Scapula fracture
Scapula fracture also known as broken shoulder blade represent less than 1% of all broken bones and many of them can be treated without surgery. Scapula is a triangular-shaped bone that is protected by a complex system of surrounding muscles (see Figure 1). Scapula fractures can result from high-energy, blunt trauma injuries, such as those experienced in a motorcycle or motor vehicle collision or falling from a significant height. Because of the high-energy nature of scapular fractures, 80% to 95% are associated with additional traumatic injuries 1. On average, patients with fractures of the scapula have four other injuries 2. In particular, these patients are more likely to have upper extremity, thoracic, spinal cord and pelvic ring injuries than trauma patients without scapular fractures, even after adjustment for injury severity 3. Potentially life-threatening associated injuries may include pneumothorax, pulmonary contusion, arterial injury, closed head injury, and splenic or liver lacerations 2 with the associated mortality rate reaching nearly 15% 4. Brachial plexus injury occurs in 5% to 13% of cases 5 and serves as an important prognostic indicator of ultimate clinical outcome. As a result, diagnosis and treatment of scapular injuries may be delayed or suboptimal. Long-term functional impairment may occur.
One or more parts of the scapula may be fractured.
- Scapular body (50% to 60% of patients)
- Scapular neck (25% of patients)
- Glenoid cavity (glenoid rim and fossa) (10% of scapula fractures)
- Acromion (8% of scapula fractures)
- Coracoid (7% of scapula fractures)
Patients with scapular fractures present with the ipsilateral upper extremity adducted against the body and protected from movement. Typical physical examination findings may include swelling, ecchymosis, crepitus, and tenderness about the shoulder. Range of motion of the shoulder is limited, particularly with abduction. A meticulous neurovascular examination is necessary in order to evaluate for injury to the ipsilateral brachial plexus and/or vascular structures.
