Status epilepticus
Status epilepticus also known as ‘status’ or continuous seizures, is a tonic clonic seizure that does not stop or one seizure follows another without the person fully regain consciousness between recurring seizures. Status epilepticus is a medical emergency, a life-threatening neurologic disorder that is essentially an acute, prolonged epileptic crisis 1. Prolonged status epilepticus can lead to cardiac dysrhythmia, metabolic derangements, autonomic dysfunction, neurogenic pulmonary edema, hyperthermia, rhabdomyolysis, and pulmonary aspiration. Permanent neurologic damage can occur with prolonged status epilepticus 2. Status epilepticus is the most common pediatric neurological emergency 3. Status epilepticus was defined as a continuous seizure lasting more than 30 min, or two or more seizures without full recovery of consciousness between any of them 1. The Neurocritical Care Society guidelines from 2012 revised the definition of status epilepticus to a seizure with 5 minutes or more of continuous clinical and/or electrographic seizure activity, or recurrent seizure activity without recovery between seizures 4. There is some evidence that 5 minutes is sufficient to damage neurons and that seizures are unlikely to end on their own, making it necessary to seek medical care immediately. One study showed that 80 percent of people in status epilepticus who received medication within 30 minutes of seizure onset eventually stopped having seizures, whereas only 40 percent recovered if 2 hours had passed before they received medication. The mortality rate can be as high as 20 percent if treatment is not initiated immediately 5.
Status epilepticus can be convulsive (in which outward signs of a seizure are observed) or nonconvulsive (which has no outward signs and is diagnosed by an abnormal EEG) or refractory.
- Convulsive status epilepticus consists of generalized tonic-clonic movements and mental status impairment 2.
- Non-convulsive status epilepticus is defined as seizure activity identified on an electroencephalogram (EEG), with no accompanying tonic-clonic movements. Non-convulsive status epilepticus may appear as a sustained episode of confusion, agitation, loss of consciousness, or even coma.
- Refractory status epilepticus is defined as continuing seizures (convulsive or non-convulsive) lasting longer than 60 minutes despite administration of appropriate anti-epileptic drugs such benzodiazepine (lorazepam) and another standard anticonvulsant (usually phenytoin/fosphenytoin) in adequate loading dose 6. About 9–31% of patients with status epilepticus may fail to respond to standard treatment. This subgroup of refractory status epilepticus has greater morbidity and mortality.
- Malignant status epilepticus is a severe variant of refractory status epilepticus, in which the seizure fails to respond to aggressive treatment with even anesthetic agents. It typically occurs in young patients (18–50 years) in the setting of encephalitis.
Most seizures terminate spontaneously; status epilepticus represents a failure of seizure termination. Status epilepticus can represent an exacerbation of a preexisting seizure disorder or the initial manifestation of a seizure disorder (epilepsy), or it can represent an insult other than a seizure disorder. Among such insults, status epilepticus can occur in the context of an acute cerebral injury, or be due to a systemic process or illness, in a patient with or without a remote cerebral injury. In patients with known epilepsy, the most common cause of status epilepticus is a change in medication.
Status epilepticus is a common medical emergency associated with high morbidity and mortality. Mortality from status epilepticus varies from 3–50% in different studies. The short-term mortality (within 30 days) of status epilepticus ranges from 7.6% to 22% across all age groups and is highest amongst the elderly 7. In elderly patients, refractory status epilepticus may lead to death in over 76% cases 8. The lifetime prevalence of status epilepticus in persons with epilepsy range from 1–16%. It has been estimated that up to 150,000 cases of status epilepticus occur annually in the US, with 55,000 associated deaths 9. The incidence of status epilepticus in the US ranges from 7 to 40 per 100,000 population per year 2. Status epilepticus seems to be more common in males. A significant proportion of both children (16% to 38%) and adults (42% to 50%) with status epilepticus have a history of epilepsy.
If you see someone having a seizure or fit, there are some simple things you can do to help. You should call an ambulance if you know it’s their first seizure or it’s lasting longer than 5 minutes.
It might be scary to witness, but don’t panic.
- Do not try to restrain the person or stop the jerking.
- Don’t try to move them. Only move them if they’re in danger – such as near a busy road or hot cooker.
- Don’t put anything in their mouth, including your fingers. They shouldn’t have any food or drink until they fully recover.
- Protect the patient from harming themselves.
- Put something soft under their head.
- Loosen any tight clothing around their neck – such as a collar or tie to – aid breathing
- Time the seizure.
- Put them on their side in the recovery position as soon as the jerking stops, or immediately if they have vomited or have food or fluid in their mouth.
- Don’t wake them up, but do check their breathing.
- Look after any injuries they may have.
If they’re in a wheelchair, put the brakes on and leave any seatbelt or harness on. Support them gently and cushion their head, but don’t try to move them.
Call your local emergency services number if:
- the seizure continues for more than 5 minutes or a second seizure quickly follows
- the patient remains unresponsive for more than 5 minutes after a seizure stops
- the patient has been injured
- the patient has diabetes or is pregnant
- you know, or believe it to be the patient’s first seizure.
People with epilepsy don’t always need to go to hospital every time they have a seizure.
Some people with epilepsy wear a special bracelet or carry a card to let medical professionals and anyone witnessing a seizure know they have epilepsy.
Figure 1. Recovery position

Status epilepticus classification
Semiologically and electrophysiologically there are several types of seizures; these have been broadly classified as either generalized or partial seizures by the International League Against Epilepsy. In principle there can be as many types of status epilepticus as there are types of seizures. This has led to complex classifications of status epilepticus. However, using electroclinical features, status epilepticus may be classified broadly as convulsive status epilepticus and nonconvulsive status epilepticus.
