What is Drinking Alcohol
Alcohol in the form of ethanol (ethyl alcohol) is found in alcoholic beverages, mouthwash, cooking extracts, some medications and certain household products. Ethanol (alcohol) is a central nervous system depressant that produces euphoria and behavioral excitation at low blood concentrations and acute intoxication (drowsiness, ataxia, slurred speech, stupor, and coma) at higher concentrations. The short-term effects of alcohol result from its actions on ligand-gated and voltage-gated ion channels 1. Prolonged alcohol consumption leads to the development of tolerance and physical dependence, which may result from compensatory functional changes in the same ion channels. Abrupt cessation of prolonged alcohol consumption unmasks these changes, leading to the alcohol withdrawal syndrome, which includes blackouts, tremors, muscular rigidity, delirium tremens, and seizures 2. Alcohol withdrawal seizures typically occur 6 to 48 hours after discontinuation of alcohol consumption and are usually generalized tonic–clonic seizures, although partial seizures also occur 3.
While there is no guaranteed safe amount of alcohol for anyone, the answer from current research is, the less alcohol, the better 4, 5. Alcohol is a carcinogen associated with cancer of the oral cavity, pharynx, larynx, esophagus, colon, rectum, liver, and female breast, with breast cancer risk rising with less than one drink a day. Your whole body is impacted by alcohol use not just your liver, but also your brain, gut, pancreas, lungs, cardiovascular system, immune system, and more and may explain, for example, challenges in managing hypertension, atrial fibrillation, diabetes, and recurrent lung infections.
Alcohol contributes to more than 200 health conditions including liver cirrhosis, cancers, and injuries and causes more than 3 million deaths each year globally (5.3% of all deaths worldwide) 6, 7. In the U.S., about 99,000 people die every year from alcohol-related causes 8, making alcohol one of the leading causes of preventable death 9, 10. More than half of the deaths result from chronic heavy alcohol consumption while the remainder result from acute injuries sustained while intoxicated 11.
The health risks of alcohol tend to be dose-dependent, and the likelihood of certain harms, such as cancer, begin at relatively low amounts 12. Even drinking within the U.S. Dietary Guidelines (see drinking level terms below), for example, increases the risk of breast cancer 13, 14. Additionally, earlier research suggested cardiovascular benefits, but newer, more rigorous studies are finding little or no protective effect of alcohol on cardiovascular or other outcomes 15, 16, 17, 18. In short, current research indicates there is no safe drinking level,11 underscoring the message to patients that “the less, the better” when it comes to alcohol.
The 2020-2025 U.S. Dietary Guidelines states that for adults who choose to drink alcohol, women should have 1 drink or less in a day and men should have 2 drinks or less in a day 19. These amounts are not intended as an average but rather a daily limit.
You are abusing alcohol when:
- You drink 7 drinks per week or more than 3 drinks per occasion (for women).
- You drink more than 14 drinks per week or more than 4 drinks per occasion (for men).
- You have more than 7 drinks per week or more than 3 drinks per occasion (for men and women older than 65).
- Consuming these amounts of alcohol harms your health, relationships, work, and/or causes legal problems.
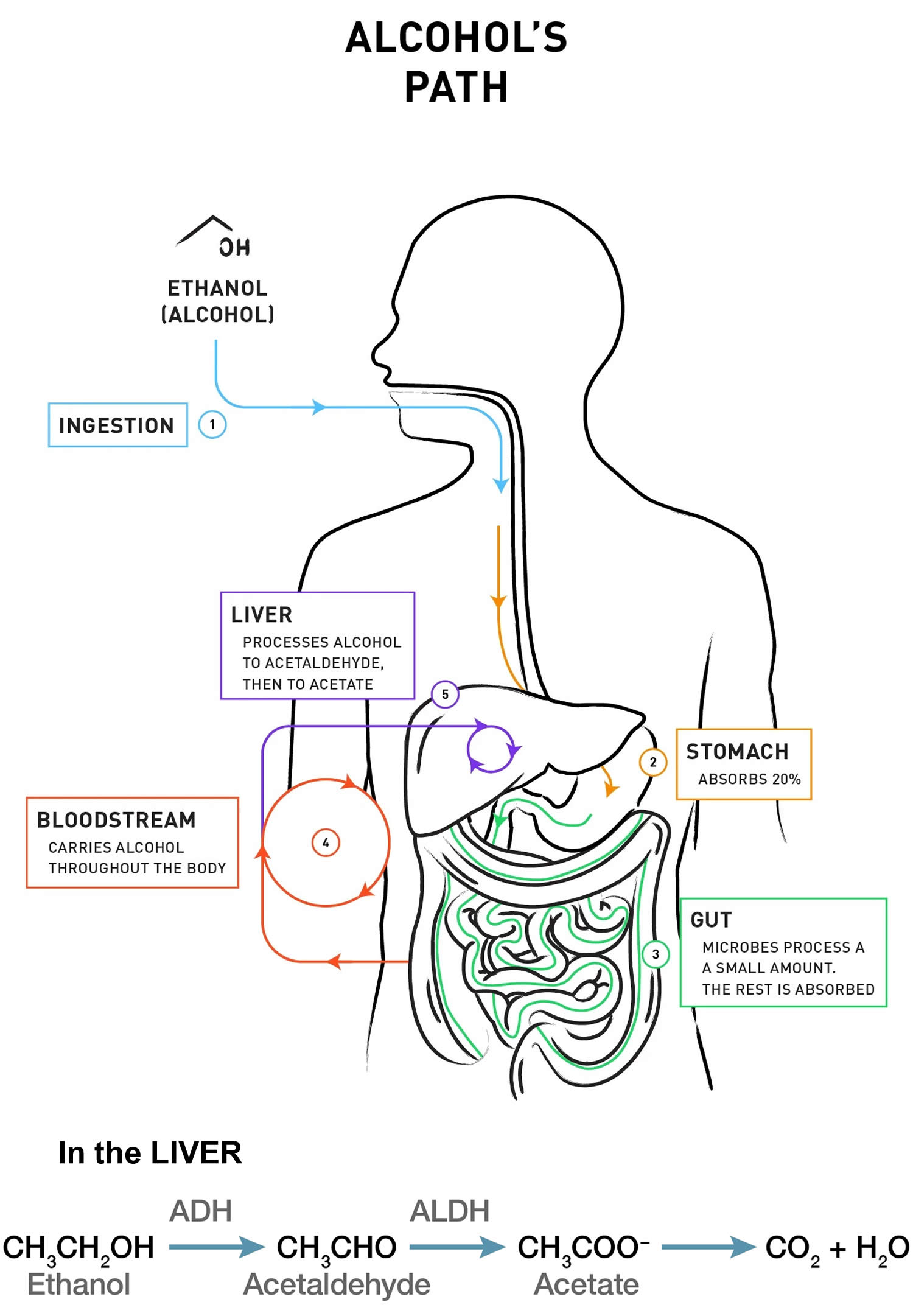
How does my body process alcohol?
When alcohol is consumed, it passes from your stomach and intestines into your bloodstream, where it distributes itself evenly throughout all the water in your body’s tissues and fluids. Drinking alcohol on an empty stomach increases the rate of absorption, resulting in higher blood alcohol level, compared to drinking on a full stomach. In either case, however, alcohol is still absorbed into the bloodstream at a much faster rate than it is metabolized. Thus, your blood alcohol concentration (BAC) builds when you have additional drinks before prior drinks are metabolized.
Your blood alcohol concentration (BAC) is largely determined by how much and how quickly you drink alcohol as well as by your body’s rates of alcohol absorption, distribution, and metabolism. Binge drinking is defined as reaching a BAC of 0.08% (0.08 grams of alcohol per deciliter of blood) or higher. A typical adult reaches this BAC after consuming 4 or more drinks (women) or 5 or more drinks (men), in about 2 hours.
Your body begins to metabolize alcohol within seconds after ingestion and proceeds at a steady rate, regardless of how much alcohol a person drinks or of attempts to sober up with caffeine or by other means. Most of the alcohol is broken down in your liver by the enzyme alcohol dehydrogenase (ADH). Alcohol dehydrogenase (ADH) transforms ethanol, the type of alcohol in alcohol beverages, into acetaldehyde, a toxic, carcinogenic compound. Generally, acetaldehyde is quickly broken down to a less toxic compound, acetate, by acetaldehyde dehydrogenase (ALDH) (also called aldehyde dehydrogenase). Acetate then is broken down, mainly in tissues other than the liver, into carbon dioxide (CO2) and water (H2O), which are easily eliminated. To a lesser degree, other enzymes (CYP2E1 and catalase) also break down alcohol to acetaldehyde 20.
Although the rate of metabolism is steady in any given person, it varies widely among individuals depending on factors including liver size and body mass, as well as genetics. There are multiple ADH and ALDH enzymes that are encoded by different genes 20. These genetic variants have been shown to influence a person’s drinking levels and, consequently, the risk of developing alcohol abuse or dependence 21. Studies have shown that people carrying certain ADH and ALDH alleles (one of two or more variants of a gene) are at significantly reduced risk of becoming alcohol dependent. In fact, these associations are the strongest and most widely reproduced associations of any gene with the risk of alcoholism. Some people of Asian descent, for example, carry variations of the genes for alcohol dehydrogenase (ADH) or acetaldehyde dehydrogenase (ALDH) that cause acetaldehyde (a toxic carcinogenic compound) to build up when alcohol is consumed, which in turn produces a flushing reaction and increases the risk of cancer risk 22, 23, 24. 20% of Chinese and Japanese cannot drink alcohol because of an inherited deficiency of acetaldehyde dehydrogenase 25.
Figure 2. How the body processes alcohol
Do you have a drinking problem?
While there is no guaranteed safe amount of alcohol for anyone, the answer from current research is, the less alcohol, the better 4, 5. The 2020-2025 U.S. Dietary Guidelines states that for adults who choose to drink alcohol, women should have 1 drink or less in a day and men should have 2 drinks or less in a day 19. These amounts are not intended as an average but rather a daily limit. Many people with alcohol problems cannot tell when their drinking is out of control. It is important to be aware of how much you are drinking. You should also know how your alcohol use may affect your life and those around you.
Many patients may think that heavy drinking is not a concern because they can “hold their liquor.” However, having an innate “low level of response” or “high tolerance” to alcohol is a reason for caution, as people with this trait tend to drink more and thus have an increased risk for alcohol-related problems including alcohol use disorder 26. People who drink within the U.S. Dietary Guidelines, too, may be unaware that even if they don’t feel a “buzz,” driving can be impaired 27.
Doctors consider your drinking medically unsafe when you drink:
- Many times a month, or even many times a week
- 3 to 4 drinks (or more) in 1 day
- 5 or more drinks on one occasion monthly, or even weekly
Twelve questions to ask if you think you may have a drinking problem
- Have you ever decided to stop drinking for a week or so, but only lasted for a couple of days? (Yes or No)
- Do you wish people would mind their own business about your drinking– stop telling you what to do? (Yes or No)
- Have you ever switched from one kind of drink to another in the hope that this would keep you from getting drunk? (Yes or No)
- Have you had to have a drink upon awakening during the past year? (Yes or No)
- Do you envy people who can drink without getting into trouble? (Yes or No)
- Have you had problems connected with drinking during the past year? (Yes or No)
- Has your drinking caused trouble at home? (Yes or No)
- Do you ever try to get “extra” drinks at a party because you do not get enough? (Yes or No)
- Do you tell yourself you can stop drinking any time you want to, even though you keep getting drunk when you don’t mean to? (Yes or No)
- Have you missed days of work or school because of drinking? (Yes or No)
- Do you have “blackouts”? (Yes or No) (Alcohol-related blackouts are gaps in a person’s memory for events that occurred while they were intoxicated. These gaps happen when a person drinks enough alcohol to temporarily block the transfer of memories from short-term to long-term storage, known as memory consolidation, in a brain area called the hippocampus.)
- Have you ever felt that your life would be better if you did not drink? (Yes or No)
If you answer YES 4 or more times – you are probably in trouble with alcohol.
However severe your drinking problem may seem, most people with alcohol use disorder can benefit from treatment. Unfortunately, less than 10 percent of them receive any treatment.
Ultimately, receiving treatment can improve your chances of success in overcoming alcohol use disorder.
Talk with your doctor to determine the best course of action for you.
What are the dangers of too much alcohol?
Too much alcohol is dangerous. Heavy drinking can increase the risk of certain cancers. It may lead to liver diseases, such as fatty liver disease and cirrhosis. It can also cause damage to the brain and other organs. Drinking during pregnancy can harm your baby. Alcohol also increases the risk of death from car crashes, injuries, homicide, and suicide.
Alcohol use is the fourth leading cause of preventable death in the United States (after smoking, high blood pressure, and obesity). According to a 2018 report from the WHO, in 2016 the harmful use of alcohol resulted in about 3 million deaths, or 5.3% of all deaths around the world, with most of these occurring among men 6. An average of 6 people die of alcohol poisoning each day in the US from 2010 to 2012 28. Alcohol poisoning is caused by drinking large quantities of alcohol in a short period of time. Very high levels of alcohol in the body can shutdown critical areas of the brain that control breathing, heart rate, and body temperature, resulting in death. Alcohol poisoning deaths affect people of all ages but are most common among middle-aged adults and men.
76% of alcohol poisoning deaths are among adults ages 35 to 64 28.
About 76% of those who die from alcohol poisoning are men 28.
The economic costs of excessive alcohol consumption in 2010 were estimated at $249 billion, or $2.05 a drink 29.
Alcohol poisoning deaths
- Most people who die are 35-64 years old.
- Most people who die are men.
- Most alcohol poisoning deaths are among non- Hispanic whites. Although a smaller share of the US population, American Indians/Alaska Natives have the most alcohol poisoning deaths per million people of any of the races.
- Alaska has the most alcohol poisoning deaths per million people, while Alabama has the least.
- Alcohol dependence (alcoholism) was identified as a factor in 30% of alcohol poisoning deaths.
Binge drinking can lead to death from alcohol poisoning
- Binge drinking (4 or more drinks for women or 5 or more drinks for men in a short period of time) typically leads to a blood alcohol concentration (BAC) that exceeds 0.08 g/dL, the legal limit for driving in all states.
- US adults who binge drink consume an average of about 8 drinks per binge, which can result in even higher levels of alcohol in the body.
- The more you drink the greater your risk of death.
An estimated 88,000 people (approximately 62,000 men and 26,000 women) die from alcohol-related causes annually, making alcohol the fourth leading preventable cause of death in the United States 30. Alcohol deaths accounted for 1 in 10 deaths among working-age adults aged 20–64 years 31. Excessive alcohol use shortened the lives of those who died by about 30 years. These deaths were due to health effects from drinking too much over time, such as breast cancer, liver disease, and heart disease, and health effects from consuming a large amount of alcohol in a short period of time, such as violence, alcohol poisoning, and motor vehicle crashes.
In 2014, alcohol-impaired driving fatalities accounted for 9,967 deaths (31 percent of overall driving fatalities) 32.
Figure 1. Alcohol Poisoning Deaths
[Source: Centers for Disease Control and Prevention 28]What counts as a standard drink?
In the United States, a “standard drink” or “alcoholic drink equivalent” is any drink containing 14 grams, or about 0.6 fluid ounces, of “pure” ethanol. One alcoholic drink equals one 12-ounce (oz), or 355 milliliters (mL), can or bottle of beer (with 5% alcohol by volume or alc/vol), a 5-ounce (148 mL) glass of wine (with 12% alc/vol), 1 wine cooler, 1 cocktail, 1 shot of hard liquor; or 1.5 ounces of 80-proof distilled spirits (such as whiskey, rum, or tequila) (with 40% alc/vol) 33.
Knowing how much alcohol constitutes a “standard” drink can help you determine how much you are drinking and understand the risks. One standard drink contains about 0.6 fluid ounces or 14 grams of pure alcohol.
The National Institute on Alcohol Abuse and Alcoholism defines one standard drink as any one of these:
- 12 ounces (355 milliliters) of regular beer (about 5 percent alcohol)
- 8 to 9 ounces (237 to 266 milliliters) of malt liquor (about 7 percent alcohol)
- 5 ounces (148 milliliters) of unfortified wine (about 12 percent alcohol)
- 1.5 ounces (44 milliliters) of 80-proof hard liquor (about 40 percent alcohol)
If you want to know the alcohol content of a canned or bottled beverage, start by checking the label. Not all beverages are required to list the alcohol content, so you may need to search online for a reliable source of information, such as the bottler’s Web site. For fact sheets about how to read wine, malt beverage, and distilled spirits labels, visit the consumer corner of the U.S. Alcohol and Tobacco Tax and Trade Bureau 34.
Although the “standard” drink amounts are helpful for following health guidelines, they may not reflect customary serving sizes. In addition, while the alcohol concentrations listed are “typical,” there is considerable variability in alcohol content within each type of beverage (e.g., beer, wine, distilled spirits). If you want to know how much alcohol is in a cocktail or a beverage container, try the U.S. Department of Health and Human Services. Rethinking Drinking – Alcohol calculators 35 or go here https://www.rethinkingdrinking.niaaa.nih.gov/Tools/Calculators/Default.aspx.
Footnotes: The sample standard drinks above are just starting points for comparison, because actual alcohol content and customary serving sizes can vary greatly both across and within types of beverages. For example:
- Beer: The most popular type of beer is light beer, which may be light in calories, but not necessarily in alcohol. The mean alc/vol for light beers is 4.3%, almost as much as a regular beer with 5% alc/vol.4 On average, craft beers have more than 5% alc/vol and flavored malt beverages, such as hard seltzers, more than 6% alc/vol.4 Some craft beers and flavored malt beverages have in the range of 8-9% alc/vol. Advise patients to check container labels for the alcohol content and adjust their intake accordingly.
- Wine: The largest category of wine is table wine. On average, table wines contain about 12% alc/vol4 and can range from about 5% to 16%. Larger wine glasses can encourage larger pours. People are often unaware that a 25-ounce (750ml) bottle of table wine with 12% alc/vol contains five standard drinks, and one with 14% alc/vol holds nearly six.
- Cocktails: Recipes for cocktails often exceed one standard drink’s worth of alcohol. The cocktail content calculator on Rethinking Drinking shows the alcohol content in sample cocktails.
How many drinks are in common containers?
In the United States, a “standard” drink is any drink that contains about 0.6 fluid ounces or 14 grams of “pure” alcohol. Below is the approximate number of standard drinks in different sized containers of
Table 1. How many drinks are in common containers
| Regular beer (5% alc/vol) | Malt liquor (7% alc/vol) | Table wine (12% alc/vol) | 80-proof distilled spirits (40% alc/vol) |
|---|---|---|---|
| 12 fl oz = 1 16 fl oz = 1⅓ 22 fl oz = 2 40 fl oz = 3⅓ | 12 fl oz = 1½ 16 fl oz = 2 22 fl oz = 2½ 40 fl oz = 4½ | 750 ml (a regular wine bottle) = 5 | a shot (1.5-oz glass/50-ml bottle) = 1 a mixed drink or cocktail = 1 or more 200 ml (a “half pint”) = 4½ 375 ml (a “pint” or “half bottle”) = 8½ 750 ml (a “fifth”) = 17 |
Footnote: Although the “standard” drink amounts are helpful for following health guidelines, they may not reflect customary serving sizes. In addition, while the alcohol concentrations listed are “typical,” there is considerable variability in alcohol content within each type of beverage (e.g., beer, wine, distilled spirits).
Do you drink cocktails or a beverage not listed above ? If you’re curious and willing to do a little research on your drink’s alcohol content, you can use Rethinking Drinking’s calculators (https://www.rethinkingdrinking.niaaa.nih.gov/Tools/Calculators/Default.aspx) to estimate the number of standard drinks per cocktail or container.
[Source 36 ]Levels of alcohol use
There are four levels of alcohol use:
- Social drinking: There is no guaranteed safe amount of alcohol for anyone. According to the “Dietary Guidelines for Americans 2020-2025” 19, adults of legal drinking age can choose not to drink or to drink in moderation by limiting intake to 2 drinks or less in a day for men (less than 14 drinks per week for men) and 1 drink or less in a day for women (less than 7 drinks per week for women), when alcohol is consumed. Drinking less is better for health than drinking more.
- At risk consumption: the level of drinking begins to pose a health risk. Frequent heavy drinking raises the risk for both acute harms, such as falls and medication interactions, and for chronic consequences, such as alcohol use disorder and dose-dependent increases in liver disease, heart disease and cancers 37, 38, 39.
- For men, consuming more than 5 drinks on any day or more than 15 drinks per week
- For women, consuming more than 4 drinks on any day or more than 8 drinks per week
- Binge drinking on 5 or more days in the past month
- Heavy drinking thresholds for women are lower than men because after consumption, alcohol distributes itself evenly in body water, and pound for pound, women have proportionally less water in their bodies than men do. This means that after a woman and a man of the same weight drink the same amount of alcohol, the woman’s blood alcohol concentration (BAC) will tend to be higher, putting her at greater risk for harm.
- Problem drinking: drinking causes serious problems to you, your family, your work and society in general
- Alcohol dependence and addiction:
- periodic or chronic intoxication
- uncontrollable craving for drink when sober
- tolerance to the effects of alcohol
- psychological and/or physical dependence
How much is too much?
How much alcohol is too much? It could mean drinking too much at one time, drinking too often, or both. It’s important to be aware of how much you are drinking, whether your drinking pattern is risky, the harm that some drinking patterns can cause, and ways to reduce your risks.
The Dietary Guidelines for Americans defines moderate drinking as up to 1 drink per day for women and up to 2 drinks per day for men 19. In addition, the Dietary Guidelines do not recommend that individuals who do not drink alcohol start drinking for any reason.
You are drinking too much if:
- On any day in the past year, For MEN: you drink more than 4 “standard” drinks per day and For WOMEN: you drink more than 3 “standard” drinks per day.
- On average, you drink alcohol more than 2 days per week.
