Suprascapular neuropathy
Suprascapular neuropathy also known as suprascapular nerve entrapment or suprascapular nerve neuropathy, is associated with upper extremity weakness and shoulder pain and suprascapular neuropathy is usually caused by trauma or strenuous activities 1. The most common lesion occurs at the suprascapular notch, resulting in paralysis of the common trunk of the suprascapular nerve with supraspinatus and infraspinatus hypotrophy 2. Suprascapular nerve neuropathy is a less common cause of shoulder pain in athletes but is seen particularly in those who participate in overhead activities. Athletes who participate regularly in overhead sports are more susceptible to developing suprascapular neuropathy. Sports such as baseball, volleyball, and tennis demand skills that place substantial load on the athlete’s shoulder when the upper limb is in an overhead or abducted and externally rotated position. Volleyball players with increased range of motion of the shoulder girdle appear to be more likely to suffer suprascapular nerve entrapment with isolated paralysis of the infraspinatus muscle.
The suprascapular nerve is a mixed nerve that provides the motor innervation of the supraspinatus and infraspinatus muscles and the sensory and proprioceptive innervation of the posterior aspect of the glenohumeral joint, as well as the acromioclavicular joint, subacromial bursa, and scapula 3. Although the suprascapular nerve is a mixed nerve, it typically carries no cutaneous afferent fibers. The suprascapular nerve is thought to carry cutaneous afferent fibers in only 15-25% of the general population.
Epidemiologic studies have demonstrated that athletes who participate in these and other overhead sports are at higher risk for overuse injuries of the shoulder in particular, including rotator cuff tendinopathy and injuries to the glenoid labrum 4. Suprascapular neuropathy has been reported to cause 1-2% of all shoulder pain 5 and is therefore often overlooked. However, the prevalence in higher risk athletic populations, such as volleyball players, has been reported to be as high as 33% 5. Therefore, suprascapular neuropathy should be considered when evaluating shoulder pain in an overhead athlete.
Studies have reported that 13-33% of elite volleyball athletes have signs of suprascapular neuropathy 5. This observation lends credence to the term “volleyball shoulder.”
In addition to overhead athletes, some other higher risk populations for suprascapular neuropathy include patients with massive rotator cuff tears resulting in fatty infiltration of the muscle. Patients with posterior labral tears resulting in paralabral cysts that can compress the nerve are also a higher risk population 5.
Causes for suprascapular neuropathy may include repetitive overhead activities, traction from a rotator cuff tear, and compression from a space-occupying lesion at the suprascapular or spinoglenoid notch. Suprascapular neuropathy may be associated with a rotator cuff tear, especially tears bigger than 3 cm 6. The proposed mechanism involves suprascapular nerve nerve traction that is caused by tethering of the suprascapular nerve nerve against fixed location points; these are the major and minor scapular notches 7.
Suprascapular nerve anatomy
The suprascapular nerve is derived from the upper trunk of the brachial plexus, receiving its axons from the fifth and sixth cervical roots 8. Some authors suggest that the nerve may also receive contributions from the fourth cervical nerve root in as many as 25% of people. Mestdagh et al 9 found, in their study on 20 human cadavers, almost no variation between different subjects in the origin of the suprascapular nerve. The suprascapular nerve then courses laterally through the posterior triangle of the neck across the scalenus medius muscle, under the trapezius and omohyoideus to enter the supraspinous fossa by obliquely passing through the suprascapular notch. The suprascapular nerve continues its course laterally in the supraspinatus fossa, where it is in direct contact with the belly of the supraspinatus muscle. The suprascapular nerve provides motor fibers to the supraspinatus through fibro-osseous foramina and a sensory fiber to the subacromial bursa and glenohumeral and acromioclavicular joints. The suprascapular nerve continues its course by curving around the lateral border of the spine of the scapula, the spinoglenoid notch, to gain entrance to the infraspinatus fossa. This notch is covered by the inferior transverse ligament or spinoglenoid ligament, a narrow fibrous band that forms a separation between the supraspinatus and infraspinatus muscle. The prevalence of this ligament has been reported to range from 50 to 72% 10. The suprascapular nerve then completes its course at a right angle and travels medially to the scapular spine. The suprascapular nerve is held against the bone by the belly and musculotendinous part of the infraspinatus muscle and provides several successive branches to the belly of the infraspinatus muscle. Mestdagh et al 9 have shown that, in contrast with its origin, individual variation in the terminal branches of the suprascapular nerve is possible. Ferretti et al 11 postulated players whose suprascapular nerve divides into three terminal branches instead of into a plexus of motor branches may be susceptible to the injury. When this variant is present, the suprascapular nerve forms an acute angle as it curves around the lateral edge of the spine of the scapula. It cannot be excluded that this variation may partly explain why some volleyball players become injured and others do not. There are no skin sensory endings for the suprascapular nerve as it is a motor nerve.