Most scapula fractures can be managed effectively with closed treatment. Some injuries with significant displacement have poor long-term outcomes for the shoulder and the upper extremity as a whole if treated with closed techniques.
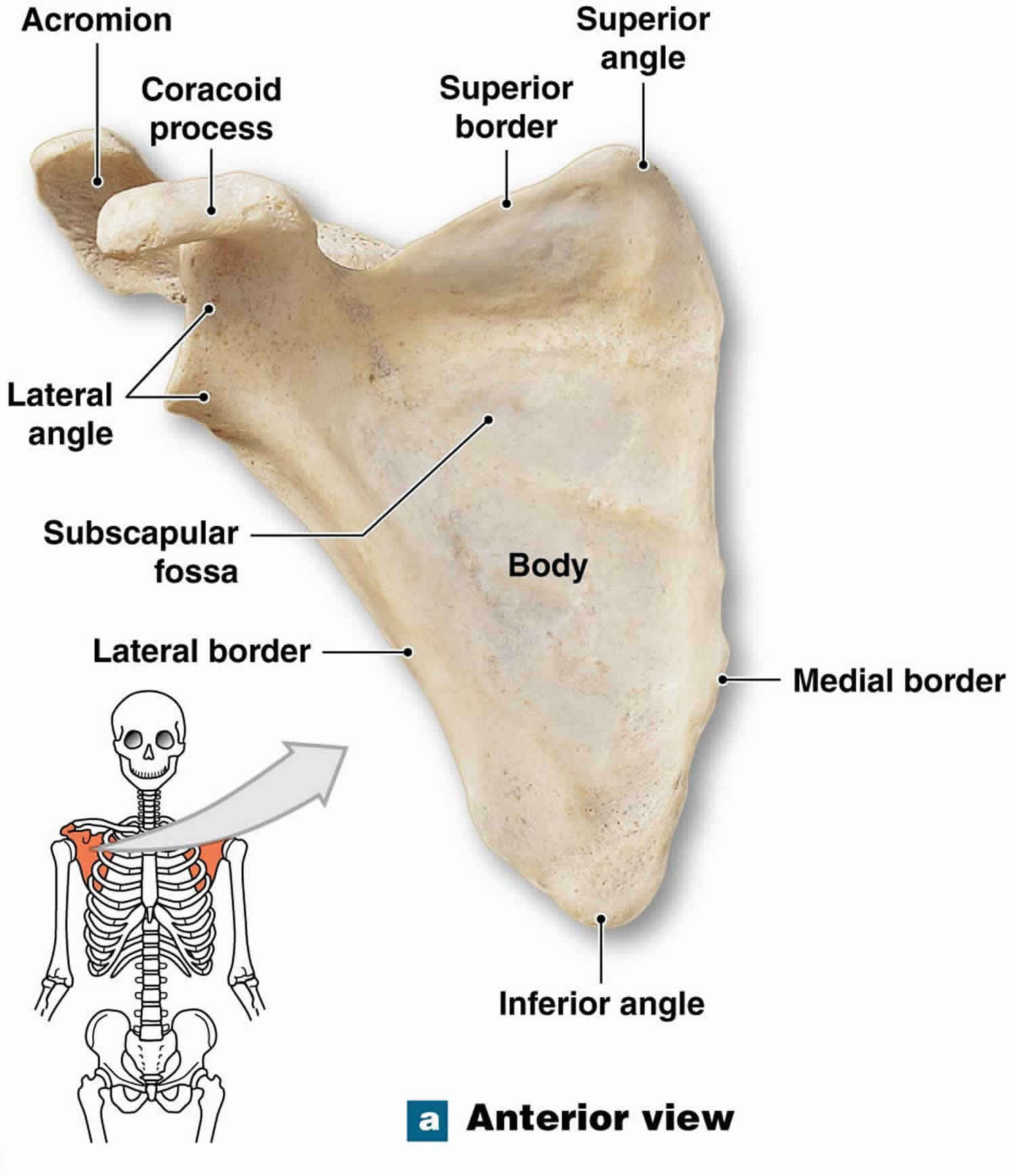
Scapula anatomy
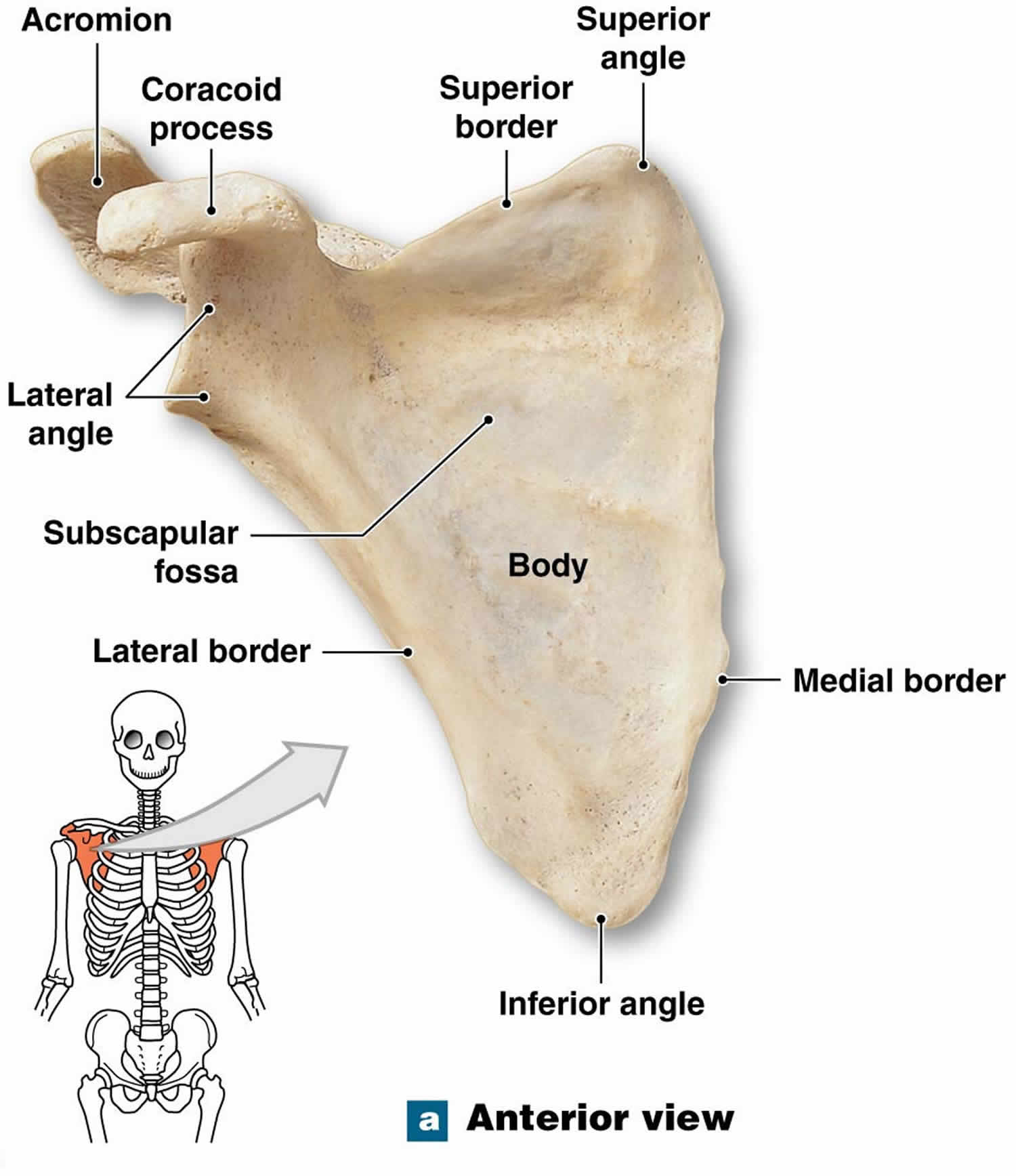
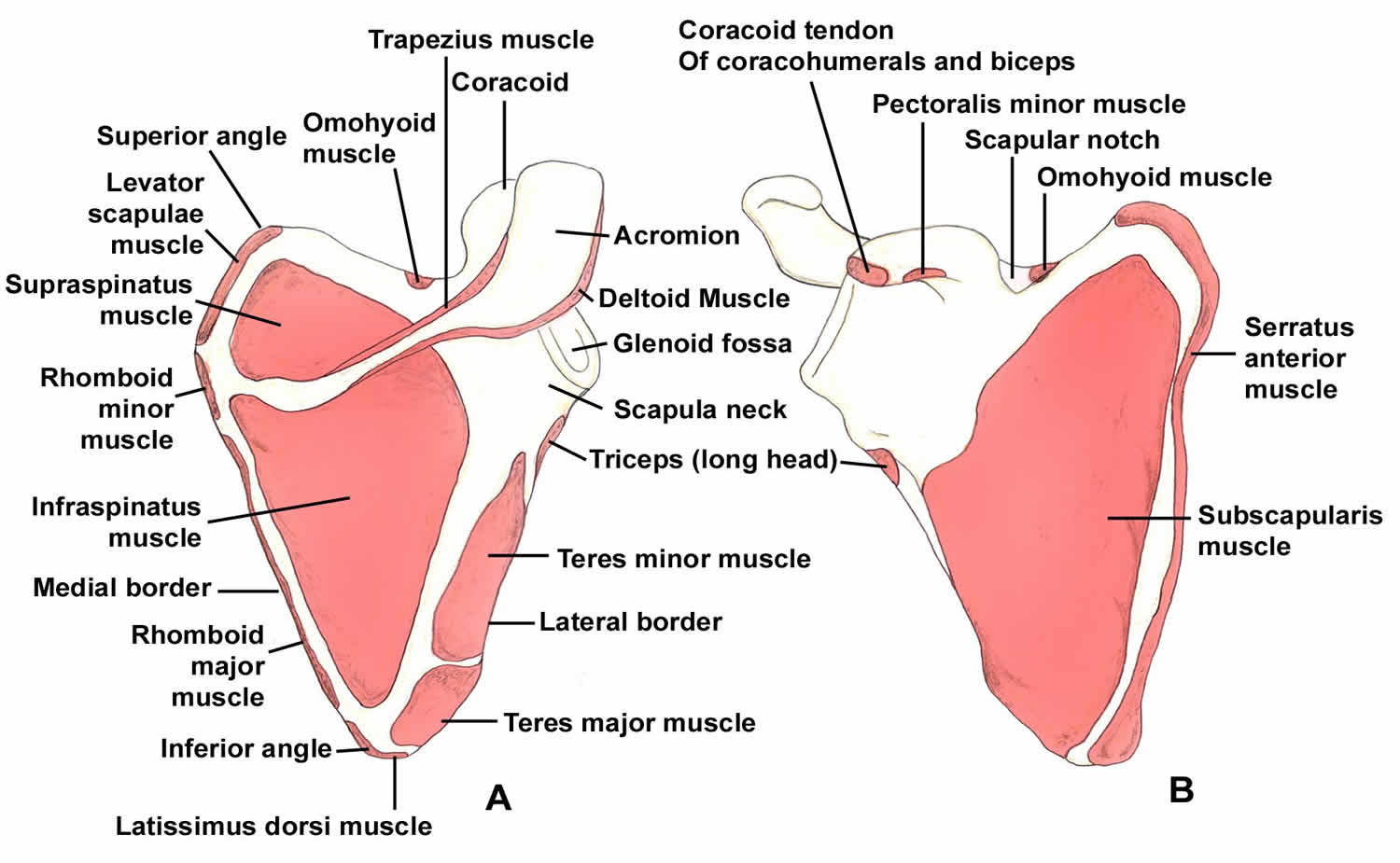
The scapula serves as the attachment site for 18 muscles, which link it to the thorax, spine, and upper extremity. The subscapularis covers the anterior surface, and the serratus anterior attaches to the inferior angle along the anterior medial border. The supraspinatus and the infraspinatus lie on the posterior border of the scapula. Overlying them is the trapezius, which inserts on the spine and the clavicle. The deltoid originates from the scapular spine, acromion, and anterior clavicle. Many other muscles attach to the scapular margins.
The coracoid process projects from the superior border of the scapula. The coracobrachialis and the short head of the biceps originate from the coracoid, and the pectoralis minor inserts on the coracoid. The brachial plexus and the axillary artery run posterior to the pectoralis minor tendon. The scapular notch lies just medial to the coracoid base and is covered by the transverse scapular ligament. The suprascapular nerve runs under the ligament, and the suprascapular artery passes over it.
The acromion is the lateral projection from the spine of the scapula. The spinoglenoid notch is the gap between the acromion and the glenoid neck of the scapula. The suprascapular nerve and vessels pass through the notch en route to the infraspinatus.
Figure 1. Scapula anatomy
Figure 2. Scapula anatomy showing muscle origin and insertion
Figure 3. Shoulder joint