- On a typical drinking day, you drink more than 4 standard drinks (for Men) or more than 3 standard drinks (for Women).
Figure 2. U.S. Adults Drinking Patterns
[Source: U.S. Department of Health and Human Services. Rethinking Drinking 40 ]You have had more “heavy drinking days” in the past year than 7 in 10 U.S. adults . Although your weekly average is typically within low-risk limits, once or twice a week you have more than the single-day limit of 4 drinks for men. You may be surprised that the majority of U.S. adults never exceed the low-risk drinking limits.
Your particular risk depends on how much, how quickly, and how often you drink. According to the National Institutes of Health survey, about 1 in 3 people in your drinking pattern group has an alcohol use disorder. In addition, just a single episode of drinking too much, too quickly, can lead to a serious injury.
Excessive drinking includes binge drinking, heavy drinking, and any drinking by pregnant women or people younger than age 21.
- Binge drinking, the most common form of excessive drinking, is defined as consuming
+ For women, 4 or more drinks during a single occasion.
+ For men, 5 or more drinks during a single occasion. - Heavy drinking is defined as consuming
+For women, 8 or more drinks per week.
+ For men, 15 or more drinks per week.
Most people who drink excessively are not alcoholics or alcohol dependent 41
You can reduce your risks. Research shows that people who stay within both the single-day and weekly limits have the lowest rates of alcohol-related problems. It’s safest to quit, however, if you already have signs of a problem.
Figure 3. “Low-Risk” Drinking Patterns
[Source: U.S. Department of Health and Human Services. Rethinking Drinking 42]“Low risk” is not “no risk.” Even within these limits, alcohol can cause problems if people drink too quickly, have health problems, or are older (both men and women over 65 are generally advised to have no more than 3 drinks on any day and 7 per week) 42. Based on your health and how alcohol affects you, you may need to drink less or not at all.
Research demonstrates “low-risk” drinking levels for men are no more than 4 drinks on any single day AND no more than 14 drinks per week 43. For women, “low-risk” drinking levels are no more than three drinks on any single day AND no more than seven drinks per week 43. To stay low-risk, you must keep within both the single-day and weekly limits.
Even within these limits, you can have problems if you drink too quickly, have health conditions, or are over age 65. Older adults should have no more than three drinks on any day and no more than seven drinks per week.
When is “low-risk” drinking still too much?
It’s safest to avoid alcohol altogether if you are:
- Taking medications that interact with alcohol
- Managing a medical condition that can be made worse by drinking
- Underage
- Planning to drive a vehicle or operate machinery
- Pregnant or trying to become pregnant
- Recovering from alcoholism or are unable to control the amount they drink.
Research shows that women start to have alcohol-related problems at lower drinking levels than men do 40. One reason is that, on average, women weigh less than men. In addition, alcohol disperses in body water, and pound for pound, women have less water in their bodies than men do. So after a man and woman of the same weight drink the same amount of alcohol, the woman’s blood alcohol concentration will tend to be higher, putting her at greater risk for harm.
How can you reduce your risks of alcohol use disorder?
Options for reducing alcohol-related risks include:
- Staying within low-risk drinking limits.
- Taking steps to be safe when you drink.
- Quitting drinking altogether.
For some people, staying within low-risk limits will be sufficient, whereas for others, it’s best to quit.
If you sometimes drink more than the low-risk limits, but don’t feel ready to make a change, see Pros and cons and Ready… or not. Don’t wait for an injury or a crisis, however. When it comes to changing risky drinking, sooner is better than later.
What’s “at-risk” or “heavy” drinking?
For healthy adults in general, drinking more than these single-day or weekly limits is considered “at-risk” or “heavy” drinking:
- Men: More than 4 drinks on any day or 14 per week.
- Women: More than 3 drinks on any day or 7 per week.
About 1 in 4 people who exceed these limits already has an alcohol use disorder, and the rest are at greater risk for developing these and other problems. Again, individual risks vary. People can have problems drinking less than these amounts, particularly if they drink too quickly 44.
In short, the more drinks on any day and the more heavy drinking days over time, the greater the risk—not only for an alcohol use disorder, but also for other health and personal problems.
Too much + too often = too risky
It makes a difference both how much you drink on any day and how often you have a “heavy drinking day,” that is, more than 4 drinks on any day for men or more than 3 drinks for women.
What is binge drinking?
The National Institute on Alcohol Abuse and Alcoholism (NIAAA) defines binge drinking is drinking so much at once that your blood alcohol concentration (BAC) level is 0.08% (0.08 grams of alcohol per deciliter of blood) or more. For a man, this usually happens after having 5 or more drinks within about 2 hours. For a woman, it is after about 4 or more drinks within about 2 hours 45. Not everyone who binge drinks has an alcohol use disorder, but they are at higher risk for getting one.
The Substance Abuse and Mental Health Services Administration (SAMHSA), which conducts the annual National Survey on Drug Use and Health, defines binge drinking as 5 or more alcoholic drinks for males or 4 or more alcoholic drinks for females on the same occasion (i.e., at the same time or within a couple of hours of each other) on at least 1 day in the past month.
Binge drinking occurs in the majority of adolescents who drink 46, in half of adults who drink 46 and in 1 in 10 adults over age 65 47 and is increasing among women 48, 49.
Binge drinking causes more than half of the alcohol-related deaths in the U.S. 46. Binge drinking increases the risk of falls, burns, car crashes, memory blackouts, medication interactions, assaults, drownings, and overdose deaths 46.
Alcohol use disorder
Alcohol use disorder (AUD) also called alcohol abuse or alcohol dependence syndrome, is an impaired ability to stop or control alcohol use despite adverse social, occupational, or health consequences 50. Alcohol use disorder encompasses the conditions that some people refer to as alcohol abuse, alcohol dependence, alcohol addiction, and the colloquial term, alcoholism. Alcohol use disorder can be mild, moderate, or severe. Severe alcohol use disorder is sometimes called alcoholism or alcohol dependence.
Alcohol use disorder is a medical condition in which you:
- Drink alcohol compulsively
- Can’t control how much you drink
- Feel anxious, irritable, and/or stressed when you are not drinking
An alcohol use disorder can range from mild to severe, depending on your symptoms.
With alcohol use disorder, you are not physically dependent, but you still have a serious problem. The drinking may cause problems at home, work, or school. Alcohol use disorder may cause you to put yourself in dangerous situations, or lead to legal or social problems.
Another common problem is binge drinking. Binge drinking is drinking about five or more drinks in two hours for men. For women, it is about four or more drinks in two hours.
Too much alcohol is dangerous. Heavy drinking can increase your risk of getting certain cancers. Too much alcohol can cause damage to the liver, brain, and other organs. Drinking during pregnancy can harm your baby. Alcohol also increases the risk of death from car crashes, injuries, homicide, and suicide.
Alcoholism or alcohol dependence, is a disease that causes:
- Craving – a strong need to drink
- Loss of control – not being able to stop drinking once you’ve started
- Physical dependence – withdrawal symptoms
- Tolerance – the need to drink more alcohol to feel the same effect
Alcohol use disorder is considered a brain disorder characterized by compulsive alcohol use, loss of control over alcohol intake, and a negative emotional state when not using 51. Lasting changes in the brain caused by alcohol misuse perpetuate alcohol use disorder and make individuals vulnerable to relapse. The good news is that no matter how severe the problem may seem, evidence-based treatment with behavioral therapies, mutual-support groups, and/or medications can help people with alcohol use disorder achieve and maintain recovery. According to a National Survey on Drug Use and Health conducted by the Substance Abuse and Mental Health Administration, 14.1 million adults ages 18 and older (5.6 percent of this age group) had alcohol use disorder in 2019 52, 53. Among youth, an estimated 414,000 adolescents ages 12–17 (1.7 percent of this age group) had alcohol use disorder during this timeframe.
An estimated 16 million people in the United States have alcohol use disorder 51. This means that their drinking causes distress and harm. It includes alcoholism and alcohol abuse. Approximately 6.2 percent or 15.1 million adults in the United States ages 18 and older had alcohol use disorder in 2015. This includes 9.8 million men and 5.3 million women. Adolescents can be diagnosed with alcohol use disorder as well, and in 2015, an estimated 623,000 adolescents ages 12–17 had alcohol use disorder 51.
To be diagnosed with alcohol use disorder, individuals must meet certain criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM), under DSM–5, the current version of the DSM, anyone meeting any two of the 11 criteria during the same 12-month period receives a diagnosis of alcohol use disorder. The severity of alcohol use disorder—mild, moderate, or severe—is based on the number of criteria met.
To assess whether you or loved one may have alcohol use disorder, here are some questions to ask.
Alcohol use disorder is diagnosed when a person answers “yes” to two or more of the questions below.
In the past year, have you:
- Ended up drinking more or for a longer time than you had planned to?
- Wanted to cut down or stop drinking, or tried to, but couldn’t?
- Spent a lot of your time drinking, or recovering from drinking?
- Needed a drink first thing in the morning to steady your nerves or get rid of a hangover?
- Felt a strong need to drink?
- Felt annoyed by criticism of your drinking?
- Had guilty feelings about drinking?
- Found that drinking – or being sick from drinking – often interfered with your family life, job, or school?
- Kept drinking even though it was causing trouble with your family or friends?
- Given up or cut back on activities that you enjoyed just so you could drink?
- Gotten into dangerous situations while drinking or after drinking? Some examples are driving drunk and having unsafe sex.
- Kept drinking even though it was making you feel depressed or anxious? Or when it was adding to another health problem?
- Had to drink more and more to feel the effects of the alcohol?
- Had withdrawal symptoms when the alcohol was wearing off? They include trouble sleeping, shakiness, irritability, anxiety, depression, restlessness, nausea, and sweating. In severe cases, you could have a fever, seizures, or hallucinations.
If you have any of these symptoms, your drinking may already be a cause for concern. The more symptoms you have, the more urgent the need for change. A health professional can conduct a formal assessment of your symptoms to see if alcohol use disorder is present.
However severe the problem may seem, most people with alcohol use disorder can benefit from treatment. Unfortunately, less than 10 percent of them receive any treatment.
Ultimately, receiving treatment can improve an individual’s chances of success in overcoming alcohol use disorder.
Talk with your doctor to determine the best course of action for you.
If you feel that you sometimes drink too much alcohol, or your drinking is causing problems, or your family is concerned about your drinking, talk with your doctor. Other ways to get help include talking with a mental health professional or seeking help from a support group such as Alcoholics Anonymous or a similar type of self-help group.
Because denial is common, you may not feel like you have a problem with drinking. You might not recognize how much you drink or how many problems in your life are related to alcohol use. Listen to relatives, friends or co-workers when they ask you to examine your drinking habits or to seek help. Consider talking with someone who has had a problem drinking, but has stopped.
If your loved one needs help
Many people with alcohol use disorder hesitate to get treatment because they don’t recognize they have a problem. An intervention from loved ones can help some people recognize and accept that they need professional help. If you’re concerned about someone who drinks too much, ask a professional experienced in alcohol treatment for advice on how to approach that person.
What cause alcohol use disorder?
The cause of alcohol use disorder is not well understood; however, several factors are thought to contribute to its development. These include the home environment, peer interactions, genetic factors, level of cognitive functioning, and certain existing personality disorders 54.Personality disorders associated with the development of an alcohol use disorder include disinhibition and impulsivity-type disorders, as well as depressive and socialization-related disorders 55.
Almost half of the people with any substance abuse problem, including alcohol use disorder, also had a co-existing mental illness 56, 57. Overall, alcohol use disorder tends to be more common in individuals with less education and low income.
Multiple theories have been suggested as to why some people develop alcohol use disorders. Some of the more evidence-supported theories include positive-effect regulation, negative-effect regulation, pharmacological vulnerability, and deviance proneness. Positive-effect regulation results in drinking for positive rewards (such as feelings of euphoria). Negative-effect regulation is seen when one drinks to cope with feelings of a negative nature, such as depression, anxiety, or feelings of worthlessness. Pharmacological vulnerability makes a note of an individual’s varied response to both acute and chronic effects of alcohol intake and the individual differences in the body’s ability to metabolize the alcohol. Deviance proneness speaks more to an individual’s tendency towards deviant behavior established during childhood, often due to a deficiency in socialization at an early age.
Some of the genes suspected in alcohol use disorder include GABRG2 and GABRA2, COMT Val 158Met, DRD2 Taq1A, and KIAA0040.
Risk factors for developing alcohol-use disorder
There is no single factor that accounts for the variation in individual risk of developing alcohol-use disorders. Alcohol use may begin in the teens, but alcohol use disorder occurs more frequently in the 20s and 30s, though it can start at any age. The evidence suggests that harmful alcohol use and alcohol dependence have a wide range of causal factors
- Family history of alcohol abuse. The risk of alcohol use disorder is higher for people who have a parent or other close relative who has problems with alcohol. This may be influenced by genetic factors.
- offspring of parents with alcohol dependence are four times more likely to develop alcohol dependence
- genetic studies (particularly those in twins) has clearly demonstrated a genetic component to the risk of alcohol dependence
- a meta-analysis of 9,897 twin pairs from Australian and US studies found the heritability of alcohol dependence to be in excess of 50%
- Psychological factors
- psychiatric comorbidity particularly depression, schizophrenia, bipolar disorder (BPD), anxiety, post-traumatic stress disorder (PTSD), psychosis and drug misuse. It’s common for people with a mental health disorder such as anxiety, depression, schizophrenia or bipolar disorder to have problems with alcohol or other substances.
- Stress, adverse life events and abuse
- Sex: men are twice as likely to be problem drinkers
- Occupation:
- publicans and brewers have an increased access to drink and are at a higher risk
- heavy drinking is seen as the norm in some jobs e.g. sailors
- Homelessness:
- a third of homeless people have a drink problem
- Steady drinking over time. Drinking too much on a regular basis for an extended period or binge drinking on a regular basis can lead to alcohol-related problems or alcohol use disorder.
- Started drinking at an early age. People who begin drinking — especially binge drinking — at an early age are at a higher risk of alcohol use disorder.
- History of trauma. People with a history of emotional or other trauma are at increased risk of alcohol use disorder.
- Having bariatric surgery (weight-loss surgery — involves making changes to your digestive system to help you lose weight). Some research studies indicate that having bariatric surgery may increase the risk of developing alcohol use disorder or of relapsing after recovering from alcohol use disorder.
- Social and cultural factors. Having friends or a close partner who drinks regularly could increase your risk of alcohol use disorder. The glamorous way that drinking is sometimes portrayed in the media also may send the message that it’s OK to drink too much. For young people, the influence of parents, peers and other role models can impact risk.
Alcohol use disorder prevention
Early intervention can prevent alcohol-related problems in teens. If you have a teenager, be alert to signs and symptoms that may indicate a problem with alcohol:
- Loss of interest in activities and hobbies and in personal appearance
- Red eyes, slurred speech, problems with coordination and memory lapses
- Difficulties or changes in relationships with friends, such as joining a new crowd
- Declining grades and problems in school
- Frequent mood changes and defensive behavior
You can help prevent teenage alcohol use:
- Set a good example with your own alcohol use.
- Talk openly with your child, spend quality time together and become actively involved in your child’s life.
- Let your child know what behavior you expect — and what the consequences will be if he or she doesn’t follow the rules.
Alcohol use disorder symptoms
A few mild symptoms — which you might not see as trouble signs — can signal the start of a drinking problem. It helps to know the signs so you can make a change early. If heavy drinking continues, then over time, the number and severity of symptoms can grow and add up to “alcohol use disorder.” Doctors diagnose alcohol use disorder when a patient’s drinking causes distress or harm. See if you recognize any of these symptoms in yourself. And don’t worry — even if you have symptoms, you can take steps to reduce your risks.
Alcohol use disorder can be mild, moderate or severe, based on the number of symptoms you experience.
Alcohol use disorder signs and symptoms may include:
- Being unable to limit the amount of alcohol you drink
- Wanting to cut down on how much you drink or making unsuccessful attempts to do so
- Spending a lot of time drinking, getting alcohol or recovering from alcohol use
- Feeling a strong craving or urge to drink alcohol
- Failing to fulfill major obligations at work, school or home due to repeated alcohol use
- Continuing to drink alcohol even though you know it’s causing physical, social or interpersonal problems
- Giving up or reducing social and work activities and hobbies
- Using alcohol in situations where it’s not safe, such as when driving or swimming
- Developing a tolerance to alcohol so you need more to feel its effect or you have a reduced effect from the same amount
- Experiencing withdrawal symptoms — such as nausea, sweating and shaking — when you don’t drink, or drinking to avoid these symptoms
Alcohol use disorder can include periods of alcohol intoxication and symptoms of withdrawal.
- Alcohol intoxication results as the amount of alcohol in your bloodstream increases. The higher the blood alcohol concentration is, the more impaired you become. Alcohol intoxication causes behavior problems and mental changes. These may include inappropriate behavior, unstable moods, impaired judgment, slurred speech, impaired attention or memory, and poor coordination. You can also have periods called “blackouts,” where you don’t remember events. Very high blood alcohol levels can lead to coma or even death.
- Alcohol withdrawal can occur when alcohol use has been heavy and prolonged and is then stopped or greatly reduced. It can occur within several hours to four or five days later. Signs and symptoms include sweating, rapid heartbeat, hand tremors, problems sleeping, nausea and vomiting, hallucinations, restlessness and agitation, anxiety, and occasionally seizures. Symptoms can be severe enough to impair your ability to function at work or in social situations.
The more symptoms you have, the more serious the problem is. If you think you might have an alcohol use disorder, see your health care provider for an evaluation. Your provider can help make a treatment plan, prescribe medicines, and if needed, give you treatment referrals.
People with alcohol use disorder may also report frequent falls, blackout spells, unsteadiness, or visual disturbances 54. They may report seizures if they went a few days without drinking, or tremors, confusion, emotional disturbances, and frequent job changes. They may also report social issues, such as job termination, separation/divorce, estrangement from family, or loss of home. They may also report sleep disturbances.
People with alcohol use disorder may have hypertension (high blood pressure) or insomnia (trouble falling and staying asleep) initially. In later stages, the patient may complain of nausea or vomiting, hematemesis (vomiting blood), bloated abdomen, epigastric pain, weight loss, jaundice, or other symptoms or signs suggestive of liver dysfunction. They may be asymptomatic early on.
People with alcohol use disorder may exhibit signs of cerebellar dysfunction, such as ataxia (impaired balance or coordination) or difficulty with fine motor skills, on exam. They may exhibit slurred speech, tachycardia (fast heart rate), memory impairment, nystagmus (involuntary eye movement which may cause the eye to rapidly move from side to side, up and down or in a circle), disinhibited behavior, or hypotension (low blood pressure). People with alcohol use disorder may present with tremors, confusion/mental status changes, asterixis, reddsih palms, jaundice, ascites, or other signs of advanced liver disease. There may also be spider angiomata, hepatomegaly/splenomegaly (early; liver becomes cirrhotic and shrunken in advanced disease). They may develop bleeding disorders, anemia, gastritis/ulcers, or pancreatitis as complications of alcohol use. Labs will reveal anemia, thrombocytopenia, coagulopathy, hyponatremia, hyperammonemia, elevated ammonia levels, or decreased B12/folate levels as the advanced liver disease develops.
Alcohol use disorder complications
Alcohol depresses your central nervous system. In some people, the initial reaction may be stimulation. But as you continue to drink, you become sedated.
Too much alcohol affects your speech, muscle coordination and vital centers of your brain. A heavy drinking binge may even cause a life-threatening coma or death. This is of particular concern when you’re taking certain medications that also depress the brain’s function.
Alcohol use disorder impact on your safety
Excessive drinking can reduce your judgment skills and lower inhibitions, leading to poor choices and dangerous situations or behaviors, including:
- Motor vehicle accidents and other types of accidental injury, such as drowning
- Relationship problems
- Poor performance at work or school
- Increased likelihood of committing violent crimes or being the victim of a crime
- Legal problems or problems with employment or finances
- Problems with other substance use
- Engaging in risky, unprotected sex, or experiencing sexual abuse or date rape
- Increased risk of attempted or completed suicide
Alcohol use disorder impact on your health
Drinking too much alcohol on a single occasion or over time can cause health problems, including:
- Liver disease. Heavy drinking can cause increased fat in the liver (hepatic steatosis), inflammation of the liver (alcoholic hepatitis), and over time, irreversible destruction and scarring of liver tissue (cirrhosis).
- Digestive problems. Heavy drinking can result in inflammation of the stomach lining (gastritis), as well as stomach and esophageal ulcers. It can also interfere with absorption of B vitamins and other nutrients. Heavy drinking can damage your pancreas or lead to inflammation of the pancreas (pancreatitis).
- Heart problems. Excessive drinking can lead to high blood pressure and increases your risk of an enlarged heart, heart failure or stroke. Even a single binge can cause a serious heart arrhythmia called atrial fibrillation.
- Diabetes complications. Alcohol interferes with the release of glucose from your liver and can increase the risk of low blood sugar (hypoglycemia). This is dangerous if you have diabetes and are already taking insulin to lower your blood sugar level.
- Sexual function and menstruation issues. Excessive drinking can cause erectile dysfunction in men. In women, it can interrupt menstruation.
- Eye problems. Over time, heavy drinking can cause involuntary rapid eye movement (nystagmus) as well as weakness and paralysis of your eye muscles due to a deficiency of vitamin B-1 (thiamin). A thiamin deficiency can also be associated with other brain changes, such as irreversible dementia, if not promptly treated.
- Birth defects. Alcohol use during pregnancy may cause miscarriage. It may also cause fetal alcohol syndrome, resulting in giving birth to a child who has physical and developmental problems that last a lifetime.
- Bone damage. Alcohol may interfere with the production of new bone. This bone loss can lead to thinning bones (osteoporosis) and an increased risk of fractures. Alcohol can also damage bone marrow, which makes blood cells. This can cause a low platelet count, which may result in bruising and bleeding.