The suprascapular nerve is susceptible to entrapment or traction injury because it traverses various scapular recesses 12. Acute injury of the suprascapular nerve is often caused by direct trauma, such as fracture or dislocation of the shoulder. However, chronic lesions of this nerve result from repetitive microtrauma associated with forceful occupational and sports activities 12. The supraspinatus and infraspinatus muscles assist in the abduction and external rotation of the shoulder, as well as stabilization of the shoulder girdle. Weakness of these muscles is manifested as altered ability to externally rotate the shoulder, which might lead to abnormal scapular motion. Altered scapular motion can further aggravate supraspinatus and infraspinatus weakness and result in shoulder dysfunction 13.
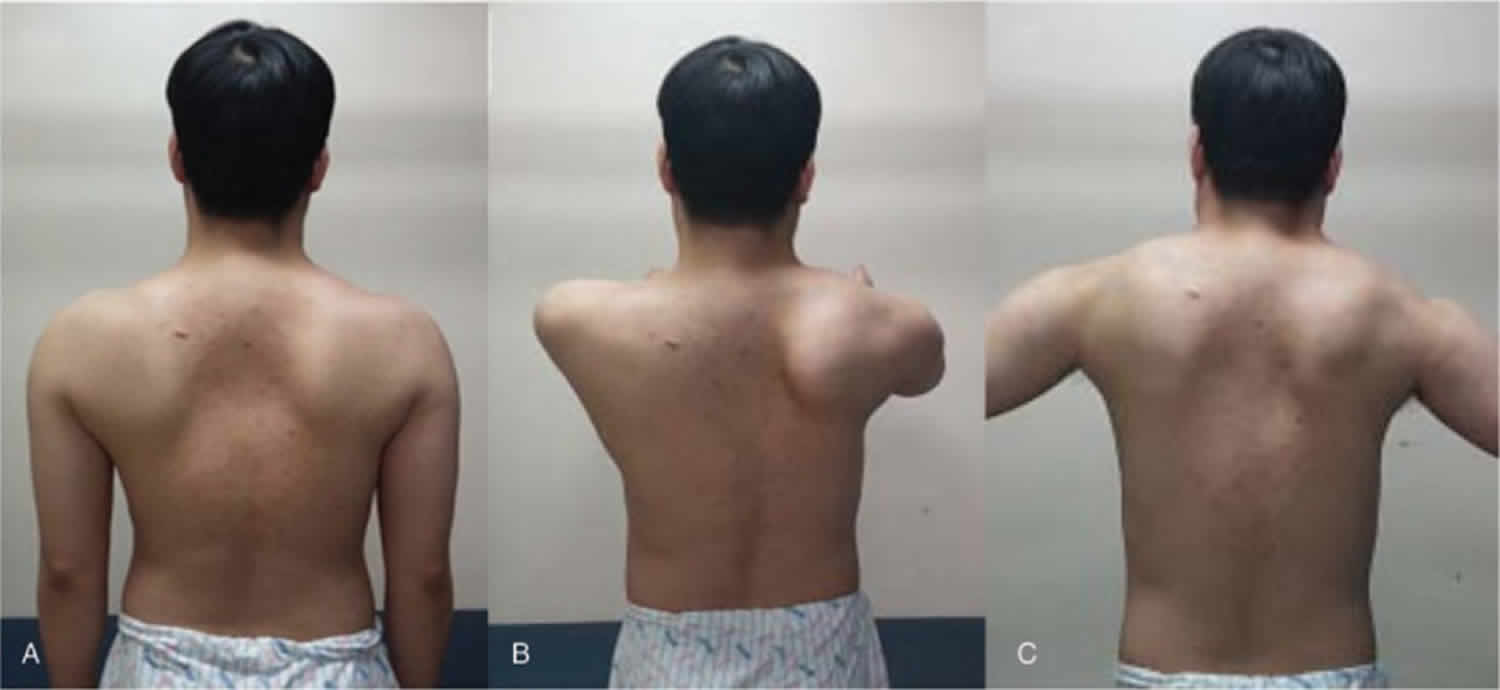
Figure 1. Suprascapular nerve
 Footnote: Clinically relevant anatomy of the suprascapular nerve and the structures it innervates. The suprascapular nerve is vulnerable to entrapment at the superior scapular notch and the spinoglenoid notch, beneath the inferior transverse scapular ligament. The inset depicts the clinical appearance in an individual with predominantly right-sided atrophy of the infraspinatus muscle due to suprascapular neuropathy.
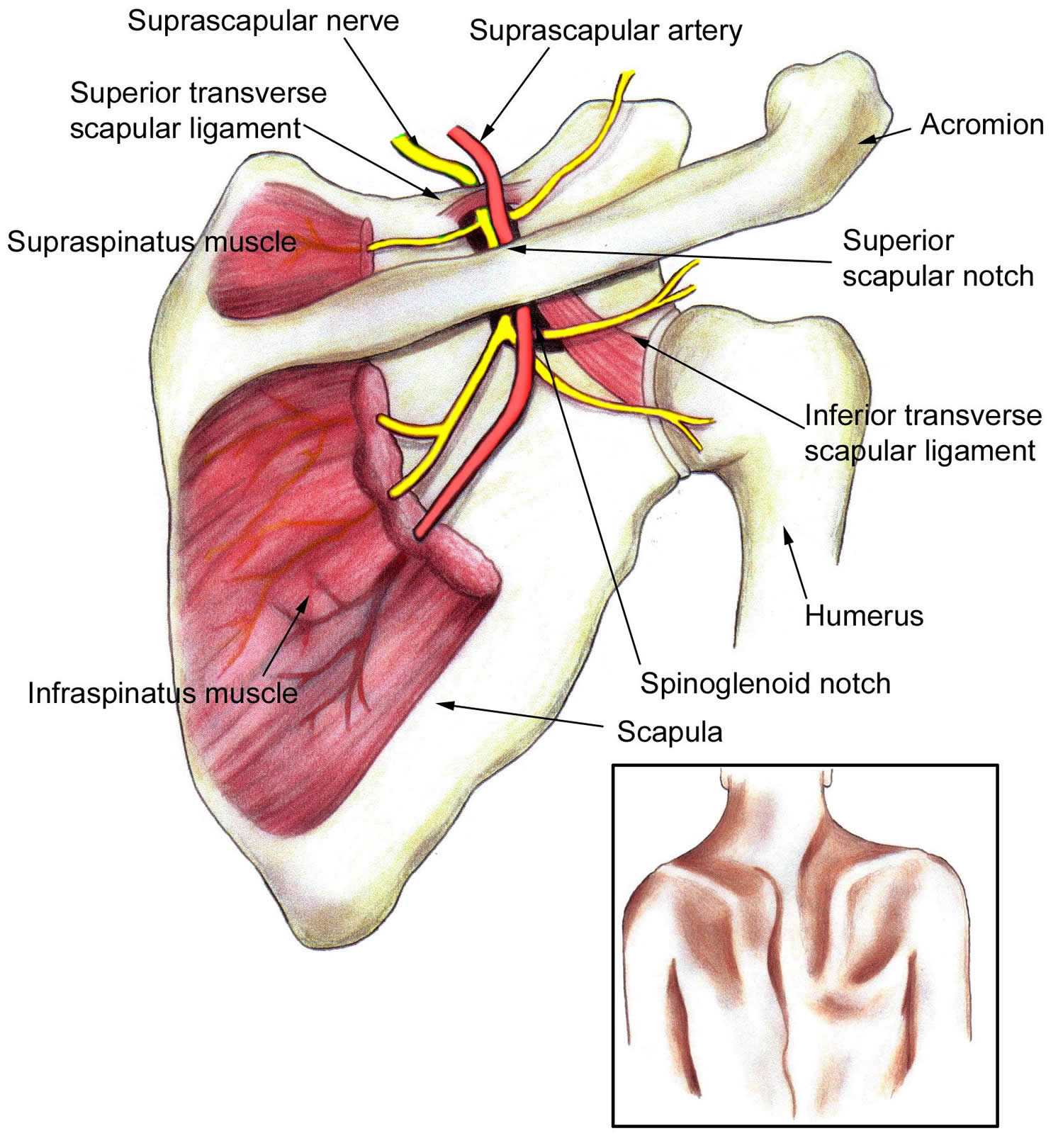
Footnote: Clinically relevant anatomy of the suprascapular nerve and the structures it innervates. The suprascapular nerve is vulnerable to entrapment at the superior scapular notch and the spinoglenoid notch, beneath the inferior transverse scapular ligament. The inset depicts the clinical appearance in an individual with predominantly right-sided atrophy of the infraspinatus muscle due to suprascapular neuropathy.Figure 2. Suprascapular neuropathy