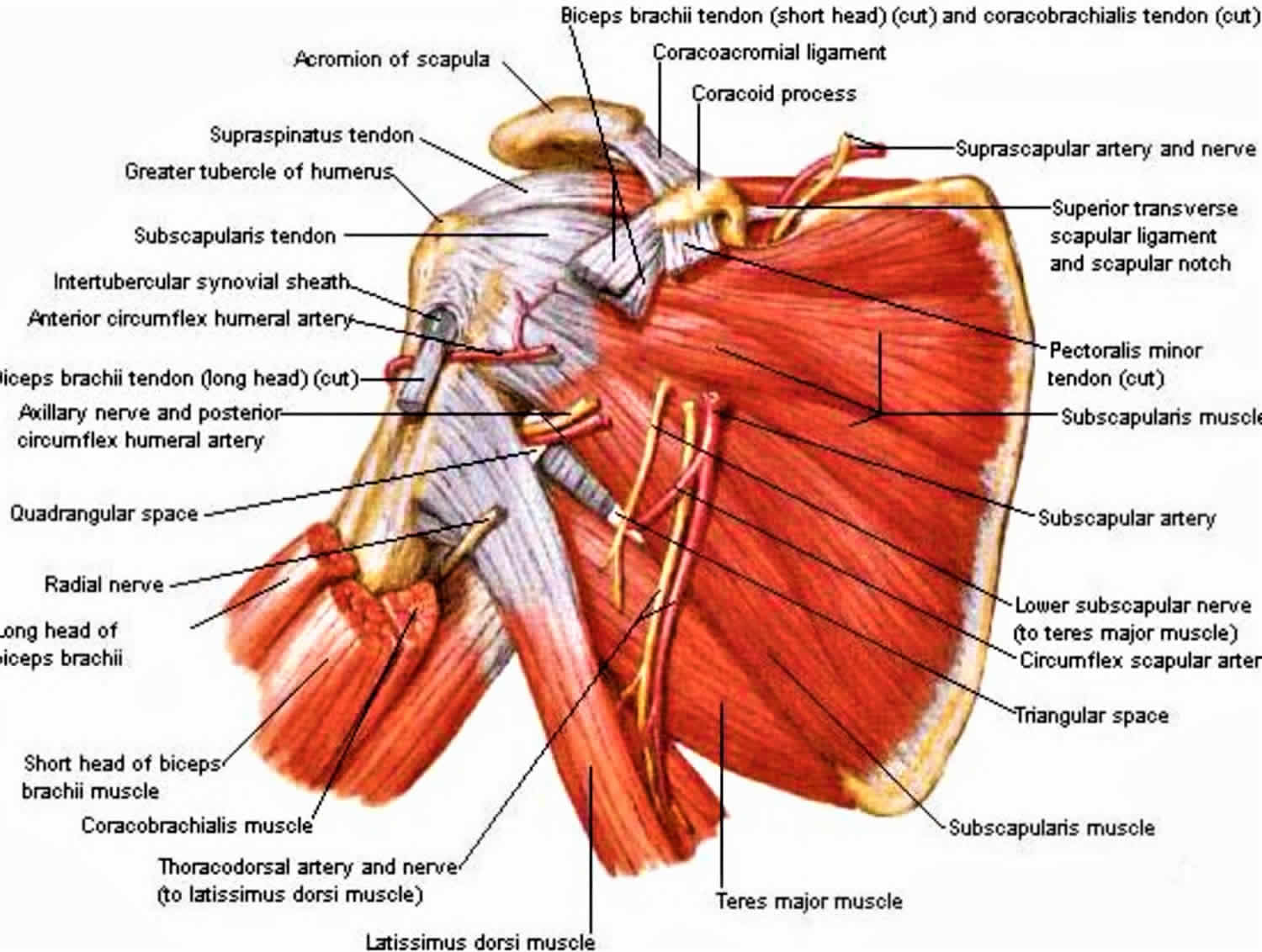
Figure 4. Shoulder joint rotator cuff muscles
Scapula fracture classification
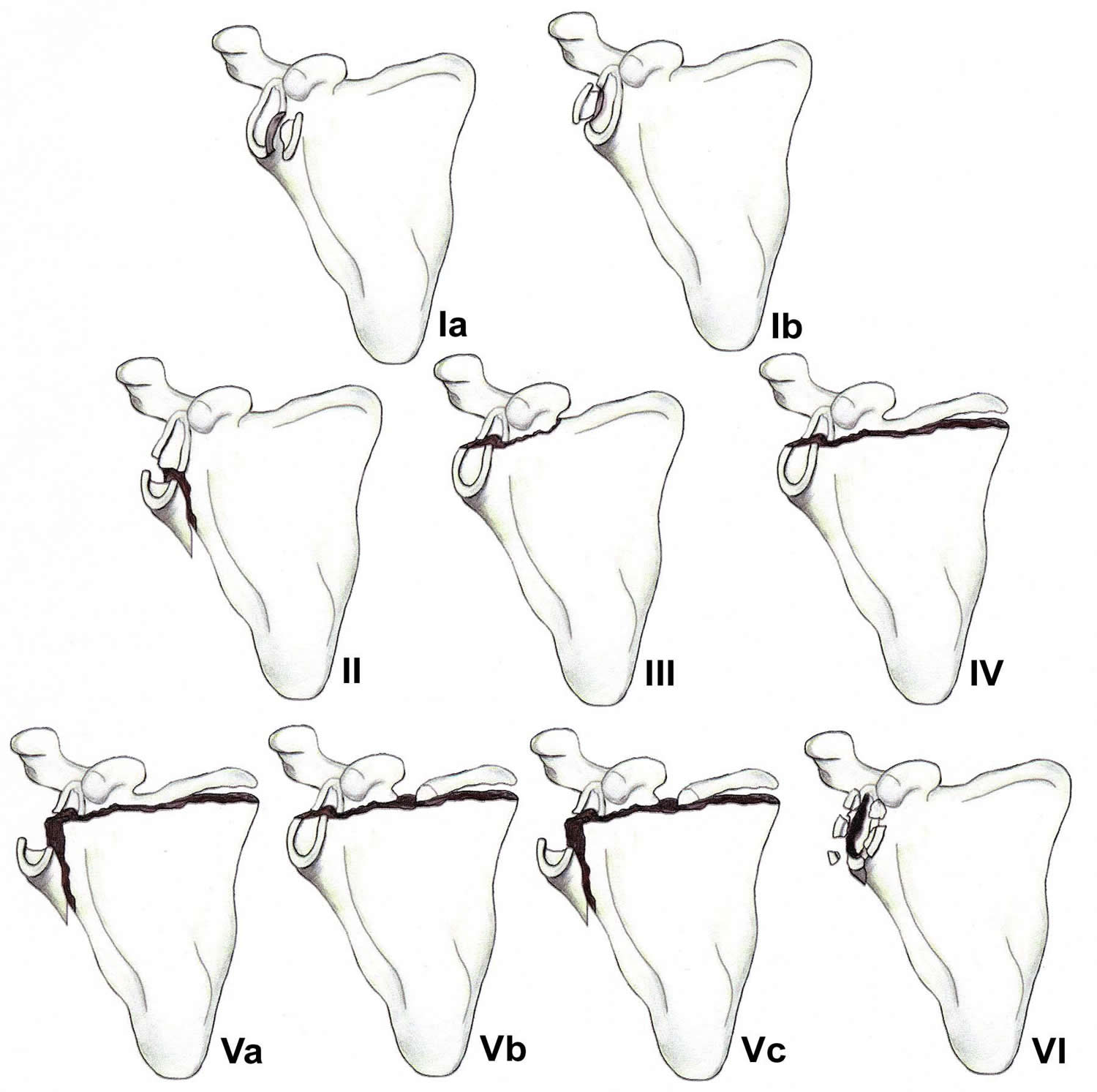
Fractures involving the glenoid cavity may be classified into the following types (see Figure 5 below):
- Type IA – Anterior rim fracture
- Type IB – Posterior rim fracture
- Type II – Fracture line through the glenoid fossa exiting at the lateral border of the scapula
- Type III – Fracture line through the glenoid fossa exiting at the superior border of the scapula
- Type IV – Fracture line through the glenoid fossa exiting at the medial border of the scapula
- Type VA – Combination of types II and IV
- Type VB – Combination of types III and IV
- Type VC – Combination of types II, III, and IV
- Type VI – Comminuted fracture
Fractures of the glenoid neck may be classified into the following two types:
- Type I – Includes all nondisplaced or minimally displaced fractures
- Type II – Includes all significantly displaced fractures (translational displacement equal to or greater than 1 cm or angulatory displacement equal to or greater than 40°)
Bartonicek et al described a clinically oriented classification of scapular body fractures based on involvement of the pillars of the scapular body as seen on 3D CT, as follows 6:
- Fracture of spinal pillar
- Fracture of lateral pillar (two-part, three-part, comminuted)
- Fracture of both pillars (medial, central)
In 2013, the AO Foundation and Orthopaedic Trauma Association published a comprehensive and reliable scapula classification involving glenoid fracture patterns 7.
Fractures of the glenoid rim occur when the humeral head is driven against the glenoid margin. Surgical management is indicated if the fracture results in persistent subluxation of the humeral head, defined as failure of the humeral head to lie concentrically within the glenoid fossa, or if the reduction is unstable. DePalma stated that instability can be anticipated if the fracture is displaced 10 mm or more and if at least one fourth of the anterior aspect of the glenoid cavity or one third of the posterior aspect of the glenoid cavity is involved 8.
