What is schizencephaly
Schizencephaly is an extremely rare developmental birth defect characterized by abnormal slits, or clefts, in the cerebral hemispheres of the brain. The defect can be unilateral or bilateral and involves clefts of the cortex associated with thickened cortex adjacent to the clefts (white regions on MRI diagram). Babies with clefts in both hemispheres called bilateral clefts, commonly have developmental delays, delays in speech and language skills, and problems with brain-spinal cord communication. Individuals with clefts in only one hemisphere called unilateral clefts, are often paralyzed on one side of the body, but may have average to near-average intelligence. Individuals with schizencephaly may also have an abnormally small head, cognitive delay and impairment, partial or complete paralysis, or poor muscle tone. Developmental delay, cerebral palsy or seizure onset is the typical presentation. Refractory seizures are often seen in the milder degrees of schizencephaly. Some individuals may have an excessive accumulation of fluid in the brain called hydrocephalus. EMX2 mutations occur in a minority of cases. Most cases appear to have occurred sporadically. Vascular disruptions during fetal brain development have been postulated as a causative factor in some cases.
Schizencephaly is a rare congenital abnormality of the brain that has estimated prevalence of schizencephaly of 1 out of every 64,935 births in the United States and 1 out of every 69,444 in UK 1. Schizencephaly has a prevalence of approximately 1.5 per 100,000 live-born babies as estimated from a review of four million births in California 2. Howe and colleagues reported a combined live birth/stillbirth rate of 1.48 per 100,000 from a population of over 2.5 million in the UK and less than half of those cases were detected antenatally 3.
Treatment generally consists of physical therapy and drugs to prevent seizures. In cases that are complicated by hydrocephalus, a surgically implanted tube, called a shunt, is often used to divert fluid to another area of the body where it can be absorbed.
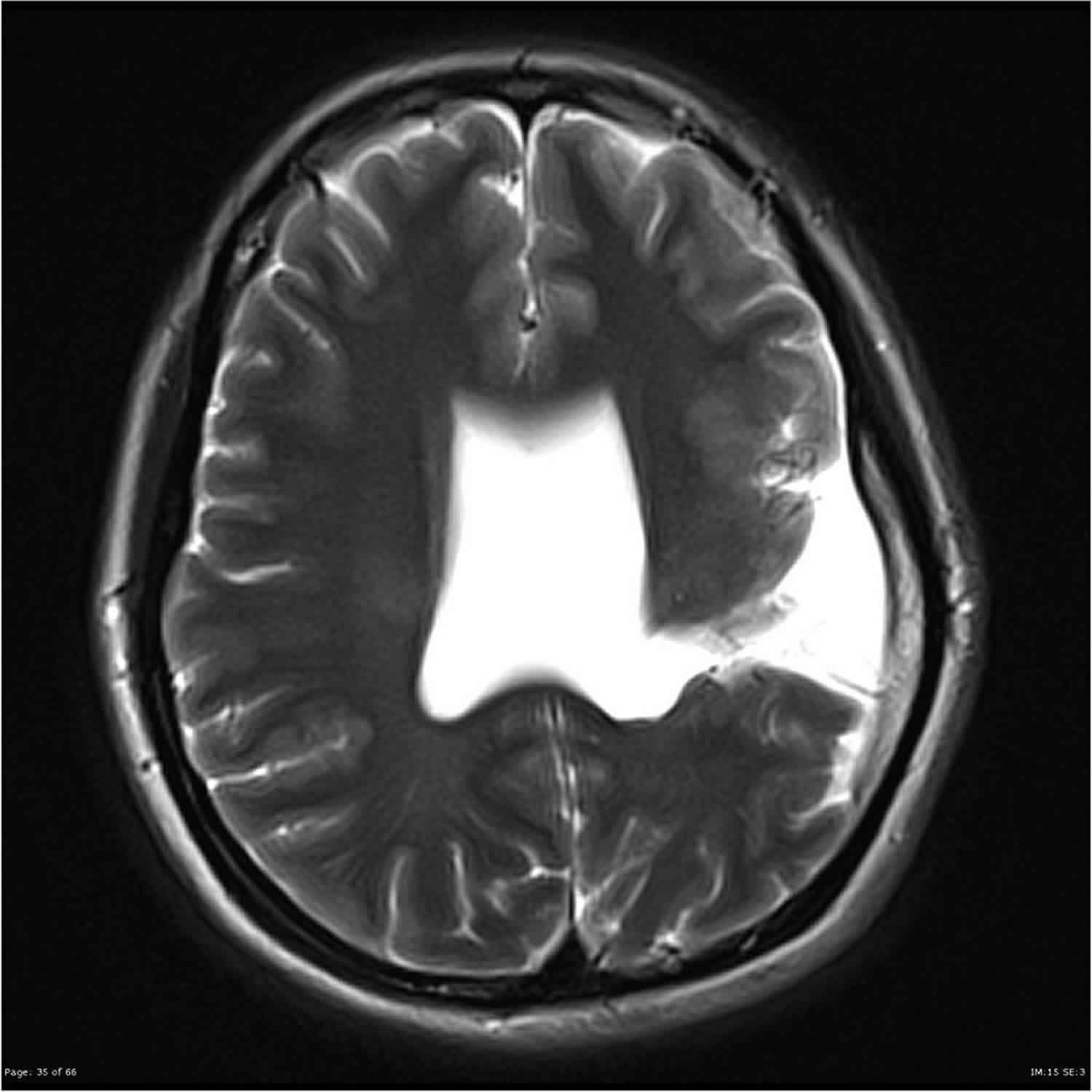
Figure 1. Schizencephaly radiology
Footnote: A number of congenital developmental abnormalities are demonstrated. Most notably, extending from the left lateral ventricle to the posterior cortex of the left frontal lobe is a grey matter lined CSF cleft. The grey matter lining this defect, and seen quite extensively in the perisylvian grey matter, is abnormal consistent with a finely nodular surface and grey white matter junction. Similar abnormal grey matter is seen involving the posterior frontal lobe on the right, without evidence of an associated cleft. The septum pellucidum is absent. The optic apparatus appears normal. The falx is present, and no abnormal fusion across the midline can be identified. The corpus callosum is normally formed. The posterior fossa is unremarkable.
Schizencephaly types
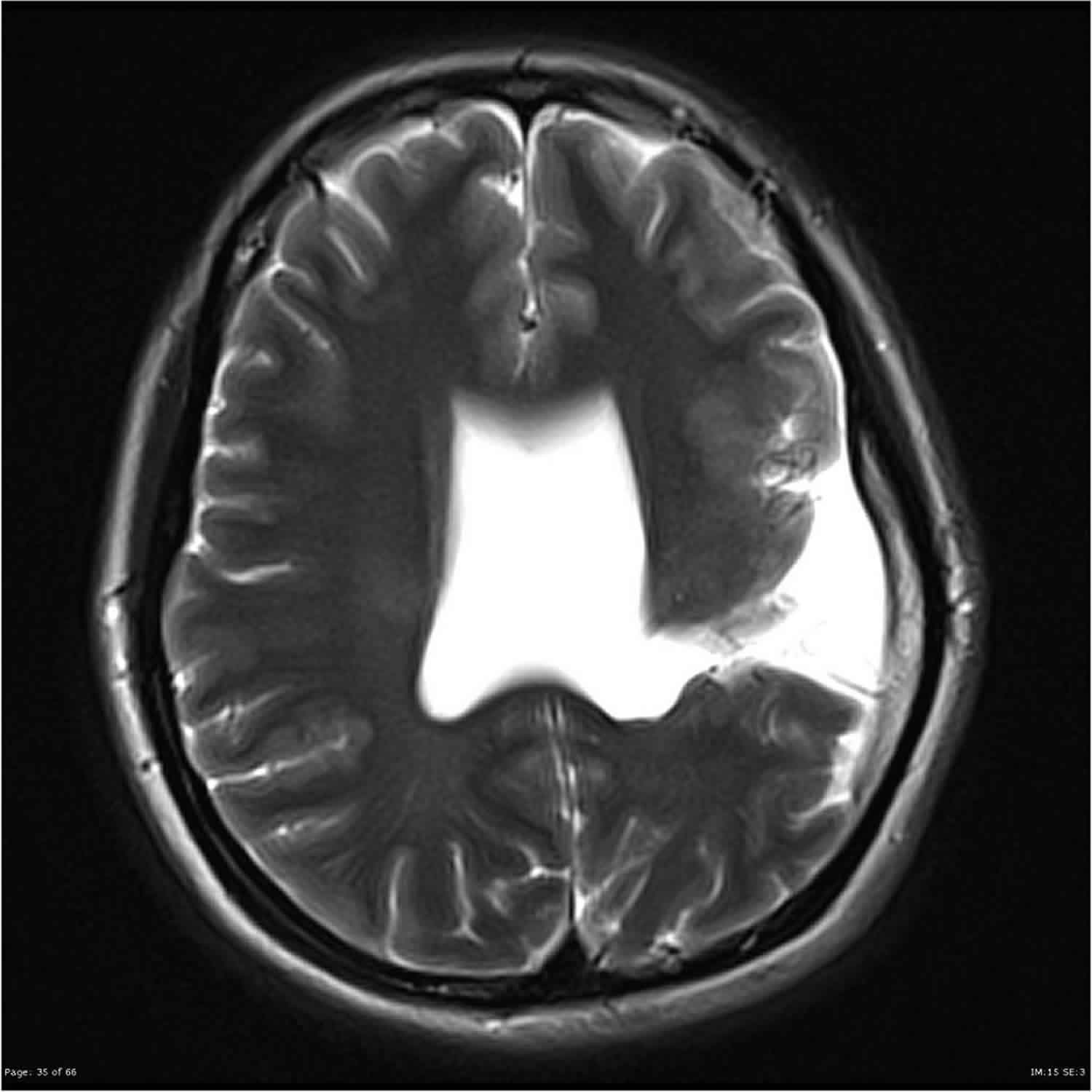