Footnote: Inspection of the patient’s scapula at admission in neutral (A), shoulder flexion (B), and shoulder abduction (C) positions.
Suprascapular nerve entrapment causes
Sports that place a substantial load on the athlete’s shoulder when the upper limb is in an overhead or abducted and externally rotated position may precipitate suprascapular neuropathy 14. The site of suprascapular nerve entrapment determines whether the infraspinatus muscle alone or both the supraspinatus and infraspinatus muscles are affected.
Although sports-related overuse mechanisms of suprascapular nerve injury are the most common causes, the suprascapular nerve can also be damaged as a result of direct trauma as well as iatrogenic factors. The relationship of the nerve to the clavicle makes it vulnerable to injury after a clavicular fracture occurs. Surgical procedures involving the shoulder (eg, Bankhart repair) can place the nerve at risk for either direct injury or indirect injury. Interestingly, suprascapular neuropathy has also been reported to occur after positioning patients for spinal surgery.
Other diagnoses should be considered. Most commonly, the clinician diagnoses rotator cuff tendinopathy and prescribes a conservative treatment program. Because the rehabilitation programs for rotator cuff tendinopathy and infraspinatus syndrome are similar, in many (perhaps most) instances, the patient’s condition improves, and the correct diagnosis goes unrecognized. Delayed-onset muscular soreness may be present, but this soreness is not expected to progress over 3 weeks. Rather, symptoms of delayed-onset muscular soreness tend to spontaneously resolve over 7-10 days.
Suprascapular neuropathy prevention
Ferretti 11 proposed that suprascapular neuropathy in volleyball players is related to performance of the floater serve. If so, the incidence of volleyball shoulder is expected to decrease because, with the advent of the jump serve or spike serve, the floater serve has become less popular.
To the author’s knowledge, no definitive study findings implicate specific spiking styles in suprascapular neuropathy; thus, providing technical advice about biomechanics to volleyball athletes with suprascapular neuropathy is difficult 11. Additional considerations remain unanswered; for example, the duration and magnitude of the load that is sufficient to precipitate volleyball shoulder through chronic overuse is unknown. Furthermore, the extent to which a SICK scapula is associated with the incidence of suprascapular neuropathy deserves further investigation.
Suprascapular neuropathy symptoms
Although knowledge of the clinical symptom complex has improved since Kopell and Thompson 15 first reported shoulder pain as the result of suprascapular nerve injury in 1959, from a practical standpoint, the diagnosis of suprascapular neuropathy remains largely a diagnosis of exclusion unless the clinician remains alert to the diagnostic possibility when the affected athlete initially presents for treatment.