Convulsive status epilepticus
Convulsive status epilepticus can be further classified into:
- Tonic–clonic status epilepticus,
- Tonic status epilepticus,
- Clonic status epilepticus and
- Myoclonic status epilepticus.
Generalized tonic–clonic status epilepticus is the most common form of status epilepticus. Myoclonic status epilepticus presents as a bilateral massive myoclonus, along with polyspike discharges on electroencephalogram (EEG), and usually carries a good prognosis. But the myoclonic status that follows severe hypoxic-ischemic insult, viral encephalitis, and prion disease is associated with poor prognosis.
Nonconvulsive status epilepticus
Non-convulsive status epilepticus refers to continuous or near-continuous generalized electrical seizure activity lasting for at least 30 min, but without physical convulsions. Cstatus epilepticus may evolve into the nonconvulsive form after treatment or non-convulsive status epilepticus may arise de novo. Non-convulsive status epilepticus is characterized by abnormal mental status, unresponsiveness, ocular motor abnormalities, persistent electrographic seizures, and possible response to anticonvulsants 6. All patients with prolonged postictal confusion or unexplained coma should undergo electroencephalogram (EEG) monitoring for confirmation 10. Non-convulsive status epilepticus has long been divided into two main categories: absence status epilepticus and complex partial status epilepticus. Until recently most cases of non-convulsive status epilepticus were considered to be absence status epilepticus, and complex partial status epilepticus was thought to be a rarity. Several investigators have shown that complex partial status epilepticus is more common than previously thought and that many cases of absence status epilepticus are actually cases of complex partial status epilepticus that have generalized. Tomson et al. 11 reported on 32 consecutive non-convulsive status epilepticus patients, most of who had complex partial status epilepticus, and suggested that in adults most cases of non-convulsive status epilepticus are in fact partial in onset. The distinction between absence status epilepticus and complex partial status epilepticus is an important one, as absence status epilepticus is usually easier to treat and may not be associated with significant neuronal damage.
Refractory status epilepticus
Refractory status epilepticus is defined as continuing seizures (convulsive or non-convulsive) lasting longer than 60 minutes despite administration of appropriate anti-epileptic drugs such benzodiazepine (lorazepam) and another standard anticonvulsant (usually phenytoin/fosphenytoin) in adequate loading dose 6. About 9–31% of patients with status epilepticus may fail to respond to standard treatment. This subgroup of refractory status epilepticus has greater morbidity and mortality.
Malignant status epilepticus is a severe variant of refractory status epilepticus, in which the seizure fails to respond to aggressive treatment with even anesthetic agents. It typically occurs in young patients (18–50 years) in the setting of encephalitis.
Status epilepticus causes
There are multiple etiologies for status epilepticus 12. Nearly a quarter of persons presenting with status epilepticus have preexisting epilepsy 1. A dramatic drop in serum levels of antiepileptic drugs due to noncompliance or other reasons is the most common mechanism of status epilepticus in such instances. In many patients with a preexisting seizure disorder, no obvious precipitating factor can be identified for the occurrence of status epilepticus. Status epilepticus is more common in patients with secondary generalized epilepsy than in those with idiopathic generalized epilepsy.
Potential acute processes include:
- Central nervous system (CNS) infections (meningitis, encephalitis, and intracranial abscess)
- Metabolic abnormalities (hypoglycemia, hyponatremia, hypocalcemia, hepatic encephalopathy, and inborn errors of metabolism in children)
- Cerebrovascular accidents
- Head trauma (with or without intracranial bleed)
- Drug toxicity
- Drug withdrawal syndromes (e.g., alcohol, benzodiazepines, and barbiturates)
- Hypoxia
- Hypertensive emergency
- Autoimmune disorders
Commonly used drugs that may predispose to status epilepticus by lowering the seizure threshold or by increasing the clearance of antiepileptic drugs 1:
- Antibiotics (especially in older adults or in patients with renal impairment)
- Penicillins
- Imipenem
- Cephalosporins
- Isoniazid
- Metronidazole
- Erythromycin
- Ciprofloxacin, ofloxacin
- Antihistamines
- Diphenhydramine
- Antipsychotics
- Clozapine, chlorpromazine
- Antidepressants
- Maprotiline
- Bupropion
- Tricyclics, especially clomipramine
- Other drugs
- Fentanyl
- Flumazenil
- Ketamine
- Lidocaine
- Lithium
- Meperidine
- Propoxyphene
- Theophylline
- Baclofen (acute withdrawal)
The causes of status epilepticus may differ according to the age at presentation and geographic location. For example, central nervous system (CNS) infections may predominate in children and cerebral malaria can be a common cause in malaria endemic area 13. In patients with status epilepticus and CNS infection, 24.3% had a refractory status that was associated with a high mortality 14.
Chronic processes that may result in status epilepticus include, pre-existing epilepsy with breakthrough seizures or non-use of anti-epileptic drugs, ethanol withdrawal, central nervous system (CNS) tumors, and remote central nervous system pathology (e.g., traumatic brain injury, stroke).
Acute processes account for most cases of status epilepticus in adults. Febrile status epilepticus is the most common cause in pediatric patients. Central nervous system (CNS) infections and inborn errors of metabolism are also common etiologies in children. The majority of pediatric patients with the first presentation of status epilepticus have no previous history of seizures.
