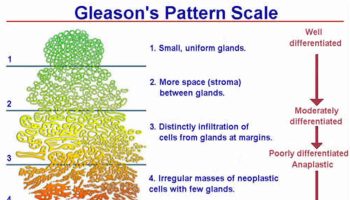
Multiple classification system exist to categorize radial nerve injury grading. A popular one is the Sunderland Classification which is detailed as follows 24:
- 1st degree
- Mild neurapraxia (traction/compression)
- At most in early/low grade nerve injuries, the myelin sheath is compromised
- 2nd degree
- Only the myelin sheath and axon are injured or disrupted
- 3rd degree
- Injury with endoneurial scarring; all components of the peripheral nerve are injured except the perineurium and epineurium
- Most variable degree of ultimate recovery
- 4th degree
- Nerve in continuity but at the level of injury there is complete scarring across the nerve, only the epineurium remains intact
- 5th degree
- Included within Seddon’s neurotmesis
Correlating Sunderland and Seddon’s classification systems with one another:
- Seddon first degree neurapraxia is the same as Sunderland 1st degree injury
- Seddon second degree axonotmesis is the same as Sunderland 2nd degree injury
- Seddon third degree neurotmesis injuries span Sunderland 3rd, 4th, and 5th degree injuries
Table 1. Correlation between Seddon’s & Sunderland’s classification of nerve injury with imaging findings
| Seddon | Sunderland | Description | MRI | Ultrasound |
|---|---|---|---|---|
| Neuropraxia | 1 | Conduction block | T2 hyperintensity | Decreased nerve echogenicity (hypoechoic) |
| Axonotmesis | 2 | Discontinuity of the axon with Wallerian degeneration | T2 hyperintensity with increased size. Hyperintensity in muscles due to denervation. | Decreased echogenicity and increased calibre of the nerve |
| 3 | Scarring of the endoneurium | Endoneurium can not be delineated with current MR technique. T2 hyperintensity with increased size. Hyperintensity in muscles due to denervation. | Focal decrease in echogenicity with increase in calibre with change in echotexture of the affected muscles. | |
| 4 | Neuroma in continuity with formation of a scar which blocks nerve regeneration | T1 hypointense, T2 hyperintense focal enlargement with loss of fascicular pattern. Hyperintensity in muscles due to denervation. | Hypoechoic fusiform lesion in continuity with the nerve with loss of fascicular architecture with altered echogenicity of denervated muscles. | |
| Neurotmesis | 5 | Rupture of the nerve | End neuroma formation at proximal end with denervation changes in muscle | Hypoechoic neuroma at proximal end with local soft-tissue oedema and denervation changes in muscle. |
| Mackinnon and Dellon type VI | Mixed injury | Variable findings with nerve heterogeneity and muscle denervation changes | Hypoechoic enlarged with mixed findings of scarring, discontinuity or neuroma formation. |
Radial nerve entrapment symptoms
Radial nerve entrapment presentation can certainly vary given multiple areas of possible entrapment. Symptoms are usually very slow developing. The duration of symptoms often averages multiple years before a definitive diagnosis is made 24. Symptoms of radial nerve entrapment are pain, sensory and motor changes, paresthesias, and/or paralysis.
Physical exam and/or history often reveal symptoms limited to the dorsoradial aspect of the distal forearm and hand. Findings of decreased sensation over the dorsoradial aspect of the forearm or hand are helpful in establishing the diagnosis. A positive Tinel sign along the radial aspect of the mid forearm is suggestive of this process. Wrist flexion, ulnar deviation, and pronation place strain on the nerve and will often reproduce or exacerbate symptoms. Resisted extension of the middle finger with the elbow extended is another sign of nerve entrapment. This sign is often used to aid in the diagnosis of lateral epicondylitis but it also often positive in cases of radial nerve entrapment.
Radial nerve entrapment complications
Most complications are related to surgery and include:
- Stretching of the radial nerve
- Severing of the radial nerve
- Incomplete release
- Muscle atrophy
Radial nerve entrapment diagnosis
- If radial nerve entrapment is suspected, radiography should be performed to detect or rule out a fracture, healing callus, or tumor as the cause of radial nerve entrapment.
- Ultrasonography can often provide reliable visualization of injured nerves. Axonal swelling, hypoechogenicity of the nerve, loss of continuity of a nerve bundle, formation of a neuroma, and/or partial laceration of a nerve can all be visualized which may aid in diagnosis.
- Magnetic resonance imaging (MRI) can be useful in detecting more subtle causes not found on radiographs or ultrasound such as small tumors, masses, aneurysms, or a compressive synovitis. MRI can also at times detect nerve changes during acute radial nerve entrapments.