The typical patient is a young overhead athlete who reports vague posterior shoulder pain. Although, the athlete can have painless atropy presenting as supraspinatus and/or infraspinatus weakness, depending on the location of the suprascapular nerve.
Because of the anatomy, more distal nerve injuries are often relatively painless. In particular, nerve injuries at the spinoglenoid notch that result in selective denervation of the infraspinatus muscle may be insidious in their onset due to the relative lack of pain. In Ferretti et al’s 16 series, elite volleyball players with isolated atrophy of the infraspinatus generally did not report any pain or sports-related functional disability.
Based on anatomic considerations, athletes with more proximal lesions of the suprascapular nerve that affect both the supraspinatus and infraspinatus muscles are more likely to have pain and symptom-limited function than are individuals with distal nerve lesions that affect only the infraspinatus.
Although case reports of bilateral involvement exist, symptoms are typically unilateral and involve the dominant side.
Male athletes account for most of the cases reported in the literature; however, Ferretti et al 16 reported one series of 38 athletes in which the incidence was approximately equal among males and females.
More often than not, the pain (when present) is described as a deep, dull, aching discomfort.
Activities that involve overhead motions or sport-specific skills may exacerbate symptoms. Diagnostic signs may include weakness and compromised endurance in performing overhead, sport-specific skills.
Genetic factors undoubtedly play a role in the predisposition and susceptibility of individual athletes to suprascapular neuropathy, but the specific factors that are involved have yet to be elucidated.
Physical examination
Atrophy of the supraspinatus and/or infraspinatus muscles may be present on the physical examination, depending on the site of the suprascapular nerve entrapment.
Note that supraspinatus involvement may be frequently overlooked because of the bulk of the overlying trapezius.
Manual muscle testing may reveal relative weakness of ipsilateral shoulder abduction (a function of the supraspinatus muscle in addition to the deltoid muscle) and/or weakness of external rotation (a function of the infraspinatus muscle in addition to the teres minor muscle).
The athlete may report worsening pain with cross-body adduction or internal rotation of the ipsilateral upper limb 17.
Pressure applied over the suprascapular or spinoglenoid notches may elicit pain. Tenderness may between the clavicle and the spine of the scapula or deep and posterior to the acromioclavicular joint 5.
Muscle stretch reflexes are unaffected by this condition.
Rarely, cutaneous appreciation of sensory modalities may be affected in an approximate axillary nerve distribution.
Suprascapular neuropathy diagnosis
When suprascapular neuropathy is suspected, radiography should be performed. In addition to standard views, suprascapular notch and Stryker views can be ordered 17. In suprascapular neuropathy, conventional radiographic findings in the shoulder girdle are typically unremarkable in the absence of bony trauma that may account for the condition (eg, fractured clavicle). Conventional radiography of the cervical spine is warranted if concern exists about a possible radicular etiology for the patient’s symptoms.
Shoulder MRI may reveal supraspinatus or infraspinatus muscle edema in acute cases and atrophy with fatty replacement in more chronic cases 18.
MRI may also reveal a ganglion cyst or other mass such as a paralabral cyst with resultant suprascapular nerve compression 19.
3-T magnetic resonance neurography has been shown to be a valuable diagnostic tool in clinically suspected suprascapular neuropathy. It can demonstrate the nerve abnormality and any secondary muscle denervation changes 20.
Ultrasonography is a reasonable, less expensive initial imaging option 18. The suprascapular nerve can be identified under ultrasound, and can be used to screen for parascapular ganglia or masses 21. Spinoglenoid notch cysts can be identified with ultrasound, particularly in a lean athletic population 22.
Suprascapular nerve entrapment test
The clinical diagnosis of suprascapular neuropathy may be confirmed with electrodiagnostic testing and has been the criterion standard for diagnosis of suprascapular neuropathy. Electromyography (EMG) and nerve conduction velocity studies remain the standard for diagnosis of suprascapular neuropathy 23.
