Sinus pericranii
Sinus pericranii also called subgaleal varix, is a rare venous anomaly characterized by an abnormal communication between the intracranial and extracranial veins through a bone defect 1. It is usually located near the dural sinuses and presents as a soft, palpable scalp mass 2. In sinus pericranii there is an abnormal communication between intracranial dural sinuses and extracranial venous structures, usually via an emissary transosseous vein. Sinus pericranii is considered a type of low flow vascular malformation. It occurs in close communication with the cranial vault and most frequently involves the superior sagittal sinus. Pathologically, it exhibits a direct communication between the nonmuscular veins adhering to the outer surface of the skull and the intracranial venous sinuses 3. The distribution of the lesions is more commonly found in the frontal region (43%), followed by parietal (36%) and occipital regions (7.4%) 4. A lateral location is unusual 5.
Sinus pericranii patients may present with mild (local pain, nausea, headache, and dizziness) to severe (increased intracranial pressure, bradypnea, bradycardia, ataxia, hearing loss, and epileptic seizures) symptoms 6. However, most cases are asymptomatic, with the main complaint being the associated cosmetic problems 7. Additionally, considering its clinical presentation, it is imperative to identify sinus pericranii from other diseases presenting as a mass on the scalp and it is vital to avoid harmful biopsy because of the communicating venous anomalies 8. When suspected on radiological basis, a simple clinical test can be performed. Unless thrombosed, the sinus pericranii will appear more prominent on supine position than when sitting, because of variable venous pressure with gravity. The lesions are not classically associated with discoloration of the overlying skin.
Sinus pericranii can be congenital (present at birth), in which case it is often obvious, but may also be acquired through trauma or iatrogenic and might be subtle in these cases. Most of sinus pericranii is a congenital type, which formed at late embryogenesis. After birth, the lesion which has been for several years can have a typical feature of pathologic findings. The existence of thick accumulated stroma suggested a possibility of congenital type sinus pericranii. On the other hand, acquired type sinus pericranii usually depicts fibrous microstructure encapsulating the blood. This is because trauma disrupts emissary veins and calvarium, making a fibrous lining or capsule around the extravasated blood.
Sinus pericranii has been defined as a varix and classified into three types according to the size of the venous communication between the extracranial blood sac and intracranial venous sinus 9. Newton and Troost 10 described it as a communication between the extracranial and intracranial venous circulation via large, tortuous, thin walled vascular channels. Volkmann described two types of sinus pericranii : ‘true sinus’ which fills with increased intracranial pressure and disappears completely with compression and ‘pseudo sinus’, which fails to disappear completely with compression. They considered the latter to be angioma or cavernoma of mainly venous component.
Since it is a venous anomaly, it can be diagnosed with methods similar to those used for other venous anomalies in the head and neck region. Doppler ultrasonography is a useful radiological tool to differentiate different vascular anomalies 1. Following which, MRI can be used to characterize the size and extent of the lesion. T2-weighted MRI shows a mass with high levels of mixed signals, which includes a signal void due to the blood flow 11. Some authors recommend direct percutaneous venography as a confirmatory tool 12, however, it is associated with a high risk of bleeding and infarction.
Because most sinus pericranii has benign features, asymptomatic sinus pericranii can be observed or conservatively treated 13. Although spontaneous regression of sinus pericranii has been reported 14, most patients require removal of the sinus and blocking the communicating veins. Cosmetic reasons remain the main indication for surgery in sinus pericranii 15. However, all symptomatic sinus pericranii cannot be actively treated. Using the venous drainage pattern, sinus pericranii can be classified into a dominant type or an accessory type 16. The dominant type of sinus pericranii is defined when a majority of the venous outflow occurs through the sinus pericranii. Meanwhile, when only a small portion of the venous drainage flows through the sinus pericranii, it is called as the accessory type. In the dominant sinus pericranii, active treatment should be avoided because of the consequential venous infarction and bleeding 15. On the contrary, the accessory type of sinus pericranii can be treated by surgical resection or endovascular embolization 17. Some reports suggest that surgical excisions for sinus pericranii could be considered in the presence of neurologic symptoms, psychological discomforts, dermatological changes, patient’s wishes, and coexisting morbidity. Additionally, coexisting morbidities included syndromic craniosynostosis, additional vascular anomalies, meningocerebral anomalies, and systemic anomalies or malformations 6, 7. The occlusion of this abnormal pathway has not been reported to result in intracranial venous hypertension 18.