There is a range of opinion about the definition of schizencephaly; specifically, some authorities consider a CSF-containing cleft running from the pial to the ependymal surfaces to be the sine qua non of schizencephaly 4. In contrast, the definition of schizencephaly recently put forward by Naidich et al. 5 includes a trans-mantle column of dysplastic grey matter extending from the ependyma to the pia without a CSF cleft. Those authors reference supportive evidence from the publications of Yakovlev and Wadsworth 6 and specimens housed in the Yakovlev-Haalem collection at the Armed Forces Institute of Pathology, Washington, DC. The differences in nomenclature used by the two groups are summarized in Figure 2.
- Schizencephaly (type 1)—Trans-mantle column of abnormal grey matter but no evidence of a CSF-containing cleft on MR imaging
- Schizencephaly (type 2)—CSF-containing cleft present, abutting lining lips of abnormal grey matter opposed
- Schizencephaly (type 3)—CSF-containing cleft present, non-abutting lining lips of abnormal grey matter.
If two types of schizencephaly are present in the same individual, it is described by the numerically higher category; e.g. if a child has an open and a closed lip cleft, the individual will be classified as having schizencephaly (type 3). Porencephaly, the major differential diagnosis of schizencephaly is distinguished by the lack of abnormal grey matter lining the cleft 7.
Figure 2. Schizencephaly types
Footnote: Classification of the three different types of schizencephaly compared with other nomenclature systems with pictorial examples.