More than half of status epilepticus episodes occur in patients without a history of prior seizures. Genetic factors may also play a role as twin studies have demonstrated a greater concordance in monozygotic as opposed to dizygotic twins. Cerebral toxoplasmosis, lymphoma, and anticonvulsant withdrawal are important causes of status epilepticus in HIV infection.
Pathophysiology
A seizure is a paroxysmal electrical discharge of the neurons in the brain resulting in a change of function or behavior. It is important to understand that a seizure is a CNS event and may present as convulsive or non-convulsive. There are both excitatory neurotransmitters (glutamate, aspartate, and acetylcholine) and inhibitory neurotransmitters (gamma-aminobutyric acid) and mechanisms (calcium ion-dependent potassium ion current, and magnesium blockade of N-methyl-d-aspartate (NMDA)) in the brain that play a role in the genesis and inhibition of isolated seizures. Excessive excitation and/or inadequate inhibition results in status epilepticus.
Status epilepticus symptoms
Status epilepticus is defined as a seizure with 5 minutes or more of continuous clinical and/or electrographic seizure activity, or recurrent seizure activity without recovery between seizures. The findings of convulsive status epilepticus include generalized tonic-clonic movements of the extremities and impaired mental status. Temporary focal neurological deficits (e.g., Todd’s paralysis) may be present in the post-ictal period. Non-convulsive status epilepticus presents with impaired mental status, and may or may not have subtle motor signs such as tonic eye deviation. In non-convulsive status epilepticus, seizure activity is seen on the electroencephalogram (EEG) despite the absence or paucity of overt clinical signs.
Status epilepticus key features include:
Airway
- Airway compromise
- Secretions and trismus are common
- Complete airway obstruction is very rare
Breathing
- Peri-oral cyanosis common
Circulation
- Tachycardia and poor peripheral perfusion common
- Shock uncommon (if present consider sepsis as underlying cause)
Disability
- Check blood glucose
- Give IV glucose if low (2mLs/kg 10% glucose)
Is the patient still convulsing?
- Critical concept is the longer seizures = less motor movements
- Limb Tone
- Pupils – if unreactive then ongoing seizure likely
- Eyes – if deviation of both eyes then ongoing seizure likely, however absence of eye deviation does not exclude ongoing seizure activity
- Response to pain – bilateral localization to pain
Status epilepticus diagnosis
The diagnosis of convulsive status epilepticus is made clinically but occasionally, the diagnosis of status epilepticus can be difficult. Fulminant tonic–clonic movements with frothing, and dysautonomic features with loss of consciousness are important pointers to the diagnosis of status epilepticus. Moreover, there are several other conditions that may mimic status epilepticus at some point of time.
Although the diagnosis of convulsive status epilepticus is made clinically, it requires emergent neuroimaging and laboratory studies to identify a potential cause. A head computed tomography (CT) scan is appropriate in most situations and most easily obtained. Magnetic resonance imaging (MRI) of the brain is more sensitive for identifying malformations in pediatric patients, but may be difficult to obtain and may require sedation.
Blood investigations in a patient with status epilepticus:
- Random blood sugar
- Electrolytes – sodium, potassium, calcium, magnesium
- Complete blood count
- Renal function test, liver function test
- Antiepileptic drug level
- Arterial blood gas
Laboratory studies should include bedside blood glucose level, serum electrolytes (sodium, potassium, calcium, and magnesium), BUN, creatinine, serum bicarbonate, a complete blood count, and a lumbar puncture with cerebrospinal fluid (CSF) evaluation. If the patient has a known seizure disorder, anti-epileptic drug levels should be obtained. Suspicion of toxic ingestion mandates toxicology studies (e.g., urine toxicology screen, serum levels of specific toxins such as theophylline or lithium). Other studies may be considered based on the presentation (liver function tests, inborn errors of metabolism, and coagulation studies). A pregnancy test should be obtained in all women of child-bearing years. An electroencephalogram (EEG) should be obtained. Non-convulsive status epilepticus requires all of the previously mentioned imaging and laboratory studies for identification of an underlying etiology, but also requires electroencephalogram (EEG) monitoring for diagnosis 15.
Status epilepticus treatment
Status epilepticus must be addressed quickly and in an organized manner, with simultaneous assessment/management of the airway, breathing, and circulation, while also administering antiepileptic drug treatment. The primary goal of management is to definitively abort seizure activity as rapidly as possible while supporting the patient’s cardiovascular and respiratory status 16.
- Position the head to maintain an open airway (rapid sequence intubation may be necessary at any point during management if oxygenation or ventilation is impaired).
- Provide supplemental oxygen.
- Initiate monitoring of the heart rate, respiratory rate, blood pressure, and oxygen saturation.
- Obtain vascular access.
- Check a bedside blood glucose and treat hypoglycemia if present (if thiamine deficiency a possibility, administer thiamine before dextrose).
- Benzodiazepines are the antiepileptic drug of choice for emergent control treatment. A repeat dose may be administered if seizures do not resolve following the first dose. Intravenous administration is preferred, but benzodiazepines can be administered via the intramuscular, rectal, nasal, or buccal route if vascular access is not available.
- If benzodiazepines do not abort the seizures, other antiepileptic drug choices include fosphenytoin, phenobarbital, levetiracetam, and valproic acid (concern for hepatotoxicity with valproic acid use in children younger than two years).
- Urgent control therapy with an antiepileptic drug (fosphenytoin, phenobarbital, levetiracetam, or valproic acid) following seizure control is required in all patients.