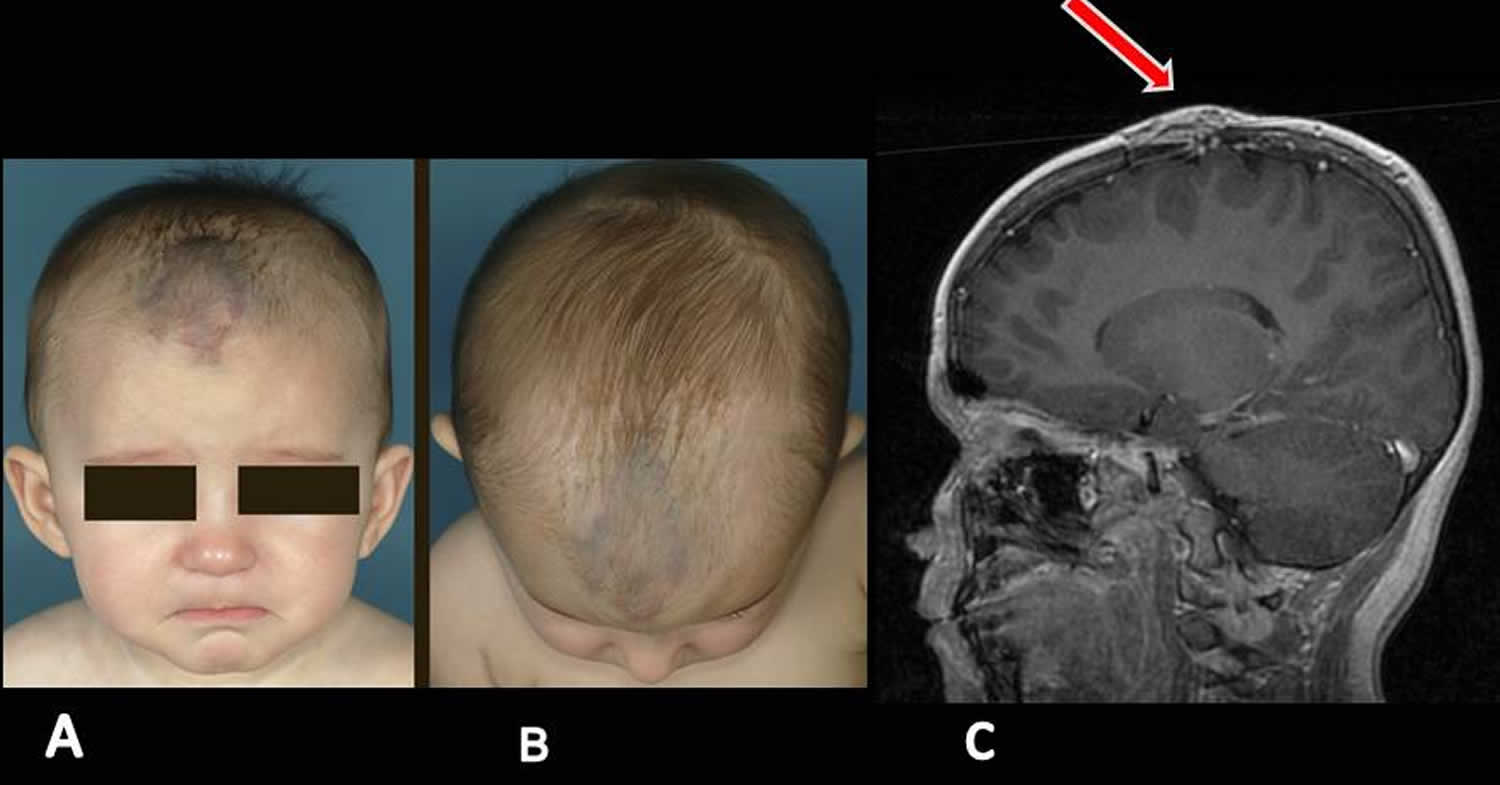
Figure 1. Sinus pericranii
Footnote: (A and B) Front and top view show a well-defined blue plate, located in the medial frontal area, the patient underwent surgery with complete removal of the sinus pericranii. (C) MRI demonstrating a sinus pericranii.