- Neurological complications. Excessive drinking can affect your nervous system, causing numbness and pain in your hands and feet, disordered thinking, dementia, and short-term memory loss.
- Weakened immune system. Excessive alcohol use can make it harder for your body to resist disease, increasing your risk of various illnesses, especially pneumonia.
- Increased risk of cancer. Long-term, excessive alcohol use has been linked to a higher risk of many cancers, including mouth, throat, liver, esophagus, colon and breast cancers. Even moderate drinking can increase the risk of breast cancer.
- Medication and alcohol interactions. Some medications interact with alcohol, increasing its toxic effects. Drinking while taking these medications can either increase or decrease their effectiveness, or make them dangerous.
Alcohol use disorder diagnosis
You’re likely to start by seeing your doctor. If your doctor suspects you have a problem with alcohol, he or she may refer you to a mental health professional.
To assess your problem with alcohol, your doctor will likely:
- Ask you several questions related to your drinking habits. The doctor may ask for permission to speak with family members or friends. However, confidentiality laws prevent your doctor from giving out any information about you without your consent.
- Perform a physical exam. Your doctor may do a physical exam and ask questions about your health. There are many physical signs that indicate complications of alcohol use.
- Lab tests and imaging tests. While there are no specific tests to diagnose alcohol use disorder, certain patterns of lab test abnormalities may strongly suggest it. And you may need tests to identify health problems that may be linked to your alcohol use. Damage to your organs may be seen on tests.
- Complete a psychological evaluation. This evaluation includes questions about your symptoms, thoughts, feelings and behavior patterns. You may be asked to complete a questionnaire to help answer these questions.
- Use the DSM-5 criteria. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), published by the American Psychiatric Association, is often used by mental health professionals to diagnose mental health conditions.
DSM-5 alcohol use disorder
DSM-5 Criteria for the Diagnosis of Alcohol Use Disorder 58:
- Criterion A. A problematic pattern of alcohol use leading to clinically significant impairment or distress, as manifested by at least two of the following, occurring within a 12-month period:
- Alcohol is often taken in larger amounts or over a longer period than was intended.
- There is a persistent desire or unsuccessful efforts to cut down or control alcohol use.
- A great deal of time is spent in activities necessary to obtain alcohol, use alcohol, or recover from its effects.
- Craving, or a strong desire or urge to use alcohol.
- Recurrent alcohol use resulting in a failure to fulfill major role obligations at work, school, or home.
- Continued alcohol use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of alcohol.
- Important social, occupational, or recreational activities are given up or reduced because of alcohol use.
- Recurrent alcohol use in situations in which it is physically hazardous.
- Alcohol use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by alcohol.
- Tolerance, as defined by either of the following:
- a. A need for markedly increased amounts of alcohol to achieve intoxication or desired effect.
- b. A markedly diminished effect with continued use of the same amount of alcohol.
- Withdrawal, as manifested by either of the following:
- a. The characteristic withdrawal syndrome for alcohol.
- b. Alcohol (or a closely related substance, such as a benzodiazepine) is taken to relieve or avoid withdrawal symptoms.
Specify if:
- In early remission: After full criteria for alcohol use disorder were previously met, none of the criteria for alcohol use disorder have been met for at least 3 months but for less than 12 months (with the exception that Criterion A4, “Craving, or a strong desire or urge to use alcohol,” may be met).
- In sustained remission: After full criteria for alcohol use disorder were previously met, none of the criteria for alcohol use disorder have been met at any time during a period of 12 months or longer (with the exception that Criterion A4, “Craving, or a strong desire or urge to use alcohol,” may be met).
Specify if:
- In a controlled environment: This additional specifier is used if the individual is in an environment where access to alcohol is restricted.
Alcohol use disorder is defined by a cluster of behavioral and physical symptoms, which can include withdrawal, tolerance, and craving. Alcohol withdrawal is characterized by withdrawal symptoms that develop approximately 4-12 hours after the reduction of intake following prolonged, heavy alcohol ingestion. Because withdrawal from alcohol can be unpleasant and intense, individuals may continue to consume alcohol despite adverse consequences, often to avoid or to relieve withdrawal symptoms. Some withdrawal symptoms (e.g., sleep problems) can persist at lower intensities for months and can contribute to relapse. Once a pattern of repetitive and intense use develops, individuals with alcohol use disorder may devote substantial periods of time to obtaining and consuming alcoholic beverages.
Craving for alcohol is indicated by a strong desire to drink that makes it difficult to think of anything else and that often results in the onset of drinking. School and job performance may also suffer either from the aftereffects of drinking or from actual intoxication at school or on the job; child care or household responsibilities may be neglected; and alcohol-related absences may occur from school or work. The individual may use alcohol in physically hazardous circumstances (e.g., driving an automobile, swimming, operating machinery while intoxicated). Finally, individuals with an alcohol use disorder may continue to consume alcohol despite the knowledge that continued consumption poses significant physical (e.g., blackouts, liver disease), psychological (e.g., depression), social, or interpersonal problems (e.g., violent arguments with spouse while intoxicated, child abuse).
Treatment of Alcohol Use Disorder
Alcohol use disorder is when your drinking causes serious problems in your life, yet you keep drinking. You may also need more and more alcohol to feel drunk. Stopping suddenly may cause withdrawal symptoms. This means that your drinking causes distress and harm. It includes alcoholism and alcohol abuse. Many people with an alcohol problem need to completely stop using alcohol. This is called abstinence. Having strong social and family support can help make it easier to quit drinking.
Some people are able to just cut back on their drinking. So even if you do not give up alcohol altogether, you may be able to drink less. This can improve your health and relationships with others. It can also help you perform better at work or school.
However, many people who drink too much find they can’t just cut back. Abstinence may be the only way to manage a drinking problem.
The good news is that no matter how severe the problem may seem, most people with an alcohol use disorder can benefit from some form of treatment.
Research shows that about one-third of people who are treated for alcohol problems have no further symptoms 1 year later. Many others substantially reduce their drinking and report fewer alcohol-related problems.
Ultimately, there is no one-size-fits-all solution, and what may work for one person may not be a good fit for someone else. Simply understanding the different options can be an important first step.
Treatment for alcohol use disorder may include:
- Detox and withdrawal. Treatment may begin with a program of detoxification or detox — withdrawal that’s medically managed — which generally takes two to seven days. You may need to take sedating medications to prevent withdrawal symptoms. Detox is usually done at an inpatient treatment center or a hospital.
- Learning skills and establishing a treatment plan. This usually involves alcohol treatment specialists. It may include goal setting, behavior change techniques, use of self-help manuals, counseling and follow-up care at a treatment center.
- Psychological counseling. Counseling and therapy for groups and individuals help you better understand your problem with alcohol and support recovery from the psychological aspects of alcohol use. You may benefit from couples or family therapy — family support can be an important part of the recovery process.
- Oral medications. A drug called disulfiram (Antabuse) may help prevent you from drinking, although it won’t cure alcohol use disorder or remove the compulsion to drink. If you drink alcohol, the drug produces a physical reaction that may include flushing, nausea, vomiting and headaches. Naltrexone, a drug that blocks the good feelings alcohol causes, may prevent heavy drinking and reduce the urge to drink. Acamprosate may help you combat alcohol cravings once you stop drinking. Unlike disulfiram, naltrexone and acamprosate don’t make you feel sick after taking a drink.
- Injected medication. Vivitrol, a version of the drug naltrexone, is injected once a month by a health care professional. Although similar medication can be taken in pill form, the injectable version of the drug may be easier for people recovering from alcohol use disorder to use consistently.
- Continuing support. Aftercare programs and support groups help people recovering from alcohol use disorder to stop drinking, manage relapses and cope with necessary lifestyle changes. This may include medical or psychological care or attending a support group.
- Treatment for psychological problems. Alcohol use disorder commonly occurs along with other mental health disorders. If you have depression, anxiety or another mental health condition, you may need talk therapy (psychotherapy), medications or other treatment.
- Medical treatment for health conditions. Many alcohol-related health problems improve significantly once you stop drinking. But some health conditions may warrant continued treatment and follow-up.
- Spiritual practice. People who are involved with some type of regular spiritual practice may find it easier to maintain recovery from alcohol use disorder or other addictions. For many people, gaining greater insight into their spiritual side is a key element in recovery.
Some people may need intensive treatment for alcohol use disorder. They may go to a residential treatment center for rehabilitation (rehab). Residential treatment programs typically include licensed alcohol and drug counselors, social workers, nurses, doctors and others with expertise and experience in treating alcohol use disorder. Treatment there is highly structured. It usually includes several different kinds of behavioral therapies. Most residential treatment programs include individual and group therapy, support groups, educational lectures, family involvement and activity therapy. It may also include medicines for detox (medical treatment for alcohol withdrawal) and/or for treating the alcohol use disorder.
DECIDING TO QUIT
Like many people with an alcohol problem, you may not recognize that your drinking has gotten out of hand. An important first step is to be aware of how much you drink. It also helps to understand the health risks of alcohol.
If you decide to quit drinking, talk with your provider. Treatment involves helping you realize how much your alcohol use is harming your life and the lives those around you.
Depending on how much and how long you have been drinking, you may be at risk for alcohol withdrawal. Withdrawal can be very uncomfortable and even life threatening. If you have been drinking a lot, you should cut back or stop drinking only under the care of a doctor. Talk with your provider about how to stop using alcohol.
LONG-TERM SUPPORT
Alcohol recovery or support programs can help you stop drinking completely. These programs usually offer:
- Education about alcohol use and its effects
- Counseling and therapy to discuss how to control your thoughts and behaviors
- Physical health care
For the best chance of success, you should live with people who support your efforts to avoid alcohol. Some programs offer housing options for people with alcohol problems. Depending on your needs and the programs that are available:
- You may be treated in a special recovery center (inpatient)
- You may attend a program while you live at home (outpatient)
You may be prescribed medicines to help you quit. They are often used with long-term counseling or support groups. These medicines make it less likely that you will drink again or help limit the amount you drink.
Drinking may mask depression or other mood or anxiety disorders. If you have a mood disorder, it may become more noticeable when you stop drinking. Your provider will treat any mental disorders in addition to your alcohol treatment.
Support Groups for Alcohol use disorder
Because an alcohol use disorder can be a chronic relapsing disease, persistence is key. It is rare that someone would go to treatment once and then never drink again. More often, people must repeatedly try to quit or cut back, experience recurrences, learn from them, and then keep trying. For many, continued followup with a treatment provider is critical to overcoming problem drinking. Support groups help many people who are dealing with alcohol use and relapses.
Relapse is common among people who overcome alcohol problems. People with drinking problems are most likely to relapse during periods of stress or when exposed to people or places associated with past drinking.
Just as some people with diabetes or asthma may have flare-ups of their disease, a relapse to drinking can be seen as a temporary set-back to full recovery and not a complete failure. Seeking professional help can prevent relapse — behavioral therapies can help people develop skills to avoid and overcome triggers, such as stress, that might lead to drinking. Most people benefit from regular checkups with a treatment provider. Medications also can deter drinking during times when individuals may be at greater risk of relapse (e.g., divorce, death of a family member).
If you cannot stop drinking, GET HELP. You may have a disease called alcoholism. There are programs that can help you stop drinking. They are called alcohol treatment programs. Your doctor or nurse can find a program to help you. Even if you have been through a treatment program before, try it again. There are also programs just for women.
Consider joining Alcoholics Anonymous or another mutual support group (see links below). Recovering people who attend groups regularly do better than those who do not. Groups can vary widely, so shop around for one that’s comfortable. You’ll get more out of it if you become actively involved by having a sponsor and reaching out to other members for assistance.
- Alcoholics Anonymous (https://www.aa.org)
- Moderation Management (https://moderation.org)
- Secular Organizations for Sobriety (https://www.sossobriety.org)
- SMART Recovery (https://www.smartrecovery.org)
- Women for Sobriety (https://womenforsobriety.org)
- Al-Anon Family Groups (https://al-anon.org)
- Adult Children of Alcoholics (https://adultchildren.org)
- National Council on Alcoholism and Drug Dependence (https://recovered.org)
- National Institute on Alcohol Abuse and Alcoholism (https://www.niaaa.nih.gov)
- National Organization on Fetal Alcohol Syndrome (https://fasdunited.org)
- Substance Abuse and Mental Health Services Administration (https://findtreatment.gov)
Medications for alcohol use disorder
The U.S. Food and Drug Administration (FDA) has approved three medications for treating alcohol dependence, and alcohol use disorder (see Table 1 below) 59. All of these medications are non-addictive, so you don’t have to worry about trading one addiction for another. Your health care provider can help you figure out if one of these medicines is right for you. They are not a cure, but they can help you manage alcohol use disorder. This is just like taking medicines to manage a chronic disease such as asthma or diabetes.
- Naltrexone can help people reduce heavy drinking.
- Acamprosate makes it easier to maintain abstinence.
- Disulfiram blocks the breakdown (metabolism) of alcohol by the body, causing unpleasant symptoms such as nausea and flushing of the skin. Those unpleasant effects can help some people avoid drinking while taking disulfiram.
It is important to remember that not all people will respond to medications, but for a subset of individuals, they can be an important tool in overcoming alcohol dependence.
Of the FDA approved medications, the two newer ones (naltrexone and acamprosate) can make it easier to quit drinking by offsetting changes in the brain caused by alcoholism. They don’t make you sick if you do drink, unlike the older approved medication (disulfiram) 60.
Used in the context of a comprehensive treatment plan, medications for alcohol use disorder can provide an opportunity for behavioral therapies (counseling) to be helpful by reducing craving or helping to maintain abstinence from alcohol. In that way, medications can give people with an alcohol problem some traction in the recovery process.
It’s important to consult a doctor who understands which people are good candidates for alcohol use disorder medications. Some studies suggest that people with a family history of alcohol use disorder may be likely to benefit from naltrexone, for example. But those who have a liver condition or use opioid medications (such as those prescribed for pain) should not take naltrexone. A doctor can assess these and other conditions and match an appropriate medication with the patient.
As with any other medication, patients should communicate with their doctor about how the medication is working, and the doctor may be able to adjust the dose if needed.
Medications for alcohol use disorder can be prescribed not only by specialists in addiction treatment, but also by primary care physicians.
Scientists are working to develop a larger menu of pharmaceutical treatments that could be tailored to individual needs. As more medications become available, people may be able to try multiple medications to find which they respond to best.
Certain medications already approved for other uses have shown promise for treating alcohol dependence and problem drinking:
- The anti-smoking drug varenicline (marketed under the name Chantix) significantly reduced alcohol consumption and craving among people with alcoholism.
- Gabapentin, a medication used to treat pain conditions and epilepsy, was shown to increase abstinence and reduce heavy drinking. Those taking the medication also reported fewer alcohol cravings and improved mood and sleep.
- The anti-epileptic medication topiramate was shown to help people curb problem drinking, particularly among those with a certain genetic makeup that appears to be linked to the treatment’s effectiveness.
Naltrexone
Naltrexone blocks opioid receptors that are involved in the rewarding effects of drinking and the craving for alcohol 61. Naltrexone is an opioid antagonist, reduces alcohol consumption in patients with alcohol use disorder and is more successful in those who are abstinent before starting the medication 62. The opioid receptor system mediates the pleasurable effects of alcohol. Alcohol ingestion stimulates endogenous opioid release and increases dopamine transmission. Naltrexone blocks these effects, reducing euphoria and cravings 63. Naltrexone comes either as a pill that is taken daily, or as an injection that can be given once per month. Because naltrexone is metabolized by the liver, liver toxicity is possible, although uncommon. Patients with alcohol use disorder may have liver dysfunction; therefore, caution is warranted. Naltrexone can precipitate severe opioid withdrawal in patients who are opioid-dependent, so these agents should not be used together, and opioids should not be used for at least seven days before starting naltrexone 62. Pain management is challenging for patients taking naltrexone; these patients should carry a medical alert card.
Naltrexone is well tolerated and is not habit-forming. Naltrexone can also reduce your craving for alcohol. This can help you cut back on your drinking.
A Cochrane review that included 50 randomized trials and 7,793 patients found that oral naltrexone decreased heavy drinking (number needed to treat (NNT) = 10) and slightly decreased daily drinking (NNT = 25). The number of heavy drinking days and the amount of alcohol consumed also decreased. Injectable naltrexone did not decrease heavy drinking, but the sample size was small 64. A subsequent systematic review of 53 randomized trials including 9,140 patients found that oral naltrexone increased abstinence rates (NNT = 20) and decreased heavy drinking (NNT = 12). There was no difference between naltrexone and acamprosate. Injectable naltrexone did not demonstrate benefit 65. A randomized trial of 627 veterans with alcohol use disorder who received injectable naltrexone or placebo found that 380 mg of naltrexone given intramuscularly decreased heavy drinking days over six months but did not increase abstinence rates 66. Another meta-analysis found no difference in heavy drinking between acamprosate and naltrexone; however, it favored acamprosate for abstinence and naltrexone for cravings 67. Studies of combination therapy with acamprosate and naltrexone have produced mixed results. The COMBINE study did not show that combined therapy was more effective than either agent alone 68. Another study showed that relapse rates were lower with combined therapy compared with placebo or acamprosate alone, but not compared with naltrexone alone 69. It is unclear if and when combination therapy should be used, although it may be reasonable to consider it if monotherapy fails. Opioid antagonists may also be helpful when used as needed during high-risk situations, such as social events or weekends 70.
Like any medicine, naltrexone can cause side effects. Nausea is the most common one. Other side effects include:
- Headache
- Diarrhea
- Constipation
- Dizziness
- Nervousness
- Insomnia
- Drowsiness
- Anxiety
If you get any of these side effects, tell your doctor. They may change your treatment or suggest ways you can deal with the side effects.
Call your doctor immediately if you experience any of the following symptoms:
- Blurry vision
- Confusion
- Hallucinations (hearing or seeing things that aren’t there)
- Severe vomiting or diarrhea
- Vomiting up blood
- Excessive fatigue
- Bleeding or bruising
- Loss of appetite
- Pain in the upper right part of your stomach that lasts more than a few days
- Light-colored bowel movements
- Dark urine
- Yellowing of the skin or eyes
Talk to your doctor if you have a history of depression. Naltrexone may cause liver damage when taken in large doses. Tell your doctor if you have had hepatitis or liver disease.
Acamprosate
Acamprosate (Campral®) acts on the gamma-aminobutyric acid (GABA) and glutamate neurotransmitter systems and is thought to reduce symptoms of protracted withdrawal, such as insomnia, anxiety, restlessness, and dysphoria 61. Acamprosate has been shown to help dependent drinkers maintain abstinence for several weeks to months, and it may be more effective in patients with severe dependence. Acamprosate is a pill that is taken three times per day.
Acamprosate appears to be most effective at maintaining abstinence in patients who are not currently drinking alcohol 67. Acamprosate seems to interact with glutamate at the N-methyl-d-aspartate receptor, although its exact mechanism is unclear 71. Acamprosate is safe in patients with impaired liver function but should be avoided in patients with severe kidney dysfunction. A systematic review of 27 studies including 7,519 patients using acamprosate showed a number needed to treat (NNT) of 12 to prevent a return to any drinking 65. A Cochrane review of 24 trials including 6,915 patients concluded that acamprosate reduced drinking compared with placebo (NNT = 9) 72. One randomized trial found no difference between acamprosate and placebo, although outcomes improved significantly in both groups. This may be because enrolled patients were highly motivated to decrease alcohol use, increasing the likelihood of success with any treatment 73.
Disulfiram
Disulfiram (Antabuse®) interferes with degradation of alcohol, resulting in the accumulation of acetaldehyde, which, in turn, produces a very unpleasant reaction that includes flushing, nausea, and plapitations whenever you drink alcohol 61. Knowing that drinking will cause these unpleasant effects may help you stay away from alcohol. The utility and effectiveness of disulfiram are considered limited because compliance is generally poor. However, among patients who are highly motivated, disulfiram can be effective, and some patients use it episodically for high-risk situations, such as social occasions where alcohol is present. It can also be administered in a monitored fashion, such as in a clinic or by a spouse, improving its efficacy.
There are limited trials to support the effectiveness of disulfiram. It does not reduce the craving for alcohol, but it causes unpleasant symptoms when alcohol is ingested because it inhibits aldehyde dehydrogenase and alcohol metabolism. Compliance is a major limitation, and disulfiram is more effective when taken under supervision. One trial randomized 243 patients to naltrexone, acamprosate, or disulfiram with supervision over 12 weeks and determined that patients taking disulfiram had fewer heavy drinking days, lower weekly consumption, and a longer period of abstinence compared with the other drugs 74. However, a 2014 meta-analysis of 22 randomized trials found that in open-label studies, disulfiram was more effective than naltrexone, acamprosate, and no disulfiram, but blinded studies did not demonstrate benefit for disulfiram 75. In a systematic review of two studies including 492 patients, disulfiram did not reduce drinking rates 65. A review by the Agency for Healthcare Research and Quality on pharmacotherapy for adults with alcohol-use disorders in outpatient settings found insufficient evidence to support disulfiram’s effectiveness 76.
Topiramate
Topiramate is thought to work by increasing inhibitory (GABA) neurotransmission and reducing stimulatory (glutamate) neurotransmission, although its precise mechanism of action is not known 61. Although topiramate has not yet received FDA approval for treating alcohol addiction, it is sometimes used off-label for this purpose. Topiramate has been shown in studies to significantly improve multiple drinking outcomes, compared with a placebo.
Isn’t taking medications just trading one addiction for another?
This is not an uncommon concern, but the short answer is “no.” All medications approved for treating alcohol dependence are non-addictive 59. These medicines are designed to help manage a chronic disease, just as someone might take drugs to keep their cholesterol or diabetes in check.
Behavioral therapies
Another name for behavioral therapies for alcohol use disorder is alcohol counseling. It involves working with a health care professional to identify and help change the behaviors that lead to your heavy drinking.