- Refractory status epilepticus should be treated with a continuous infusion of an antiepileptic drug. Choices include an intravenous (IV) infusion of midazolam, pentobarbital, thiopental, or propofol (propofol infusion should not be used in children due to the risk of propofol infusion syndrome).
- Magnesium sulfate is indicated for pregnant women with eclampsia.
- A neurologist should be consulted early in the treatment stage right after the administration of first-line therapy.
All patients with status epilepticus require hospital admission, preferably to the intensive care unit.
In 2016, the American Epilepsy Society issued new guidelines for the treatment of status epilepticus. The guidelines provide a time-dependent treatment algorithm that includes four phases 17.
In the stabilization phase, standard first-aid for seizures should be initiated.
In the initial therapy phase, a benzodiazepine (specifically IM midazolam, IV lorazepam, or IV diazepam) is recommended as initial therapy.
In the second phase, options include IV fosphenytoin, valproic acid, or levetiracetam. If none of these is available, IV phenobarbital is a reasonable alternative.
In the third phase, if a patient experiences 40+ minutes of seizure activity, treatment considerations should include repeating second-line therapy or anesthetic doses of thiopental, midazolam, pentobarbital, or propofol.
Status epilepticus in pregnancy
In the setting of status epilepticus, fetal well-being is dependent on immediate, successful management of seizure activity in the mother. Lorazepam is recommended for emergency control treatment if status epilepticus occurs during the first trimester. Levetiracetam should be considered for urgent control therapy in this setting as evidence suggests a lower risk of associated congenital disabilities in comparison to some other antiepileptic drugs (phenytoin, valproate sodium, and phenobarbital). If eclampsia is suspected, intravenous magnesium sulfate is the antiepileptic drug of choice. Delivery of the fetus is the definitive treatment of eclampsia.
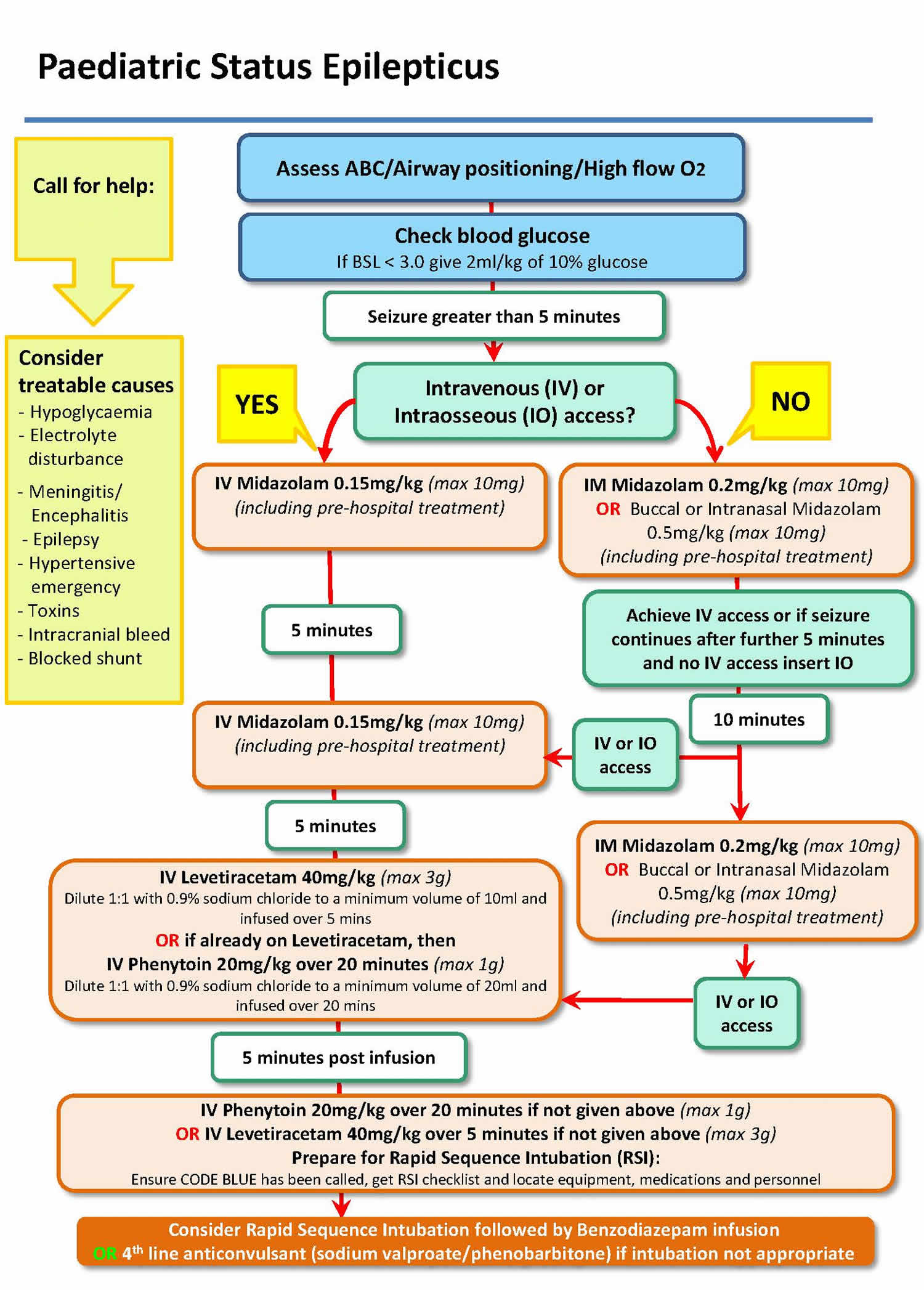
Status epilepticus in children
Prehospital care
Supportive care, including ABCs, must be addressed in the prehospital setting. If the seizure fails to stop within 4-5 minutes or if the patient is continuing to seize at the time of emergency medical system (EMS) personnel arrival, prompt administration of anticonvulsants may be necessary.