Fractures of the glenoid fossa occur when a laterally applied force drives the humeral head directly into the glenoid cavity. Soslowsky et al 9 found the maximum depth of glenoid articular cartilage to measure 5 mm. Consequently, with displacement more than 5 mm, subchondral bone is exposed, making posttraumatic arthritis more likely.
Figure 5. Scapula glenoid cavity fracture classification
Footnote: Classification of glenoid cavity fractures: IA – Anterior rim fracture; IB – Posterior rim fracture; II – Fracture line through the glenoid fossa exiting at the lateral border of the scapula; III – Fracture line through the glenoid fossa exiting at the superior border of the scapula; IV – Fracture line through the glenoid fossa exiting at the medial border of the scapula; VA – Combination of types II and IV; VB – Combination of types III and IV; VC – Combination of types II, III, and IV; VI – Comminuted fracture
Scapula fracture causes
Typically, scapula fractures result from high-energy trauma 10. Direct forces are most common, but indirect mechanisms can also be responsible. An example of an indirect force is a fall on an outstretched arm that causes the humeral head to impact on the glenoid cavity.
Scapula fracture has been reported as a potential complication of reverse total shoulder arthroplasty for rotator cuff tear arthropathy 11.
Scapula fracture symptoms
Most patients with scapula fractures present after high-energy trauma. Associated injuries are common and may delay the diagnosis.
The most common symptoms of a scapula fracture include:
- Extreme pain when you move the arm
- Swelling around the back of the shoulder
- Scrapes around the affected area.
