Retrocalcaneal bursitis
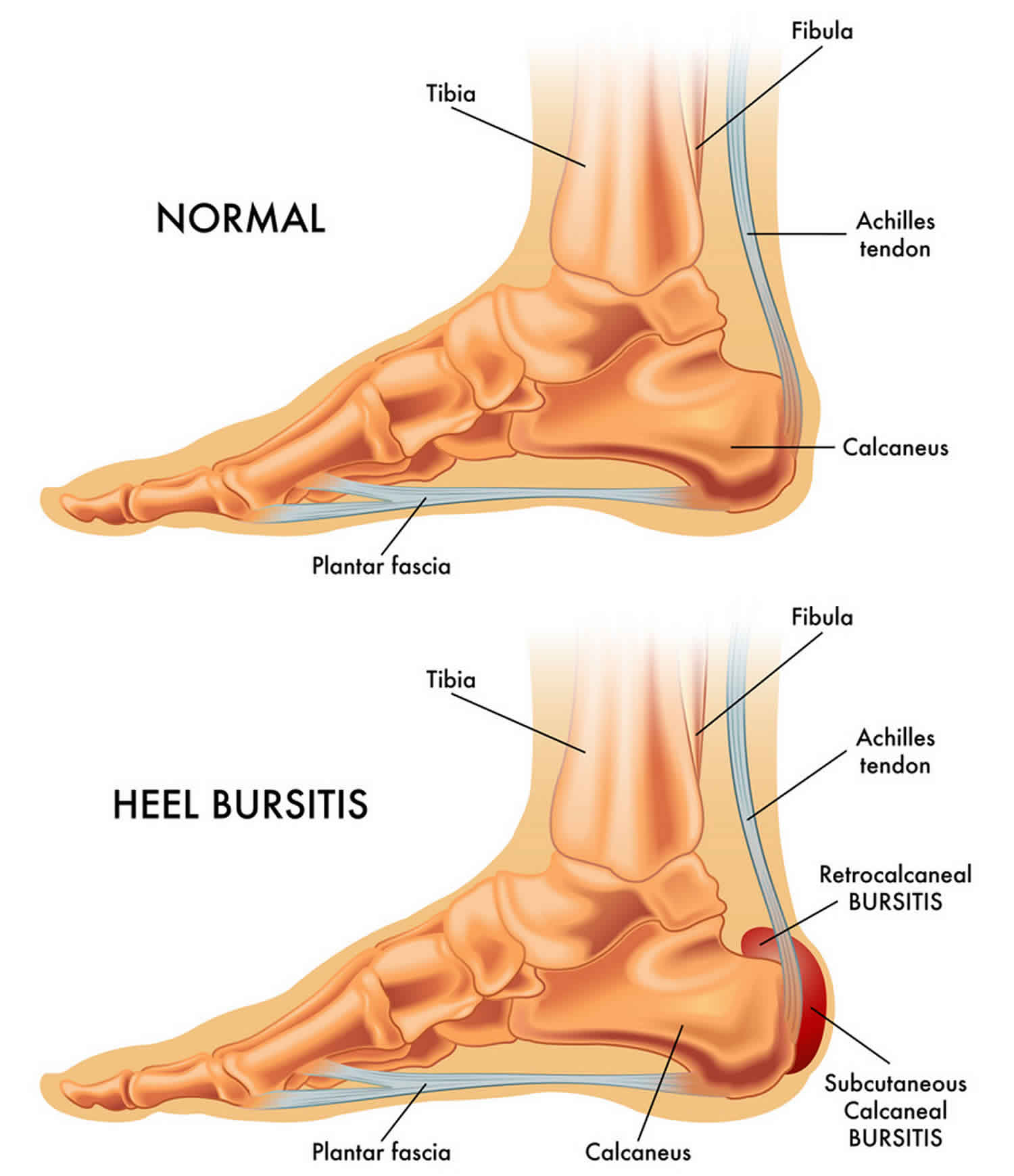
Retrocalcaneal bursitis is a swelling or inflammation of a bursa, which is a synovium-lined, sac-like structure found posterior calcaneus (at the calcaneal insertion site of the Achilles tendon). Two bursae are located just superior to the insertion of the Achilles (calcaneal) tendon. Anterior or deep to the tendon is the retrocalcaneal (subtendinous) bursa, which is located between the Achilles tendon and the calcaneus. Posterior or superficial to the Achilles tendon is the subcutaneous calcaneal bursa, also called the Achilles bursa. Achilles bursa is located between the skin and posterior aspect of the distal Achilles tendon. Inflammation of either or both of these bursa can cause pain at the posterior heel and ankle region 1.