Because of the refrigeration requirements and the infrequent use of most anticonvulsants, diazepam (Valium) is often the only anticonvulsant available in the prehospital setting. Diazepam may be administered intravenously (IV) or per rectum. Midazolam (Versed) is available in some emergency medical systems and is currently the subject of study because of the option for intramuscular and intranasal administration.
If persons who know the patient, or who witnessed the onset of the seizures, are present at the scene, EMS providers may be able to collect information that offers clues to the cause of the status epilepticus.
Emergency Department Care
Regardless of the clinical manifestations of generalized status epilepticus, aggressive supportive care and prompt termination of electrical seizure activity are the goals. Care is individualized to the patient.
Establish intravenous access, ideally in a large vein. Intravenous administration is the preferred route for anticonvulsant administration because it allows therapeutic levels to be attained more rapidly. Begin cardiac and other hemodynamic monitoring.
Administer a 50-mL bolus of 50% dextrose IV and 100 mg of thiamine. If seizure activity does not terminate within 4-5 minutes, start anticonvulsant medication. If emergency medical system history has already defined status epilepticus, treatment should begin immediately. In some settings where drug intoxication might be likely, consider also adding naloxone at 0.4-2.0 mg IV to the dextrose bag.
Administer diazepam (0.15 mg/kg) or lorazepam (0.1 mg/kg) IV over 5 minutes, followed by fosphenytoin or phenytoin. Fosphenytoin is preferable, as it provides the advantage of a potentially rapid rate of administration with less risk of venous irritation (eg, to avoid the risk of purple-glove syndrome with phenytoin).
Fosphenytoin is given in a dose of 15-20 mg phenytoin equivalents [PE]/kg, at a rate not to exceed 150 mg PE/min). The dose of phenytoin is 18-20 mg/kg, at a rate not to exceed 50 mg/min). Never mix phenytoin with a 5% dextrose solution; put it in a normal saline solution to minimize the risk of crystal precipitation.
Ensure airway control. Nasopharyngeal airway placement is sufficient for some patients, particularly if the seizures are stopped and the patient is awakening. For other patients, endotracheal intubation is necessary. In neuromuscular paralysis, rapid sequence induction is necessary at times. Use short-acting paralytics to ensure that ongoing seizure activity is not masked. Use EEG monitoring if long-acting paralytics are used and if a question exists about seizure cessation.
Correct any metabolic imbalances. Control hyperthermia.
If seizures continue after 20 minutes, give additional fosphenytoin (10 mg PE/kg IV) or phenytoin (10 mg/kg IV). Aim for a total serum phenytoin level of about 22-25 µg/mL.
In patients with epilepsy partialis continua who had been receiving antiepileptic drug treatment, knowledge of the patient’s usual regimen and current levels may be pivotal. As an alternative to fosphenytoin or phenytoin, supplementation of their routine medication (guided by stat antiepileptic drug levels) may help suppress their seizures.
Failure to respond to optimal benzodiazepine and phenytoin loading operationally defines refractory status epilepticus. If seizures continue after 20 minutes, give phenobarbital (15 mg/kg IV). Use caution when adding barbiturates to benzodiazepines because their coadministration may potentiate ventilatory failure. This may be especially true for patients (eg, elderly patients) with impaired drug clearance.
For this reason, especially in the setting of partially treated epilepsy partialis continua or simple partial status epilepticus, in which the morbidity of the underlying illness is less than in generalized convulsive status epilepticus, a tempered approach may be preferred. Incremental doses of phenobarbital may offer satisfactory efficacy in these uncommon settings and may be safer than full intravenous loading doses, which increase the risk of respiratory suppression.
Alternatives to phenobarbital that are shorter acting and allow for periodic neurologic assessments include the following 18:
If seizures continue, consider administering general anesthesia with medications such as propofol, midazolam, or pentobarbital. Ketamine infusion can alternatively (or additionally) be used in the treatment of refractory status epilepticus, with some evidence of safety and efficacy. These agents are given by IV drip and titrated to a burst-suppression pattern in the EEG trace. In a patient with epilepsy partialis continua or simple partial status epilepticus, one might even consider rapid oral loading of one of the newer antiepileptic drugs (eg, topiramate), depending on the ongoing clinical urgency 21. Lacosamide is a novel antiepileptic drug available in IV form; though anecdotally it appears safe, its effectiveness in treatment of refractory status epilepticus is unknown.
If the patient promptly becomes alert after receiving a benzodiazepine or other antiepileptic drug, that tends to corroborate the diagnosis of status epilepticus. Nevertheless, the failure to become alert by no means excludes the diagnosis of status epilepticus. Most patients remain sleepy or stuporous after the resolution of a prolonged episode of status epilepticus, whether focal or generalized.
For this reason, bedside EEG assessment can be invaluable in guiding treatment decisions. This is true not only early in the treatment paradigm but also late to help gauge the patient’s recovery and to ensure that he or she is not having repeated subclinical seizures. Portable computer-aided EEG monitoring (LTM system) can be particularly helpful in this task.