- Cognitive-behavioral therapy (CBT) helps you identify the feelings and situations that can lead to heavy drinking. It teaches you coping skills, including how to manage stress and how to change the thoughts that cause you to want to drink. You may get CBT one-on-one with a therapist or in small groups.
- Motivational enhancement therapy helps you build and strengthen the motivation to change your drinking behavior. It includes about four sessions over a short period of time. The therapy starts with identifying the pros and cons of seeking treatment. Then you and your therapist work on forming a plan for making changes in your drinking. The next sessions focus on building up your confidence and developing the skills you need to be able to stick to the plan.
- Marital and family counseling includes spouses and other family members. It can help to repair and improve your family relationships. Studies show that strong family support through family therapy may help you to stay away from drinking.
- Brief interventions are short, one-on-one or small-group counseling sessions. It includes one to four sessions. The counselor gives you information about your drinking pattern and potential risks. The counselor works with you to set goals and provide ideas that may help you make a change.
Lifestyle choices
As part of your recovery, you’ll need to focus on changing your habits and making different lifestyle choices. These strategies may help.
- Consider your social situation. Make it clear to your friends and family that you’re not drinking alcohol. Develop a support system of friends and family who can support your recovery. You may need to distance yourself from friends and social situations that impair your recovery.
- Develop healthy habits. For example, good sleep, regular physical activity, managing stress more effectively and eating well all can make it easier for you to recover from alcohol use disorder.
- Do things that don’t involve alcohol. You may find that many of your activities involve drinking. Replace them with hobbies or activities that are not centered around alcohol.
Alternative medicine
Avoid replacing conventional medical treatment or psychotherapy with alternative medicine. But if used in addition to your treatment plan when recovering from alcohol use disorder, these techniques may be helpful:
- Yoga. Yoga’s series of postures and controlled breathing exercises may help you relax and manage stress.
- Meditation. During meditation, you focus your attention and eliminate the stream of jumbled thoughts that may be crowding your mind and causing stress.
- Acupuncture. With acupuncture, hair-thin needles are inserted under the skin. Acupuncture may help reduce anxiety and depression.
Side effects and risks of alcohol
You may have heard that regular light to moderate drinking (Men: Up to 2 drinks per day; Women: Up to 1 drink per day) can be good for the heart. Alcohol has biphasic and complex physiological effects that result in both higher and lower cardiovascular risk depending on the amount consumed, drinking frequency and the outcome under study 77, 78. For instance, moderate and high alcohol intake is associated with increased heart rate 79, electromechanical delay 80 and impaired fibrinolysis 81 within hours of intake but there are long-term improvements in blood pressure 82 and coagulation 83. In addition, the risk of cardiovascular events triggered by alcohol may be modified by usual drinking patterns 77.
With heavy or at-risk drinking (Men: More than 4 drinks on any day or more than 14 drinks per week / Women: More than 3 drinks on any day or more than 7 drinks per week), however, any potential benefits are outweighed by greater risks, including 84:
- Alcohol poisoning, a medical emergency that results from high blood alcohol levels 85.
- Injuries. Drinking too much increases your chances of being injured or even killed. Alcohol is a factor, for example, in about 60% of fatal burn injuries, drownings, and homicides 86; 50% of severe trauma injuries and sexual assaults and intimate partner violence 87, 88; and 40% of fatal motor vehicle crashes, suicides, and fatal falls 89.
- Risky sexual behaviors, including unprotected sex or sex with multiple partners. These behaviors can result in unintended pregnancy or sexually transmitted diseases, including HIV 90, 91.
- Health problems. People who drink heavily have a greater risk of liver disease, heart disease, sleep disorders, depression, stroke, bleeding from the stomach, sexually transmitted infections from unsafe sex, and several types of cancer. They may have problems managing diabetes, high blood pressure, and other conditions.
- Birth defects, miscarriage and stillbirth or fetal alcohol spectrum disorders (FASDs) among pregnant women. Drinking during pregnancy can cause brain damage and other serious problems in the baby. Because it is not yet known whether any amount of alcohol is safe for a developing baby, women who are pregnant or may become pregnant should not drink 89, 90, 92, 93.
- Alcohol use disorders. An alcohol use disorder is a medical condition that doctors can diagnose when a patient’s drinking causes distress or harm. In the United States, about 17 million people have an alcohol use disorder.
Beyond these physical and mental health risks, frequent heavy drinking also is linked with personal problems, including losing a driver’s license and having relationship troubles.
Long-Term Health Risks
Over time, excessive alcohol use can lead to the development of chronic diseases and other serious problems including:
- High blood pressure, heart disease, stroke, liver disease, and digestive problems 94.
- Cancer of the breast, mouth, throat, esophagus, liver, and colon 95.
- Learning and memory problems, including dementia and poor school performance 96.
- Mental health problems, including depression and anxiety 97.
- Social problems, including lost productivity, family problems, and unemployment 98.
- Alcohol dependence, or alcoholism 41.
By not drinking too much, you can reduce the risk of these short- and long-term health risks.
Table 2. Disease conditions which are by definition 100% alcohol-attributable
| Disease |
|---|
| Alcohol-induced pseudo-Cushing’s syndrome |
| Mental and behavioural disorders due to use of alcohol |
| Acute intoxication |
| Harmful use |
| Dependence syndrome |
| Withdrawal state |
| Withdrawal state with delirium |
| Psychotic disorder |
| Amnesic syndrome |
| Residual and late-onset psychotic disorder |
| Other mental and behavioural disorders |
| Unspecified mental and behavioural disorder |
| Degeneration of nervous system due to alcohol |
| Alcoholic polyneuropathy |
| Alcoholic myopathy |
| Alcoholic cardiomyopathy |
| Alcoholic gastritis |
| Alcoholic liver disease |
| Alcoholic fatty liver |
| Alcoholic hepatitis |
| Alcoholic fibrosis and sclerosis of liver |
| Alcoholic cirrhosis of liver |
| Alcoholic hepatic failure |
| Alcoholic liver disease, unspecified |
| Alcohol-induced acute pancreatitis |
| Alcohol-induced chronic pancreatitis |
| Maternal care for (suspected) damage to foetus from alcohol |
| Foetus and newborn affected by maternal use of alcohol |
| Foetal alcohol syndrome (dysmorphic) |
| Finding of alcohol in blood |
| Toxic effect of alcohol |
| Ethanol |
| Methanol |
| Other alcohols |
| Alcohol unspecified |
| Accidental poisoning by and exposure to alcohol |
| Intentional self-poisoning by and exposure to alcohol |
| Poisoning by and exposure to alcohol, undetermined intent |
| Evidence of alcohol involvement determined by blood alcohol level |
Table 3. Disease conditions which are by definition alcohol-attributable
| Tuberculosis |
| Human Immunodeficiency Virus / Acquired Immune Deficiency Syndrome (HIV/AIDS) |
| Mouth, nasopharynx, other pharynx and oropharynx cancer |
| Osophagus cancer |
| Stomach cancer |
| Colon and rectum cancer |
| Liver cancer |
| Larynx cancer |
| Trachea, bronchus and lung cancer |
| Breast cancer (female) |
| Other neoplasms |
| Diabetes mellitus |
| Alzheimer’s disease and other dementias |
| Unipolar depressive disorders |
| Epilepsy |
| Hypertensive heart disease |
| Ischemic heart disease |
| Cardiomyopathy |
| Conduction disorders and other dysrhythmias |
| Heart failure |
| Ischemic stroke |
| Hemorrhagic and other non-ischemic stroke |
| Esophageal varices |
| Lower respiratory infections: pneumonia |
| Cirrhosis of the liver |
| Gall bladder and bile duct disease |
| Pancreatitis |
| Other digestive diseases |
| Psoriasis |
| Abortion |
| Preterm birth complications |
Table 4. Injuries which are by definition 100% alcohol-attributable
| Category |
|---|
| Unintentional injuries |
| Transport injuries (including road traffic accidents) |
| Poisonings |
| Falls |
| Fires, heat, and hot substances |
| Drowning |
| Exposure to mechanical forces (including machinery accidents) |
| Natural disasters |
| Adverse effects of medical treatment |
| Injuries due to animal bites or contact with a marine animal |
| Other unintentional injuries |
| Intentional injuries |
| Self-inflicted injuries |
| Interpersonal violence |
| Collective violence |
| Legally sanctioned deaths |
Alcohol Effects on the Brain
You’re chatting with friends at a party and a waitress comes around with glasses of champagne. You drink one, then another, maybe even a few more. Before you realize it, you are laughing more loudly than usual and swaying as you walk. By the end of the evening, you are too slow to move out of the way of a waiter with a dessert tray and have trouble speaking clearly. The next morning, you wake up feeling dizzy and your head hurts. You may have a hard time remembering everything you did the night before.
These reactions illustrate how quickly and dramatically alcohol affects the brain. The brain is an intricate maze of connections that keeps our physical and psychological processes running smoothly. Disruption of any of these connections can affect how the brain works. Alcohol also can have longer-lasting consequences for the brain—changing the way it looks and works and resulting in a range of problems.
Most people do not realize how extensively alcohol can affect the brain. But recognizing these potential consequences will help you make better decisions about what amount of alcohol is appropriate for you.
The brain’s structure is complex. It includes multiple systems that interact to support all of your body’s functions—from thinking to breathing and moving.
These multiple brain systems communicate with each other through about a trillion tiny nerve cells called neurons. Neurons in the brain translate information into electrical and chemical signals the brain can understand. They also send messages from the brain to the rest of the body.
Chemicals called neurotransmitters carry messages between the neurons. Neurotransmitters can be very powerful. Depending on the type and the amount of neurotransmitter, these chemicals can either intensify or minimize your body’s responses, your feelings, and your mood. The brain works to balance the neurotransmitters that speed things up with the ones that slow things down to keep your body operating at the right pace.
Alcohol can slow the pace of communication between neurotransmitters in the brain 100.
There still is much we do not understand about how the brain works and how alcohol affects it. Researchers are constantly discovering more about how alcohol interrupts communication pathways in the brain and changes brain structure, and the resulting effects on behavior and functioning. A variety of research methods broaden our understanding in different ways:
- Brain Imaging – Various imaging tools, including structural magnetic resonance imaging (MRI), functional magnetic resonance imaging (fMRI), diffusion tensor imaging (DTI), and positron emission tomography (PET), are used to create pictures of the brain. MRI and DTI create images of brain structure, or what the brain looks like. fMRI looks at brain function, or what the brain is doing. It can detect changes in brain activity. PET scans look at changes in neurotransmitter function. All of these imaging techniques are useful to track changes in the alcoholic brain. For example, they can show how an alcoholic brain changes immediately after drinking stops, and again after a long period of sobriety, to check for possible relapses.
- Psychological Tests – Researchers also use psychological tests to evaluate how alcohol-related brain changes affect mental functioning. These tests demonstrate how alcohol affects emotions and personality, as well as how it compromises learning and memory skills.
- Animal Studies – Testing the effect of alcohol on animals’ brains helps researchers better understand how alcohol injures the human brain, and how abstinence can reverse this damage.
Using brain imaging and psychological tests, researchers have identified the regions of the brain most vulnerable to alcohol’s effects. These include:
- Cerebellum – This area controls motor coordination. Damage to the cerebellum results in a loss of balance and stumbling, and also may affect cognitive functions such as memory and emotional response.
- Limbic System – This complex brain system monitors a variety of tasks including memory and emotion. Damage to this area impairs each of these functions.
- Cerebral Cortex – Our abilities to think, plan, behave intelligently, and interact socially stem from this brain region. In addition, this area connects the brain to the rest of the nervous system. Changes and damage to this area impair the ability to solve problems, remember, and learn.
Alcohol Shrinks and Disturbs Brain Tissue
Heavy alcohol consumption—even on a single occasion—can throw the delicate balance of neurotransmitters off course. Alcohol can cause your neurotransmitters to relay information too slowly, so you feel extremely drowsy. Alcohol-related disruptions to the neurotransmitter balance also can trigger mood and behavioral changes, including depression, agitation, memory loss, and even seizures.
Long-term, heavy drinking causes alterations in the neurons, such as reductions in the size of brain cells. As a result of these and other changes, brain mass shrinks and the brain’s inner cavity grows bigger. These changes may affect a wide range of abilities, including motor coordination; temperature regulation; sleep; mood; and various cognitive functions, including learning and memory.
One neurotransmitter particularly susceptible to even small amounts of alcohol is called glutamate. Among other things, glutamate affects memory. Researchers believe that alcohol interferes with glutamate action, and this may be what causes some people to temporarily “black out,” or forget much of what happened during a night of heavy drinking.
Alcohol also causes an increased release of serotonin, another neurotransmitter, which helps regulate emotional expression, and endorphins, which are natural substances that may spark feelings of relaxation and euphoria as intoxication sets in. Researchers now understand that the brain tries to compensate for these disruptions. Neurotransmitters adapt to create balance in the brain despite the presence of alcohol. But making these adaptations can have negative results, including building alcohol tolerance, developing alcohol dependence, and experiencing alcohol withdrawal symptoms.
What factors make a difference?
Different people react differently to alcohol. That is because a variety of factors can influence your brain’s response to alcohol. These factors include 100:
- HOW MUCH AND HOW OFTEN YOU DRINK – The more you drink, the more vulnerable your brain is.
- YOUR GENETIC BACKGROUND AND FAMILY HISTORY OF ALCOHOLISM – Certain ethnic populations can have stronger reactions to alcohol, and children of alcoholics are more likely to become alcoholics themselves.
- YOUR PHYSICAL HEALTH – If you have liver or nutrition problems, the effects of alcohol will take longer to wear off.
Are brain problems reversible?
Abstaining from alcohol over several months to a year may allow structural brain changes to partially correct 100. Abstinence also can help reverse negative effects on thinking skills, including problem-solving, memory, and attention.
Other alcohol-related brain conditions
Liver Damage That Affects The Brain
Not only does alcoholic liver disease affect liver function itself, it also damages the brain. The liver breaks down alcohol—and the toxins it releases. During this process, alcohol’s byproducts damage liver cells. These damaged liver cells no longer function as well as they should and allow too much of these toxic substances, ammonia and manganese in particular, to travel to the brain.These substances proceed to damage brain cells, causing a serious and potentially fatal brain disorder known as hepatic encephalopathy 100.
Hepatic encephalopathy causes a range of problems, from less severe to fatal. These problems can include:
- Sleep disturbances
- Mood and personality changes
- Anxiety
- Depression
- Shortened attention span
- Coordination problems, including asterixis, which results in hand shaking or flapping
- Coma
- Death
Doctors can help treat hepatic encephalopathy with compounds that lower blood ammonia concentrations and with devices that help remove harmful toxins from the blood. In some cases, people suffering from hepatic encephalopathy require a liver transplant, which generally helps improve brain function.
Fetal Alcohol Spectrum Disorders
Alcohol can affect the brain at any stage of development—even before birth 100. Fetal alcohol spectrum disorders are the full range of physical, learning, and behavioral problems, and other birth defects that result from prenatal alcohol exposure. The most serious of these disorders, fetal alcohol syndrome, is characterized by abnormal facial features and is usually associated with severe reductions in brain function and overall growth. Fetal alcohol syndrome is the leading preventable birth defect associated with mental and behavioral impairment in the United States today. The brains of children with fetal alcohol syndrome are smaller than normal and contain fewer cells, including neurons. These deficiencies result in life-long learning and behavioral problems. Current research is investigating whether the brain function of children and adults with fetal alcohol syndrome can be improved with complex rehabilitative training, dietary supplements, or medications.
Alcohol Effects on the Heart
Your cardiovascular system consists of your heart, blood vessels, and blood. This system works constantly—every second of your life—delivering oxygen and nutrients to your cells, and carrying away carbon dioxide and other unnecessary material.
Your heart drives this process. It is a muscle that contracts and relaxes over and over again, moving the blood along the necessary path. Your heart beats about 100,000 times each day, pumping the equivalent of 2,000 gallons of blood throughout your body.
The two sides, or chambers, of the heart receive blood and pump it back into the body. The right ventricle of the heart pumps blood into the lungs to exchange carbon dioxide from the cells for oxygen. The heart relaxes to allow this blood back into its left chamber. It then pumps the oxygen-rich blood to tissues and organs. Blood passing through the kidneys allows the body to get rid of waste products. Electrical signals keep the heart pumping continuously and at the appropriate rate to propel this routine.
Americans know how prevalent heart disease is—about 1 in 12 of us suffer from it. What we don’t always recognize are the connections heart disease shares with alcohol. On the one hand, researchers have known for centuries that excessive alcohol consumption can damage the heart. Drinking a lot over a long period of time or drinking too much on a single occasion can put your heart—and your life—at risk. On the other hand, researchers now understand that drinking moderate amounts of alcohol can protect the hearts of some people from the risks of coronary artery disease.
Alcoholic Cardiomyopathy
Long-term heavy drinking weakens the heart muscle, causing a condition called alcoholic cardiomyopathy. A weakened heart droops and stretches and cannot contract effectively. As a result, it cannot pump enough blood to sufficiently nourish the organs. In some cases, this blood flow shortage causes severe damage to organs and tissues. Symptoms of cardiomyopathy include shortness of breath and other breathing difficulties, fatigue, swollen legs and feet, and irregular heartbeat. It can even lead to heart failure.
Cardiac Arrhythmias
Both binge drinking and long-term drinking can affect how quickly a heart beats.The heart depends on an internal pacemaker system to keep it pumping consistently and at the right speed. Alcohol disturbs this pacemaker system and causes the heart to beat too rapidly, or irregularly. These heart rate abnormalities are called arrhythmias. Two types of alcohol induced arrhythmias are:
- Atrial Fibrillation – In this form of arrhythmia, the heart’s upper, or atrial, chambers shudder weakly but do not contract. Blood can collect and even clot in these upper chambers. If a blood clot travels from the heart to the brain, a stroke can occur; if it travels to other organs such as the lungs, an embolism, or blood vessel blockage, occurs.
- Ventricular Tachycardia – This form of arrhythmia occurs in the heart’s lower, or ventricular, chambers. Electrical signals travel throughout the heart’s muscles, triggering contractions that keep blood flowing at the right pace. Alcohol-induced damage to heart muscle cells can cause these electrical impulses to circle through the ventricle too many times, causing too many contractions. The heart beats too quickly, and so does not fill up with enough blood between each beat. As a result, the rest of the body does not get enough blood. Ventricular tachycardia causes dizziness, lightheadedness, unconsciousness, cardiac arrest, and even sudden death. Drinking to excess on a particular occasion, especially when you generally don’t drink, can trigger either of these irregularities. In these cases, the problem is nicknamed “holiday heart syndrome,” because people who don’t usually drink may consume too much alcohol at parties during the holiday season. Over the long-term, chronic drinking changes the course of electrical impulses that drive the heart’s beating, which creates arrhythmia.
Strokes
A stroke occurs when blood cannot reach the brain. In about 80 percent of strokes, a blood clot prevents blood flow to the brain. These are called ischemic strokes. Sometimes, blood accumulates in the brain, or in the spaces surrounding it. This causes hemorrhagic strokes.
Both binge drinking and long-term heavy drinking can lead to strokes even in people without coronary heart disease. Recent studies show that people who binge drink are about 56 percent more likely than people who never binge drink to suffer an ischemic stroke over 10 years. Binge drinkers also are about 39 percent more likely to suffer any type of stroke than people who never binge drink.
In addition, alcohol exacerbates the problems that often lead to strokes, including hypertension, arrhythmias, and cardiomyopathy.
Hypertension
Chronic alcohol use, as well as binge drinking, can cause high blood pressure, or hypertension. Your blood pressure is a measurement of the pressure your heart creates as it beats, and the pressure inside your veins and arteries. Healthy blood vessels stretch like elastic as the heart pumps blood through them.
Hypertension develops when the blood vessels stiffen, making them less flexible. Heavy alcohol consumption triggers the release of certain stress hormones that in turn constrict blood vessels.This elevates blood pressure. In addition, alcohol may affect the function of the muscles within the blood vessels, causing them to constrict and elevate blood pressure.
Alcohol Effects on the Liver
Your liver works hard to keep your body productive and healthy. It stores energy and nutrients. It generates proteins and enzymes your body uses to function and ward off disease. It also rids your body of substances that can be dangerous—including alcohol.
The liver breaks down most of the alcohol a person consumes. But the process of breaking alcohol down generates toxins even more harmful than alcohol itself. These by-products damage liver cells, promote inflammation, and weaken the body’s natural defenses. Eventually, these problems can disrupt the body’s metabolism and impair the function of other organs.
Because the liver plays such a vital role in alcohol detoxification, it is especially vulnerable to damage from excessive alcohol.
Liver disease is one of the leading causes of illness and death in the United States. More than 2 million Americans suffer from liver disease caused by alcohol.
In general, liver disease strikes people who drink heavily over many years.
While many of us recognize that excessive alcohol consumption can lead to liver disease, we might not know why. Understanding the connections between alcohol and the liver can help you make smarter decisions about drinking and take better control of your health.
Alcoholic Liver Disease
Heavy drinking—even for just a few days at a time—can cause fat to build up in the liver. This condition, called steatosis, or fatty liver, is the earliest stage of alcoholic liver disease and the most common alcohol-induced liver disorder. The excessive fat makes it more difficult for the liver to operate and leaves it open to developing dangerous inflammations, like alcoholic hepatitis.
For some, alcoholic hepatitis does not present obvious symptoms. For others, though, alcoholic hepatitis can cause fever, nausea, appetite loss, abdominal pain, and even mental confusion. As it increases in severity, alcoholic hepatitis dangerously enlarges the liver, and causes jaundice, excessive bleeding, and clotting difficulties.
Another liver condition associated with heavy drinking is fibrosis, which causes scar tissue to build up in the liver. Alcohol alters the chemicals in the liver needed to break down and remove this scar tissue. As a result, liver function suffers.
If you continue to drink, this excessive scar tissue builds up and creates a condition called cirrhosis, which is a slow deterioration of the liver. Cirrhosis prevents the liver from performing critical functions, including managing infections, removing harmful substances from the blood, and absorbing nutrients.