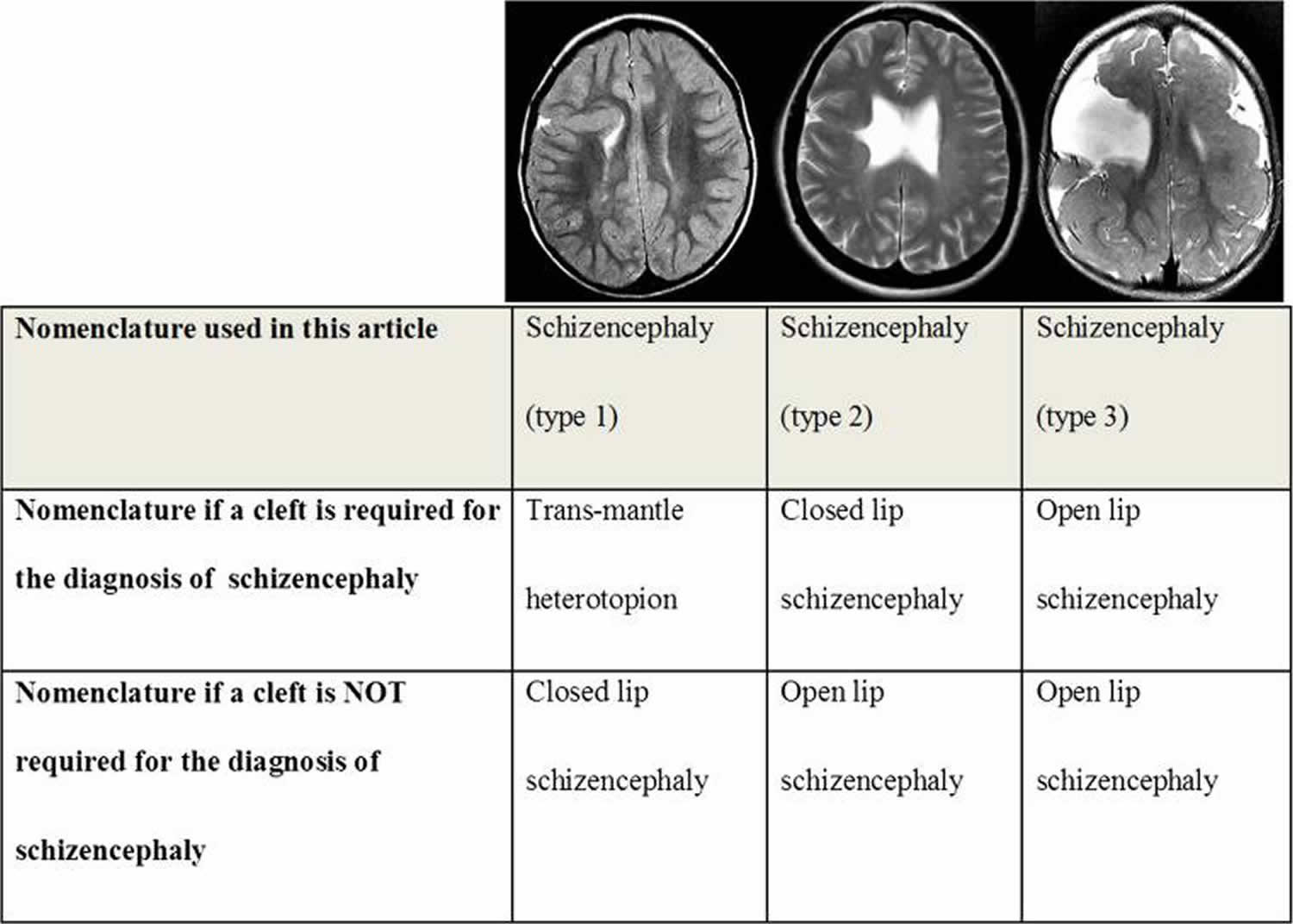
[Source 7 ]Figure 3. Schizencephaly type 1
Footnote: Unilateral schizencephaly type 1. MR images of a 4-year-old child with focal epilepsy. Axial T2-weighted (a), right parasagittal T2-weighted (b), axial (c) and coronal reconstructions from T1 volume imaging show abnormal grey matter extending from ventricular to out surface of the brain, centred on the right middle frontal gyrus. No CSF cleft is visible, hence the classification as schizencephaly type 1. The septum pellucidum is present and the course of the fornices is normal. No other brain abnormalities are present