Antiepileptic Drugs
Since only a small fraction of seizures go on to become status epilepticus, the probability that a given seizure will proceed to status epilepticus is small at the start of the seizure but increases as the seizure duration increases. If a seizure lasts > 5 min, clinical experience suggests that the likelihood of spontaneous termination decreases. The goal of pharmacologic therapy is to achieve rapid and safe termination of the seizure and to prevent its recurrence, without adverse effects on the cardiovascular and respiratory systems or alteration of the level of consciousness. Benzodiazepines (diazepam, lorazepam, midazolam) and hydantoin (phenytoin, fosphenytoin) are the first-line drugs for termination of status epilepticus. These drugs have different pharmacodynamic and pharmacokinetic properties, which determine the rapidity of their clinical effect, their efficacy in terminating status epilepticus, and their duration of action (Table 1). Benzodiazepines carry the disadvantage of excessive sedation, which may interfere with subsequent monitoring of the patient. The benzodiazepines bind to the benzodiazepine binding site on the GABA receptor complex, increasing GABAergic transmission, while the barbiturates act directly on the GABA receptor. The antiseizure activity of phenytoin is complex; however, its major action appears to the blocking of voltage-sensitive, use-dependent sodium channels.
Table 1. Medication List – commonly used drugs for status epilepticus
| Drug | Route | Dose | Comments |
| Midazolam | IV/IO IM Buccal Intranasal | 0.15mg/kg 0.2mg/kg 0.5mg/kg 0.5mg/kg | Max 10mg. Takes effect within minutes but shorter duration of effect than lorazepam. Can depress respiration, particularly if repeated dosing. Is usually short-lived and is usually easily managed with bag-mask-valve ventilatory support. IM midazolam more effective than buccal or intra-nasal routes. Intra-nasal route requires mucosal atomiser device for optimal delivery. Buccal midazolam is twice as effective as rectal diazepam, but both drugs produce the same level and degree of respiratory depression. |
| Diazepam | IV/IO PR | 0.25mg/kg 0.5mg/kg | Max 10mg. Rapid onset, duration less than 1 hour. Well absorbed rectally. Widely used but may now be superseded by the more effective midazolam or lorazepam where available. |
| Lorazepam | IV/IO | 0.1mg/kg | Max 4 mg. Dilute with saline or water to at least twice the ‘neat’ volume and give over 2 minutes. Consider using 0.05mg/kg if prior benzodiazepines or likely to have impaired respiratory drive.Equally or more effective than midazolam and diazepam, possibly less respiratory depression. Longer duration of action (12-24 hours) |
| Phenytoin | IV/IO | 20mg/kg | Max 1g. Give over 20 minutes, made up in 0.9% sodium chloride solution to a maximum concentration of 10mg in 1 ml. Can cause dysrhythmias and hypotension, therefore monitor ECG and BP. Little depressant effect on respiration. |
| Phenobarbitone | IV/IO | 20mg/kg | Max 1g. Give over 20 minutes. Ensure airway support available, often causes respiratory depression. Monitor blood pressure. |
| Paraldehyde | PR | 0.4ml/kg | Max 10 ml. Make up as 50:50 solution in olive oil or 0.9% sodium chloride (avoid Arachis oil because children with peanut allergy may react to it). Can cause rectal irritation. Avoid IM use as causes severe pain and may lead to sterile abscess formation. Paraldehyde causes little respiratory depression. Avoid in liver disease. Takes 10-15 minutes to act, sustained for 2-4 hours. Don’t leave paraldehyde standing in a plastic syringe for longer than a few minutes. |
Abbreviations: IV = intravenous; IO = intraosseous infusion; IM = intramuscular injection; PR = per rectum
Paraldehyde
Paraldehyde is formulated for intramuscular (IM) use. However due to the risks of severe muscle necrosis, the most common method of use is to administer rectally. For rectal (PR) administration, the intramuscular preparation has to be diluted with oil.
Can be administered from plastic syringes if used quickly.
Recommended administration in 20ml syringe attached to 10F feeding tube, inserted 10cm rectally. Hold buttock cheeks together for 2-3min (per rectum [PR] paraldehyde is a powerful gastrointestinal stimulant). Insoluble at room temperature in solutions above 7.8% (1 in 12). Warm ampoules if crystals appear. Do not take from a vial that is discoloured or has been open for a while. Paraldehyde degrades to acetate and acetaldehyde on contact with air, and these may be fatal.
Rectal paraldehyde
May be effective in terminating status epilepticus when IV access is not available.
- Dose: 0.4ml/kg, q 2-4 hours as required
- Method: Dilute 1:2 in olive oil
- Action may be delayed up to 2-4 hours.
- Metabolic acidosis is a possible complication in infants.
Valproate therapy
Valproate can be given intravenously in convulsive status epilepticus.
- Dose = 40 mg/kg IV sodium valproate given over 10 minutes (diluted to a maximum concentration of 50mg/ml with 0.9% sodium chloride or 5% glucose)
Peak levels are reached within 30 minutes, with an effective half-life of approximately 12 hours. A continuous intravenous infusion can also be considered if the initial dose was effective. There are also reports of the effective use of intravenous valproate in nonconvulsive status.
Levetiracetam therapy
- Dose = 40mg/kg IV levetiracetam (maximum 3g) given over 5 minutes. Dilute 1:1 to give concentration of 50mg/1ml with sodium chloride 0.9% or 5% glucose to a minimum of 10ml.
Status epilepticus prognosis
Prognosis is related most strongly to the underlying process causing status epilepticus. For example, if meningitis is the cause, the course of that disease dictates outcome. Patients with status epilepticus from anticonvulsant irregularity or those with alcohol-related seizures generally have a favorable prognosis if treatment is commenced rapidly and complications are prevented.