Associated injury patterns commonly involve the ipsilateral upper extremity and thorax. Frequencies of associated injuries are as follows:
- Rib fractures – 25-45%
- Pulmonary injury (eg, hemopneumothorax or pulmonary contusion) – 15-55%
- Humeral fractures – 12% (5-10% sustain a brachial plexus injury)
- Skull fractures – 25%
- Central neurologic deficits 5%
- Major vascular injury – 11%
- Splenic injury requiring splenectomy – 8%
Typically, physical examination reveals swelling, tenderness, crepitus, and ecchymosis over the scapular region. Perform a careful neurovascular examination to rule out arterial injury or brachial plexopathy.
Scapula fracture complications
The most significant complications associated with scapular fractures are those that result from accompanying injuries to adjacent and distant osseous and soft-tissue structures. On average, there are 3.9 additional injuries, with the ipsilateral shoulder girdle, upper extremity, lung, and chest wall being affected most commonly. Pulmonary injuries, such as hemopneumothorax or pulmonary contusion, occur in 15-55% of cases. Cerebral contusions occur in 10-40% of cases, with central neurologic deficits in 5% of cases. Splenectomy is required in 8% of patients, and the mortality is 2%.
Complications related to the scapular fractures themselves are relatively uncommon. Nonunion is rare. Malunion can occur in a variety of forms, depending on the particular fracture type. Malunion of a scapular body fracture generally is well tolerated, though painful scapulothoracic crepitus has been described. Fractures of the glenoid cavity can result in symptomatic glenohumeral degenerative joint disease and instability. Angulated fractures of the glenoid neck can result in shoulder instability. Fractures of the glenoid neck with translational displacement can lead to altered mechanics of the surrounding soft tissues, giving rise to glenohumeral pain and dysfunction.