A variety of complications, including jaundice, insulin resistance and type 2 diabetes, and even liver cancer, can result as cirrhosis weakens liver function.
Risk factors ranging from genetics and gender, to alcohol accessibility, social customs around drinking, and even diet can affect a person’s individual susceptibility to alcoholic liver disease. Statistics show that about one in five heavy drinkers will develop alcoholic hepatitis, while one in four will develop cirrhosis.
The good news is that a variety of lifestyle changes can help treat alcoholic liver disease. The most critical lifestyle change is abstinence from alcohol. Quitting drinking will help prevent further injury to your liver. Cigarette smoking, obesity, and poor nutrition all contribute to alcoholic liver disease. It is important to stop smoking and improve your eating habits to keep liver disease in check. But when conditions like cirrhosis become severe, a liver transplant may be the primary treatment option.
Alcohol Effects on the Pancreas
The pancreas plays an important role in food digestion and its conversion into fuel to power your body. It sends enzymes into the small intestine to digest carbohydrates, proteins, and fat. It also secretes insulin and glucagon, hormones that regulate the process of utilizing glucose, the body’s main source of energy. Insulin and glucagon control glucose levels, which helps all cells use the energy glucose provides. Insulin also ensures that extra glucose gets stored away as either glycogen or fat.
When you drink, alcohol damages pancreatic cells and influences metabolic processes involving insulin. This process leaves the pancreas open to dangerous inflammations.
Each year, acute pancreatitis sends more than 200,000 Americans to the hospital. Many of those who suffer from pancreatic problems are also heavy drinkers. Habitual and excessive drinking damages the pancreas, and commonly causes pancreatitis.
Learning more about the links between alcohol and pancreatic problems can help you make better decisions to protect your health.
Alcohol and the Pancreas
A pancreas unaffected by alcohol sends enzymes out to the small intestine to metabolize food. Alcohol jumbles this process. It causes the pancreas to secrete its digestive juices internally, rather than sending the enzymes to the small intestine. These enzymes, as well as acetaldehyde—a substance produced from metabolizing, or breaking down the alcohol—are harmful to the pancreas. If you consume alcohol excessively over a long time, this continued process can cause inflammation, as well as swelling of tissues and blood vessels.
This inflammation is called pancreatitis, and it prevents the pancreas from working properly. Pancreatitis occurs as a sudden attack, called acute pancreatitis. As excessive drinking continues, the inflammation can become constant. This condition is known as chronic pancreatitis.
Pancreatitis is also a risk factor for the development of pancreatic cancer.
A heavy drinker may not be able to detect the build-up of pancreatic damage until the problems set off an attack.
An acute pancreatic attack causes symptoms including:
- Abdominal pain, which may radiate up the back
- Nausea and vomiting
- Fever
- Rapid heart rate
- Diarrhea
- Sweating
Chronic pancreatitis causes these symptoms as well as severe abdominal pain, significant reduction in pancreatic function and digestion, and blood sugar problems. Chronic pancreatitis can slowly destroy the pancreas and lead to diabetes or even death.
While a single drinking binge will not automatically lead to pancreatitis, the risk of developing the disease increases as excessive drinking continues over time.
These risks apply to all heavy drinkers, but only about 5 percent of people with alcohol dependence develop pancreatitis. Some people are more susceptible to the disease than others, but researchers have not yet identified exactly what environmental and genetic factors play the biggest role.
Abstinence from alcohol can slow the progression of pancreatitis and reduce its painful symptoms.A low-fat diet also may help. It is also critical to guard against infections and to get supportive treatment. Treatment options, including enzyme-replacement therapy or insulin, can improve pancreatic function. In some cases, surgery is necessary to relieve pain, clear blockages, and reduce attacks.
The effects of alcoholic pancreatitis can be managed, but not easily reversed.
Alcohol and Cancer
Genetics, environment, and lifestyle habits can all heighten your risk of getting cancer. We can’t do anything to change our genes, and we often can’t do much to change our environment. But lifestyle habits are a different story.
Drinking too much alcohol is one lifestyle habit that can increase your risk of developing certain cancers. This does not mean that anyone who drinks too much will develop cancer. But numerous studies do show the more you drink, the more you increase your chances of developing certain types of cancer.
For example, a group of Italy-based scientists reviewed more than 200 studies examining alcohol’s impact on cancer risk.The collective results of these studies clearly demonstrate that the more you drink, the higher your risk for developing a variety of cancers.The National Cancer Institute identifies alcohol as a risk factor for the following types of cancer:
- Mouth
- Esophagus
- Pharynx
- Larynx
- Liver
- Breast
At least 7 out of 10 people with mouth cancer drink heavily. Drinking five or more drinks per day can also increase your risk of developing other types of cancers, including colon or rectal cancer. In fact, summary estimates from the recent World Cancer Research Fund report indicate that women who drink five standard alcohol drinks each day have about 1.2 times the risk of developing colon or rectal cancer than women who do not drink at all.
People who drink are also more likely to smoke, and the combination increases the risk significantly. Smoking alone is a known risk factor for some cancers. But smoking and drinking together intensifies the cancer-causing properties of each substance. The overall effect poses an even greater risk.
The risk of throat and mouth cancers is especially high because alcohol and tobacco both come in direct contact with those areas. Overall, people who drink and smoke are 15 times more likely to develop cancers of the mouth and throat than nondrinkers and nonsmokers. In addition, recent studies estimate that alcohol and tobacco together are responsible for:
- 80 percent of throat and mouth cancer in men
- 65 percent of throat and mouth cancer in women
- 80 percent of esophageal squamous cell carcinoma, a type of esophagus cancer
- 25 to 30 percent of all liver cancers.
Scientists are still trying to figure out exactly how and why alcohol can promote cancer. There are a variety of possible explanations.
One explanation is that alcohol itself is not the primary trigger for cancer.We know that metabolizing, or breaking down, alcohol results in harmful toxins in the body. One of these toxins is called acetylaldehyde. Acetylaldehyde damages the genetic material in cells—and renders the cells incapable of repairing the damage. It also causes cells to grow too quickly, which makes conditions ripe for genetic changes and mistakes. Cancer can develop more easily in cells with damaged genetic material.
In addition, recent animal studies have shown that as cells try to break down alcohol, they cause the body to produce additional amounts of a protein called vascular endothelial growth factor (VEGF). VEGF promotes the growth of blood vessels and organ tissue. But, the flip side of having too much VEGF is that it allows blood vessels to grow in cancer cells that would die on their own. This allows the cancer cells to develop into tumors.
We also know that alcohol can damage the liver, causing cirrhosis. Cirrhosis results when too much scar tissue builds up within the liver and leaves it unable to perform its vital functions. One of the many complications that can result from cirrhosis is liver cancer.
Hormones may be the link between alcohol and breast cancer. Alcohol can increase the amounts of some hormones in the body, including estrogen. An excess of estrogen may lead to breast cancer.
Finally, genetics may play a role in preventing some heavy drinkers from developing cancer. A European research team examined 9,000 people with similar lifestyle habits to determine why some of them developed mouth and throat cancers, and some did not. Of the participants who were heavy drinkers, those who did not develop cancers had a particular genetic alteration that enabled them to break down alcohol about 100 times faster than in those without it. The study suggested that this gene is the reason why some people are less likely to develop cancer in response to heavy drinking.
Fortunately, studies show that you can reduce your risk for cancer by drinking less. A recent Canadian report analyzed studies from 1966 through 2006 and concluded that risk reduction is possible, specifically for head and neck cancers.The study found that as people abstained from drinking, their risk for developing cancer plunged. After 20 years of abstinence, former drinkers had the same risk for head and neck cancers as people who never drank.
Alcohol and Cancer in Women
One recent, groundbreaking study followed the drinking habits of 1.2 million middle-aged women over 7 years. The study found that alcohol increases women’s chances of developing cancers of the breast,mouth, throat, rectum, liver, and esophagus. The researchers link alcohol to about 13 percent of these cancer cases.
In addition, the study concluded that cancer risk increases no matter how little or what kind of alcohol a woman drinks. Even one drink a day can raise risk, and it continues to rise with each additional drink. While men did not participate in this study, the researchers believe this risk is likely similar for men.
This study also attributes about 11 percent of all breast cancer cases to alcohol. That means that of the 250,000 breast cancer cases diagnosed in the United States in 2008, about 27,000 may stem from alcohol.
Alcohol Effects on the Immune System
Your immune system is often compared to an army. This army defends your body from infection and disease. Your skin and the mucous that lines your respiratory and gastrointestinal tracts help block bacteria from entering or staying in your body. If foreign substances somehow make it through these barriers, your immune system kicks into gear with two defensive systems: innate and adaptive.
The innate system exists in your body before you are exposed to foreign substances like bacteria, viruses, fungi, or parasites. These substances, which are called antigens, can invade your body and make you sick. The components of the innate system include:
- White Blood Cells – White blood cells form your first line of defense against infection.They surround and swallow foreign bodies quickly.
- Natural Killer (NK) Cells – Natural Killers are special white blood cells that detect and destroy cells infected with cancer or viruses.
- Cytokines – White blood cells send out these chemical messengers directly to an infected site. Cytokines trigger inflammatory responses, like dilating blood vessels and increasing blood flow to the affected area. They also call on more white blood cells to swarm an infected area.
The adaptive system kicks in after you are exposed to an infection for the first time. The next time you encounter the same infection, your adaptive system fights it off even faster and more efficiently than the first time. The components of the adaptive system include:
- T-lymphocyte cells – T-cells reinforce the work of white blood cells by targeting individual foreign substances.T-cells can identify and destroy a vast array of bacteria and viruses.They can also kill infected cells and secrete cytokines.
- B-lymphocyte cells – B-cells produce antibodies that fight off harmful substances by sticking to them and making them stand out to other immune cells.
- Antibodies – After B-cells encounter antigens, they produce antibodies.These are proteins that target specific antigens and then remember how to combat the antigen.
Drinking too much alcohol weakens the immune system, making your body a much easier target for disease. Understanding the effect alcohol can have on your immune system can inform the decisions you make about drinking alcohol.
Alcohol suppresses both the innate and the adaptive immune systems. Chronic alcohol use reduces the ability of white blood cells to effectively engulf and swallow harmful bacteria. Excessive drinking also disrupts the production of cytokines, causing your body to either produce too much or not enough of these chemical messengers. An abundance of cytokines can damage your tissues, whereas a lack of cytokines leaves you open to infection.
Chronic alcohol use also suppresses the development of T-cells and may impair the ability of Natural Killer (NK) Cells to attack tumor cells. This reduced function makes you more vulnerable to bacteria and viruses, and less capable of destroying cancerous cells.
With a compromised immune system, chronic drinkers are more liable to contract diseases like pneumonia and tuberculosis than people who do not drink too much. There is also data linking alcohol’s damage to the immune system with an increased susceptibility to contracting HIV infection. HIV develops faster in chronic drinkers who already have the virus.
Drinking a lot on a single occasion also can compromise your immune system. Drinking to intoxication can slow your body’s ability to produce cytokines that ward off infections by causing inflammations.Without these inflammatory responses, your body’s ability to defend itself against bacteria is significantly reduced. A recent study shows that slower inflammatory cytokine production can reduce your ability to fight off infections for up to 24 hours after getting drunk.
At this point in time, scientists do not know whether abstinence, reduced drinking, or other measures will help reverse the effects of alcohol on the immune system. Nevertheless, it is important to keep in mind that avoiding drinking helps minimize the burden on your immune system, particularly if you are fighting a viral or bacterial infection.
Alcohol and Pregnancy
When You Are Pregnant…Drinking Can Hurt Your Baby 101.
When you are pregnant, your baby grows inside you. Everything you eat and drink while you are pregnant affects your baby. If you drink alcohol, it can hurt your baby’s growth. Your baby may have physical and behavioral problems that can last for the rest of his or her life. Children born with the most serious problems caused by alcohol have fetal alcohol syndrome.
Children with fetal alcohol syndrome may:
- Be born small.
- Have problems eating and sleeping.
- Have problems seeing and hearing.
- Have trouble following directions and learning how to do simple things.
- Have trouble paying attention and learning in school.
- Need special teachers and schools.
- Have trouble getting along with others and controlling their behavior.
- Need medical care all their lives.
Here are some questions you may have about alcohol and drinking while you are pregnant.
Can I drink alcohol if I’m are pregnant?
No. Do not drink alcohol when you are pregnant. Why? Because when you drink alcohol, so does your baby. Think about it. Everything you drink, your baby also drinks.
Is any kind of alcohol safe to drink during pregnancy?
No. Drinking any kind of alcohol when you are pregnant can hurt your baby. Alcoholic drinks are beer, wine, wine coolers, liquor, or mixed drinks. A glass of wine, a can of beer, and a mixed drink all have about the same amount of alcohol.
What if you drank during your last pregnancy and your baby was fine?
Every pregnancy is different. Drinking alcohol may hurt one baby more than another. You could have one child that is born healthy, and another child that is born with problems.
Will these problems go away?
No. These problems will last for a child’s whole life. People with severe problems may not be able to take care of themselves as adults. They may never be able to work.
What if I’m pregnant and have been drinking?
If you drank alcohol before you knew you were pregnant, stop drinking now. You will feel better and your baby will have a good chance to be born healthy. If you want to get pregnant, do not drink alcohol. You may not know you are pregnant right away. Alcohol can hurt a baby even when you are only 1 or 2 months pregnant.
How you can stop drinking?
There are many ways to help yourself stop drinking. You do not have to drink when other people drink. If someone gives you a drink, it is OK to say no. Stay away from people or places that make you drink. Do not keep alcohol at home.
Support Groups for Alcohol use disorder
Because an alcohol use disorder can be a chronic relapsing disease, persistence is key. It is rare that someone would go to treatment once and then never drink again. More often, people must repeatedly try to quit or cut back, experience recurrences, learn from them, and then keep trying. For many, continued followup with a treatment provider is critical to overcoming problem drinking. Support groups help many people who are dealing with alcohol use and relapses.
Relapse is common among people who overcome alcohol problems. People with drinking problems are most likely to relapse during periods of stress or when exposed to people or places associated with past drinking.
Just as some people with diabetes or asthma may have flare-ups of their disease, a relapse to drinking can be seen as a temporary set-back to full recovery and not a complete failure. Seeking professional help can prevent relapse — behavioral therapies can help people develop skills to avoid and overcome triggers, such as stress, that might lead to drinking. Most people benefit from regular checkups with a treatment provider. Medications also can deter drinking during times when individuals may be at greater risk of relapse (e.g., divorce, death of a family member).
If you cannot stop drinking, GET HELP. You may have a disease called alcoholism. There are programs that can help you stop drinking. They are called alcohol treatment programs. Your doctor or nurse can find a program to help you. Even if you have been through a treatment program before, try it again. There are also programs just for women.
Consider joining Alcoholics Anonymous or another mutual support group (see links below). Recovering people who attend support groups regularly do better than those who do not. Groups can vary widely, so shop around for one that’s comfortable. You’ll get more out of it if you become actively involved by having a sponsor and reaching out to other members for assistance.
- Alcoholics Anonymous (https://www.aa.org)
- Moderation Management (https://moderation.org)
- Secular Organizations for Sobriety (https://www.sossobriety.org)
- SMART Recovery (https://www.smartrecovery.org)
- Women for Sobriety (https://womenforsobriety.org)
- Al-Anon Family Groups (https://al-anon.org)
- Adult Children of Alcoholics (https://adultchildren.org)
- National Council on Alcoholism and Drug Dependence (https://recovered.org)
- National Institute on Alcohol Abuse and Alcoholism (https://www.niaaa.nih.gov)
- National Organization on Fetal Alcohol Syndrome (https://fasdunited.org)
- Substance Abuse and Mental Health Services Administration (https://findtreatment.gov)
Tips to try reduce your risks of alcohol use disorder
Small changes can make a big difference in reducing your chances of having alcohol-related problems. Whatever strategies you choose, give them a fair trial. If one approach doesn’t work, try something else. But if you haven’t made progress in cutting down after 2 to 3 months, consider quitting drinking altogether, seeking professional help, or both 102.
Here are some strategies to try 102 and you can add your own at the end. Check off perhaps two or three to try in the next week or two.
- Keep track. Keep track of how much you drink. Find a way that works for you: Carry a drinking tracker card in your wallet, make check marks on a kitchen calendar, or enter notes in a mobile phone notepad or personal digital assistant. Making note of each drink before you drink it may help you slow down when needed.
- Count and measure. Know the standard drink sizes so you can count your drinks accurately. Measure drinks at home. Away from home, it can be hard to keep track, especially with mixed drinks, and at times, you may be getting more alcohol than you think. With wine, you may need to ask the host or server not to “top off” a partially filled glass.
- Set goals. Decide how many days a week you want to drink and how many drinks you’ll have on those days. It’s a good idea to have some days when you don’t drink. People who always stay within the low-risk limits when they drink have the lowest rates of alcohol-related problems.
- Pace and space. When you do drink, pace yourself. Sip slowly. Have no more than one standard drink with alcohol per hour. Have “drink spacers”—make every other drink a non-alcoholic one, such as water, soda, or juice.
- Include food. Don’t drink on an empty stomach. Eat some food so the alcohol will be absorbed into your system more slowly.
- Find alternatives. If drinking has occupied a lot of your time, then fill free time by developing new, healthy activities, hobbies, and relationships, or renewing ones you’ve missed. If you have counted on alcohol to be more comfortable in social situations, manage moods, or cope with problems, then seek other, healthy ways to deal with those areas of your life.
- Avoid “triggers.” What triggers your urge to drink? If certain people or places make you drink even when you don’t want to, try to avoid them. If certain activities, times of day, or feelings trigger the urge, plan something else to do instead of drinking. If drinking at home is a problem, keep little or no alcohol there.
- Plan to handle urges. When you cannot avoid a trigger and an urge hits, consider these options: Remind yourself of your reasons for changing (it can help to carry them in writing or store them in an electronic message you can access easily). Or talk things through with someone you trust. Or get involved with a healthy, distracting activity, such as physical exercise or a hobby that doesn’t involve drinking. Or, instead of fighting the feeling, accept it and ride it out without giving in, knowing that it will soon crest like a wave and pass. Also, see the short module to help you handle urges to drink.
- Know your “NO”. You’re likely to be offered a drink at times when you don’t want one. Have a polite, convincing “no, thanks” ready. The faster you can say no to these offers, the less likely you are to give in. If you hesitate, it allows you time to think of excuses to go along. Also, see the short module to help you build drink refusal skills.
Handling your urges to drink
Plan ahead to stay in control
As you change your drinking, it’s normal and common to have urges or a craving for alcohol. The words “urge” and “craving” refer to a broad range of thoughts, physical sensations, or emotions that tempt you to drink, even though you have at least some desire not to. You may feel an uncomfortable pull in two directions or sense a loss of control 103.
Fortunately, urges to drink are short-lived, predictable, and controllable. This short strategy offers a recognize-avoid-cope approach commonly used in cognitive behavioral therapy, which helps people to change unhelpful thinking patterns and reactions. It also provides worksheets to help you uncover the nature of your urges to drink and to make a plan for handling them.
With time, and by practicing new responses, you’ll find that your urges to drink will lose strength, and you’ll gain confidence in your ability to deal with urges that may still arise at times. If you are having a very difficult time with urges, or do not make progress with the strategies in this module after a few weeks, then consult a doctor or therapist for support. In addition, some new, non-habit forming medications can reduce the desire to drink or lessen the rewarding effect of drinking so it is easier to stop.
Recognize two types of “triggers”
An urge to drink can be set off by external triggers in the environment and internal ones within yourself.
- External triggers are people, places, things, or times of day that offer drinking opportunities or remind you of drinking. These “high-risk situations” are more obvious, predictable, and avoidable than internal triggers.
- Internal triggers can be puzzling because the urge to drink just seems to “pop up.” But if you pause to think about it when it happens, you’ll find that the urge may have been set off by a fleeting thought, a positive emotion such as excitement, a negative emotion such as frustration, or a physical sensation such as a headache, tension, or nervousness.
Consider tracking and analyzing your urges to drink for a couple of weeks. This will help you become more aware of when and how you experience urges, what triggers them, and ways to avoid or control them. A sample “urge to drink” tracking form is provided below.
Urge To Drink Tracker Form – Record the details as soon after an urge as possible.
| Date/time | Situation (people, place) or trigger (incident, feelings) | What was the urge like? | How I responded | What I’ll do next time | |
|---|---|---|---|---|---|
| Was it a thought? Emotion? Physical sensation? | Rate it from 1 (mild) to 10 (strong) | ||||
Footnote: You can Print a copy of this form and carry it with you from here: https://www.rethinkingdrinking.niaaa.nih.gov/Tools/Interactive-worksheets-and-more/Stay-in-control/Coping-With-Urges-To-Drink-urge-tracker.aspx
[Source: U.S. Department of Health and Human Services. Rethinking Drinking 104]Avoid high-risk situations
In many cases, your best strategy will be to avoid taking the chance that you’ll have an urge, then slip and drink. At home, keep little or no alcohol. Socially, avoid activities involving drinking. If you feel guilty about turning down an invitation, remind yourself that you are not necessarily talking about “forever.” When the urges subside or become more manageable, you may decide to ease gradually into some situations you now choose to avoid. In the meantime, you can stay connected with friends by suggesting alternate activities that don’t involve drinking.
Building your drink refusal skills
- Plan ahead to stay in control
Even if you are committed to changing your drinking, “social pressure” to drink from friends or others can make it hard to cut back or quit. This short module offers a recognize-avoid-cope approach commonly used in cognitive-behavioral therapy, which helps people to change unhelpful thinking patterns and reactions. It also provides links to worksheets to help you get started with your own plan to resist pressure to drink.
Recognize two types of pressure
The first step is to become aware of the two different types of social pressure to drink alcohol—direct and indirect.