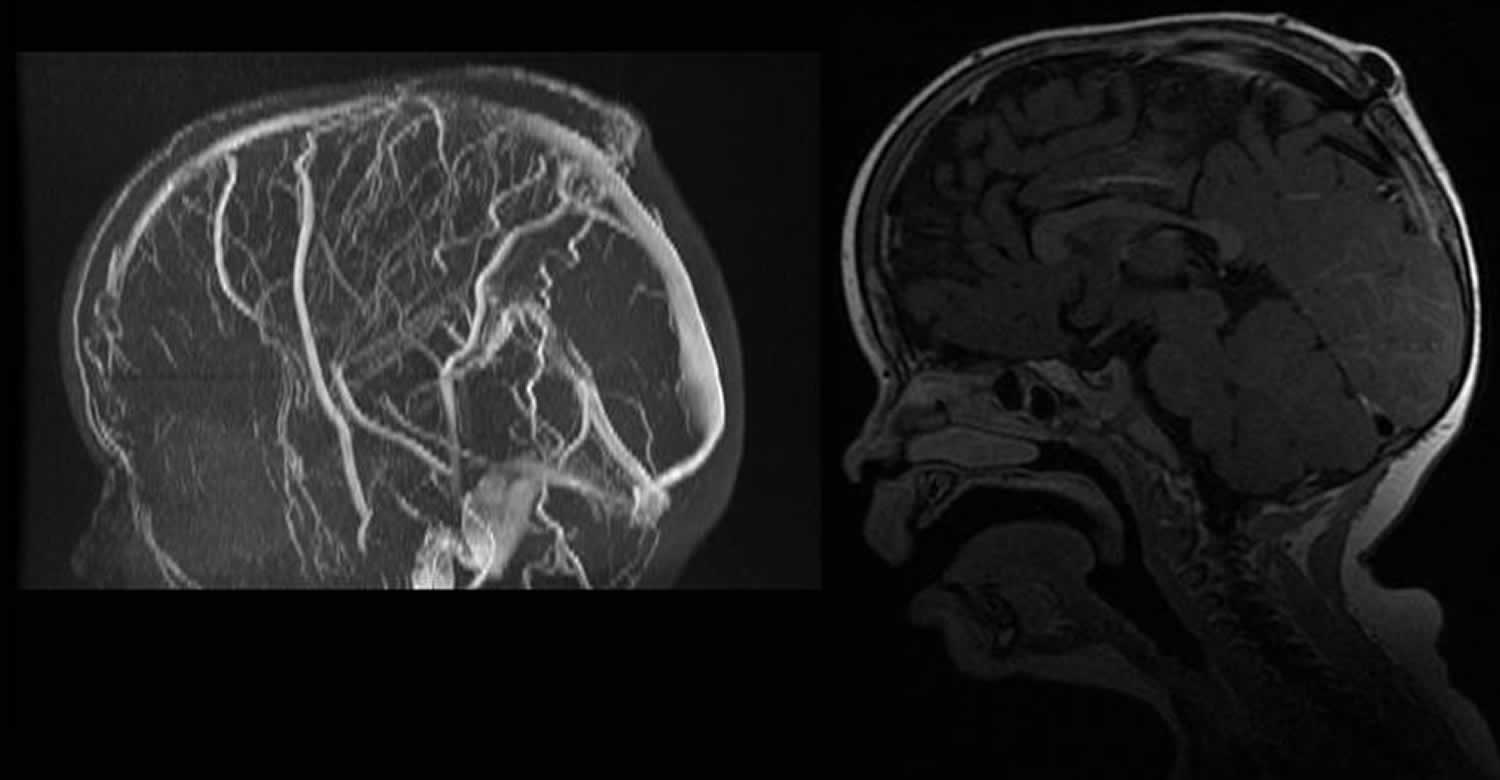
[Source 19 ]Figure 2. Sinus pericranii radiology
Footnote: MRI T2 weighted images (sagittal) and (frontal) shows venous communication between a cortical dilated vein and the superior sagittal venous sinus with bulging of the subcutaneous tissues that conditions a mass effect in the midline.
Figure 3. Sinus pericranii
Footnote: A 2-year-old girl with sinus pericranii was brought to the hospital due to an apparent disfigurement and bluish skin in the right periorbital region and a soft mass-like diffuse lesion on the scalp. The lesion was non-pulsatile and bluish, and the patient did not complain of pain. (A) Venous malformations in the right periorbital region are seen on the frontal view. (B) Vascular masses on the scalp are also seen.