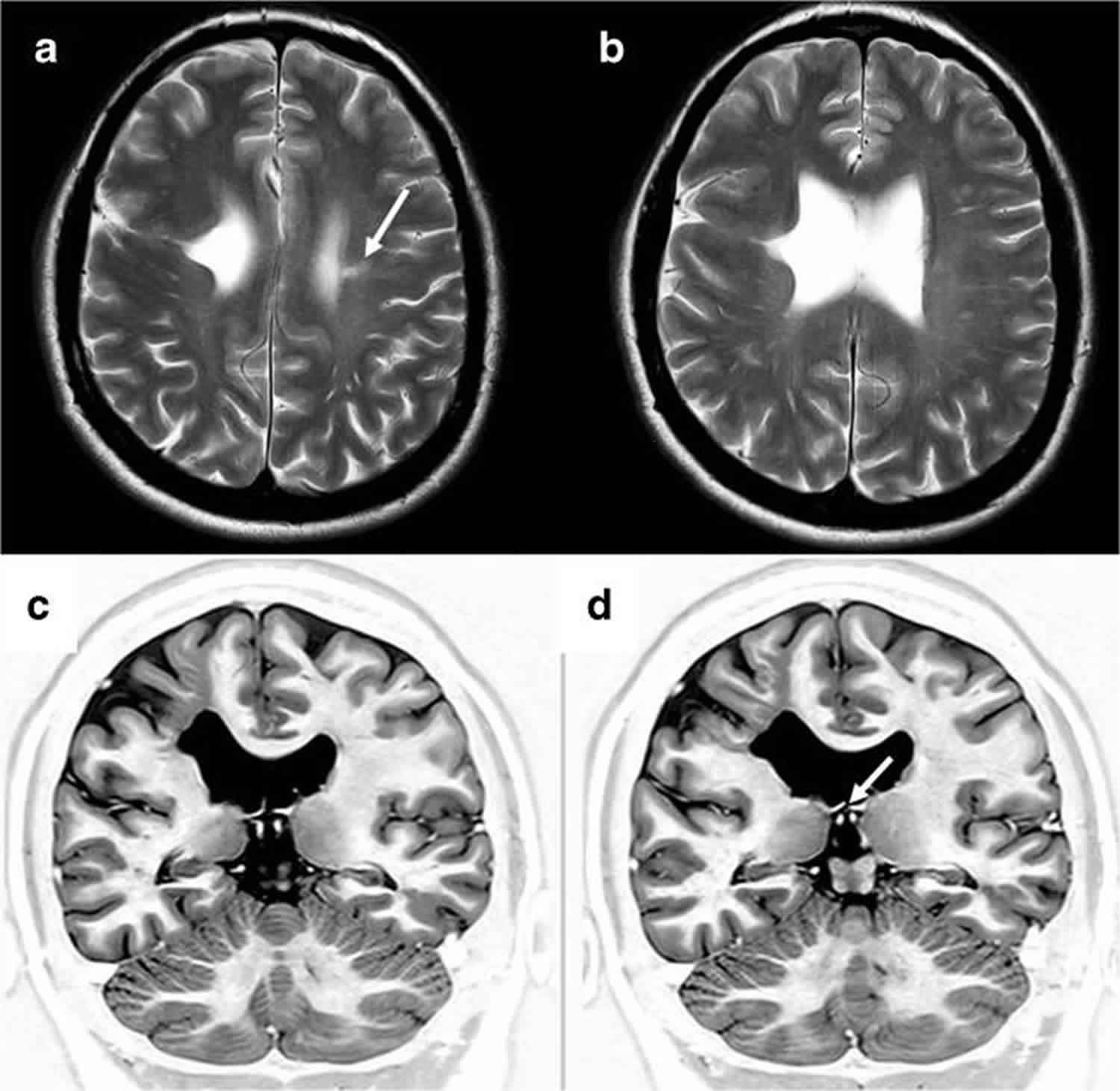
[Source 7 ]Figure 4. Schizencephaly type 2
Footnote: Unilateral schizencephaly type 2. MR images of a 4-year-old child with focal epilepsy and developmental delay. Axial T2-weighted (a, b) and coronal inversion recovery (c, d) images show a CSF cleft with closely opposed borders lined with polymicrogyria. There is also a small area of gliosis in the white matter of the contralateral paracentral lobule (arrowed on a). The septum pellucidum is absent and the fornices lie abnormally low (arrowed on d). No other brain abnormalities were present.