Patients with insertional Achilles tendinopathy often have thickened subcutaneous and retrocalcaneal bursae with higher blood flow in the bursa walls. These patients may also have Haglund deformities 2.
Retrocalcaneal bursitis causes
Inflammation of the calcaneal bursae is most commonly caused by repetitive (cumulative) trauma or overuse, and the condition is aggravated by pressure, such as when athletes wear tight-fitting shoes 3. Retrocalcaneal bursitis may also be associated with conditions such as gout, rheumatoid arthritis, and seronegative spondyloarthropathies. In some cases, retrocalcaneal bursitis may be caused by bursal impingement between the Achilles tendon and an excessively prominent posterosuperior aspect of the calcaneus (Haglund deformity). In Haglund disease, impingement occurs during ankle dorsiflexion 4.
- Overtraining in an athlete, such as with excessive increases in running mileage may lead to retrocalcaneal bursitis.
- Tight or poorly fitting shoes that produce excessive pressure at the posterior heel and ankle due to a restrictive heel counter are another cause of retrocalcaneal bursitis.
- Haglund deformity, which causes impingement between the increased posterosuperior calcaneal prominence and Achilles tendon during dorsiflexion, may lead to retrocalcaneal bursitis.
More recent research suggests that a misaligned subtalar joint axis (measured in terms of joint inclination and deviation) in relation to the Achilles tendon can result in an asymmetrical force load on the tendon disrupting normal biomechanics. This altered joint axis is associated with an increased risk for Achilles pathologies, including bursitis 5.
Retrocalcaneal bursitis prevention
Patients with retrocalcaneal bursitis should consider the following preventive measures:
- Wear properly fitting footwear, and change running shoes on a regular basis, depending on the amount of use.
- Avoid footwear that fits too tightly at the posterior heel.
- Avoid high-heeled shoes.
- Avoid corticosteroid injection by other clinicians, unless the risk of Achilles tendon rupture is fully understood.
Retrocalcaneal bursitis symptoms
In retrocalcaneal bursitis, posterior heel pain is the primary presenting chief complaint, and patients may report limping.
Some individuals may also present with an obvious or noticeable swelling (eg, a “pump bump,” presumably named in association with the wearing of high-heeled shoes or pumps).
- Ask the patient about footwear, such as high-heeled shoes or tight-fitting athletic shoes.
- Specifically ask about any recent change in footwear (eg, new athletic shoes, transition from flat shoes to high heels or from road running shoes to racing flats or to cleats).
Retrocalcaneal bursitis may be unilateral or bilateral.
Individuals who are accustomed to wearing high-heeled shoes on a long-term basis may experience increased stretch and irritation of the Achilles tendon and its associated bursae when switching to flat shoes.
- Ask about the specifics of the patient’s activity levels (eg, include the distances runners travel).
Symptoms often worsen when the athlete is first beginning an activity after resting.
- Ask about previously known or suspected underlying rheumatologic conditions (eg, gout, rheumatoid arthritis, seronegative spondyloarthropathies).
An underlying inflammatory arthritis should be considered in cases where the retrocalcaneal bursitis occurs bilaterally 6.
Physical examination
- Swelling and redness of the posterior heel may be clearly apparent in patients with retrocalcaneal bursitis (eg, pump bump).
- The inflamed area may be slightly warm and tender to palpation.
- Careful examination can help the clinician distinguish whether the inflammation is posterior (superficial) to the Achilles tendon (within the subcutaneous bursa) or anterior (deep) to the Achilles tendon (within the subtendinous bursa).
- Tenderness caused by isolated subtendinous bursitis can best be isolated by palpation just anterior to both the medial and lateral edge of the distal Achilles tendon.
- Tenderness due to insertional Achilles tendinitis is located slightly more distal, where the Achilles tendon inserts onto the posterior calcaneus.
- Plantar fasciitis causes tenderness along the posterior aspect of the sole, but patients should not experience tenderness with palpation of the posterior heel or ankle.
A patient with avulsion or rupture of the Achilles tendon demonstrates a palpable defect in the tendon and a positive Thompson test (ie, squeezing the calf fails to cause plantar flexion due to the loss of Achilles tendon continuity).
Retrocalcaneal bursitis complications
The posterior heel pain may become chronic or progressive, resulting in limping (antalgic gait) and decreased athletic performance.