- Direct social pressure is when someone offers you a drink or an opportunity to drink.
- Indirect social pressure is when you feel tempted to drink just by being around others who are drinking—even if no one offers you a drink.
Take a moment to think about situations where you feel direct or indirect pressure to drink or to drink too much. You can use the form below to write them down. Then, for each situation, choose some resistance strategies from below,or come up with your own. When you’re done, you can print the form or email it to yourself.
- Avoid pressure when possible
For some situations, your best strategy may be avoiding them altogether. If you feel guilty about avoiding an event or turning down an invitation, remind yourself that you are not necessarily talking about “forever.” When you have confidence in your resistance skills, you may decide to ease gradually into situations you now choose to avoid. In the meantime, you can stay connected with friends by suggesting alternate activities that don’t involve drinking.
Cope with situations you can’t avoid
- Know your “NO”
When you know alcohol will be served, it’s important to have some resistance strategies lined up in advance. If you expect to be offered a drink, you’ll need to be ready to deliver a convincing “no thanks.” Your goal is to be clear and firm, yet friendly and respectful. Avoid long explanations and vague excuses, as they tend to prolong the discussion and provide more of an opportunity to give in. Here are some other points to keep in mind:
- Don’t hesitate, as that will give you the chance to think of reasons to go along
- Look directly at the person and make eye contact
- Keep your response short, clear, and simple
The person offering you a drink may not know you are trying to cut down or stop, and his or her level of insistence may vary. It’s a good idea to plan a series of responses in case the person persists, from a simple refusal to a more assertive reply. Consider a sequence like this:
- No, thank you.
- No, thanks, I don’t want to.
- You know, I’m (cutting back/not drinking) now (to get healthier/to take care of myself/because my doctor said to). I’d really appreciate it if you’d help me out.
You can also try the “broken record” strategy. Each time the person makes a statement, you can simply repeat the same short, clear response. You might want to acknowledge some part of the person’s points (“I hear you…”) and then go back to your broken-record reply (“…but no thanks”). And if words fail, you can walk away.
- Script and practice your “NO”
Many people are surprised at how hard it can be to say no the first few times. You can build confidence by scripting and practicing your lines. First imagine the situation and the person who’s offering the drink. Then write both what the person will say and how you’ll respond, whether it’s a broken record strategy (mentioned above) or your own unique approach. Rehearse it aloud to get comfortable with your phrasing and delivery. Also, consider asking a supportive person to role-play with you, someone who would offer realistic pressure to drink and honest feedback about your responses. Whether you practice through made-up or real-world experiences, you’ll learn as you go. Keep at it, and your skills will grow over time.
- Try other strategies
In addition to being prepared with your “no thanks,” consider these strategies:
- Have non-alcoholic drinks always in hand if you’re quitting, or as “drink spacers” between drinks if you’re cutting back
- Keep track of every drink if you’re cutting back so you stay within your limits
- Ask for support from others to cope with temptation
- Plan an escape if the temptation gets too great
- Ask others to refrain from pressuring you or drinking in your presence (this can be hard)
If you have successfully refused drink offers before, then recall what worked and build on it.
Remember, it’s your choice
How you think about any decision to change can affect your success. Many people who decide to cut back or quit drinking think, “I am not allowed to drink,” as if an external authority were imposing rules on them. Thoughts like this can breed resentment and make it easier to give in. It’s important to challenge this kind of thinking by telling yourself that you are in charge, that you know how you want your life to be, and that you have decided to make a change.
Similarly, you may worry about how others will react or view you if you make a change. Again, challenge these thoughts by remembering that it’s your life and your choice, and that your decision should be respected.
Plan to resist pressure to drink
It’s not possible to avoid all high-risk situations or to block internal triggers, so you’ll need a range of strategies to handle urges to drink. Here are some options:
- Remind yourself of your reasons for making a change. Carry your top reasons on a wallet card or in an electronic message that you can access easily, such as a mobile phone notepad entry or a saved email.
- Talk it through with someone you trust. Have a trusted friend on standby for a phone call, or bring one along to high-risk situations.
- Distract yourself with a healthy, alternative activity. For different situations, come up with engaging short, mid-range, and longer options, like texting or calling someone, watching short online videos, lifting weights to music, showering, meditating, taking a walk, or doing a hobby.
- Challenge the thought that drives the urge. Stop it, analyze the error in it, and replace it. Example: “It couldn’t hurt to have one little drink. WAIT a minute—what am I thinking? One could hurt, as I’ve seen ‘just one’ lead to lots more. I am sticking with my choice not to drink.”
- Ride it out without giving in. Instead of fighting an urge, accept it as normal and temporary. As you ride it out, keep in mind that it will soon crest like an ocean wave and pass.
- Leave high-risk situations quickly and gracefully. It helps to plan your escape in advance.
Are you ready to change your drinking ?
If so, choose whether to cut down or quit and make a change plan. Don’t be surprised if you continue to have mixed feelings. You may need to re-make your decision several times before becoming comfortable with it.
If not, consider these suggestions in the meantime:
- Keep track of how often and how much you’re drinking.
- Notice how drinking affects you.
- Make or re-make a list of pros and cons about changing.
- Deal with other priorities that may be in the way.
- Ask for support from your doctor, a friend, or someone else you trust.
- Take steps to be safe.
- Come back to visit this site from time to time.
Don’t wait for a crisis or to “hit bottom.”
When someone is drinking too much, making a change earlier is likely to be more successful and less destructive to individuals and their families.
How to cut down or to quit drinking alcohol
If you’re considering changing your drinking, you’ll need to decide whether to cut down or to quit. It’s a good idea to discuss different options with a doctor, a friend, or someone else you trust.
Quitting is strongly advised if you:
- Try cutting down but cannot stay within the limits you set.
- Have had an alcohol use disorder or now have symptoms.
- Have a physical or mental condition that is caused or worsened by drinking.
- Are taking a medication that interacts with alcohol.
- Are or may become pregnant.
If none of the conditions above apply to you, then talk with your doctor to determine whether you should cut down or quit based on factors such as:
- Family history of alcohol problems
- Your age
- Whether you’ve had drinking-related injuries
- Symptoms such as sleep disorders and sexual dysfunction
Planning for change
Even when you have committed to making a change, you still may have mixed feelings at times. Making a written “My Alcohol Change Plan” will help you to solidify your goals, why you want to reach them, and how you plan to do it.
A sample format is provided below. After filling it in, you can print it or email it to yourself.
- Goal:(select one) I want to drink no more than drink(s) on any day and no more than drink(s) per week OR I want to stop drinking.
- Timing: I will start on this date:
- Reasons: My most important reasons to make these changes are:
- Strategies: I will use these strategies:
- People: The people who can help me are (names and how they can help):
- Signs of success: I will know my plan is working if:
- Possible roadblocks: Some things that might interfere—and how I’ll handle them:
Reminder strategies
Change can be hard, so it helps to have concrete reminders of why and how you’ve decided to do it. Some standard options include carrying a change plan in your wallet or posting sticky notes at home. Also consider these high-tech ideas:
- Fill out a change plan, email it to your personal (non-work) account, store it in a private online folder, and review it weekly.
- Store your goals, reasons, or strategies in your mobile phone as short text messages or notepad entries that you can retrieve when an urge hits.
- Set up automated mobile phone or email calendar alerts that deliver reminders when you choose, such as a few hours before you usually go out. (Email providers such as Gmail and Yahoo mail have online calendars with alert options.)
- Create passwords that are motivating phrases in code, which you’ll reinforce each time you log in, such as 1Day@aTime, 1stThings1st!, or 0Pain=0Gain.
Social support to stop drinking
One potential challenge when people stop drinking is rebuilding a life without alcohol. It may be important to:
- Educate family and friends.
- Develop new interests and social groups.
- Find rewarding ways to spend your time that don’t involve alcohol.
- Ask for help from others.
When asking for support from friends or significant others, be specific. This could include:
- Not offering you alcohol
- Not using alcohol around you
- Giving words of support and withholding criticism
- Not asking you to take on new demands right now
- Going to a group like Alcoholics Anonymous 105
Consider joining Alcoholics Anonymous or another mutual support group (see links below). Recovering people who attend support groups regularly do better than those who do not. Groups can vary widely, so shop around for one that’s comfortable. You’ll get more out of it if you become actively involved by having a sponsor and reaching out to other members for assistance.
- Alcoholics Anonymous (https://www.aa.org)
- Moderation Management (https://moderation.org)
- Secular Organizations for Sobriety (https://www.sossobriety.org)
- SMART Recovery (https://www.smartrecovery.org)
- Women for Sobriety (https://womenforsobriety.org)
- Al-Anon Family Groups (https://al-anon.org)
- Adult Children of Alcoholics (https://adultchildren.org)
- National Council on Alcoholism and Drug Dependence (https://recovered.org)
- National Institute on Alcohol Abuse and Alcoholism (https://www.niaaa.nih.gov)
- National Organization on Fetal Alcohol Syndrome (https://fasdunited.org)
- Substance Abuse and Mental Health Services Administration (https://findtreatment.gov)
Alcohol Addiction
Alcohol use disorder (alcohol addiction) is a medical condition that doctors diagnose when a patient’s drinking causes distress or harm. The condition can range from mild to severe and is diagnosed when a patient answers “yes” to two or more of the following questions 59.
What are symptoms of an alcohol addiction or alcohol use disorder ?
A few mild symptoms — which you might not see as trouble signs — can signal the start of a drinking problem. It helps to know the signs so you can make a change early. If heavy drinking continues, then over time, the number and severity of symptoms can grow and add up to an “alcohol use disorder.” Doctors diagnose an alcohol use disorder when a patient’s drinking causes distress or harm. See if you recognize any of these symptoms in yourself. And don’t worry — even if you have symptoms, you can take steps to reduce your risks.
In the past year, have you 106:
- Had times when you ended up drinking more, or longer, than you intended ?
- More than once wanted to cut down or stop drinking, or tried to, but couldn’t ?
- More than once gotten into situations while or after drinking that increased your chances of getting hurt (such as driving, swimming, using machinery, walking in a dangerous area, or having unsafe sex) ?
- Had to drink much more than you once did to get the effect you want ? Or found that your usual number of drinks had much less effect than before ?
- Continued to drink even though it was making you feel depressed or anxious or adding to another health problem ? Or after having had a memory blackout ?
- Spent a lot of time drinking ? Or being sick or getting over other aftereffects ?
- Continued to drink even though it was causing trouble with your family or friends ?
- Found that drinking—or being sick from drinking—often interfered with taking care of your home or family ? Or caused job troubles ? Or school problems ?
- Given up or cut back on activities that were important or interesting to you, or gave you pleasure, in order to drink ?
- More than once gotten arrested, been held at a police station, or had other legal problems because of your drinking ?
- Found that when the effects of alcohol were wearing off, you had withdrawal symptoms, such as trouble sleeping, shakiness, restlessness, nausea, sweating, a racing heart, or a seizure ? Or sensed things that were not there ?
If you have any of these symptoms, your drinking may already be a cause for concern. The more symptoms you have, the more urgent the need for change. A health professional can conduct a formal assessment of your symptoms to see if an alcohol use disorder is present.
Alcohol detox
Alcohol detox or alcohol withdrawal refers to symptoms that may occur when a person who has been drinking too much alcohol on a regular basis suddenly stops drinking alcohol 107.
Alcohol withdrawal (detox) occurs most often in adults. But, it may occur in teenagers or children.
The more you drink regularly, the more likely you are to develop alcohol withdrawal symptoms when you stop drinking.
You may have more severe withdrawal symptoms if you have certain other medical problems.
Alcohol withdrawal is a serious condition that may rapidly become life threatening.
- Call your provider or go the emergency room if you think you might be in alcohol withdrawal, especially if you were using alcohol often and recently stopped. Call for an appointment with your provider if symptoms persist after treatment.
- Go to the emergency room or call the local emergency number if seizures, fever, severe confusion, hallucinations, or irregular heartbeats occur.
If you go to the hospital for another reason, tell the providers if you’ve been drinking heavily so they can monitor you for symptoms of alcohol withdrawal.
Symptoms of Alcohol withdrawal
Alcohol withdrawal symptoms usually occur within 8 hours after the last drink, but can occur days later. Symptoms usually peak by 24 to 72 hours, but may go on for weeks.
Common symptoms include:
- Anxiety or nervousness
- Depression
- Fatigue
- Irritability
- Jumpiness or shakiness
- Mood swings
- Nightmares
- Not thinking clearly
Other symptoms may include:
- Sweating, clammy skin
- Enlarged (dilated) pupils
- Headache
- Insomnia (sleeping difficulty)
- Loss of appetite
- Nausea and vomiting
- Pallor
- Rapid heart rate
- Tremor of the hands or other body parts
A severe form of alcohol withdrawal called delirium tremens can cause:
- Agitation
- Fever
- Seeing or feeling things that aren’t there (hallucinations)
- Seizures
- Severe confusion.
Treatment of alcohol withdrawal
The goal of treatment includes:
- Reducing withdrawal symptoms
- Preventing complications of alcohol use
- Therapy to get you to stop drinking (abstinence)
INPATIENT TREATMENT
People with moderate-to-severe symptoms of alcohol withdrawal may need inpatient treatment at a hospital or other facility that treats alcohol withdrawal. You will be watched closely for hallucinations and other signs of delirium tremens.
Treatment may include:
- Monitoring of blood pressure, body temperature, heart rate, and blood levels of different chemicals in the body
- Fluids or medicines given through a vein (by IV)
- Sedation using medicines until withdrawal is complete
OUTPATIENT TREATMENT
If you have mild-to-moderate alcohol withdrawal symptoms, you can often be treated in an outpatient setting. During this process, you will need someone who can stay with and keep an eye on you. You will likely need to make daily visits to your provider until you are stable.
Treatment usually includes:
- Sedative drugs to help ease withdrawal symptoms
- Blood tests
- Patient and family counseling to discuss the long-term issue of alcoholism
- Testing and treatment for other medical problems linked to alcohol use
It is important to go to a living situation that helps support you in staying sober. Some areas have housing options that provide a supportive environment for those trying to stay sober.
Permanent and life-long abstinence from alcohol is the best treatment for those who have gone through withdrawal.
Outlook (Prognosis) of alcohol withdrawal
How well a person does depends on the amount of organ damage and whether the person can stop drinking completely. Alcohol withdrawal may range from a mild and uncomfortable disorder to a serious, life-threatening condition.
Symptoms such as sleep changes, rapid changes in mood, and fatigue may last for months. People who continue to drink a lot may develop health problems such as liver, heart, and nervous system disease.
Most people who go through alcohol withdrawal make a full recovery. But, death is possible, especially if delirium tremens occurs.
What is delirium tremens ?
Delirium tremens is a severe form of alcohol withdrawal. It involves sudden and severe mental or nervous system changes 108.
Causes of delirium tremens
Delirium tremens can occur when you stop drinking alcohol after a period of heavy drinking, especially if you do not eat enough food.
Delirium tremens may also be caused by head injury, infection, or illness in people with a history of heavy alcohol use.
It occurs most often in people who have a history of alcohol withdrawal. It is especially common in those who drink 4 to 5 pints (1.8 to 2.4 liters) of wine, 7 to 8 pints (3.3 to 3.8 liters) of beer, or 1 pint (1/2 liter) of “hard” alcohol every day for several months. Delirium tremens also commonly affects people who have used alcohol for more than 10 years.
Symptoms of delirium tremens
Symptoms most often occur within 48 to 96 hours after the last drink. But, they can occur 7 to 10 days after the last drink.
Symptoms may get worse quickly, and can include:
- Delirium, which is sudden severe confusion
- Body tremors
- Changes in mental function
- Agitation, irritability
- Deep sleep that lasts for a day or longer
- Excitement or fear
- Hallucinations (seeing or feeling things that are not really there)
- Bursts of energy
- Quick mood changes
- Restlessness, excitement
- Sensitivity to light, sound, touch
- Stupor, sleepiness, fatigue
Seizures (may occur without other symptoms of delirium tremens):
- Most common in the first 12 to 48 hours after the last drink
- Most common in people with past complications from alcohol withdrawal
- Usually generalized tonic-clonic seizures
Symptoms of alcohol withdrawal, including:
- Anxiety, depression
- Fatigue
- Headache
- Insomnia (difficulty falling and staying asleep)
- Irritability or excitability
- Loss of appetite
- Nausea, vomiting
- Nervousness, jumpiness, shakiness, palpitations (sensation of feeling the heart beat)
- Pale skin
- Rapid emotional changes
- Sweating, especially on the palms of the hands or the face
Other symptoms that may occur:
- Chest pain
- Fever
- Stomach pain
Treatment of Delirium Tremens
The goals of treatment are to:
- Save the person’s life
- Relieve symptoms
- Prevent complications
A hospital stay is needed. The health care team will regularly check:
- Blood chemistry results, such as electrolyte levels
- Body fluid levels
- Vital signs (temperature, pulse, breathing rate, blood pressure)
While in the hospital, the person will receive medicines to:
- Stay calm and relaxed (sedated) until the delirium tremens are finished
- Treat seizures, anxiety, or tremors
- Treat mental disorders, if any
Long-term preventive treatment should begin after the person recovers from delirium tremens symptoms. This may involve:
- A “drying out” period, in which no alcohol is allowed
- Total and lifelong avoidance of alcohol (abstinence)
- Counseling
- Going to support groups (such as Alcoholics Anonymous)
Treatment may be needed for other medical problems that can occur with alcohol use, including:
- Alcoholic cardiomyopathy
- Alcoholic liver disease
- Alcoholic neuropathy
- Wernicke-Korsakoff syndrome.
Outlook (Prognosis) for Delirium tremens
Delirium tremens is serious and may be life threatening. Some symptoms related to alcohol withdrawal may last for a year or more, including:
- Emotional mood swings
- Feeling tired
- Sleeplessness
Possible Complications of Delirium tremens
Complications can include:
- Injury from falls during seizures
- Injury to self or others caused by mental state (confusion/delirium)
- Irregular heartbeat, may be life threatening
- Seizures
Long term effects of alcohol
Alcoholic cardiomyopathy
Exposure to high levels of alcohol for a long period could lead to progressive cardiac dysfunction and heart failure. Cardiac dysfunction associated with chronic and excessive alcohol intake is a specific cardiac disease known as alcoholic cardiomyopathy 109.
At present alcoholic cardiomyopathy is considered a specific disease both by the European Society of Cardiology (ESC) 110 and by the American Heart Association (AHA) 111. In the ESC consensus document on the classification of cardiomyopathies, Alcoholic cardiomyopathy is classified among the acquired forms of dilated cardiomyopathy 110.
The diagnosis of Alcoholic cardiomyopathy is usually one of exclusion in a patient with dilated cardiomyopathy with no identified cause and a long history of heavy alcohol abuse. According to most studies, the alcohol consumption required to establish a diagnosis of Alcoholic cardiomyopathy is over 80 g per day during at least 5 years 112.
Causes of Dilated cardiomyopathy
The most common causes of dilated cardiomyopathy are:
- Heart disease caused by a narrowings or blockages of the coronary arteries
- Poorly controlled high blood pressure
There are many other causes of dilated cardiomyopathy, including:
- Alcohol or cocaine abuse
- Diabetes, thyroid disease, or hepatitis
- Medicines that can be toxic to the heart, such as drugs used to treat cancer
- Abnormal heart rhythms in which the heart beats very fast for a long period of time
- Autoimmune illnesses
- Conditions that run in families
- Infections that involve the heart muscle
- Heart valves that are either too narrow or too leaky
- During the last month of pregnancy, or within 5 months after the baby is born.
- Exposure to heavy metals such as lead, arsenic, cobalt, or mercury
This condition can affect anyone at any age. However, it is most common in adult men.
Symptoms of Dilated cardiomyopathy
Symptoms of heart failure are most common. They most often develop slowly over time. However, sometimes symptoms start very suddenly and are severe.
Common symptoms are:
- Chest pain or pressure (more likely with exercise)
- Cough
- Fatigue, weakness, faintness
- Irregular or rapid pulse
- Loss of appetite
- Shortness of breath with activity or after lying down (or being asleep) for a while
- Swelling of feet and ankles
Exams and Tests for Dilated cardiomyopathy
During the exam, the health care provider may find:
- The heart is enlarged.
- Lung crackles (a sign of fluid buildup), heart murmur, or other abnormal sounds.
- The liver is possibly enlarged.
- Neck veins may be bulging.
A number of laboratory tests may be done to determine the cause:
- Antinuclear antibody (ANA), erythrocyte sedimentation rate (ESR), and other tests to diagnose autoimmune illnesses
- Antibody test to identify infections such as Lyme disease and HIV
- Iron tests of the blood
- Serum TSH and T4 test to identify thyroid problems
- Tests for amyloidosis
Heart enlargement or other problems with the structure and function of the heart (such as weak squeezing) may show up on these tests. They may also help diagnose the exact cause of the problem:
- Echocardiogram (ultrasound of the heart)
- Cardiac stress tests
- Chest x-ray
- Coronary angiogram to look at blood flow to the heart
- CT scan of the heart
- MRI of the heart
- Nuclear heart scan (MUGA, RNV)
Heart biopsy, in which a small piece of heart muscle is removed, may be needed depending on the cause. However, this is rarely done.
Treatment for Dilated cardiomyopathy
Things you can do at home to take care of your condition include:
- Know your body, and watch for symptoms that your heart failure is getting worse.
- Watch for changes in your symptoms, heart rate, pulse, blood pressure, and weight.
- Limit how much you drink and how much salt (sodium) you get in your diet.
Most people who have heart failure need to take medicines. Some medicines treat your symptoms. Others may help prevent your heart failure from becoming worse, or may prevent other heart problems.
Procedures and surgeries you may need include:
- A pacemaker to help treat slow heart rates or help your heartbeat stay in sync
- A defibrillator that recognizes life-threatening heart rhythms and sends an electrical pulse to stop them
- Heart bypass (CABG) surgery or angioplasty to improve blood flow to the damaged or weakened heart muscle
- Valve replacement or repair
For advanced cardiomyopathy:
A heart transplant may be recommended if standard treatments have not worked and heart failure symptoms are very severe.