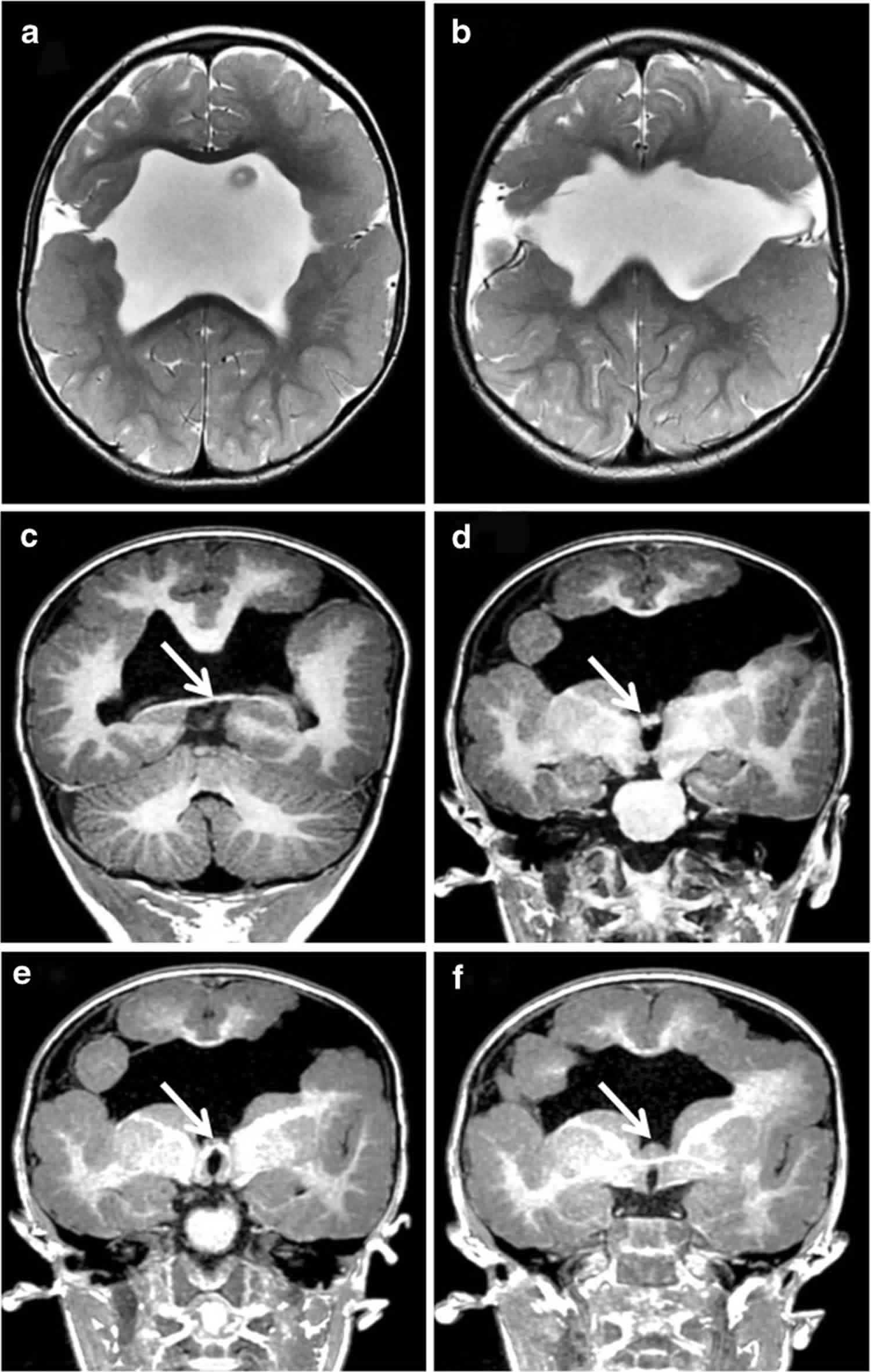
[Source 7 ]Figure 5. Schizencephaly type 3
Footnote: Bilateral schizencephaly type 3. MR images of a 2-year-old child with global developmental delay. Axial T2-weighted (a, b) and coronal reconstructions from T1-weighted volume data (c–f) show bilateral CSF clefts with non-opposed borders lined with polymicrogyria. The septum pellucidum is absent and the fornices lie abnormally low (arrowed on c–f). Extensive cortical formation abnormalities were present in both hemispheres.
[Source 7 ]Schizencephaly causes
The majority of cases of schizencephaly are sporadic and not thought to be inherited and in most cases, a cause is not found 7. Rarely, schizencephaly can affect more than one family member. This suggests that in some cases, schizencephaly may be hereditary. Both autosomal dominant and autosomal recessive patterns of inheritance have been reported 1.
A small number of people with schizencephaly are found to have changes (mutations) in one of four genes: EMX2, SIX3, SHH, and COL4A1 8. Recently, mutations in the COL4A1 gene encoding the major type IV alpha collagen chain of basement membranes have been found responsible of some schizencephaly cases. Rarely, schizencephaly can affect more than one family member 9. This supports a genetic cause in some cases 9.
Schizencephaly has also been linked to a variety of non-genetic factors, including young maternal age and certain medications and infections that can cause vascular disruptions (disruption of blood flow or blood supply) in a developing baby 1. Schizencephaly has been linked to vascular disruption such as maternal drug administration (e.g. warfarin), amniocentesis, and infections (cytomegalovirus) 1.
Schizencephaly symptoms
Signs and symptoms of schizencephaly may include:
- Developmental delay