[Source 1 ]Sinus pericranii causes
Sinus pericranii etiology is not fully elucidated. It is divided into three types: congenital, spontaneous, and posttraumatic 20. After trauma and cranial injuries, rich vein circulation in the skin and intracranial cavity can cause sinus pericranii 21. Sinus pericranii can spontaneously occur when there is erosion in the skull caused by increased intracranial pressure1 22. If sinus pericranii is congenital, incidence of sinus pericranii increases with other vascular pathologies such as venous angioma, aneurysmal malformations, internal cerebral vein, and cavernous hemangiomas. Thus, all cerebral vascular pathology should be considered in patients diagnosed with sinus pericranii 23.
Heinke 24 stated that vomiting, forceful coughing, respiratory disturbances and other such forces might cause tearing of emissary veins at the bone surface eventually resulting into a communicating blood cyst on the skull surface. Cohn 25 stated that the endothelial lining of the wall of the sinus pericranii differentiates the congenital type from the acquired type. Most cases of sinus pericranii are located near the midline. The frontal region is most frequently involved followed by the parietal region 9. Frontal sinus pericranii with an orbital extension has not been reported in the literature. Usually the patients are not symptomatic and the problems are cosmetic. Rarely there may be headache, giddiness and vertigo.
Sinus pericranii may be part of a syndrome in some patients, but can occur as an isolated condition. Associations with craniosynostosis, Crouzon’s syndrome, Apert’s syndrome and Hunter’s syndrome are well documented 26.
Sinus pericranii differential diagnosis
Sinus pericranii differential diagnosis includes arteriovenous malformation, epicranial varix, cavernoma, growing skull fracture, eosinophilic granuloma, epidermoid tumour, dermoid, meningocele and encephalocele.
Sinus pericranii symptoms
Most sinus pericranii patients visit their doctor primarily complaining of the mass on the scalp. The distribution of the lesions is more commonly found in the frontal region (43%), followed by parietal (36%) and occipital regions (7.4%) 4. A lateral location is unusual 5. Some sinus pericranii patients may present with mild (local pain, nausea, headache, and dizziness) to severe (increased intracranial pressure, bradypnea, bradycardia, ataxia, hearing loss, and epileptic seizures) symptoms 6. The main concern is usually cosmetic due to the bulging nature of the malformation. The sinus pericranii are reported to be associated with vascular malformation, haemangioma of the cerebellum or retina as a part of the von Hippel-Lindau syndrome, blue naevus syndrome, venous cavernoma of the scalp and hemangioma of the tongue.
Coexisting diseases associated with sinus pericranii have been reported, such as cerebellar venous angioma 27, blue rubber bleb nevus syndrome 28, arteriovenous malformation 29, dural sinus malformation 29, vein of Galen aneurysmal malformation 29, cavernous hemangioma 30, aneurysmal malformation of the internal cerebral vein 31, vein of Galen aplasia 29, PHACE syndrome 32, craniosynostosis 33, and subcutaneous venous cavernoma 34.
Sinus pericranii complications
The occurrence of thrombosis is common in sinus pericranii because of the slow flow of blood within the sinus pericranii as well as the common occurrence of thrombi within venous malformations elsewhere in the body 35. If dominant venous drainage had been affected by trauma or thrombosis, a life-threatening complication may occur, such as venous congestion and/or infarction, brain swelling, or hemorrhage. The possible complications during surgery are hemorrhage and air embolism 9.
Awareness of both the patency and direction of flow in a dominant emissary vein is important for preventing life-threatening complications during surgery. Although intraoperative cerebral angiography or indocyanine green video-angiography can be used to evaluate the venous flow, these are invasive methods that only provide intermittent monitoring. Alternatively, ultrasonography is non-invasive and inexpensive relative to other imaging modalities, and can provide continuous evaluation of venous flow during surgery. As in the present case, ultrasonography can also detect extracranial venous tubular structures and visualize the emissary vein. Moreover, color Doppler ultrasonography can confirm venous flow in these tubular structures and reveal both the direction and pattern of venous flow in the emissary vein 36. Recent advances in technology have yielded a variety of ultrasonography probes suitable for diverse operative situations.
Sinus pericranii diagnosis
The diagnosis of sinus pericranii can be made by the appearance of soft, fluctuant mass located near the intracranial sinus, which usually vary in size with change in the intracranial pressure. Confirmation of sinus pericranii can be identified by various imaging techniques such as CT scan, MRI and Doppler ultrasonography. CT scanning allows direct visualization of the bony defect. MRI with or without MR angiography is believed to be of great benefit at providing a definitive diagnosis of sinus pericranii and its drainage into the dural sinuses 37. Angiography can separate sinus pericranii into two patterns; dominant and accessory.