Placement of a left ventricular assist device or artificial heart may be considered.
Chronic heart failure becomes worse over time. Many people who have heart failure will die from the condition. Thinking about the type of care you may want at the end of life and discussing these issues with loved ones and your health care provider is important.
Outlook (Prognosis) for Dilated cardiomyopathy
Heart failure is most often a chronic illness, which may get worse over time. Some people develop severe heart failure, in which medicines, other treatments, and surgery no longer help. Many people are at risk for deadly heart rhythms, and may need medicines or a defibrillator.
Alcoholic liver disease
Alcoholic liver disease – liver cirrhosis or alcoholic hepatitis, is damage to the liver and its function due to alcohol abuse 113.
Causes of Alcoholic liver disease
Alcoholic liver disease occurs after years of heavy drinking. Over time, scarring and cirrhosis can occur. Cirrhosis is the final phase of alcoholic liver disease.
Alcoholic liver disease does not occur in all heavy drinkers. The chances of getting liver disease go up the longer you have been drinking and more alcohol you consume. You do not have to get drunk for the disease to happen.
The disease seems to be more common in some families. Women may be more likely to have this problem than men.
Symptoms of Alcoholic liver disease
There may be no symptoms, or symptoms may come on slowly, depending on how well the liver is working. Symptoms tend to be worse after a period of heavy drinking.
Early symptoms include:
- Fatigue and loss of energy
- Poor appetite and weight loss
- Nausea or belly pain
- Small, red spider-like blood vessels on the skin
As liver function worsens, symptoms may include:
- Fluid buildup of the legs (edema) and in the abdomen (ascites)
- Yellow color in the skin, mucous membranes, or eyes (jaundice)
- Redness on the palms of the hands
- In men, impotence, shrinking of the testicles, and breast swelling
- Easy bruising and abnormal bleeding
- Confusion or problems thinking
- Pale or clay-colored stools
Exams and Tests for Alcoholic liver disease
Your health care provider will do a physical exam to look for:
- An enlarged liver or spleen
- Excess breast tissue
- Swollen abdomen, as a result of too much fluid
- Reddened palms
- Red spider-like blood vessels on the skin
- Small testicles
- Widened veins in the abdomen wall
- Yellow eyes or skin (jaundice)
Tests you may have include:
- Complete blood count (CBC)
- Liver biopsy
- Liver function tests
- Coagulation studies
Tests to rule out other diseases include:
- Abdominal CT scan
- Blood tests for other causes of liver disease
- Ultrasound of the abdomen
Treatment of Alcoholic liver disease
LIFESTYLE CHANGES
Some things you can do to help take care of your liver disease are:
- Drink less alcohol or even better quit drinking.
- Eat a healthy diet that is low in salt.
- Get vaccinated for diseases such as influenza, hepatitis A and hepatitis B, and pneumococcal pneumonia.
- Talk to your doctor about all medicines you take, including herbs and supplements and over-the-counter medicines.
MEDICINES FROM YOUR DOCTOR
- “Water pills” (diuretics) to get rid of fluid build-up
- Vitamin K or blood products to prevent excess bleeding
- Medicines for mental confusion
- Antibiotics for infections
OTHER TREATMENTS
- Endoscopic treatments for enlarged veins in the throat (bleeding varices)
- Removal of fluid from the abdomen (paracentesis)
- Placement of a transjugular intrahepatic portosystemic shunt (TIPS) to repair blood flow in the liver
When cirrhosis progresses to end-stage liver disease, a liver transplant may be needed.
Outlook (Prognosis) of Alcoholic liver disease
Continued excessive drinking can shorten your lifespan. Your risk for complications such as bleeding, brain changes, and severe liver damage go up. The outcome will likely be poor if you keep drinking.
Cirrhosis is caused by scarring of the liver. In most cases, the liver cannot heal or return to normal function once the damage is severe. Cirrhosis can lead to serious complications.
Possible Complications of Alcoholic liver disease
Complications may include:
- Bleeding disorders (coagulopathy)
- Buildup of fluid in the abdomen (ascites) and infection of the fluid (bacterial peritonitis)
- Enlarged veins in the esophagus, stomach, or intestines that bleed easily (esophageal varices)
- Increased pressure in the blood vessels of the liver (portal hypertension)
- Kidney failure (hepatorenal syndrome)
- Liver cancer (hepatocellular carcinoma)
- Mental confusion, change in the level of consciousness, or coma (hepatic encephalopathy).
Prevention of Alcoholic liver disease
Talk to your healthcare provider about your alcohol intake. Your healthcare provider can counsel you about how much alcohol is safe for you.
Alcoholic neuropathy
Alcoholic neuropathy (also called alcoholic polyneuropathy) is damage to the nerves that results from excessive drinking of alcohol 114.
Causes of Alcoholic neuropathy
The exact cause of alcoholic neuropathy is unknown. It likely includes both a direct poisoning of the nerve by the alcohol and the effect of poor nutrition associated with alcoholism. Up to half of long-term heavy alcohol users develop this condition.
In severe cases, nerves that regulate internal body functions (autonomic nerves) may be involved.
Risks of alcoholic neuropathy include:
- Long-term, heavy alcohol use
- Alcoholism that is present for 10 years or more
Symptoms of Alcoholic neuropathy
Symptoms of this condition include any of the following:
- Numbness in the arms and legs
- Abnormal sensations, such as “pins and needles”
- Painful sensations in the arms and legs
- Muscle problems, including weakness, cramps, aches, or spasms
- Heat intolerance, especially after exercise
- Erection problems (impotence)
- Problems urinating, incontinence (leaking urine), feeling of incomplete bladder emptying, difficulty beginning to urinate
- Constipation or diarrhea
- Nausea, vomiting
- Problems swallowing or talking
Changes in muscle strength or sensation usually occur on both sides of the body and are more common in the legs than in the arms. Symptoms usually develop gradually and become worse over time.
Exams and Tests for Alcoholic neuropathy
The health care provider will perform a physical exam and ask about symptoms. An eye exam may show eye problems.
Alcoholism often makes the body unable to use or store certain vitamins and minerals. Blood tests will be ordered to check for a deficiency (lack) of:
- Thiamine (vitamin B1)
- Pyridoxine (vitamin B6)
- Pantothenic acid and biotin
- Vitamin B12
- Folic acid
- Niacin (vitamin B3)
- Vitamin A
Other tests may be ordered to rule out other possible causes of neuropathy. Tests may include:
- Electrolyte levels
- Electromyography (EMG)
- Liver and kidney function tests
- Thyroid function tests
- Levels of vitamins and minerals in the body
- Nerve conduction tests
- Nerve biopsy
- Upper GI and small bowel series
- Esophagogastroduodenoscopy (EGD)
- Voiding cystourethrogram
Treatment of Alcoholic neuropathy
Once the alcohol problem has been addressed, treatment goals include:
- Controlling symptoms
- Maximizing ability to function independently
- Preventing injury
It is important to supplement the diet with vitamins, including thiamine and folic acid.
Physical therapy and orthopedic appliances (such as splints) may be needed to maintain muscle function and limb position.
Medicines may be needed to treat pain or uncomfortable sensations. People with alcoholic neuropathy have alcohol use problems. They will be prescribed the smallest dose of medicine needed to reduce symptoms, to help prevent drug dependence and other side effects of chronic use.
Positioning or the use of a bed frame that keeps the covers off the legs may help reduce pain.
People with lightheadedness or dizziness when standing up (orthostatic hypotension) may need to try several different treatments before finding one that successfully reduces their symptoms. Treatments that may help include:
- Wearing compression stockings
- Eating extra salt
- Sleeping with the head elevated
- Using medicines
Bladder problems may be treated with:
- Manual expression of urine
- Intermittent catheterization (male or female)
- Medicines
Impotence, diarrhea, constipation, or other symptoms are treated when necessary. These symptoms often respond poorly to treatment in people with alcoholic neuropathy.
It is important to protect body parts with reduced sensation from injury. This may include:
- Checking the temperature of bath water to prevent burns
- Changing footwear
- Frequently inspecting the feet and shoes to reduce injury caused by pressure or objects in the shoes
- Guarding the extremities to prevent injury from pressure
Alcohol must be stopped to prevent the damage from getting worse. Treatment for alcoholism may include counseling, social support such as Alcoholics Anonymous (AA), or medicines.
Outlook (Prognosis) of Alcoholic neuropathy
Damage to nerves from alcoholic neuropathy is usually permanent. It is likely to get worse if the person continues to use alcohol or if nutritional problems are not corrected. Alcoholic neuropathy is usually not life-threatening, but it can severely affect quality of life.
Prevention of Alcoholic neuropathy
The only way to prevent alcoholic neuropathy is not to drink excessive amounts of alcohol.
Wernicke-Korsakoff syndrome
Wernicke-Korsakoff syndrome, also known as alcoholic encephalopathy, is a brain disorder due to vitamin B1 (thiamine) deficiency 115.
Causes of Wernicke-Korsakoff syndrome (alcoholic encephalopathy)
Wernicke encephalopathy and Korsakoff syndrome are different conditions that often occur together. Both are due to brain damage caused by a lack of vitamin B1.
Lack of vitamin B1 is common in people who have alcohol use disorder. It is also common in people whose bodies do not absorb food properly (malabsorption). This can sometimes occur with a chronic illness or after weight-loss (bariatric) surgery.
Korsakoff syndrome, or Korsakoff psychosis, tends to develop as Wernicke symptoms go away. Wernicke encephalopathy causes brain damage in lower parts of the brain called the thalamus and hypothalamus. Korsakoff psychosis results from permanent damage to areas of the brain involved with memory.
Symptoms of Wernicke-Korsakoff syndrome (alcoholic encephalopathy)
Symptoms of Wernicke encephalopathy include:
- Confusion and loss of mental activity that can progress to coma and death
- Loss of muscle coordination (ataxia) that can cause leg tremor
- Vision changes such as abnormal eye movements (back and forth movements called nystagmus), double vision, eyelid drooping
- Alcohol withdrawal
Symptoms of Korsakoff syndrome:
- Inability to form new memories
- Loss of memory, can be severe
- Making up stories (confabulation)
- Seeing or hearing things that are not really there (hallucinations)
Exams and Tests for Wernicke-Korsakoff syndrome (alcoholic encephalopathy)
Examination of the nervous/muscular system may show damage to many nerve systems:
- Abnormal eye movement
- Decreased or abnormal reflexes
- Fast pulse (heart rate)
- Low blood pressure
- Low body temperature
- Muscle weakness and atrophy (loss of tissue mass)
- Problems with walk (gait) and coordination
The person may appear poorly nourished. The following tests are used to check a person’s nutrition level:
- Serum albumin (relates to person’s general nutrition)
- Serum vitamin B1 levels
- Transketolase activity in red blood cells (reduced in people with thiamine deficiency)
Liver enzymes may be high in people with a history of long-term alcohol abuse.
Other conditions that may cause vitamin B1 deficiency include:
- HIV/AIDS
- Cancers that have spread throughout the body
- Extreme nausea and vomiting during pregnancy (hyperemesis gravidarum)
- Heart failure (when treated with long-term diuretic therapy)
- Long periods of intravenous (IV) therapy without receiving thiamine supplements
- Long-term dialysis
- Very high thyroid hormone levels (thyrotoxicosis)
A brain MRI may show changes in the tissue of the brain. But if Wernicke-Korsakoff syndrome is suspected, treatment should start immediately. Usually a brain MRI exam is not needed.
Treatment of Wernicke-Korsakoff syndrome (alcoholic encephalopathy)
The goals of treatment are to control symptoms and to prevent the disorder from getting worse. Some people may need to stay in the hospital early in the condition to help control symptoms.
Monitoring and special care may be needed if the person is:
- In a coma
- Lethargic
- Unconscious
Vitamin B1 may be given by injection into a vein or a muscle, or by mouth. This may improve symptoms of:
- Confusion or delirium
- Difficulties with vision and eye movement
- Lack of muscle coordination
Vitamin B1 often does not improve loss of memory and intellect that occur with Korsakoff psychosis.
Stopping alcohol use can prevent more loss of brain function and damage to nerves. A well-balanced, nourishing diet can help, but it is not a substitute for stopping alcohol use.
Outlook (Prognosis) for Wernicke-Korsakoff syndrome (alcoholic encephalopathy)
Without treatment, Wernicke-Korsakoff syndrome gets steadily worse, and can be life threatening. With treatment, it is possible to control symptoms (such as uncoordinated movement and vision difficulties). This disorder can also be slowed or stopped.
Possible Complications of Wernicke-Korsakoff syndrome (alcoholic encephalopathy)
Complications that may result include:
- Alcohol withdrawal
- Difficulty with personal or social interaction
- Injury caused by falls
- Permanent alcoholic neuropathy
- Permanent loss of thinking skills
- Permanent loss of memory
- Shortened life span
Prevention
Not drinking alcohol or drinking in moderation and getting enough nutrition reduce the risk of developing Wernicke-Korsakoff syndrome. If a heavy drinker will not quit, thiamine supplements and a good diet may reduce the chance of getting this condition, but the risk is not eliminated.
- Effects of ethanol on ion channels. Crews FT, Morrow AL, Criswell H, Breese G. Int Rev Neurobiol. 1996; 39():283-367. https://www.ncbi.nlm.nih.gov/pubmed/8894851/[↩]
- Management of drug and alcohol withdrawal. Kosten TR, O’Connor PG. N Engl J Med. 2003 May 1; 348(18):1786-95. https://www.ncbi.nlm.nih.gov/pubmed/12724485/[↩]
- Mattson RH. Seizures associated with alcohol use and alcohol withdrawal. In: Feldman B, editor. Epilepsy:Diagnosis and Management. Boston: Little Brown; 1983. pp. 325–332.[↩]
- GBD 2016 Alcohol and Drug Use Collaborators. The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Psychiatry. 2018 Dec;5(12):987-1012. doi: 10.1016/S2215-0366(18)30337-7. Epub 2018 Nov 1. Erratum in: Lancet Psychiatry. 2019 Jan;6(1):e2.[↩][↩]
- GBD 2016 Alcohol Collaborators. Alcohol use and burden for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2018 Sep 22;392(10152):1015-1035. doi: 10.1016/S0140-6736(18)31310-2. Epub 2018 Aug 23. Erratum in: Lancet. 2018 Sep 29;392(10153):1116. Erratum in: Lancet. 2019 Jun 22;393(10190):e44.[↩][↩]
- Alcohol. https://www.who.int/news-room/fact-sheets/detail/alcohol[↩][↩]
- Global status report on alcohol and health 2018 [Internet]. Geneva: World Health Organization; 2018. https://apps.who.int/iris/bitstream/handle/10665/274603/9789241565639-eng.pdf[↩]
- White AM, Castle IP, Powell PA, Hingson RW, Koob GF. Alcohol-Related Deaths During the COVID-19 Pandemic. JAMA. 2022;327(17):1704–1706. doi:10.1001/jama.2022.4308[↩]
- Pilar MR, Eyler AA, Moreland-Russell S, Brownson RC. Actual Causes of Death in Relation to Media, Policy, and Funding Attention: Examining Public Health Priorities. Front Public Health. 2020 Jul 7;8:279. doi: 10.3389/fpubh.2020.00279[↩]
- Centers for Disease Control and Prevention (CDC). Alcohol and Public Health: Alcohol-Related Disease Impact (ARDI). Annual Average for United States 2011–2015 Alcohol-Attributable Deaths Due to Excessive Alcohol Use, All Ages. https://nccd.cdc.gov/DPH_ARDI/Default/Default.aspx[↩]
- Esser MB, Sherk A, Liu Y, et al. Deaths and Years of Potential Life Lost From Excessive Alcohol Use — United States, 2011–2015. MMWR Morb Mortal Wkly Rep 2020;69:1428–1433. DOI: http://dx.doi.org/10.15585/mmwr.mm6939a6[↩]
- Rehm J, Gmel GE Sr, Gmel G, Hasan OSM, Imtiaz S, Popova S, Probst C, Roerecke M, Room R, Samokhvalov AV, Shield KD, Shuper PA. The relationship between different dimensions of alcohol use and the burden of disease-an update. Addiction. 2017 Jun;112(6):968-1001. doi: 10.1111/add.13757[↩]
- Cao Y, Willett WC, Rimm EB, Stampfer MJ, Giovannucci EL. Light to moderate intake of alcohol, drinking patterns, and risk of cancer: results from two prospective US cohort studies. BMJ. 2015 Aug 18;351:h4238. doi: 10.1136/bmj.h4238[↩]
- Freudenheim JL. Alcohol’s Effects on Breast Cancer in Women. Alcohol Res. 2020 Jun 18;40(2):11. doi: 10.35946/arcr.v40.2.11[↩]
- Stockwell T, Zhao J, Panwar S, Roemer A, Naimi T, Chikritzhs T. Do “Moderate” Drinkers Have Reduced Mortality Risk? A Systematic Review and Meta-Analysis of Alcohol Consumption and All-Cause Mortality. J Stud Alcohol Drugs. 2016 Mar;77(2):185-98. doi: 10.15288/jsad.2016.77.185[↩]
- GBD 2016 Alcohol Collaborators. Alcohol use and burden for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2018 Sep 22;392(10152):1015-1035. doi: 10.1016/S0140-6736(18)31310-2. Epub 2018 Aug 23. Erratum in: Lancet. 2018 Sep 29;392(10153):1116. Erratum in: Lancet. 2019 Jun 22;393(10190):e44[↩]
- Wood AM, Kaptoge S, Butterworth AS, et al. Emerging Risk Factors Collaboration/EPIC-CVD/UK Biobank Alcohol Study Group. Risk thresholds for alcohol consumption: combined analysis of individual-participant data for 599 912 current drinkers in 83 prospective studies. Lancet. 2018 Apr 14;391(10129):1513-1523. doi: 10.1016/S0140-6736(18)30134-X. Erratum in: Lancet. 2018 Jun 2;391(10136):2212.[↩]
- Millwood IY, Walters RG, Mei XW, Guo Y, Yang L, Bian Z, Bennett DA, Chen Y, Dong C, Hu R, Zhou G, Yu B, Jia W, Parish S, Clarke R, Davey Smith G, Collins R, Holmes MV, Li L, Peto R, Chen Z; China Kadoorie Biobank Collaborative Group. Conventional and genetic evidence on alcohol and vascular disease aetiology: a prospective study of 500 000 men and women in China. Lancet. 2019 May 4;393(10183):1831-1842. doi: 10.1016/S0140-6736(18)31772-0[↩]
- U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020-2025. 9th Edition. December 2020. https://www.dietaryguidelines.gov/sites/default/files/2021-03/Dietary_Guidelines_for_Americans-2020-2025.pdf[↩][↩][↩][↩]
- Edenberg HJ. The genetics of alcohol metabolism: role of alcohol dehydrogenase and aldehyde dehydrogenase variants. Alcohol Res Health. 2007;30(1):5-13. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3860432[↩][↩]
- Hurley TD, Edenberg HJ, Li T-K. Pharmacogenomics: The Search for Individualized Therapies. Weinheim, Germany: Wiley-VCH; 2002. The pharmacogenomics of alcoholism; pp. 417–441.[↩]
- Zaso MJ, Goodhines PA, Wall TL, Park A. Meta-Analysis on Associations of Alcohol Metabolism Genes With Alcohol Use Disorder in East Asians. Alcohol Alcohol. 2019 May 1;54(3):216-224. doi: 10.1093/alcalc/agz011[↩]
- Goldman D, Oroszi G, Ducci F. The genetics of addictions: uncovering the genes. Nat Rev Genet. 2005 Jul;6(7):521-32. doi: 10.1038/nrg1635[↩]
- Hurley TD, Edenberg HJ. Genes encoding enzymes involved in ethanol metabolism. Alcohol Res. 2012;34(3):339-44. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3756590[↩]
- National Collaborating Centre for Mental Health (UK). Alcohol-Use Disorders: Diagnosis, Assessment and Management of Harmful Drinking and Alcohol Dependence. Leicester (UK): British Psychological Society (UK); 2011. (NICE Clinical Guidelines, No. 115.) Available from: https://www.ncbi.nlm.nih.gov/books/NBK65487[↩]