- A diagnostic nerve block to help define the distribution of pathology and presentation is considered in some situations.
- Electromyography (EMG)/nerve conduction studies can also be considered but are inconsistent and should only be considered if surgery is a possibility.
- No standard laboratory work is necessary for establishing the diagnosis 26.
Radial nerve entrapment treatment
The acute management of radial nerve entrapment is surgical 24. However, once the surgery is completed, the patient needs to be followed by a neurologist, hand surgeon, physical and occupational therapist. After the healing is complete, most patients require extensive rehabilitation to recover motor and sensory function. In addition, the patient must wear protective splints to protect the hand. Recovery often takes months, and compliance with the exercise program is key 27.
First and Second Degree Radial Nerve Injuries
- Most patients respond and recover after several months — recommended management consists of serial exams and serial electromyography (EMG)/nerve conduction studies testing
- Most patients respond well to conservative therapy. Consider removing any restrictive or compressive devices that are routinely worn. Consider relative rest from offending activity such as limiting repetitive pronation, supination, wrist flexion, and ulnar deviation. Often nerve glide exercises as part of occupation/physical therapy are performed in conjunction with rest and activity modification. If symptoms do not resolve with cessation of activity and rest, then consider splinting.
- If an area of pathology indicates possible compression and can be visualized on ultrasound, providers can consider ultrasound guided hydrodissection to free the compressed portion of the nerve.
- Oral or topical NSAIDs can be used for pain. Steroid and an anesthetic combination can be injected into the point of maximal tenderness for symptomatic relief. The steroid may help decrease any inflammation contributing to the process.
- In the setting of suspected mild degrees of nerve injury, but either prolonged, absent, or delayed evidence of recovery of nerve function both clinically and by serial electromyography (EMG)/nerve conduction study testing, surgery should be the last option if this process has become chronic and conservative treatment has failed after six to 12 months 28.
Third Degree Radial Nerve Injuries (Neurotmesis)
- Acutely, direct surgical repair of the partial versus complete nerve laceration
- Nerve grafting techniques are employed in the setting of lacerations with retractions; often this can present in the subacute setting after injury
- Residual defects or “injury gap” measuring >2.5cm are recommended for nerve grafting techniques
- Autograft options include the sural or saphenous nerves
- There is no documented improved functional recovery or outcome when comparing autograft versus allograft or nerve conduits
- Autograft options include the sural or saphenous nerves
Radial nerve entrapment prognosis
The prognosis after radial nerve entrapment depend on the severity of the injury. For those with neuropraxic injury, the outcome is good in most cases. For those with axonotmesis, recovery depends on the completeness of release. Unfortunately, many patients have residual deficits. Following neurotmesis, recovery is usually limited even with surgical repair. All patients need extended physical and occupational therapy, and recovery can take months or even years 29.
- Agarwal A, Chandra A, Jaipal U, Saini N. A panorama of radial nerve pathologies- an imaging diagnosis: a step ahead. Insights Imaging. 2018;9(6):1021-1034. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6269333/[↩][↩][↩][↩]
- Kameda Y. An anomalous muscle (accessory subscapularis-teres-latissimus muscle) in the axilla penetrating the brachial plexus in man. Acta Anat (Basel) 1976;96:513–533. doi: 10.1159/000144700.[↩]
- Spinner M. Management of nerve compression lesions of the upper extremity. In: Omer GE Jr, Spinner M, editors. Management of Peripheral Nerve Problems. Philadelphia: WB Saunders; 1980. pp. 569–587.[↩]
- Lotem M, Fried A, Levy M, Solzi P, Najenson T, Nathan H. Radial palsy following muscular effort: a nerve compression syndrome possibly related to a fibrous arch of the lateral head of the triceps. J Bone Joint Surg Br. 1971;53:500–506. doi: 10.1302/0301-620X.53B3.500.[↩]