- Seizures
- Abnormally small head (microcephaly)
- Intellectual disability
- Partial or complete paralysis
- Poor muscle tone (hypotonia)
- Hydrocephalus
Severity of symptoms depends on many factors, including the extent of the clefting and whether or not other brain abnormalities are present. For example, people with a small cleft in one hemisphere may have paralysis on one side of the body and little to no intellectual disability, while clefts in both hemispheres can lead to quadriplegia (paralysis of both arms and legs) and severe intellectual disability 1.
What are the effects of seizures on development?
The long-term effects of seizures vary widely depending on the seizure’s cause. Children whose epilepsy is a result of a specific condition (such as schizencephaly) have lower survival rates than the normal population, but this is most often due to the underlying condition.
Both clinical and laboratory studies show that seizures early in life can result in permanent behavioral abnormalities 10. In general, the earlier a child has seizures and the more extensive the area of the brain affected, the poorer the outcome. Children with seizures that are not well-controlled are at higher risk for intellectual decline. Learning and language problems as well as emotional and behavioral disorders occur in a significant number of children with epilepsy. It is worth noting, however, that progressive mental deterioration is often related to the neurologic disorder that caused the seizures rather than to the seizures themselves 11.
Schizencephaly diagnosis
Magnetic resonance imaging (MRI) is central to the diagnosis of children with congenital brain abnormalities, and in utero MR imaging (iuMRI) is now used for antenatal detection of brain abnormalities, including schizencephaly.