The normal distal motor latencies to the supraspinatus muscles during stimulation at the Erb point are 2.7 msec ± 0.5 and and to the infraspinatus muscles, 3.3 msec ± 0.5.
Side-to-side differences greater than 0.4 msec suggest focal entrapment of the suprascapular nerve or other neural injury.
Electromyography (EMG) may reveal the following:
- Evidence of denervation, such as positive sharp waves and fibrillation potentials
- Motor unit recruitment abnormalities, such as motor unit dropout in acute cases and polyphasic motor unit action potentials in cases of long-term neuropathy. This latter finding suggests a degree of reinnervation.
- The physical examination and electrodiagnostic test results should enable the clinician to rule out underlying cervical radiculopathy, brachial plexopathy, or axillary neuropathy and to localize the site of suprascapular nerve impairment.
Suprascapular neuropathy treatment
The treatment for suprascapular neuropathy depends on the cause, severity, and duration of the symptoms; degree of functional disability; and patient preference. In the absence of specific compressive lesions, conservative initial treatment for suprascapular neuropathy is recommended. The natural history of suprascapular neuropathy is typically favorable, and most cases respond to conservative care within 6 months.
In athletes without pain or limitations in the performance of sport-specific skills, a simple program of exercises for scapular stabilization/mobilization and rotator cuff strengthening is probably reasonable. Such a program should prevent not only progression of the condition, but also secondary impingement of the rotator cuff.
A similar program is recommended in symptomatic athletes; however, activity modification to limit symptoms during the acute phase is warranted. The athlete should then progress through a series of functionally oriented exercises designed to restore flexibility and proprioception, scapular control, and balanced rotator cuff strength and endurance. This program should culminate in the resumption of sport-specific skills.
The use of passive modalities (eg, superficial or deep heat application, iontophoresis) and/or injection procedures for pain relief (see Other Treatment) may help symptomatic athletes make the transition to such exercise programs.
On the basis of reports in the available literature, nonsurgical care should result in a satisfactory outcome in most idiopathic cases within 6-8 months. Most reports indicate that patients who are treated conservatively are generally able to resume their previous level of function, including high-level sports participation.
Longitudinal follow-up findings suggest that muscular atrophy is generally not reversible to a significant extent, although symptoms of pain may improve with time. The athlete may return to play when he or she is able to perform appropriate skills without provoking symptoms.
Ideally, the rehabilitation program should extend beyond the mere resolution of symptoms to address the other facets of Kibler’s “vicious cycle” 24. The rehabilitation program should include an analysis of the athlete’s technique to determine if any flaws or compensatory biomechanical changes need to be corrected to minimize the risk of recurrent injury or overload of other soft tissues further down the kinetic chain.
Surgical treatment
Should conservative care fail to resolve the symptoms and allow the athlete to return to the sport activity, surgical intervention may be therapeutic. A degree of controversy exists in the literature because some authors believe that early surgical intervention is the treatment of choice.
Described surgical treatment procedures for suprascapular neuropathy unrelated to a space-occupying lesion include simple widening of the spinoglenoid notch or suprascapular notch, depending on the site of nerve injury. In one retrospective review of 3 cases of idiopathic infraspinatus syndrome refractory to conservative care, subsequent surgery was beneficial in 2 cases.
Some authors argue that documented compressive lesions of the suprascapular nerve (eg, ganglia) should be promptly resected because of the high failure rate of nonsurgical care in this situation. Any accompanying labral pathology can be simultaneously repaired, if indicated. Both open and arthroscopic procedures have been described 25.
In general, surgical outcomes reported in the literature are good. Patients in whom the condition is diagnosed promptly and treated with early surgical decompression seem to have a better likelihood of regaining full muscular strength and bulk 26. The patient should participate in a postoperative program of rehabilitation and/or functional restoration to ensure the return of balanced strength and flexibility.
Other treatment
In addition to the approaches discussed above (see Physical therapy and Surgical intervention), other nonsurgical treatment options include suprascapular nerve blocks 27. Because such blocks have been used to manage perioperative shoulder pain and adhesive capsulitis in addition to other painful shoulder conditions, the diagnostic use and specificity of such blocks is debatable. Nevertheless, blocks may provide symptomatic relief, thereby permitting the patient to more fully participate in a rehabilitation program.