Sinus pericranii treatment
There is little available evidence with regards to available guidelines and recommendations concerning the management of sinus pericranii 15. Previous reports on sinus pericranii included surgical treatment, endovascular embolization, and conservative treatment 20, 6, 38, 39, 40, 41. A recent retrospective study by Pavanello et al 42, looking at the diagnosis and management in 21 pediatric patients, suggests that only accessory sinus pericranii is amenable to treatment, whereas dominant sinus pericranii must be preserved due to its potential life-threatening complications associated with it, such as hemorrhage and venous congestion.
Endovascular approach to treatment has proven to be safe and effective when treated for cosmetic reasons, in cases of accessory sinus pericranii. Digital subtraction angiography has proven to be effective in excluding other vascular malformations as well as assessing the intracranial venous dynamics and their relationship to the sinus pericranii 43. While this has been rarely reported in the available literature, endovascular embolisation appears to have good results when patients are identified for potential complications 44. This method of managing sinus pericranii is less invasive than surgery but still carries the risk of causing skin necrosis and embolic events 45.
Surgical management has been demonstrated in a retrospective study conducted by Park et al 46 where 10 patients underwent operations for sinus pericranii. All patients with sinus pericranii associated with craniosynostosis were managed conservatively. This study concluded that surgery can be performed in cases without intracranial venous compromise. Surgery can be safely carried out with thorough preoperative planning and imaging of the cranial vault.
Conservative management has rarely been reported in the literature with regards to follow-up. One case reports the case of a 6-year-old who was safely managed through this method 47. Surveillance proved an effected method of monitoring the condition, with no reported complications. Another retrospective study identified four patients with untreated accessory sinus pericranii, two of which resolved spontaneously, one was lost in follow-up and the remaining one was unchanged.
Sinus pericranii prognosis
Due to sinus pericranii rarity, its pathogenesis and natural history remains unclear. The long-term outcomes of sinus pericranii are poorly understood 15.
- Ryu JY, Lee JH, Lee JS, et al. Combined treatment of surgery and sclerotherapy for sinus pericranii. Arch Craniofac Surg. 2020;21(2):109-113. doi:10.7181/acfs.2019.00521 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7206457[↩][↩][↩]
- Pons Escoda A, Naval Baudin P, Mora P, et al. Imaging of skull vault tumors in adults. Insights Imaging. 2020;11(1):23. Published 2020 Feb 13. doi:10.1186/s13244-019-0820-9 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7018895[↩]
- Amuluru K, Al-Mufti F, Shah M, Prestigiacomo CJ, Liu JK, Gandhi CD. Acquired Sinus Pericranii Due To Parasagittal Meningiomatous Invasion of the Superior Sagittal Sinus and Bilateral Transverse Sinuses. World Neurosurg. 2017 Feb;98:872.e5-872.e9. doi: 10.1016/j.wneu.2016.11.129[↩]
- Akram H, Prezerakos G, Haliasos N, et al. . Sinus pericranii: an overview and literature review of a rare cranial venous anomaly. Neurosurg Rev 2012;35:15–26.[↩][↩]
- Vaquero J, de Sola RG, Martinez R : Lateral sinus pericranii. Case report. J Neurosurg1983; 58 : 139-140.[↩][↩]
- Pavanello M, Melloni I, Antichi E, Severino M, Ravegnani M, Piatelli G, et al. Sinus pericranii: diagnosis and management in 21 pediatric patients. J Neurosurg Pediatr. 2015;15:60–70.[↩][↩][↩][↩]