Achilles tendon rupture may occur secondary to chronic inflammation and/or due to corticosteroid injection.
Retrocalcaneal bursitis diagnosis
Diagnosing retrocalcaneal bursitis requires a multifaceted approach based on patient history and physical and radiographic imaging 7. In current practice, no definitive diagnostic measures exist, as many pathogenic features are not entirely understood. It has been speculated, however, that heel pain in Haglund deformity (which can be associated with retrocalcaneal bursitis) may be secondary to increased bursal pressure. Based on this, a recent pilot project developed minimally invasive technology (butterfly needle and water column) that precisely measured bursal pressure in cadaveric specimens and may serve to aide in the diagnosis of retrocalcaneal bursitis if further studies lend support to the “hypothesis of pressure-induced pathogenesis” 8.
If the retrocalcaneal bursitis cannot be explained by local factors (eg, poorly fitting shoes, increased running, high heels), or if systemic symptoms or signs of rheumatologic involvement exist, consider laboratory studies to evaluate the possibility of gout (hyperuricemia), rheumatoid arthritis (rheumatoid factor [RF]), and seronegative spondyloarthropathies (eg, human leukocyte antigen [HLA] B-27, erythrocyte sedimentation rate [ESR], C-reactive protein [CRP]).
Imaging studies
Plain radiographs of the calcaneus may reveal a Haglund deformity (increased prominence of the posterosuperior aspect of the calcaneus). However, on weight-bearing lateral radiographs, the retrocalcaneal recess often appears normal even in patients with retrocalcaneal bursitis, limiting its usefulness in making this diagnosis 9.
Radiographs may be used as a diagnostic measure to support a clinician’s diagnosis of retrocalcaneal bursitis. Individuals with retrocalcaneal bursitis may have an absence of the normal radiolucency (ie, blunting) that is seen in the posteroinferior corner of the Kager fat pad, known as the retrocalcaneal recess or bursal wedge. This may occur with or without an associated erosion of the calcaneus 10.
Retrocalcaneal bursitis is sometimes associated with several rheumatic conditions such as rheumatoid arthritis, gout and pseudogout. These rheumatic conditions can cause erosions of the bone in the retrocalcaneal region. When these erosions have an undulating, wave-like pattern on lateral radiographs, they have been compared to the appearance of the silhouette of the comb/crest seen on top of a rooster’s head 11.
Evaluation of the soft tissue in the retrocalcaneal space on conventional lateral radiographs is less reliable in assessing for retrocalcaneal bursitis in patients who have previously undergone endoscopic calcaneoplasty, making it difficult to use radiographs diagnostically in evaluating for recurrent retrocalcaneal bursitis in such patients 12.
Plain radiographs can be used to evaluate for stress fracture of the calcaneus. If the studies are negative for a stress fracture, but a stress fracture remains a significant diagnostic consideration, the clinician may wish to pursue 3-phase bone scanning or computed tomography (CT) scanning of the calcaneus.
Magnetic resonance imaging (MRI) may demonstrate bursal inflammation, but this modality probably does not offer much more information than that found by careful physical examination. Theoretically, MRI could help the physician to determine whether the inflammation is within the subcutaneous bursa, the subtendinous bursa, or even within the tendon itself; however, such testing is generally not necessary.
If MRI imaging is needed for confirmation of retrocalcaneal bursitis, the retrocalcaneal bursa will appear as an enlarged, fluid-filled structure with low signal intensity on T1-weighted images and high signal intensity on fluid-sensitive images. Further, there may be associated marrow edema in the calcaneus or the distal Achilles. Edema in the tissues surrounding the retrocalcaneal bursa may be indicative of chronic mechanical irritation 13.
Hybrid imaging modalities, most specifically single-photon emission CT (SPECT)/CT, may assist with early detection of bursitis by offering a precise, accurate, and highly localizing diagnostic image. However, little research exists on the cost benefit of this modality, and, therefore, it is not frequently used for this type of soft-tissue injury 14.
Ultrasonography may be a potentially useful tool for diagnosing pathologies of the Achilles tendon 15. Some clinicians have suggested that ultrasonography can be used in place of MRI in cases in which imaging is desired to investigate pathology at the posterior heel. One study concluded that extended field-of-view sonography when combined with traditional gray-scale sonography has similar sensitivity and specificity to MRI for diagnosing calcaneal bursitis in addition to more rapid results, lower cost, and lack of contraindications 16.
Procedures
Many clinicians advocate the use of corticosteroid injection(s) into the affected bursa, with particular care to avoid injection within the Achilles tendon.