- Lubahn JD, Lister GD. Familial radial nerve entrapment syndrome: a case report and literature review. J Hand Surg Am. 1983;8:297–299. doi: 10.1016/S0363-5023(83)80163-4.[↩]
- Mayer RF, Garcia-Mullin R. Hereditary neuropathy manifested by pressure palsies: Schwann cell disorder? Trans Am Neurol Assoc. 1968;93:238–240.[↩]
- Moradi A, Ebrahimzadeh MH, Jupiter JB. Radial tunnel syndrome, diagnostic and treatment dilemma. Arch Bone Jt Surg. 2015;3(3):156–162.[↩]
- Woltman HW, Learmonth JR (1934) Progressive paralysis of the nervous interosseous dorsalis. Brain 57:25–31[↩]
- Hazani R, Engineer NJ, Mowlavi A, Neumeister M, Lee WPA, Wilhelmi BJ. Anatomic landmarks for the radial tunnel. Eplasty. 2008;8:e37.[↩]
- Mondelli M, Morana P, Ballerini M, Rossi S, Giannini F. Mononeuropathies of the radial nerve: clinical and neurographic findings in 91 consecutive cases. J Electromyogr Kinesiol. 2005;15(4):377–383. doi: 10.1016/j.jelekin.2005.01.003.[↩][↩]
- Epidemiology of humerus fractures in the United States: nationwide emergency department sample, 2008. Kim SH, Szabo RM, Marder RA. Arthritis Care Res (Hoboken). 2012 Mar; 64(3):407-14.[↩]
- Shao YC, Harwood P, Grotz MR, Limb D, Giannoudis PV. Radial nerve palsy associated with fractures of the shaft of the humerus: a systematic review. J Bone Joint Surg Br. 2005;87(12):1647–1652. doi: 10.1302/0301-620X.87B12.16132.[↩]
- Radial nerve palsy in the newborn: a case series. Fatema S. Alsubhi, Abdullah M. Althunyan, Christine G. Curtis, Howard M. Clarke. CMAJ Sep 2011, 183 (12) 1367-1370; DOI: 10.1503/cmaj.110272 http://www.cmaj.ca/content/cmaj/183/12/1367.full.pdf[↩]
- Wadhwa V, Lee PP, Strome GM, Suh KJ, Carrino JA, Chhabra A (2014) Spectrum of superficial nerve-related tumor and tumor-like lesions: MRI features. Acta Radiol 55(3):345–358. 10.1177/0284185113494983[↩]
- Sarhadi NS, Korday SN, Bainbridge LC. Radial tunnel syndrome: diagnosis and management. J Hand Surg Br. 1998;23(5):617–619. doi: 10.1016/S0266-7681(98)80015-6.[↩]
- Lanzetta M, Foucher G. Entrapment of the superficial branch of the radial nerve (Wartenberg’s syndrome): a report of 52 cases. Int Orthop. 1993;17(6):342–345. doi: 10.1007/BF00180450.[↩]
- Mackinnon SE, Dellon AL. Diagnosis of nerve injury. Surgery of the peripheral nerve. NY: Thieme; 1988. pp. 74–78.[↩]
- Keefe P, DeCastro A. Wrist Drop. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532993[↩]
- Streib E. Upper arm radial nerve palsy after muscular effort: report of three cases. Neurology. 1992 Aug;42(8):1632-4.[↩]
- Uppal R, Charles E, Lake-Bakaar G. Acute wrist and foot drop associated with hepatitis C virus related mixed cryoglobulinemia: rapid response to treatment with rituximab. J. Clin. Virol. 2010 Jan;47(1):69-71.[↩]
- Harris AP, et al,Modified coaptation splintwith sugar tong intrinsic plus extension for initial management ofwrist drop, Am J Emerg Med (2016), http://dx.doi.org/10.1016/j.ajem.2015.12.037[↩][↩][↩]
- Dididze M, Sherman Al. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Oct 27, 2018. Pronator Teres Syndrome.[↩]
- Devi BI, Konar SK, Bhat DI, Shukla DP, Bharath R, Gopalakrishnan MS. Predictors of Surgical Outcomes of Traumatic Peripheral Nerve Injuries in Children: An Institutional Experience. Pediatr Neurosurg. 2018;53(2):94-99.[↩]
- Buchanan BK, Varacallo M. Radial Nerve Entrapment. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK431097[↩][↩][↩][↩]
- Olewnik Ł, Podgórski M, Polguj M, Wysiadecki G, Topol M. Anatomical variations of the pronator teres muscle in a Central European population and its clinical significance. Anat Sci Int. 2018 Mar;93(2):299-306.[↩]
- Brown JM, Yablon CM, Morag Y, Brandon CJ, Jacobson JA. US of the Peripheral Nerves of the Upper Extremity: A Landmark Approach. Radiographics. 2016 Mar-Apr;36(2):452-63.[↩]
- Nachef N, Bariatinsky V, Sulimovic S, Fontaine C, Chantelot C. Predictors of radial nerve palsy recovery in humeral shaft fractures: A retrospective review of 17 patients. Orthop Traumatol Surg Res. 2017 Apr;103(2):177-182.[↩]
- Sigamoney KV, Rashid A, Ng CY. Management of Atraumatic Posterior Interosseous Nerve Palsy. J Hand Surg Am. 2017 Oct;42(10):826-830.[↩]
- Bertelli J, Soldado F, Ghizoni MF. Outcomes of Radial Nerve Grafting In Children After Distal Humerus Fracture. J Hand Surg Am. 2018 Dec;43(12):1140.e1-1140.e6.[↩]