- Schuckit MA. A Critical Review of Methods and Results in the Search for Genetic Contributors to Alcohol Sensitivity. Alcohol Clin Exp Res. 2018 May;42(5):822-835. doi: 10.1111/acer.13628[↩]
- Hingson RW, Heeren T, Winter MR. Preventing impaired driving. Alcohol Res Health. 1999;23(1):31-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6761696[↩]
- Centers for Disease Control and Prevention. Alcohol Poisoning Deaths. https://www.cdc.gov/vitalsigns/alcohol-poisoning-deaths/index.html[↩][↩][↩][↩]
- Sacks JJ, Gonzales KR, Bouchery EE, Tomedi LE, Brewer RD. 2010 National and State Costs of Excessive Alcohol Consumption. Am J Prev Med. 2015 Nov;49(5):e73-e79. doi: 10.1016/j.amepre.2015.05.031[↩]
- Mokdad, A.H.; Marks, J.S.; Stroup, D.F.; and Gerberding, J.L. Actual causes of death in the United States 2000. [Published erratum in: JAMA 293(3):293–294, 298] JAMA: Journal of the American Medical Association 291(10):1238–1245, 2004. http://jamanetwork.com/journals/jama/article-abstract/198357[↩]
- Centers for Disease Control and Prevention. Alcohol Deaths. https://www.cdc.gov/features/alcohol-deaths/index.html[↩]
- National Center for Statistics and Analysis. 2014 Crash Data Key Findings (Traffic Safety Facts Crash Stats. Report No. DOT HS 812 219). Washington, DC: National Highway Traffic Safety Administration, 2015. https://crashstats.nhtsa.dot.gov/Api/Public/ViewPublication/812219 [↩]
- The Basics: Defining How Much Alcohol is Too Much. https://www.niaaa.nih.gov/health-professionals-communities/core-resource-on-alcohol/basics-defining-how-much-alcohol-too-much#pub-toc1[↩]
- U.S. Alcohol and Tobacco Tax and Trade Bureau. Alcohol Beverage Labeling and Advertising. https://www.ttb.gov/consumer/labeling_advertising.shtml[↩]
- U.S. Department of Health and Human Services. Rethinking Drinking – Alcohol Calculators. https://www.rethinkingdrinking.niaaa.nih.gov/Tools/Calculators/Default.aspx[↩]
- U.S. Department of Health and Human Services. Rethinking Drinking – How many drinks are in common containers ? https://www.rethinkingdrinking.niaaa.nih.gov/How-much-is-too-much/What-counts-as-a-drink/How-Many-Drinks-Are-In-Common-Containers.aspx[↩]
- Dawson DA, Li TK, Grant BF. A prospective study of risk drinking: at risk for what? Drug Alcohol Depend. 2008 May 1;95(1-2):62-72. doi: 10.1016/j.drugalcdep.2007.12.007[↩]
- Roerecke M, Rehm J. Chronic heavy drinking and ischaemic heart disease: a systematic review and meta-analysis. Open Heart. 2014 Aug 6;1(1):e000135. doi: 10.1136/openhrt-2014-000135[↩]
- Scoccianti C, Straif K, Romieu I. Recent evidence on alcohol and cancer epidemiology. Future Oncol. 2013 Sep;9(9):1315-22. https://doi.org/10.2217/fon.13.94[↩]
- U.S. Department of Health and Human Services. Rethinking Drinking – What’s your pattern ? https://www.rethinkingdrinking.niaaa.nih.gov/How-much-is-too-much/Is-your-drinking-pattern-risky/Whats-Your-Pattern.aspx?type=MaleFrequentlyOverSingleDayONLY&avg=10&day=5&week=2[↩][↩]
- Esser MB, Hedden SL, Kanny D, Brewer RD, Gfroerer JC, Naimi TS. Prevalence of Alcohol Dependence Among US Adult Drinkers, 2009–2011. Prev Chronic Dis 2014;11:140329. https://www.cdc.gov/pcd/issues/2014/14_0329.htm[↩][↩]
- U.S. Department of Health and Human Services. Rethinking Drinking – What’s low-risk drinking ? https://www.rethinkingdrinking.niaaa.nih.gov/How-much-is-too-much/Is-your-drinking-pattern-risky/Whats-Low-Risk-Drinking.aspx[↩][↩]
- National Institute on Alcohol Abuse and Alcoholism. Beyond Hangovers. https://pubs.niaaa.nih.gov/publications/Hangovers/beyondHangovers.htm [↩][↩]
- U.S. Department of Health and Human Services. Rethinking Drinking – What’s at-risk or heavy drinking ? https://www.rethinkingdrinking.niaaa.nih.gov/How-much-is-too-much/Is-your-drinking-pattern-risky/Whats-At-Risk-Or-Heavy-Drinking.aspx[↩]
- Drinking Levels Defined. https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking[↩]
- White AM, Tapert S, Shukla SD. Binge Drinking. Alcohol Res. 2018;39(1):1-3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6104965[↩][↩][↩][↩]
- Han BH, Moore AA, Ferris R, Palamar JJ. Binge Drinking Among Older Adults in the United States, 2015 to 2017. J Am Geriatr Soc. 2019 Oct;67(10):2139-2144. doi: 10.1111/jgs.16071[↩]
- Keyes KM, Jager J, Mal-Sarkar T, Patrick ME, Rutherford C, Hasin D. Is There a Recent Epidemic of Women’s Drinking? A Critical Review of National Studies. Alcohol Clin Exp Res. 2019 Jul;43(7):1344-1359. doi: 10.1111/acer.14082. Epub 2019 Jun 5. Erratum in: Alcohol Clin Exp Res. 2020 Feb;44(2):579.[↩]
- Wilsnack RW, Wilsnack SC, Gmel G, Kantor LW. Gender Differences in Binge Drinking. Alcohol Res. 2018;39(1):57-76. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6104960[↩]
- Understanding Alcohol Use Disorder. https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/understanding-alcohol-use-disorder[↩]
- Alcohol use disorder. https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/alcohol-use-disorders[↩][↩][↩]
- Substance Abuse and Mental Health Services Administration (SAMHSA), Center for Behavioral Health Statistics and Quality. 2019 National Survey on Drug Use and Health. Table 5.4A—Alcohol Use Disorder in Past Year Among Persons Aged 12 or Older, by Age Group and Demographic Characteristics: Numbers in Thousands, 2018 and 2019. https://www.samhsa.gov/data/sites/default/files/reports/rpt29394/NSDUHDetailedTabs2019/NSDUHDetTabsSect5pe2019.htm?s=5.4&#tab5-4a[↩]
- SAMHSA, Center for Behavioral Health Statistics and Quality. 2019 National Survey on Drug Use and Health. Table 5.4B—Alcohol Use Disorder in Past Year Among Persons Aged 12 or Older, by Age Group and Demographic Characteristics: Percentages, 2018 and 2019. https://www.samhsa.gov/data/sites/default/files/reports/rpt29394/NSDUHDetailedTabs2019/NSDUHDetTabsSect5pe2019.htm?s=5.4&#tab5-4b[↩]
- Nehring SM, Freeman AM. Alcohol Use Disorder. [Updated 2021 Apr 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK436003[↩][↩]
- Pavón, F. J., Serrano, A., Stouffer, D. G., Polis, I., Roberto, M., Cravatt, B. F., Martin-Fardon, R., Rodríguez de Fonseca, F., & Parsons, L. H. (2019). Ethanol-induced alterations in endocannabinoids and relevant neurotransmitters in the nucleus accumbens of fatty acid amide hydrolase knockout mice. Addiction biology, 24(6), 1204–1215. https://doi.org/10.1111/adb.12695[↩]
- Witkiewitz, K., Kranzler, H. R., Hallgren, K. A., O’Malley, S. S., Falk, D. E., Litten, R. Z., Hasin, D. S., Mann, K. F., & Anton, R. F. (2018). Drinking Risk Level Reductions Associated with Improvements in Physical Health and Quality of Life Among Individuals with Alcohol Use Disorder. Alcoholism, clinical and experimental research, 42(12), 2453–2465. https://doi.org/10.1111/acer.13897[↩]
- Degenhardt, L., Bharat, C., Bruno, R., Glantz, M. D., Sampson, N. A., Lago, L., Aguilar-Gaxiola, S., Alonso, J., Andrade, L. H., Bunting, B., Caldas-de-Almeida, J. M., Cia, A. H., Gureje, O., Karam, E. G., Khalaf, M., McGrath, J. J., Moskalewicz, J., Lee, S., Mneimneh, Z., Navarro-Mateu, F., … WHO World Mental Health Survey Collaborators (2019). Concordance between the diagnostic guidelines for alcohol and cannabis use disorders in the draft ICD-11 and other classification systems: analysis of data from the WHO’s World Mental Health Surveys. Addiction (Abingdon, England), 114(3), 534–552. https://doi.org/10.1111/add.14482[↩]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013:490–491.[↩]
- National Institute on Alcohol Abuse and Alcoholism. Treatment for Alcohol Problems: Finding and Getting Help. https://pubs.niaaa.nih.gov/publications/Treatment/treatment.htm[↩][↩][↩]
- National Institutes of Health. Rethinking Drinking. Professional help. https://www.rethinkingdrinking.niaaa.nih.gov/Thinking-about-a-change/support-for-quitting/Professional-Help.aspx [↩]
- National Institute on Drug Abuse. Alcohol Addiction: Principles of Drug Addiction Treatment: A Research-Based Guide (Third Edition). https://www.drugabuse.gov/publications/principles-drug-addiction-treatment-research-based-guide-third-edition/evidence-based-approaches-to-drug-addiction-treatment/pharmacotherapi-1[↩][↩][↩][↩]
- Naltrexone. https://www.samhsa.gov/medication-assisted-treatment/medications-counseling-related-conditions/naltrexone[↩][↩]
- Niciu MJ, Arias AJ. Targeted opioid receptor antagonists in the treatment of alcohol use disorders. CNS Drugs. 2013;27(10):777–787.[↩]
- Rösner S, Hackl-Herrwerth A, Leucht S, Vecchi S, Srisurapanont M, Soyka M. Opioid antagonists for alcohol dependence. Cochrane Database Syst Rev. 2010;(12):CD001867.[↩]
- Jonas DE, Amick HR, Feltner C, et al. Pharmacotherapy for adults with alcohol use disorders in outpatient settings: a systematic review and meta-analysis. JAMA. 2014;311(18):1889–1900.[↩][↩][↩]
- Garbutt JC, Kranzler HR, O’Malley SS, et al.; Vivitrex Study Group. Efficacy and tolerability of long-acting injectable naltrexone for alcohol dependence: a randomized controlled trial [published corrections appear in JAMA. 2005;293(16):1978, and JAMA. 2005;293(23):2864]. JAMA. 2005;293(13):1617–1625.[↩]
- Maisel NC, Blodgett JC, Wilbourne PL, Humphreys K, Finney JW. Meta-analysis of naltrexone and acamprosate for treating alcohol use disorders: when are these medications most helpful? Addiction. 2013;108(2):275–293.[↩][↩]
- Anton RF, O’Malley SS, Ciraulo DA, et al. Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. JAMA. 2006;295(17):2003–2017.[↩]
- Kiefer F, Jahn H, Tarnaske T, et al. Comparing and combining naltrexone and acamprosate in relapse prevention of alcoholism: a double-blind, placebo-controlled study. Arch Gen Psychiatry. 2003;60(1):92–99.[↩]
- van den Brink W, Aubin HJ, Bladström A, Torup L, Gual A, Mann K. Efficacy of as-needed nalmefene in alcohol-dependent patients with at least a high drinking risk level: results from a subgroup analysis of two randomized controlled 6-month studies [published correction appears in Alcohol Alcohol. 2013;48(6):746]. Alcohol Alcohol. 2013;48(5):570–578.[↩]
- Yahn SL, Watterson LR, Olive MF. Safety and efficacy of acamprosate for the treatment of alcohol dependence. Subst Abuse. 2013;6:1–12.[↩]
- Rösner S, Hackl-Herrwerth A, Leucht S, Lehert P, Vecchi S, Soyka M. Acamprosate for alcohol dependence. Cochrane Database Syst Rev. 2010;(9):CD004332.[↩]
- Berger L, Fisher M, Brondino M, et al. Efficacy of acamprosate for alcohol dependence in a family medicine setting in the United States: a randomized, double-blind, placebo-controlled study. Alcohol Clin Exp Res. 2013;37(4):668–674.[↩]
- Laaksonen E, Koski-Jännes A, Salaspuro M, Ahtinen H, Alho H. A randomized, multicentre, open-label, comparative trial of disulfiram, naltrexone and acamprosate in the treatment of alcohol dependence. Alcohol Alcohol. 2008;43(1):53–61.[↩]
- Skinner MD, Lahmek P, Pham H, Aubin HJ. Disulfiram efficacy in the treatment of alcohol dependence: a meta-analysis. PLoS One. 2014;9(2):e87366.[↩]
- Agency for Healthcare Research and Quality. Pharmacotherapy for adults with alcohol-use disorders in outpatient settings. Executive summary. https://effectivehealthcare.ahrq.gov/sites/default/files/related_files/alcohol-misuse-drug-therapy-surveillance.pdf[↩]
- Mukamal KJ, Conigrave KM, Mittleman MA, Camargo CA Jr, Stampfer MJ, Willett WC, Rimm EB. Roles of drinking pattern and type of alcohol consumed in coronary heart disease in men. N Engl J Med. 2003;348:109–118. doi: 10.1056/NEJMoa022095.[↩][↩]
- Whitfield JB, Heath AC, Madden PA, Pergadia ML, Montgomery GW, Martin NG. Metabolic and biochemical effects of low-to-moderate alcohol consumption. Alcohol Clin Exp Res. 2013;37:575–586. doi: 10.1111/acer.12015.[↩]
- Spaak J, Merlocco AC, Soleas GJ, Tomlinson G, Morris BL, Picton P, Notarius CF, Chan CT, Floras JS. Dose-related effects of red wine and alcohol on hemodynamics, sympathetic nerve activity, and arterial diameter. Am J Physiol Heart Circ Physiol. 2008;294:H605–H612. doi:10.1152/ajpheart. 01162.2007.[↩]
- Sengul C, Cevik C, Ozveren O, Sunbul A, Oduncu V, Akgun T, Can MM, Semiz E, Dindar I. Acute alcohol consumption is associated with increased interatrial electromechanical delay in healthy men. Cardiol J. 2011;18:682–686.[↩]
- Hendriks HF, Veenstra J, Velthuis-te Wierik EJ, Schaafsma G, Kluft C. Effect of moderate dose of alcohol with evening meal on fibrinolytic factors. BMJ. 1994;308:1003–1006.[↩]
- Briasoulis A, Agarwal V, Messerli FH. Alcohol consumption and the risk of hypertension in men and women: a systematic review and metaanalysis. J Clin Hypertens (Greenwich). 2012;14:792–798. doi: 10.1111/ jch.12008.[↩]
- Brien SE, Ronksley PE, Turner BJ, Mukamal KJ, Ghali WA. Effect of alcohol consumption on biological markers associated with risk of coronary heart disease: systematic review and meta-analysis of interventional studies. BMJ. 2011;342:d636.[↩]
- U.S. Department of Health and Human Services. Rethinking Drinking – What are the risks ? https://www.rethinkingdrinking.niaaa.nih.gov/How-much-is-too-much/Whats-the-harm/What-Are-The-Risks.aspx[↩]
- Kanny D, Brewer RD, Mesnick JB, Paulozzi LJ, Naimi TS, Lu H. Vital Signs: Alcohol Poisoning Deaths — United States, 2010–2012. MMWR 2015;63:1238-1242. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6353a2.htm?s_cid=mm6353a2_w[↩]
- Smith GS, Branas CC, Miller TR. Fatal nontraffic injuries involving alcohol: a meta analysis. Ann of Emer Med 1999;33(6):659–668. https://www.ncbi.nlm.nih.gov/pubmed/10339681?dopt=Abstract[↩]
- Greenfield LA. Alcohol and Crime: An Analysis of National Data on the Prevalence of Alcohol Involvement in Crime. Report prepared for the Assistant Attorney General’s National Symposium on Alcohol Abuse and Crime. Washington, DC: U.S. Department of Justice, 1998. https://www.bjs.gov/content/pub/pdf/ac.pdf[↩]
- Mohler-Kuo M, Dowdall GW, Koss M, Wechsler H. Correlates of rape while intoxicated in a national sample of college women. Journal of Studies on Alcohol 2004;65(1):37–45. https://www.ncbi.nlm.nih.gov/pubmed/15000502?dopt=Abstract[↩]
- World Health Organization. Global status report on alcohol and health—2014. Geneva, Switzerland: World Health Organization; 2014. http://www.who.int/substance_abuse/publications/global_alcohol_report/en/[↩][↩]
- Naimi TS, Lipscomb LE, Brewer RD, Colley BG. Binge drinking in the preconception period and the risk of unintended pregnancy: Implications for women and their children. Pediatrics 2003;11(5):1136–1141. https://www.ncbi.nlm.nih.gov/pubmed/12728126?dopt=Abstract[↩][↩]
- Wechsler H, Davenport A, Dowdall G, Moeykens B, Castillo S. Health and behavioral consequences of binge drinking in college. JAMA 1994;272(21):1672–1677. https://www.ncbi.nlm.nih.gov/pubmed/7966895?dopt=Abstract[↩]
- Kesmodel U, Wisborg K, Olsen SF, Henriksen TB, Sechler NJ. Moderate alcohol intake in pregnancy and the risk of spontaneous abortion. Alcohol & Alcoholism 2002;37(1):87–92. https://www.ncbi.nlm.nih.gov/pubmed/11825863?dopt=Abstract[↩]
- American Academy of Pediatrics, Committee on Substance Abuse and Committee on Children with Disabilities. 2000. Fetal alcohol syndrome and alcohol-related neurodevelopmental disorders. Pediatrics 2000;106:358–361. https://www.ncbi.nlm.nih.gov/pubmed/10920168?dopt=Abstract[↩]
- Rehm J, Baliunas D, Borges GL, Graham K, Irving H, Kehoe T, et al. The relation between different dimensions of alcohol consumption and burden of disease: an overview. Addiction. 2010;105(5):817-43. [↩]
- International Agency for Research on Cancer. Personal Habits and Indoor Combustions: A Review of Human Carcinogens, Volume 100E 2012. Available from: http://monographs.iarc.fr/ENG/Monographs/vol100E/index.php[↩]
- Miller JW, Naimi TS, Brewer RD, Jones SE. Binge drinking and associated health risk behaviors among high school students. Pediatrics. 2007;119(1):76-85. http://pediatrics.aappublications.org/content/119/1/76.full[↩]
- Castaneda R, Sussman N, Westreich L, Levy R, O’Malley M. A review of the effects of moderate alcohol intake on the treatment of anxiety and mood disorders. J Clin Psychiatry 1996;57(5):207–212. https://www.ncbi.nlm.nih.gov/pubmed/8626352?dopt=Abstract[↩]
- Booth BM, Feng W. The impact of drinking and drinking consequences on short-term employment outcomes in at-risk drinkers in six southern states. J Behavioral Health Services and Research 2002;29(2):157–166. https://www.ncbi.nlm.nih.gov/pubmed/12032973?dopt=Abstract[↩]
- Rehm J, Baliunas D, Borges GLG, et al. THE RELATION BETWEEN DIFFERENT DIMENSIONS OF ALCOHOL CONSUMPTION AND BURDEN OF DISEASE – AN OVERVIEW. Addiction (Abingdon, England). 2010;105(5):817-843. doi:10.1111/j.1360-0443.2010.02899.x. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3306013/[↩][↩][↩]
- National Institute on Alcohol Abuse and Alcoholism. Beyond Hangovers. https://pubs.niaaa.nih.gov/publications/Hangovers/beyondHangovers.htm[↩][↩][↩][↩][↩]
- National Institute on Alcohol Abuse and Alcoholism. Drinking and Your Pregnancy. https://pubs.niaaa.nih.gov/publications/DrinkingPregnancy_HTML/pregnancy.htm[↩]
- U.S. Department of Health and Human Services. Rethinking Drinking – Tips to try. https://www.rethinkingdrinking.niaaa.nih.gov/Thinking-about-a-change/Strategies-for-cutting-down/Tips-To-Try.aspx[↩][↩]
- U.S. Department of Health and Human Services. Rethinking Drinking – Handling urges to drink. https://www.rethinkingdrinking.niaaa.nih.gov/Tools/Interactive-worksheets-and-more/Stay-in-control/Coping-With-Urges-To-Drink.aspx[↩]
- U.S. Department of Health and Human Services. Rethinking Drinking – Handling urges to drink. https://www.rethinkingdrinking.niaaa.nih.gov/Tools/Interactive-worksheets-and-more/Stay-in-control/Coping-With-Urges-To-Drink-urge-tracker.aspx[↩]
- Alcoholics Anonymous. http://www.aa.org/[↩]
- U.S. Department of Health and Human Services. Rethinking Drinking – What are symptoms of an alcohol use disorder ? https://www.rethinkingdrinking.niaaa.nih.gov/How-much-is-too-much/Whats-the-harm/What-Are-Symptoms-Of-An-Alcohol-Use-Disorder.aspx[↩]
- U.S. National Library of Medicine. Medline Plus. Alcohol withdrawal. https://medlineplus.gov/ency/article/000764.htm[↩]
- U.S. National Library of Medicine. Medline Plus. Delirium tremens. https://medlineplus.gov/ency/article/000766.htm[↩]
- Guzzo-Merello G, Cobo-Marcos M, Gallego-Delgado M, Garcia-Pavia P. Alcoholic cardiomyopathy. World Journal of Cardiology. 2014;6(8):771-781. doi:10.4330/wjc.v6.i8.771. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4163706/[↩]
- Elliott P, Andersson B, Arbustini E, Bilinska Z, Cecchi F, Charron P, Dubourg O, Kühl U, Maisch B, McKenna WJ, et al. Classification of the cardiomyopathies: a position statement from the European Society Of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2008;29:270–276. https://www.ncbi.nlm.nih.gov/pubmed/17916581[↩][↩]
- Maron BJ, Towbin JA, Thiene G, Antzelevitch C, Corrado D, Arnett D, Moss AJ, Seidman CE, Young JB. Contemporary definitions and classification of the cardiomyopathies: an American Heart Association Scientific Statement from the Council on Clinical Cardiology, Heart Failure and Transplantation Committee; Quality of Care and Outcomes Research and Functional Genomics and Translational Biology Interdisciplinary Working Groups; and Council on Epidemiology and Prevention. Circulation. 2006;113:1807–1816. https://www.ncbi.nlm.nih.gov/pubmed/16567565[↩]
- Haissaguerre M, Fleury B, Gueguen A, Bonnet J, Lorente P, Nakache JP, Broustet JP, Dallochio M, Besse P. [Mortality of dilated myocardiopathies as a function of continuation of alcohol drinking. Multivariate analysis concerning 236 patients] Presse Med. 1989;18:711–714. https://www.ncbi.nlm.nih.gov/pubmed/2524748[↩]
- U.S. National Library of Medicine. Medline Plus. Alcoholic liver disease. https://medlineplus.gov/ency/article/000281.htm[↩]
- U.S. National Library of Medicine. Medline Plus. Alcoholic neuropathy. https://medlineplus.gov/ency/article/000714.htm[↩]
- U.S. National Library of Medicine. Medline Plus. Wernicke-Korsakoff syndrome. https://medlineplus.gov/ency/article/000771.htm[↩]