Scapula fracture diagnosis
To determine appropriate treatment, your doctor will evaluate the position and posture of your shoulder. Because other injuries are often present with scapula fractures, your doctor will look for additional injuries. He or she will also treat any soft-tissue damage (abrasions, open wounds, and muscular trauma). A detailed physical examination may not be possible if you have other severe injuries.
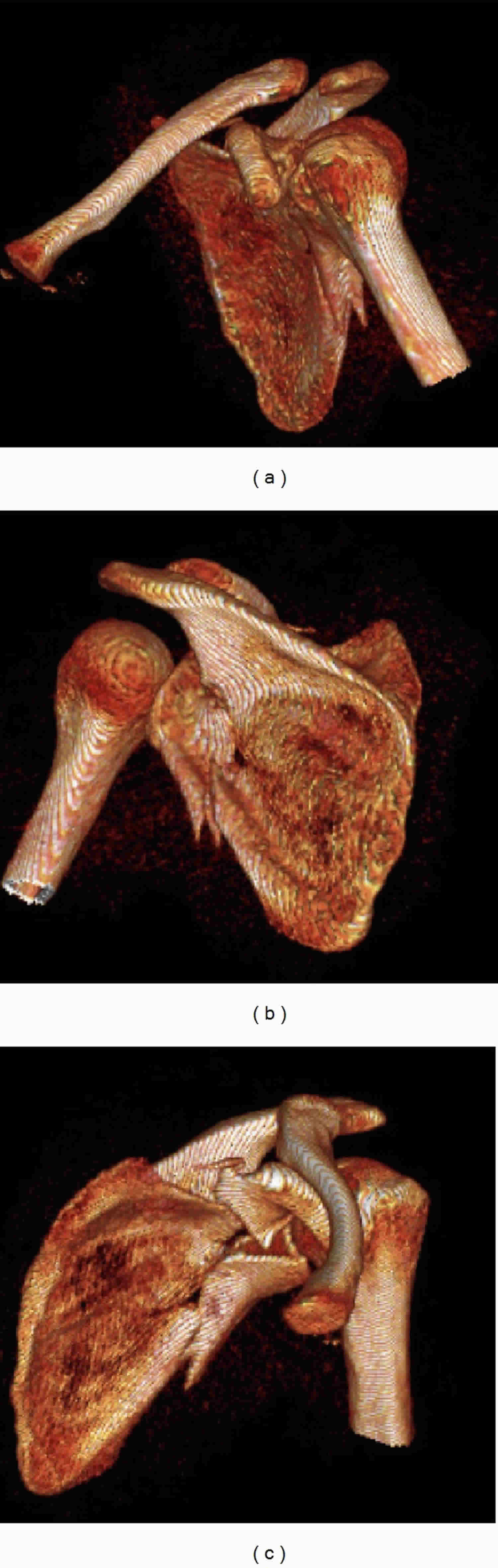
Your doctor may also order imaging tests of your shoulder and chest to determine the extent of injury to the scapula. X-rays provide clear images of dense structures like bone. Your doctor may also order a computed tomography (CT) scan to provide a more detailed image.
Electromyography (EMG) can be performed 3 weeks after injury in patients with a scapula fracture and brachial plexus injury. EMG is useful for assessing the extent of the injury and potential for recovery, if any.
Cervical myelography can be performed at 6 weeks in patients with a neurologic deficit due to a scapular injury.
Figure 6. Scapula fracture CT scan (three-dimensional reconstructions of the left shoulder CT scan.)
[Source 12 ]Scapula fracture treatment
Most scapula fractures can be managed effectively with closed treatment. Some injuries with significant displacement have poor long-term outcomes for the shoulder and the upper extremity as a whole if treated with closed techniques.
Because scapula fractures often are associated with other injuries, which are sometimes life-threatening, surgery should be delayed until the patient is medically stabilized. Absolute contraindications for surgery are few. In the case of a major vascular injury, such as an axillary or brachial artery tear, repair of the vessel should be carried out first, followed by fracture fixation.
Recognizing the exact indications for operative treatment of scapula fractures is a major issue for the future. The authors have presented guidelines for when to consider surgery. However, more data are needed to further define and support these recommendations. As surgical techniques advance, the indications for surgical intervention may expand.
Nonsurgical treatment
Nonsurgical treatment with a simple sling works for most fractures of the scapula. The sling holds your shoulder in place while the bone heals. Your doctor may want you to start moving your shoulder within the first week after the injury to minimize the risk of shoulder and elbow stiffness. The sling is discontinued as your pain improves. Passive stretching exercises should be continued until complete shoulder motion returns. This may take 6 months to 1 year.
Most scapular fractures heal completely by 6 weeks, and all external support is discontinued at this time. Progressive use of the upper extremity is encouraged. Continue range-of-motion (ROM) exercises until full shoulder mobility is recovered. As motion improves, add progressive strengthening exercises. Full functional recovery takes several months. Ultimately, the prognosis for these fractures is excellent.
Surgical treatment
Certain types of scapular fractures may need surgery:
- Fractures of the glenoid articular surface in which bone has moved out of place (displaced)
- Fractures of the neck of the scapula with a lot of angulation
- Fractures of the acromion process that cause the arm bone to hit against it (impingement syndrome)
During this operation, the bone fragments are first repositioned (reduced) in their normal alignment, and then held together by attaching metal plates with special screws to the outer surface of the bone.