The injection of an anesthetic and/or corticosteroid mixture into the suprascapular notch may provide temporary benefit. Given the variability in sensitivity and specificity of electromyography and nerve conduction studies 17. injections can be an important diagnostic tool to confirm that the pain is in fact from suprascapular neuropathy.
Several studies have reported good clinical results with ultrasound-guided paralabral cyst aspiration; thus, it can be considered as an alternative to operative management 17. However, cyst recurrence rate has been reported between 75-100% 17.
In select cases, radiofrequency suprascapular neuropathy ablative procedures may provide longer symptomatic relief. Several injection approaches to minimize the inherent risk of pneumothorax are described. However, such interventions are purely palliative and do not alter or address the underlying mechanism of suprascapular neuropathy.
Return to play
Most individuals with suprascapular neuropathy are asymptomatic and compete with little to no discernible performance deficit. This observation complicates the issue of how to handle the return-to-play decision in an athlete who is asymptomatic and whose physical examination incidentally reveals suprascapular neuropathy.
In practical terms, elite athletes (in whom the prevalence is highest) can probably continue to compete while they are concurrently participating in a rehabilitation program. However, to minimize the progression of the condition, the extent to which the athlete performs overhead skills during practice should be limited.
In symptomatic athletes, a more restrictive course seems reasonable. Once the athlete can perform sport-specific skills (eg, spiking and blocking in volleyball) in a pain-free manner, he or she can return to play. Athletes who undergo surgical decompression should participate in an appropriate postoperative rehabilitation program to restore their strength, flexibility, and endurance before returning to play.
Suprascapular neuropathy prognosis
Suprascapular neuropathy prognosis for a favorable clinical outcome is good. At the time of diagnosis, affected athletes report surprisingly little functional limitation. According to the literature, most cases respond favorably to either conservative treatment programs or when indicated, surgical intervention. Furthermore, most athletes were able to return to their previous level of sports participation following therapeutic intervention.
- Suprascapular neuropathy in volleyball players. Ferretti A, Cerullo G, Russo G. J Bone Joint Surg Am. 1987 Feb; 69(2):260-3.[↩]
- Steiman I. Painless infraspinatus atrophy due to suprascapular nerve entrapment. Arch Phys Med Rehabil1988;69:641–3.[↩]
- Antoniadis G, Richter HP, Rath S, Braun V, Moese G. Suprascapular nerve entrapment: experience with 28 cases. J Neurosurg. 1996 Dec. 85(6):1020-5.[↩]
- Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology Part III: The SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitation. Arthroscopy. 2003 Jul-Aug. 19(6):641-61.[↩]
- Boykin RE, Friedman DJ, Higgins LD, Warner JJ. Suprascapular neuropathy. J Bone Joint Surg Am. 2010 Oct 6. 92(13):2348-64.[↩][↩][↩][↩][↩]
- Arthroscopic suprascapular nerve release: indications and technique. Lafosse L, Piper K, Lanz U. J Shoulder Elbow Surg. 2011 Mar; 20(2 Suppl):S9-13.[↩]
- Sachinis NP, Boutsiadis A, Papagiannopoulos S, Ditsios K, Christodoulou A, Papadopoulos P. Suprascapular neuropathy in the setting of rotator cuff tears: study protocol for a double-blinded randomized controlled trial. Trials. 2016;17(1):554. Published 2016 Nov 22. doi:10.1186/s13063-016-1672-y https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5120427[↩]