Schizencephaly is typically diagnosed by computed tomography (CT) and/or magnetic resonance imaging (MRI). A CT scan is an imaging method that uses x-rays to create pictures of cross-sections of the body, while an MRI scan uses powerful magnets and radio waves to create pictures of the brain and surrounding nerve tissues. Both of these imaging methods can be used to identify brain abnormalities such as the slits or clefts found in people with schizencephaly.
In some cases, schizencephaly can also be diagnosed prenatally (before birth) on ultrasound after 20 weeks gestation. If clefting is seen on ultrasound, an MRI scan of the developing baby may be recommended to confirm the diagnosis 12.
Schizencephaly treatment
The best treatment options for people with schizencephaly depend on many factors, including the severity of the condition and the signs and symptoms present. For example, people with developmental delay (i.e. delayed motor milestones) or partial paralysis may be referred for physical therapy and/or occupational therapy. Medications are often prescribed to prevent seizures. In cases that are complicated by hydrocephalus, a surgically implanted tube, called a shunt, is often used to divert fluid to another area of the body where it can be absorbed.
Schizencephaly prognosis
The long-term outlook for people with schizencephaly varies depending on the size and location of the clefts and the extent of intellectual disabilities. For example, children with a small cleft in one hemisphere may have paralysis on one side of the body and little to no intellectual disability, while clefts in both hemispheres can lead to quadriplegia (paralysis of both arms and legs) and severe intellectual disability.
Schizencephaly life expectancy
The life expectancy for individuals with schizencephaly varies depending on the size of the clefts and the extent of neurological disabilities.
- Schizencephaly. https://www.orpha.net/consor/cgi-bin/OC_Exp.php?Lng=GB&Expert=799[↩][↩][↩][↩][↩]
- Schizencephaly: heterogeneous etiologies in a population of 4 million California births. Curry CJ, Lammer EJ, Nelson V, Shaw GM. Am J Med Genet A. 2005 Aug 30; 137(2):181-9.[↩]
- Schizencephaly prevalence, prenatal diagnosis and clues to etiology: a register-based study. Howe DT, Rankin J, Draper ES. Ultrasound Obstet Gynecol. 2012 Jan; 39(1):75-82.[↩]
- Barkovich AJ, Raybaud CA. Congenital malformations of the brain and skull. Chapters 4 and 5. In: Barkovich AJ, Raybaud CA, editors. Pediatric neuroimaging. 5. Philadelphia: Lippincott Williams and Wilkins; 2012[↩]
- Naidich TP, Griffiths PD, Rosenbloom L. Central nervous system injury in utero: selected entities. Pediatr Radiol. 2015;45(3):S454–S462. doi: 10.1007/s00247-015-3344-6[↩]
- Yakovlev PI, Wadsworth RC. Schizencephalies. A study of the congenital clefts in the cerebral mantle I. Clefts with fused lips. J Neuropathol Exp Neurol. 1946;5:116–130. doi: 10.1097/00005072-194604000-00003[↩]
- Griffiths PD. Schizencephaly revisited. Neuroradiology. 2018;60(9):945–960. doi:10.1007/s00234-018-2056-7 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6096842[↩][↩][↩][↩][↩][↩]
- Yoneda et al. Phenotypic spectrum of COL4A1 mutations: porencephaly to schizencephaly. Ann. Neurol. 2013; 73:48-57.[↩]
- Hilburger AC, Willis JK, Bouldin E, Henderson-Tilton A. Familial schizencephaly. Brain & Development. May-June 1993; 15(3):234-236. http://www.ncbi.nlm.nih.gov/pubmed/8214352[↩][↩]
- Holmes GL. Effects of seizures on brain development: lessons from the laboratory. Pediatric Neurology. July 2005; 33(1):1-11. http://www.ncbi.nlm.nih.gov/pubmed/15993318[↩]
- Seizure Disorders. https://www.merckmanuals.com/professional/neurologic-disorders/seizure-disorders/seizure-disorders[↩]
- Schizencephaly Imaging. https://emedicine.medscape.com/article/413051-overview[↩]