Approximately 50% of scapula fractures involve the scapular body and spine. Avulsion fractures caused by indirect forces and injuries caused by direct trauma have been described 13. The latter may be severely comminuted and displaced. Despite sporadic reports describing operative management, there seems to be little enthusiasm for surgical treatment, for the following two reasons:
- There is little substantial bone stock for internal fixation, aside from the scapular spine and lateral scapular border
- These fractures seem to heal reliably with a good functional result without surgical treatment
If painful scapulothoracic impingement occurs at a later date, bone prominences over the ventral scapular surface can be removed surgically.
Significantly displaced fractures of glenoid cavity (rim and fossa)
Fewer than 10% of glenoid cavity fractures are significantly displaced.
Kavanagh et al 14 reported on open reduction and internal fixation (ORIF) of glenoid fossa fractures in which displacement ranged from 4 to 8 mm. They found ORIF to be a useful and safe technique for the treatment of selected displaced fractures of the glenoid fossa. On the basis of these and other studies, it seems reasonable to conclude that an articular stepoff of 5 mm should warrant consideration for ORIF and that a 10-mm stepoff is a definite indication for surgery.
Other indications for surgical management of these fractures include the following:
- Glenoid fossa fractures that result in significant displacement of the humeral head such that it fails to lie in the center of the glenoid cavity, thereby resulting in glenohumeral instability
- Fractures of the glenoid fossa with such severe separation of the fracture fragments that nonunion is likely to occur
Significantly displaced fractures of glenoid neck
Glenoid neck fractures (see the image below) that cause significant translational or angulatory displacement of the glenoid fragment can interfere with normal shoulder mechanics or cause glenohumeral instability. Nordqvist et al 15 evaluated 37 glenoid neck fractures treated nonoperatively and found the functional results at 10- to 20-year follow-up to be fair or poor in 32% of cases. Hardegger et al 16 noted that displaced glenoid neck fractures result in a functional imbalance because the relation of the glenohumeral joint to the acromion and nearby muscle origins is altered.
Overall, there is support in the literature for the view that surgery should be considered for fractures with translational displacement greater than or equal to 1 cm and/or angulatory displacement greater than or equal to 40° in either the transverse or coronal plane.
Double disruptions of superior shoulder suspensory complex
The superior shoulder suspensory complex is a bone/soft-tissue ring at the end of a superior and inferior bony strut. The ring consists of the glenoid process, the coracoid process, the coracoclavicular ligaments, the distal clavicle, the acromioclavicular (AC) joint, and the acromial process. The superior strut is the middle third of the clavicle. The inferior strut is the lateral scapular body and spine.
Traumatic disruptions of one of the components of the superior shoulder suspensory complex are common. If the force is sufficient, the ring may fail in two or more places (double disruption), a situation in which significant displacement at one or both of the individual sites and of the superior shoulder suspensory complex as a whole frequently occurs. Similarly, a disruption of one portion of the ring, combined with a fracture of one of the struts or fractures of both struts, also creates a potentially unstable anatomic situation.
Adverse consequences include delayed union, malunion, and nonunion. Subacromial impingement, decreased strength and muscle fatigue, discomfort due to altered shoulder mechanics, neurovascular compromise due to a drooping shoulder, and glenohumeral degenerative joint disease also can occur.
If unacceptable displacement is present, surgical reduction and stabilization at the injury sites is necessary. Frequently, operative management of one of the injury sites satisfactorily reduces and stabilizes the second disruption indirectly 17.
Herscovici et al 18 reported results in nine patients with ipsilateral clavicular and glenoid neck fractures. Seven patients were treated surgically with plate fixation of the clavicular fracture and achieved excellent results. Two patients were treated without surgery and were found to have decreased ROM, as well as drooping of the involved shoulder. The authors strongly recommended ORIF of the clavicle to prevent glenoid neck malunion 18.
Combined fractures of the distal clavicle and the superior aspect of the glenoid cavity is another potentially unstable situation. Each disruption may lead to displacement at the other fracture site. If displacement of the clavicular fracture site is unacceptable, surgical reduction and stabilization is indicated, usually with a Kirschner-wire (K-wire) tension-band fixation construct. Because the proximal clavicular segment is attached to the superior glenoid-coracoid process fragment by means of the coracoclavicular ligaments, this may indirectly reduce and stabilize the glenoid cavity fracture satisfactorily. If not, the glenoid fracture may also require surgical management using the surgical techniques described.
Fracture of the coracoid or the acromion process with a second disruption of the superior shoulder suspensory complex is another potentially unstable situation. If displacement at either or both sites is unacceptable, surgical management is indicated. For double disruptions consisting of both an acromion and a coracoid fracture, ORIF of the acromion may be all that is required
Postoperative care
Postoperative management partially depends on the degree of stability achieved at surgery. Complete immobilization in a sling and swathe is used for the first 24-48 hours. After that, progressive ROM exercises and functional use of the shoulder out of the sling (within clearly defined limits) are initiated if fixation is satisfactory. If surgical fixation was not rigid, immobilization in a sling and swathe, abduction brace, or overhead olecranon pin traction may be required for 7-14 days.
Radiographs are taken every 2 weeks to ensure maintained reduction. By 6 weeks, healing usually is sufficient to permit discontinuance of the sling and to allow progressive functional use of the extremity.
Physical therapy is continued until ROM and strength are maximized. Initial emphasis is on regaining ROM. As ROM progresses, strengthening exercises are added. Light use of the shoulder is encouraged through postoperative week 12. Heavy physical use of the shoulder, such as athletic activity, is prohibited for 4-6 months. Patients are encouraged to work diligently on their rehabilitation programs, as final motion and strength may not be achieved for 6 months to 1 year.