A multivariate analysis by Drislane et al 22 identified presentation in coma and status epilepticus caused by anoxia/hypoxia as indicators of a poor prognosis. However, in a small case series of cardiac arrest patients who developed postanoxic status epilepticus, predictors of a favorable outcome included preserved brainstem reactions, cortical somatosensory evoked potentials, and EEG reactivity 23. These patients were treated with therapeutic hypothermia.
The more advanced the stage of status epilepticus, the less favorable the response to treatment. In the Veterans Affairs Status Epilepticus Cooperative study, 56% of patients who were first seen with overt, generalized convulsive status epilepticus responded to initial treatment. Only 15% of the individuals with subtle, generalized convulsive status epilepticus responded to initial treatment 24. Treating nonconvulsive status epilepticus is urgent because longer duration of this condition correlates with a worse prognosis 25.
Mortality from status epilepticus
Mortality rates related to status epilepticus have decreased over the last 60 years, probably in relation to faster diagnosis and more aggressive treatment. The probability of death is closely correlated with age. In prospective population-based studies, DeLorenzo et al 26 found mortality rates of 13% for young adults, 38% for the elderly, and >50% for those older than 80 years.
In 1998, the Veterans Affairs Status Epilepticus Cooperative Study Group reported mortality rates of 27% for overt generalized convulsive status epilepticus and 65% for subtle generalized convulsive status epilepticus 24. DeLorenzo et al reported a mortality rate of 21% in patients with generalized status epilepticus, defining mortality as death occurring within 30 days 27.
Aicardi and Chevrie 28 examined 239 children with generalized convulsive status epilepticus that lasted longer than an hour; 26 died, and 88 had permanent neurologic damage (47 of whom had been neurologically intact before the episode).
Death most often is related to an underlying cause of brain injury 29. According to Hauser 30, no more than 2% of patients die directly from status epilepticus.
In a prospective study of 24 status epilepticus patients who died, 10 had a gradual decrease in mean arterial pressure and/or heart rate. The remaining 14 had no cardiac changes until the time of death. About 90% of patients with cardiac decompensation had a history of many risk factors for atherosclerotic cardiovascular disease, whereas only 30% of those without acute cardiac decompensation had clinically significant risk factors 31.
Prognosis in nonconvulsive status epilepticus
Models of partial epilepsy have demonstrated profound and long-lasting neurologic changes after experimental status epilepticus. In human studies, occasional patients have reportedly had profound memory and behavioral changes after episodes of complex partial status epilepticus. In some reports, the duration of the status was linked with these lasting memory deficits. However, most cohorts of patients with nonconvulsive did not undergo prestatus and poststatus neuropsychologic testing to permit direct comparison.
Krumholz and colleagues 32 described 7 cases of serious morbidity and 3 deaths in patients with complex partial status epilepticus. The study has been criticized because many of the patients had severe neurologic or medical insults in addition to status, which may have been pivotal in the genesis of their residual neurologic deficits. Nonetheless, 3 patients had prolonged memory and/or other cognitive deficits, possibly provoked by their status epilepticus.
Data from available studies suggest that nonconvulsive status epilepticus alone usually does not cause irreversible neurologic injury, though rare instances may occur. However, nonconvulsive status epilepticus appears so often in the company of serious neurologic or medical injury that clinically significant morbidity and mortality are common.
Patients with focal motor status epilepticus (ie, epilepsy partialis continua) have a particularly poor prognosis if they are untreated in the setting of Rasmussen encephalitis.
In the author’s series of patients with focal status epilepticus, patients with new neurologic insults (eg, acute stroke) or those whose status epilepticus occurred postoperatively had a mortality rate of 67%. Those with a history of epilepsy did well overall. In this group, status epilepticus was usually precipitated by a new toxic and/or metabolic or other medical aggravator and had little to no lasting neurologic aftereffects.
The author compared patients with recurrent seizures with those who had ongoing, continuous seizure activity. No difference in outcome was observed between the subgroups of focal status epilepticus.