Although there is a theoretical risk of tendon rupture, prospective, randomized studies have not been performed to definitively establish a causal relationship between steroid injections and such tendon ruptures. Instead, the association between steroid injections and subsequent tendon ruptures is mostly based on retrospective case reports. Thus, the cases that were more likely to go on to rupture were potentially those in which a more severe presentation prompted the steroid injections in the first place.
A case report by Sofka et al demonstrated that retrocalcaneal bursitis can be diagnosed and treated with ultrasonography 17. This modality can be used to guide injection into the retrocalcaneal bursa with a combination of local anesthetic (eg, lidocaine, with relief within minutes and duration of several hours) and corticosteroid (eg, triamcinolone, with anti-inflammatory effect within 24-48 hours and a relief duration of weeks to months). In contrast, in an animal study, Hugate et al 18 demonstrated the adverse effects of local corticosteroid injections (both within the tendon substance and into the retrocalcaneal bursa) on the biomechanical properties of the Achilles tendon. The authors stressed that ultrasonographic guidance helps to ensure reliable and accurate delivery of medication into the bursa, while concurrently avoiding intratendinous injection 18.
Retrocalcaneal bursitis treatment
Acute phase
The patient with retrocalcaneal bursitis should be instructed to apply ice to the posterior heel and ankle in the acute period of the bursitis. Icing can be performed several times a day, for 15-20 minutes each. Some clinicians also advocate the use of contrast baths.
Gradual progressive stretching of the Achilles tendon may help relieve impingement on the subtendinous bursa and can be performed in the following manner:
- Stand in front of a wall, with the affected foot flat on the floor. Lean forward toward the wall until a gentle stretching is felt within the ipsilateral Achilles tendon.
- Maintain the stretch for 20-60 seconds and then relax.
- Perform the stretches with the knee extended and then again with the knee flexed.
- To maximize the benefit of the stretching program, repeat the above steps for several stretches per set, several times daily. Avoid ballistic (ie, abrupt, jerking) stretches.
If it is necessary for the patient to decrease his or her activity level due to retrocalcaneal bursitis, alternative means of maintaining strength and cardiovascular fitness should be suggested, such as swimming, water aerobics, and other aquatic exercises.
Other treatment
Changing the patient’s footwear may be the most important form of treatment for retrocalcaneal bursitis. Use of an open-backed shoe may relieve pressure on the affected region. For individuals in whom symptoms were precipitated by a dramatic change from wearing high-heeled shoes to flat shoes (or vice versa), the temporary use of footwear that is a heel height somewhere in between may be necessary. Encourage athletes to change running shoes on a regular basis, because the support and fit of their footwear may change over the course of hundreds of miles of use.
A portion of the heel counter can be cut away and replaced with a soft leather insert to decrease friction at the site where the heel counter meets the patient’s skin. The patient should avoid shoes without laces, because the nature of such footwear is to fit closely onto the heel. Inserting a heel cup in the shoe may help to raise the inflamed region slightly above the shoe’s restricting heel counter. A heel cup should also be placed in the opposite (contralateral) foot’s shoe to avoid introducing a leg-length discrepancy. Of note, a recent prospective, randomized-controlled study has called into question the efficacy of orthotic insoles, suggesting that routine use of foot orthoses by healthy men provides no significant preventive benefits against overuse injuries, including bursitis 19.
Corticosteroid injections to the retrocalcaneal region may potentially make the adjacent tissues vulnerable as the weak margins are unable to contain the injected fluid. A study of 20 cadaveric Achilles tendons by Pekala et al found that in 100% of the specimens, the ink had extravasated to the adjacent tissues demonstrating that steroid can infiltrate the Achilles tendon from the injected retrocalcaneal bursa. This extravasation of steroid may potentially result in weakening and possibly rupturing of the Achilles tendon 20.
Corticosteroid injection into the retrocalcaneal bursa should be considered as long as the patient has consented regarding the theoretical risk of Achilles tendon rupture, particularly if image guidance is not used.
A study by Goldberg-Stein et al reported that 69% of the 30 patients examined with retrocalcaneal bursitis had greater than 50% reduction in pain score after a steroid/anesthetic lateral fluoroscopically guided retrocalcaneal bursa injection 21.
Microcurrent therapy may serve as another modality for managing heel pain. Using a numerical rating scale for pain, a recent study showed that the addition of microcurrent therapy to traditional treatments significantly reduced pain (pain rating reduction from 8.9 to 2.3) compared with traditional treatments alone (pain rating reduction from 8.2 to 5.9). Improvement may be due to the induction of secondary messengers, such as cyclic adenosine monophosphate (cAMP), which modulates important processes for cellular viability 22.