Long-term monitoring
After discharge from the hospital, patients should be seen for follow-up every 2 weeks for the first 6 weeks. Radiographs are taken to ensure maintained reduction. Evaluate the patient’s ROM and update his/her rehabilitation program as needed. Patients should be seen at 12 weeks for evaluation of motion and progression of functional use of the shoulder. Final motion and strength may not be achieved until 6 months to 1 year.
Scapula fracture prognosis
Because of the low incidence of scapula fractures, little in the way of outcome data exists. Hardegger et al 16 reported 79% good-to-excellent results associated with five displaced glenoid neck fractures treated surgically (6.5-year follow-up). Kavanaugh et al 14 at the Mayo Clinic reviewed 10 displaced glenoid cavity fractures treated with open reduction and internal fixation (ORIF) and found this to be a useful and safe technique that can restore excellent function of the shoulder.
Nonoperative treatment can sometimes result in malunion, leading to poor range of motion (ROM), chronic pain, and poor cosmesis. Cole et al 19 report that surgical reconstruction of malunited scapula neck or body fractures can yield good functional and cosmetic outcomes.
Until more data are available, it is reasonable to predict a good-to-excellent functional result if surgical management restores normal or near-normal anatomy, articular congruity, and glenohumeral stability; if surgery provides secure fixation; and if a well-structured and intensive rehabilitation program is implemented 20.
- Ideberg R, Grevsten S, Larsson S. Epidemiology of scapular fractures: incidence and classification of 338 fractures. Acta Orthopaedica Scandinavica. 1995;66(5):395–397.[↩]
- Thompson DA, Flynn TC, Miller PW, Fischer RP. The significance of scapular fractures. Journal of Trauma. 1985;25(10):974–977.[↩][↩]
- Baldwin KD, Ohman-Strickland P, Mehta S, Hume E. Scapula fractures: a marker for concomitant injury? A retrospective review of data in the national trauma database. Journal of Trauma. 2008;65(2):430–435.[↩]
- Armstrong CP, Van der Spuy J. The fractured scapula: importance and management based on a series of 62 patients. Injury. 1984;15(5):324–329.[↩]
- McGahan JP, Rab GT, Dublin A. Fractures of the scapula. Journal of Trauma. 1980;20(10):880–883.[↩]
- Bartonicek J, Klika D, Tucek M. Classification of scapular body fractures. Rozhl Chir. 2018 Winter. 97 (2):67-76.[↩]
- Gilbert F, Eden L, Meffert R, Konietschke F, Lotz J, Bauer L, et al. Intra- and interobserver reliability of glenoid fracture classifications by Ideberg, Euler and AO. BMC Musculoskelet Disord. 2018 Mar 27. 19 (1):89.[↩]
- DePalma AF. Surgery of the Shoulder. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 1983.[↩]
- Soslowsky LJ, Flatow EL, Bigliani LU, Mow VC. Articular geometry of the glenohumeral joint. Clin Orthop Relat Res. 1992 Dec. 181-90.[↩]
- Coimbra R, Conroy C, Tominaga GT, Bansal V, Schwartz A. Causes of scapula fractures differ from other shoulder injuries in occupants seriously injured during motor vehicle crashes. Injury. 2010 Feb. 41(2):151-5.[↩]
- Kennon JC, Lu C, McGee-Lawrence ME, Crosby LA. Scapula fracture incidence in reverse total shoulder arthroplasty using screws above or below metaglene central cage: clinical and biomechanical outcomes. J Shoulder Elbow Surg. 2017 Jun. 26 (6):1023-1030.[↩]
- Voleti PB, Namdari S, Mehta S. Fractures of the scapula. Adv Orthop. 2012;2012:903850. doi:10.1155/2012/903850 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3508577[↩]
- Morioka T, Honma T, Ogawa K. Incomplete avulsion fractures of the scapular spine caused by violent muscle contraction. Keio J Med. 2014. 63 (1):13-7.[↩]
- Kavanagh BF, Bradway JK, Cofield RH. Open reduction and internal fixation of displaced intra-articular fractures of the glenoid fossa. J Bone Joint Surg Am. 1993 Apr. 75(4):479-84.[↩][↩]
- Nordqvist A, Petersson C. Fracture of the body, neck, or spine of the scapula. A long-term follow-up study. Clin Orthop Relat Res. 1992 Oct. (283):139-44.[↩]
- Hardegger FH, Simpson LA, Weber BG. The operative treatment of scapular fractures. J Bone Joint Surg Br. 1984 Nov. 66 (5):725-31.[↩][↩]
- Goss TP. Double disruptions of the superior shoulder suspensory complex. J Orthop Trauma. 1993. 7(2):99-106.[↩]
- Herscovici D Jr, Fiennes AG, Allgöwer M, Rüedi TP. The floating shoulder: ipsilateral clavicle and scapular neck fractures. J Bone Joint Surg Br. 1992 May. 74 (3):362-4.[↩][↩]
- Cole PA, Talbot M, Schroder LK, Anavian J. Extra-articular Malunions of the Scapula: A Comparison of Functional Outcome Before and After Reconstruction. J Orthop Trauma. 2011 Nov. 25(11):649-56.[↩]
- Anavian J, Gauger EM, Schroder LK, Wijdicks CA, Cole PA. Surgical and functional outcomes after operative management of complex and displaced intra-articular glenoid fractures. J Bone Joint Surg Am. 2012 Apr 4. 94 (7):645-53.[↩]