- Cherian A, Thomas SV. Status epilepticus. Ann Indian Acad Neurol. 2009;12(3):140–153. doi:10.4103/0972-2327.56312 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2824929[↩][↩][↩][↩]
- Wylie T, Murr N. Status Epilepticus. [Updated 2019 Jun 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430686[↩][↩][↩]
- Won SY, Dubinski D, Sautter L, Hattingen E, Seifert V, Rosenow F, Freiman T, Strzelczyk A, Konczalla J. Seizure and status epilepticus in chronic subdural hematoma. Acta Neurol. Scand. 2019 May 18;[↩]
- Horváth L, Fekete I, Molnár M, Válóczy R, Márton S, Fekete K. The Outcome of Status Epilepticus and Long-Term Follow-Up. Front Neurol. 2019;10:427.[↩]
- The Epilepsies and Seizures: Hope Through Research. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Hope-Through-Research/Epilepsies-and-Seizures-Hope-Through#3109_19[↩]
- Shorvon S. Status epilepticus: Its clinical features and treatment in children and adults. Cambridge, England: Cambridge University Press; 1994. p. 201e.[↩][↩][↩]
- Jobst BC, Ben-Menachem E, Chapman KE, Fu A, Goldman A, Hirsch LJ, Jehi LE, Kossoff EH, Plueger M, Rho JM, Schevon CA, Shinnar S, Sperling MR, Simeone TA, Wagner JL, Lado F. Highlights From the Annual Meeting of the American Epilepsy Society 2018. Epilepsy Curr. 2019 May-Jun;19(3):152-158.[↩]
- Logroscino G, Hesdorffer DC, Cascino GD, Annegers JF, Bagiella E, Hauser WA. Long-term mortality after a first episode of status epilepticus. Neurology. 2002;58:537–41.[↩]
- DeLorenzo RJ, Pellock JM, Towne AR, Boggs JG. Epidemiology of status epilepticus. J Clin Neurophysiol. 1995;12:316–25.[↩]
- Husain AM, Horn GJ, Jacobson MP. Non-convulsive status epilepticus: Usefulness of clinical features in selecting patients for urgent EEG. J Neurol Neurosurg Psychiatry. 2003;74:189–91.[↩]
- Tomson, T. , Lindbom, U. and Nilsson, B. Y. (1992), Nonconvulsive Status Epilepticus in Adults: Thirty‐Two Consecutive Patients from a General Hospital Population. Epilepsia, 33: 829-835. doi:10.1111/j.1528-1157.1992.tb02190.x[↩]
- Langenbruch L, Krämer J, Güler S, Möddel G, Geßner S, Melzer N, Elger CE, Wiendl H, Budde T, Meuth SG, Kovac S. Seizures and epilepsy in multiple sclerosis: epidemiology and prognosis in a large tertiary referral center. J. Neurol. 2019 May 08.[↩]
- Crawley J, Smith S, Kirkham F, Muthinji P, Waruiru C, Marsh K. Seizures and status epilepticus in childhood cerebral malaria. Q J Med. 1996;89:591–7.[↩]
- Misra UK, Kalita J, Nair PP. Status epilepticus in central nervous system infections: An experience from a developing country. Am J Med. 2008;121:618–23.[↩]
- Sánchez Fernández I, Gaínza-Lein M, Lamb N, Loddenkemper T. Meta-analysis and cost-effectiveness of second-line antiepileptic drugs for status epilepticus. Neurology. 2019 May 14;92(20):e2339-e2348.[↩]
- Müllges W. [Diagnosis and treatment of status epilepticus in the intensive care unit]. Med Klin Intensivmed Notfmed. 2019 Jun;114(5):475-484.[↩]
- [Guideline] Glauser, T. et al. Treatment of Convulsive Status Epilepticus in Children and Adults: Report of the Guideline Committee of the American Epilepsy Society. Epilepsy Currents. Jan/Feb 2016. 16(1):48-61.[↩]
- Arif H, Hirsch LJ. Treatment of status epilepticus. Semin Neurol. 2008 Jul. 28(3):342-54.[↩]
- Iyer VN, Hoel R, Rabinstein AA. Propofol infusion syndrome in patients with refractory status epilepticus: an 11-year clinical experience. Crit Care Med. 2009 Dec. 37(12):3024-30.[↩]
- Synowiec AS, Singh DS, Yenugadhati V, Valeriano JP, Schramke CJ, Kelly KM. Ketamine use in the treatment of refractory status epilepticus. Epilepsy Res. 2013 Jan 28.[↩]
- Blumkin L, Lerman-Sagie T, Houri T, Gilad E, Nissenkorn A, Ginsberg M, et al. Pediatric refractory partial status epilepticus responsive to topiramate. J Child Neurol. 2005 Mar. 20(3):239-41.[↩]
- Drislane FW, Blum AS, Lopez MR, Gautam S, Schomer DL. Duration of refractory status epilepticus and outcome: Loss of prognostic utility after several hours. Epilepsia. 2009 Jan 19.[↩]
- Rossetti AO, Oddo M, Liaudet L, Kaplan PW. Predictors of awakening from postanoxic status epilepticus after therapeutic hypothermia. Neurology. 2009 Feb 24. 72(8):744-9.[↩]
- Treiman DM, Meyers PD, Walton NY, et al. A comparison of four treatments for generalized convulsive status epilepticus. Veterans Affairs Status Epilepticus Cooperative Study Group. N Engl J Med. 1998 Sep 17. 339(12):792-8.[↩][↩]
- Thomas P. How urgent is the treatment of nonconvulsive status epilepticus?. Epilepsia. 2007. 48 Suppl 8:44-5.[↩]
- DeLorenzo RJ, Hauser WA, Towne AR, et al. A prospective, population-based epidemiologic study of status epilepticus in Richmond, Virginia. Neurology. 1996 Apr. 46(4):1029-35.[↩]
- DeLorenzo RJ, Pellock JM, Towne AR, Boggs JG. Epidemiology of status epilepticus. J Clin Neurophysiol. 1995 Jul. 12(4):316-25.[↩]
- Aicardi J, Chevrie JJ. Convulsive status epilepticus in infants and children. A study of 239 cases. Epilepsia. 1970 Jun. 11(2):187-97.[↩]
- Lowenstein DH, Alldredge BK. Status epilepticus. N Engl J Med. 1998 Apr 2. 338(14):970-6.[↩]
- Hauser WA. Status epilepticus: epidemiologic considerations. Neurology. 1990 May. 40(5 Suppl 2):9-13.[↩]
- Boggs JG, Marmarou A, Agnew JP, et al. Hemodynamic monitoring prior to and at the time of death in status epilepticus. Epilepsy Res. 1998 Aug. 31(3):199-209.[↩]
- Krumholz A, Sung GY, Fisher RS, Barry E, Bergey GK, Grattan LM. Complex partial status epilepticus accompanied by serious morbidity and mortality. Neurology. 1995 Aug. 45(8):1499-504.[↩]