In retrocalcaneal bursitis patients who fail to respond to conservative treatment (ie. change in footwear, adjustment of the heel), it is possible that these patients may have a secondary pathology. Paša et al. studied 24 patients who did not get adequate relief from such conservative management, and found that 54% of them had a tear in the anterior Achilles tendon, which went undetected on the initial ultrasound examination 23.
Recovery phase
Physical therapy
The patient with retrocalcaneal bursitis should continue to advance the physical therapy program outlined above (see Acute Phase), with a gradual increase of activities. The goal is for the patient to have a full return to his or her previous level of athletic function.
Medical Issues and complications
- Progressive posterior heel and ankle pain, with resultant limping and decreased athletic performance or mobility
- Rupture of the Achilles tendon, either secondary to chronic local inflammation/degeneration or due to non-image guided corticosteroid injection that is inadvertently placed into the Achilles tendon
- Immobilization: Consider partial immobilization in a walking boot or immobilization in a cast for 4-6 weeks if the patient’s symptoms are resistant to the other treatments.
Maintenance phase
The patient should continue with a home exercise program that is developed in conjunction with a physical therapist during the course of treatment.
The patient should be alert for any early signs or symptoms that indicate recurrence of the retrocalcaneal bursitis, so that intervention can be provided as soon as possible, if necessary.
Surgical therapy
Consider surgical intervention for patients with retrocalcaneal bursitis who have significant persistence or progression of symptoms, in spite of the nonsurgical treatment approaches listed above.
An orthopedic surgeon who is experienced with foot and ankle surgery should be consulted for patients in whom conservative therapy has failed and who require surgical intervention for retrocalcaneal bursitis.
Surgical management may include the following:
- Resection of a Haglund deformity (eg, removal of the calcaneal posterosuperior prominence through an ostectomy). Two surgical approaches have been described: a tendon-splitting approach and a lateral approach. A recent study showed that patients who underwent the tendon-splitting approach returned to normal function quicker than patients undergoing the lateral approach 24.
- Excision of the painful bursa(e)
- Debridement of the Achilles tendon insertion
- Repair of an Achilles tendon rupture or avulsion
- Outpatient endoscopic removal of the inflamed bursal tissue and resection of the prominent bone 25.
A recently published review of the medical literature concluded that successful outcome of surgery for chronic retrocalcaneal bursitis is dependent on resecting an adequate amount of bone during the surgical treatment. The researchers also felt that the published evidence suggested (at least to some degree), that endoscopic surgery may have better outcomes than open surgical techniques in the treatment of retrocalcaneal bursitis 26.
- Teebagy AK. Leg and ankle. In: Steinberg GG, Akins CM, Baran DT, eds. Orthopaedics in Primary Care. 3rd ed. Baltimore, Md: Lippincott Williams & Wilkins; 1999. 241-7.[↩]
- Alfredson H, Spang C. Clinical presentation and surgical management of chronic Achilles tendon disorders – A retrospective observation on a set of consecutive patients being operated by the same orthopedic surgeon. Foot Ankle Surg. 2017 Jun 12.[↩]
- Retrocalcaneal bursitis. https://emedicine.medscape.com/article/86297-overview[↩]
- Brinker MR, Miller MD. The adult foot. Fundamentals of Orthopaedics. Philadelphia, Pa: WB Saunders Co; 1999. 342-63.[↩]
- Reule CA, Alt WW, Lohrer H, Hochwald H. Spatial orientation of the subtalar joint axis is different in subjects with and without Achilles tendon disorders. Br J Sports Med. Oct 2011. 45(13):1029-34.[↩]