- Gandolfo C, Krings T, Alvarez H, Ozanne A, Schaaf M, Baccin CE, et al. Sinus pericranii: diagnostic and therapeutic considerations in 15 patients. Neuroradiology. 2007;49:505–14.[↩][↩]
- Zamora C, Castillo M. Sinus Pericranii. In: Agrawal A, Britz G, editors. Pediatric vascular neurosurgery: principles and practice of neurovascular disorders (part 1) Cham: Springer International Publishing; 2016. pp. 165–175.[↩]
- Bollar A, Allut AG, Prieto A et al : Sinus pericranii: radiological and etiolopathological considerations. J Neurosurg1992; 77: 469-472.[↩][↩][↩]
- Newton TH, Troost BT : Arteriovenous malformations and fistulae, In : Radiology of the skull and brain, Newton TH, Potts DG (eds): Vol II. Specific disease processes. CV Mosby St Louis. 1974; 2490-2565.[↩]
- Ryu JY, Lee JS, Lee JW, Choi KY, Yang JD, Cho BC, et al. Clinical approaches to vascular anomalies of the lip. Arch Plast Surg. 2015;42:709–15.[↩]
- Akram H, Prezerakos G, Haliasos N, O’Donovan D, Low H. Sinus pericranii: an overview and literature review of a rare cranial venous anomaly (a review of the existing literature with case examples) Neurosurg Rev. 2012 Jan;35(1):15–26. discussion 26.[↩]
- Chung YS, Kim JJ, Kim SH, Chung J, Lee JW, Park KY. Symptomatic Sinus Pericranii with Adult Onset Headache: A Case Report with Pathologic Perspective. J Cerebrovasc Endovasc Neurosurg. 2019;21(3):163-168. doi:10.7461/jcen.2019.21.3.163 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6911930[↩]
- Hayakawa I, Fujiwara K, Sasaki A et al : Spontaneous regression of sinus pericranii, report of a case. No Shinkei Geka 1978; 6 : 91-95.[↩]
- Goffin J, MacKenzie SA, Tallur KK, Kaliaperumal C. Sinus pericranii: long-term outcome in a 10-year-old boy with a review of literature. BMJ Case Rep. 2018;2018:bcr2017223631. Published 2018 Mar 20. doi:10.1136/bcr-2017-223631 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5878362[↩][↩][↩][↩]
- Gandolfo C, Krings T, Alvarez H, Ozanne A, Schaaf M, Baccin CE. Sinus pericranii: diagnostic and therapeutic considerations in 15 patients. Neuroradiology. 2007 Jun;49(6):505–514.[↩]
- Rangel-Castilla L, Krishna C, Klucznik R, Diaz O. Endovascular embolization with Onyx in the management of sinus pericranii: a case report. Neurosurg Focus. 2009 Nov;27(5):E13[↩]
- Buxton N, Vloeberghs M : Sinus pericranii. Report of a case and review of the literature. Pediatr Neurosurg1999; 30 : 96-99.[↩]
- Sinus pericranii: diagnosis and management in 15 pediatric patients. https://dx.doi.org/10.1594/ecr2018/C-2128[↩][↩]
- Aburto-Murrieta Y, Bonifacio-Delgadillo D, Balderrama Banares J, Zenteno Castellanos MA. Sinus pericranii: case report. Vasc Endovascular Surg. 2011;45:103–5.[↩][↩]
- Güler, S., & Tatlı, B. (2015). Rare vascular pathology sinus pericranii; becomes symptomatic with pseudotumor cerebri. The Turkish journal of pediatrics, 57 6, 618-620. http://www.turkishjournalpediatrics.org/uploads/pdf_TJP_1536.pdf[↩]
- Ota T, Waga S, Handa H, Nishimura S, Mitani T. Sinus pericranii. J Neurosurg 1975; 42: 704-712.[↩]
- Luker GD, Siegel MJ. Sinus pericranii: sonographic findings. AJR Am J Roentgenol 1995; 165: 175-176.[↩]
- Heinke W : Die chirurgischen Krankheiten des Kopfes. Dtsch Chir1882; 31 : 56-66.[↩]
- Cohn I : Sinus pericranii. Report of a case, review of literature. Surg Gynecol Obstet 1926; 42 : 614-624.[↩]
- Brisman JL, Niimi Y, Berenstein A. Sinus pericranii involving the torcular sinus in a patient with Hunter’s syndrome and trigonocephaly: Case report and review of the literature. Neurosurgery. 2004;55:433.[↩]
- Nomura S, Kato S, Ishihara H, Yoneda H, Ideguchi M, Suzuki M: Association of intra- and extradural developmental venous anomalies, so-called venous angioma and sinus pericranii. Childs Nerv Syst 22: 428– 431, 2006.[↩]