- Witvrouw E, Cools A, Lysens R, et al. Suprascapular neuropathy in volleyball players. British Journal of Sports Medicine 2000;34:174-180.[↩]
- Mestdagh H, Deinzenkoa D, Ghestem P. Anatomical bases of suprascapular nerve syndrome. Anatomia Clinica1981;3:67–71.[↩][↩]
- Demaio M, Drez D, Mullins RC. The inferior transverse scapular ligament as a possible cause of entrapment neuropathy of the nerve to the infraspinatus. J Bone Joint Surg [Am]1991;73:1061–3.[↩]
- Ferretti AG, Cerullo G, Russo G. Suprascapular neuropathy in volleyball players. J Bone Joint Surg [Am]1987;77:1061–3.[↩][↩][↩]
- Prevalence of latent and manifest suprascapular neuropathy in high-performance volleyball players. Holzgraefe M, Kukowski B, Eggert S. Br J Sports Med. 1994 Sep; 28(3):177-9.[↩][↩]
- Supraspinatus and infraspinatus weakness in overhead athletes with scapular dyskinesis: strength assessment before and after restoration of scapular musculature balance. Merolla G, De Santis E, Campi F, Paladini P, Porcellini G. Musculoskelet Surg. 2010 Dec; 94(3):119-25.[↩]
- Suprascapular Neuropathy Clinical Presentation. https://emedicine.medscape.com/article/92672-clinical[↩]
- Koppell HP, Thompson WAL. Peripheral entrapment neuropathies. Baltimore: Williams & Wilkins, 1963.[↩]
- Ferretti A, De Carli A, Fontana M. Injury of the suprascapular nerve at the spinoglenoid notch. The natural history of infraspinatus atrophy in volleyball players. Am J Sports Med. 1998 Nov-Dec. 26(6):759-63.[↩][↩]
- Moen TC, Babatunde OM, Hsu SH, Ahmad CS, Levine WN. Suprascapular neuropathy: what does the literature show?. J Shoulder Elbow Surg. 2012 Jun. 21(6):835-46.[↩][↩][↩][↩][↩]
- Hill LJ, Jelsing EJ, Terry MJ, Strommen JA. Evaluation, treatment, and outcomes of suprascapular neuropathy: a 5-year review. PM R. 2014 Sep. 6 (9):774-80.[↩][↩]
- Inokuchi W, Ogawa K, Horiuchi Y. Magnetic resonance imaging of suprascapular nerve palsy. J Shoulder Elbow Surg. 1998 May-Jun. 7(3):223-7.[↩]
- Ahlawat S, Wadhwa V, Belzberg AJ, Batra K, Chhabra A. Spectrum of suprascapular nerve lesions: normal and abnormal neuromuscular imaging appearances on 3-T MR neurography. AJR Am J Roentgenol. 2015 Mar. 204 (3):589-601.[↩]
- Hashimoto BE, Hayes AS, Ager JD. Sonographic diagnosis and treatment of ganglion cysts causing suprascapular nerve entrapment. J Ultrasound Med. 1994 Sep. 13(9):671-4.[↩]
- Martinoli C, Bianchi S, Pugliese F, et al. Sonography of entrapment neuropathies in the upper limb (wrist excluded). J Clin Ultrasound. 2004 Nov-Dec. 32(9):438-50.[↩]
- Suprascapular Neuropathy. JBJS: October 6, 2010 – Volume 92 – Issue 13 – p 2348-2364 doi: 10.2106/JBJS.I.01743[↩]
- Kibler WB, Herring SA, Press JM, Lee PA, eds. Functional Rehabilitation of Sports and Musculoskeletal Injuries. Gaithersburg, Md: Aspen Publishers; 1998.[↩]
- Memon M, Kay J, Ginsberg L, Simunovic N, Bak K, Lapner P, et al. Arthroscopic management of suprascapular neuropathy of the shoulder improves pain and functional outcomes with minimal complication rates. Knee Surg Sports Traumatol Arthrosc. 2018 Jan. 26 (1):240-266.[↩]
- Momaya AM, Kwapisz A, Choate WS, Kissenberth MJ, Tolan SJ, Lonergan KT, et al. Clinical outcomes of suprascapular nerve decompression: a systematic review. J Shoulder Elbow Surg. 2018 Jan. 27 (1):172-180.[↩]
- Jones DS, Chattopadhyay C. Suprascapular nerve block for the treatment of frozen shoulder in primary care: a randomized trial. Br J Gen Pract. 1999 Jan. 49(438):39-41.[↩]