- Chu NK, Lew HL, Chen CP. Ultrasound-guided injection treatment of retrocalcaneal bursitis. Am J Phys Med Rehabil. 2012 Jul. 91(7):635-7.[↩]
- Thomas JL, Christensen JC, Kravitz SR, Mendicino RW, Schuberth JM, Vanore JV, et al. The diagnosis and treatment of heel pain: a clinical practice guideline-revision 2010. J Foot Ankle Surg. 2010 May-Jun. 49(3 Suppl):S1-19.[↩]
- Lohrer H, Raabe T, Nauck T, Arentz S. Minimally invasive retrocalcaneal bursa pressure measurement: development and pilot application. Arch Orthop Trauma Surg. May 2011. 131(5):719-23.[↩]
- van Sterkenburg MN, Muller B, Maas M, Sierevelt IN, van Dijk CN. Appearance of the weight-bearing lateral radiograph in retrocalcaneal bursitis. Acta Orthop. 2010 Jun. 81(3):387-90.[↩]
- van Sterkenburg MN, Muller B, Maas M, Sierevelt IN, van Dijk CN. Appearance of the weight-bearing lateral radiograph in retrocalcaneal bursitis. Acta Orthop. Jun 2010. 81(3):387-90.[↩]
- Ridley LJ, Han J, Ridley WE, Xiang H. Cockscomb appearance: Retrocalcaneal bursitis. J Med Imaging Radiat Oncol. 2018 Oct. 62 Suppl 1:127.[↩]
- Wiegerinck JI, Zwiers R, van Sterkenburg MN, Maas MM, van Dijk CN. The appearance of the pre-Achilles fat pad after endoscopic calcaneoplasty. Knee Surg Sports Traumatol Arthrosc. 2014 Mar 1.[↩]
- Chang CD, Wu JS. MR Imaging Findings in Heel Pain. Magn Reson Imaging Clin N Am. 2017 Feb. 25 (1):79-93.[↩]
- Van der Wall H, Lee A, Magee M, Frater C, Wijesinghe H, Kannangara S. Radionuclide bone scintigraphy in sports injuries. Semin Nucl Med. Jan 2010. 40(1):16-30.[↩]
- Blankstein A, Cohen I, Diamant L, et al. Achilles tendon pain and related pathologies: diagnosis by ultrasonography. Isr Med Assoc J. 2001 Aug. 3(8):575-8.[↩]
- Reiter M, Ulreich N, Dirisamer A, Tscholakoff D, Bucek RA. [Extended field-of-view sonography in Achilles tendon disease: a comparison with MR imaging]. Rofo. 2004 May. 176(5):704-8.[↩]
- Sofka CM, Adler RS, Positano R, Pavlov H, Luchs JS. Haglund’s syndrome: diagnosis and treatment using sonography. HSS J. 2006 Feb. 2(1):27-9.[↩]
- Hugate R, Pennypacker J, Saunders M, Juliano P. The effects of intratendinous and retrocalcaneal intrabursal injections of corticosteroid on the biomechanical properties of rabbit Achilles tendons. J Bone Joint Surg Am. 2004 Apr. 86-A(4):794-801.[↩][↩]
- Mattila VM, Sillanpää PJ, Salo T, Laine HJ, Mäenpää H, Pihlajamäki H. Can orthotic insoles prevent lower limb overuse injuries? A randomized-controlled trial of 228 subjects. Scand J Med Sci Sports. Dec 2011. 21(6):804-8.[↩]
- Pękala PA, Henry BM, Pękala JR, Piska K, Tomaszewski KA. The Achilles tendon and the retrocalcaneal bursa: An anatomical and radiological study. Bone Joint Res. 2017 Jul. 6 (7):446-451.[↩]
- Goldberg-Stein S, Berko N, Thornhill B, Elsinger E, Walter E, Catanese D, et al. Fluoroscopically guided retrocalcaneal bursa steroid injection: description of the technique and pilot study of short-term patient outcomes. Skeletal Radiol. 2016 Aug. 45 (8):1107-12.[↩]
- Aliyev R, Muslimov Q, Geiger G. Results of conservative treatment of achillodynia with application micro-current therapy. Georgian Med News. Oct 2010. (187):35-42.[↩]
- Paša L, Kužma J, Herůfek R, Prokeš J, Šprláková-Puková A. [Arthroscopic Treatment of Chronic Retrocalcaneal Bursitis – Endoscopic Calcaneoplasty]. Acta Chir Orthop Traumatol Cech. 2018. 85 (3):209-215.[↩]
- Anderson JA, Suero E, O’Loughlin PF, Kennedy JG. Surgery for retrocalcaneal bursitis: a tendon-splitting versus a lateral approach. Clin Orthop Relat Res. 2008 Jul. 466(7):1678-82.[↩]
- Ortmann FW, McBryde AM. Endoscopic bony and soft-tissue decompression of the retrocalcaneal space for the treatment of Haglund deformity and retrocalcaneal bursitis. Foot Ankle Int. 2007 Feb. 28(2):149-53.[↩]
- Wiegerinck JI, Kok AC, van Dijk CN. Surgical treatment of chronic retrocalcaneal bursitis. Arthroscopy. 2012 Feb. 28(2):283-93.[↩]