- Gabikian P, Clatterbuck RE, Gailloud P, Rigamonti D: Developmental venous anomalies and sinus pericranii in the blue rubber-bleb nevus syndrome. Case report. J Neurosurg 99: 409– 411, 2003.[↩]
- Gandolfo C, Krings T, Alvarez H, Ozanne A, Schaaf M, Baccin CE, Zhao WY, Lasjaunias P: Sinus pericranii: diagnostic and therapeutic considerations in 15 patients. Neuroradiology 49: 505– 514, 2007.[↩][↩][↩][↩]
- Poppel MH, Roach JF, Hamlin H: Cavernous hemangioma of the frontal bone with report of a case of sinus pericranii. Am J Roentgenol Radium Ther 59: 505– 510, 1948.[↩]
- Nakayama T, Matsukado Y: Sinus pericranii with aneurysmal malformation of the internal cerebral vein. Surg Neurol 3: 133– 137, 1975.[↩]
- Drosou A, Benjamin L, Linfante I, Mallin K, Trowers A, Wakhloo AK, Thaller SR, Schachner LA: Infantile midline facial hemangioma with agenesis of the corpus callosum and sinus pericranii: another face of the PHACE syndrome. J Am Acad Dermatol 54: 348– 352, 2006.[↩]
- Mitsukawa N, Satoh K, Hayashi T, Furukawa Y, Suse T, Uemura T, Hosaka Y: Sinus pericranii associated with craniosynostosis. J Craniofac Surg 18: 78– 84, 2007.[↩]
- Ota T, Waga S, Handa H, Nishimura S, Mitani T: Sinus pericranii. J Neurosurg 42: 704– 712, 1975.[↩]
- Osanai T, Houkin K. Adult-Onset Orbital Sinus Pericranii with T2 Hyperintensity Lesion: A Case Report. Case Rep Neurol. 2018;10(1):112-117. Published 2018 Apr 24. doi:10.1159/000488477 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5968242[↩]
- Yanik B, Keyik B, Conkbayir I, Kuru AA, Hekimodlu B: Sinus pericranii: color Doppler ultrasonographic findings. J Ultrasound Med 25: 679– 682, 2006.[↩]
- Higuchi M, Fujimoto Y, Ikeda H, et al. . Sinus pericranii: neuroradiologic findings and clinical management. Pediatr Neurosurg 1997;27:325–8. 10.1159/000121278[↩]
- Shaw AV, Jayamohan J, Sheerin F, Johnson D. Staged raising of a coronal flap for fronto-orbital advancement and remodeling in saethre-chotzen syndrome complicated by sinus pericranii. J Craniofac Surg. 2018;29:1956–9.[↩]
- Tamura G, Ogiwara H, Morota N. Characteristics of recurrent congenital sinus pericranii: case report and review of the literature. Pediatr Neurosurg. 2019;54:265–9.[↩]
- Ito E, Takasu S, Hattori K. Sinus pericranii with dominant venous outflow in the superior eyelid. Neurol Med Chir (Tokyo) 2017;57:144–8.[↩]
- Ohshima T, Miyachi S, Joko M, Matsuo N, Kawaguchi R, Maejima R, et al. Endovascular embolization of sinus pericranii using plastic cup during glue injection. World Neurosurg. 2019;124:93–7.[↩]
- Pavanello M, Melloni I, Antichi E, et al. . Sinus pericranii: diagnosis and management in 21 paediatric patients. J Neurosurg Pediatr 2015:15, 1.[↩]
- Brook AL, Gold MM, Farinhas JM, et al. . Endovascular transvenous embolization of sinus pericranii. Case report. J Neurosurg Pediatr 2009;3:220–4. 10.3171/2008.10.PEDS08267[↩]
- Rangel-Castilla L, Krishna C, Klucznik R, et al. . Endovascular embolization with Onyx in the management of sinus pericranii: a case report. Neurosurg Focus 2009;27:E13 10.3171/2009.8.FOCUS09170[↩]
- Kessler IM, Esmanhoto B, Riva R, et al. . Endovascular transvenous embolization combined with direct punction of the sinus pericranii. A case report. Interv Neuroradiol 2009;15:429–34. 10.1177/159101990901500410[↩]
- Park SC, Kim SK, Cho BK, et al. . Sinus pericranii in children: report of 16 patients and preoperative evaluation of surgical risk. J Neurosurg Pediatr 2009;4:536–42. 10.3171/2009.7.PEDS0994[↩]
- Brix M, Bessaguet S, Loury J, et al. . [Sinus pericranii: a rare transcranial venous anomaly]. Rev Stomatol Chir Maxillofac 2009;110:96–100.[↩]